Abstract
Previous studies have indicated that high neuroticism is associated with early mortality. However, recent work suggests that people's level of neuroticism changes over long periods of time. We hypothesized that such changes in trait neuroticism affect mortality risk. Growth-curve parameters (levels and slopes) that quantified the trajectories of neuroticism change over 12 years were used to predict 18-year risk of mortality among 1,663 aging men. Proportional hazards models were used to estimate mortality risk from level and slope parameters, controlling for objective and subjective health, depression, and age. Although a parallel analysis of extraversion showed no significant effects, level and slope of neuroticism interacted in their effect on mortality. Men who had both a high average level of neuroticism and an increasing level of neuroticism over time had much lower survival than men without that combination. These findings suggest that it is not just the level of personality traits, but their direction of change, that is related to mortality.
Personality traits have emerged as important predictors of all-cause mortality (Friedman, 2000; Friedman et al., 1993; Maier & Smith, 1999). Although perhaps the best known of these predictors is low conscientiousness, high neuroticism and low extraversion have also been associated with an elevated mortality risk (Almada et al., 1991; Christensen et al., 2002; Danner, Snowdon, & Friesen, 2001; Friedman et al., 1993; Maruta, Colligan, Malinchoc, & Offord, 2000; Wilson, Mendes de Leon, Bienas, Evans, & Bennett, 2004).
However, if traits change over time, do such changes alter mortality risk? This question is important, because recent studies have shown that many people exhibit long-term trait change. Recent reports have demonstrated individual differences in the rate of change in neuroticism, extraversion, and other traits (Mroczek & Spiro, 2003; Small, Hertzog, Hultsch, & Dixon, 2003). Some people's trait levels are stable, whereas other people's levels change. The present study examined the association between rate of change in two traits, neuroticism and extraversion, and mortality risk over an 18-year period. We hypothesized that if higher neuroticism leads to higher risk of mortality, then long-term declines in neuroticism should bring about a reduction in the risk. Similarly, increases in extraversion should also bring about a reduced mortality risk.
There are several possible explanations for the personality-mortality link. Persons high in neuroticism, for example, may engage in poor health behaviors that contribute to earlier mortality (Friedman, 2000). In addition, higher neuroticism is associated with lower effectiveness in managing stress and higher levels of negative emotions (Bolger & Schilling, 1991; Larsen & Ketelaar, 1991; Mroczek & Almeida, 2004; Suls, Green, & Hillis, 1998; Watson & Clark, 1994). Both ineffective management of stress and negative affect have been linked to poor physical outcomes or mortality itself (Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Wilson, Bienas, Mendes de Leon, Evans, & Bennett, 2003). Additionally, high neuroticism may pull individuals toward certain situations or environments that raise the risk of disease or mortality (“tropisms”; Friedman, 2000).
Perhaps the most obvious explanation of the link between extraversion and mortality involves the size and quality of social networks. Better and more extensive social networks have been associated with lower mortality (Sugisawa, Liang, & Liu, 1994), and extraverts tend to possess greater amounts of these social resources than introverts do. However, the link with mortality is less well established for extraversion than for neuroticism.
Regardless of the causal mechanisms underlying the association between these particular traits and mortality, it is usually assumed that neuroticism and extraversion are stable over time. However, like other risk factors for mortality, such as high cholesterol or high blood pressure, neuroticism and extraversion can in fact change over time (Mroczek & Spiro, 2003). With respect to LDL cholesterol or blood pressure, a decline is generally good and lowers mortality risk. We reason that a decrease in neuroticism or an increase in extraversion may have a similar desirable effect on survival. Thus, we propose that risk of mortality should be lowered among persons who show a long-term decline in neuroticism or a long-term increase in extraversion.
We tested this hypothesis in the present study. We drew upon previous research that estimated change in neuroticism and extraversion in more than 1,600 men using growth-curve modeling (Mroczek & Spiro, 2003). In that study, we found statistically significant individual differences in both the level (intercept) and the rate of change (slope) of neuroticism and of extraversion over a 12-year period. In the current study, we used those intercepts and slopes to predict time to death in a survival analysis (Cox proportional hazards).
METHOD
Sample and Mortality
The data were from 1,663 subjects in the Department of Veterans Affairs' (VA) Normative Aging Study (NAS), a longitudinal investigation of aging in men founded at the Boston VA Outpatient Clinic in 1963 (Bosse', Ekerdt, & Silbert, 1984). More than 6,000 men were screened for the absence of serious physical or mental illness between 1961 and 1970 to assemble a panel of 2,280 initially healthy subjects. In 1988, the beginning of this study, the age range was 43 to 91 (M = 63, SD = 8).
Vital status of NAS subjects is monitored by periodic mailings; death certificates are obtained and coded for cause of death. Of the 1,663 subjects on whom we had growth-curve parameters, 503 (30%) died during the 18-year period from 1988 through 2005. Of these deaths, 34% were due to cancer, 38% to circulatory disease, and 28% to other diseases or non-disease-related causes.
Measures
Neuroticism and extraversion were assessed via the EPI-Q (Floderus, 1974), a short version of the Eysenck Personality Inventory (Eysenck & Eysenck, 1968). Each EPI-Q scale consists of nine dichotomous items; scores range from 0 to 9. The internal-consistency reliabilities were .74 and .92 for neuroticism and extraversion, respectively, at baseline.
We included both subjective and objective measures of physical health. Subjective health was assessed by asking each individual to rate the state of his physical health using one of five response options: excellent, good, fair, poor, or very poor. To assess objective health, we used a modified (Bosse', Aldwin, Levenson, & Ekerdt, 1987) version of the Seriousness of Illness Rating Scale (SIRS; Wyler, Masuda, & Holmes, 1968). SIRS ratings are coded from responses to the following question: “Is there any physical condition, illness, or health problem that bothers you now?” The most serious condition each individual named was rated from 1 to 124 (life-threatening conditions, such as cancer or leukemia); an individual who indicated no problem received a score of zero. In our analyses, we used SIRS ratings and subjective health ratings from 1987 or 1988, prior to or at the initial EPI-Q assessment of neuroticism.
Depression is a well-known predictor of mortality (Barefoot et al., 1996; Williams, Barefoot, & Schneiderman, 2003), and neuroticism is a strong predictor of depression (Watson & Clark, 1994). To rule out any confounding due to depression, we used scores on the depression scale of the Symptom Check List (SCL-90; Derogatis, 1983), which were obtained in 1988 as a control variable.
Growth-Curve Modeling of Personality
The explanatory variables in this study were the intercepts and slopes that defined the 1,663 neuroticism and extraversion growth-curve trajectories described previously (Mroczek & Spiro, 2003). These growth-curve parameters were estimated using multilevel models (Raudenbush & Bryk, 2002) of up to six administrations of the EPI-Q over a 12-year period (1988-2000). Any growth-curve model requires a time variable, usually age. In our growth curves, we used age centered at 63, the grand mean of age across all occasions, and divided by 10, to convert to age change per decade.
An evaluation of the growth-curve parameters indicated that the slope variances were statistically significant, meaning that there were individual differences in rate of change (these effects were subtle, with effect sizes of 0.15 and 0.10 for neuroticism and extraversion, respectively; Mroczek & Spiro, 2003). The slopes yielded by the growth-curve models were defined so that each slope represented the predicted amount of trait change per decade. These slopes ranged from -2.55 to 2.17 (Mdn = -0.03) for neuroticism and from -1.14 to 1.22 (Mdn = -0.02) for extraversion. Negative slopes indicate decline; positive slopes indicate increase. The standard deviations for EPI-Q neuroticism and extraversion across measurement occasions were 2.25 and 2.30, respectively; thus, a slope of -1.00 represented a decrease of 44% of a standard deviation per decade for neuroticism and a decrease of 43% of a standard deviation per decade for extraversion.
Survival Analyses
To examine the influence of personality on mortality, we used survival analysis (proportional hazards modeling). We used exact date of death to calculate survival time from the first EPI-Q, completed circa 1988, the start date for this study. Our (age-adjusted) hazard-rate model is expressed as follows:
In this equation, logh(tij) is the log of individual i's risk of dying (or hazard: h) at time t. The term logh0(tj) represents the general baseline log hazard function, which is the risk of dying when all predictors are set to 0. The term β1(age1i) is the effect of age on risk of dying. The term β2(level1i) is the effect of level of neuroticism or extraversion on risk of dying; this is what prior studies have estimated. The term β3(slope3i) is the effect of change in neuroticism or extraversion on risk of dying, which prior studies have not examined.
RESULTS
Tables 1 and 2 display models for the effects of personality level and change on mortality. Models for neuroticism are in Table 1, and models for extraversion are in Table 2. There were no significant effects of extraversion level or slope (or their interaction) on mortality, so we focus our discussion on neuroticism.
TABLE 1.
Results for Four Models of the Effect of Change in Neuroticism on Mortality Over 18 Years (1988-2005)
| Hazard ratio |
||||
|---|---|---|---|---|
| Risk factor | Model 1 | Model 2 | Model 3 | Model 4 |
| Age | 1.09 (1.08-1.11)** | 1.10 (1.09-1.11)** | 1.11 (1.09-1.12)** | 1.11 (1.09-1.12)** |
| Neuroticism level | 1.09 (1.03-1.15)* | 1.00 (0.94-1.06) | 1.04 (0.97-1.11) | 0.97 (0.89-1.05) |
| Neuroticism slope | 1.40 (1.16-1.68)** | 1.74 (1.42-2.06)** | 1.67 (1.35-1.99)** | |
| Level × Slope | 0.81 (0.73-0.89)** | 0.79 (0.71-0.87)** | ||
| Self-rated health | 0.96 (0.83-1.09) | |||
| SIRS score | 1.01 (1.01-1.01) ** | |||
| Depression | 1.29 (0.99-1.68) | |||
| -2LL | 6,578 | 6,563 | 6,545 | 5,674 |
| AIC | 6,582 | 6,581 | 6,553 | 5,688 |
Note. Numbers in parentheses are 95% confidence intervals. SIRS = Seriousness of Illness Rating Scale; -2LL = -2 log likelihood; AIC = Akaike's Information Criterion.
p < .01.
p < .001.
TABLE 2.
Results for Three Models of the Effect of Change in Extraversion on Mortality Over 18 Years (1988-2005)
| Hazard ratio |
|||
|---|---|---|---|
| Risk factor | Model 1 | Model 2 | Model 3 |
| Age | 1.10 (1.09-1.12)** | 1.11 (1.09-1.12)** | 1.11 (1.09-1.12)** |
| Extraversion level | 0.99 (0.94-1.04) | 0.99 (0.94-1.04) | 0.99 (0.94-1.04) |
| Extraversion slope | 0.98 (0.74-1.31) | 0.98 (0.73-1.32) | |
| Level × Slope | 1.00 (0.83-1.20) | ||
| -2LL | 6,689 | 6,689 | 6,689 |
| AIC | 6,693 | 6,694 | 6,696 |
Note. Numbers in parentheses are 95% confidence intervals. -2LL = -2 log likelihood; AIC = Akaike's Information Criterion.
p < .001.
In Model 1 of our analysis of neuroticism, we entered age and neuroticism level. The latter was significant. This result replicates prior results showing that lower levels of neuroticism reduce mortality risk (e.g., Wilson et al., 2004). In Model 2, we added rate of change in neuroticism (slope). This risk factor was significant, with a hazard ratio of 1.40. This means that a 1-unit increase in neuroticism slope was associated with a 40% increase in risk of mortality: A subject with a slope of 1.00 was 40% more likely to die than was someone who was the same age but had a slope of 0 (i.e., a person with a completely stable level of neuroticism). Given that the standard deviation of neuroticism was 2.25, a 1-unit increase corresponds to a change of approximately half a standard deviation over a decade; thus, a change of about half a standard deviation over a decade increased the risk of dying by 40%.
In Model 3, we added the interaction between level and slope. It was significant, indicating that the effect of slope depended on level of neuroticism. In Model 4, we added the covariates (self-rated health, SIRS rating, and depression score); the interaction of level and slope remained significant. In analyses not shown in Table 1, we added main-effect and interaction terms for cause of death (coded for cancer, circulatory disease, and other) to Model 4, for those subjects who had died. The results were unchanged.
We also performed a missingness analysis for the neuroticism growth curves in Model 4. Using a technique recommended by Little (1995), we created dummies to represent the most common patterns of missing data. Five such patterns accounted for more than 80% of subjects with missing data. For example, one pattern was to have data for all neuroticism assessments but the fifth. In two others, either the fourth or the fifth assessment was missing. Adding dummy variables for the five most common missingness patterns did not change the results.
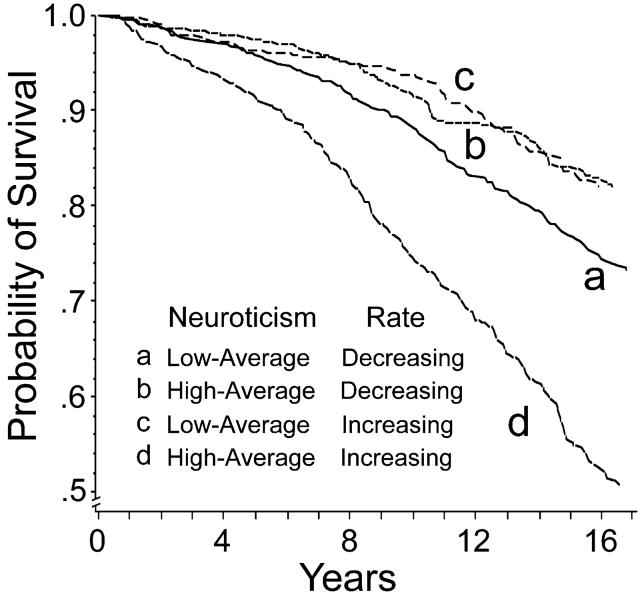
To understand the level-by-slope interaction, we created four groups by splitting each growth-curve parameter at its median. Table 3 shows the means and standard deviations of neuroticism level and slope for the four groups, along with the percentile ranks of the means. Figure 1 presents the survival curves, adjusted for age, physical health, and depression, for these groups: (a) men who had low average neuroticism and whose neuroticism decreased, (b) men who had a high average and whose neuroticism decreased, (c) men who had a low average and whose neuroticism increased, and (d) men who had a high average and an increase. It is clear from the figure that men who had high average neuroticism and whose neuroticism increased over time (curve d) had the highest mortality over the follow-up period. The other three survival curves were not significantly different from one another. Thus, the interaction obtained in the proportional hazards analysis was driven by men who had a high neuroticism intercept (mean level = 1.49) and whose level of neuroticism rose even higher (mean slope = 0.46) over the follow-up period.
TABLE 3.
Neuroticism Intercepts and Slopes for the Four Groups
| Intercept (level) |
Slope |
||||
|---|---|---|---|---|---|
| Group | N | Mean | Percentile of mean | Mean | Percentile of mean |
| High, decreasing neuroticism | 289 | 0.92 (1.00) | 73 | -0.42 (0.31) | 19 |
| High, increasing neuroticism | 541 | 1.49 (1.24) | 81 | 0.46 (0.41) | 83 |
| Low, decreasing neuroticism | 534 | -1.27 (0.55) | 25 | -0.38 (0.25) | 22 |
| Low, increasing neuroticism | 299 | -1.32 (0.64) | 23 | 0.26 (0.27) | 74 |
Note. Standard deviations are given in parentheses.
Fig. 1.
Survival curves for the four groups defined by median splits of neuroticism level and slope (with age, physical health, and depression controlled).
DISCUSSION
Prior studies have documented that amount (level) of neuroticism predicts mortality (e.g., Wilson et al., 2003). This study built on those previous investigations, finding that it is not just the level of personality traits, but also their direction of change, that is related to mortality. Men who had a high average level of neuroticism and whose neuroticism increased did not survive as long (controlling for age, physical health, and depression) as those without this combination of risk factors. Interestingly, the survival curve for the combination that should have been associated with the greatest longevity—low, decreasing neuroticism—did not differ from the curves for the other combinations (low, increasing and high, decreasing neuroticism). Thus, high neuroticism in and of itself need not place individuals at elevated risk for mortality. Mortality risk appears greatest when high neuroticism is joined with another risk factor—in this case, a long-term increase in the trait.
The question remains as to the pathways by which high, increasing neuroticism influences mortality. One potential pathway is via health behaviors. Persons with high and increasing neuroticism may assuage its effects, such as potentially elevated and chronic negative affect, by increasing their smoking or use of alcohol or other drugs (Friedman, 2000; Roberts & Bogg, 2004). Many people use tobacco, alcohol, and other drugs to help regulate negative emotions, but often at a high cost to their physical health (Roberts & Bogg, 2004). Another potential pathway is via ineffective management of stress, which may worsen physical health problems. High neuroticism that continues to increase over time may hinder people's ability to manage stress, or even to learn how to handle stress more effectively, in turn leading to undesirable health outcomes.
Our findings are also relevant to the study of personality change. It is often assumed that if personality is not stable and enduring, it loses predictive power. This is hardly the case. Again, consider cholesterol or blood pressure. These variables can and do change considerably over the life span, yet do not lose predictive power. Our findings indicate that personality traits similarly retain their forecasting power, even if they change.
Limitations
Future investigations will require broader samples. One limitation of this study is the lack of women. The NAS was founded by the VA in the 1960s, a time when women were routinely excluded not only from VA studies, but from scientific studies in general. Additionally, as the NAS sample is more than 90% Caucasian, the generalizability of our results to other ethnic groups may be limited. However, there is no theoretical or conceptual reason for expecting that women or non-Caucasians would yield a result different from the one obtained in the present study.
In addition, it is possible that high, increasing neuroticism is itself predictive of other changes that account for the raised mortality risk. Individuals with high, increasing neuroticism may experience increasing depression, anxiety, or other psychopathologies, which in turn may explain, at least partially, the lower survival documented here. Future studies might use multiple trajectories to clarify how correlated changes in two or more variables jointly influence mortality risk.
Conclusion
In recent years, personality variables have emerged as important predictors of mortality (Friedman et al., 1993; Wilson et al., 2004). The current study adds to these findings by demonstrating that in the case of neuroticism, mortality risk appears to be greatest when high levels of this trait are paired with long-term increases. The effects of a high level of neuroticism are moderated by the amount neuroticism increases in the ensuing years. Thus, high neuroticism in and of itself is not necessarily bad, but when compounded by a long-term increase in the trait, it may have serious implications for one's physical health and ultimately for how long one survives.
Acknowledgments
This study was supported by grants from the National Institute on Aging (R01-AG18436 and P01-AG020166) and by the Clinical Sciences Research and Development Service of the U.S. Department of Veterans Affairs. The VA Normative Aging Study (NAS) is supported by the Co-operative Studies Program/Epidemiology Research Information Center, U.S. Department of Veterans Affairs, and is a research component of the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC). We wish to thank Dave Almeida, Duane Alwin, John Ayanian, Paul Cleary, Chris Coe, Ken Ferraro, Karen Fingerman, Chris Fraley, Bill Graziano, Bob Krueger, Margie Lachman, Paula McKinley, Carol Ryff, Brent Roberts, Teresa Seeman, Burt Singer, and Richard Sloan for comments on earlier versions of this manuscript.
REFERENCES
- Almada SJ, Zonderman AB, Shekelle RB, Dyer AR, Daviglus ML, Costa PT, et al. Neuroticism, cynicism and risk of death in middle-aged men: The Western Electric Study. Psychosomatic Medicine. 1991;53:165–175. doi: 10.1097/00006842-199103000-00006. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Helms MJ, Mark DM, Blumenthal JA, Califf RM, Haney TL, et al. Depression and longterm mortality risk in patients with coronary artery disease. American Journal of Cardiology. 1996;78:613–617. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- Bolger N, Schilling EA. Personality and problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of Personality. 1991;59:356–386. doi: 10.1111/j.1467-6494.1991.tb00253.x. [DOI] [PubMed] [Google Scholar]
- Bosse' R, Aldwin CM, Levenson MR, Ekerdt DJ. Mental health differences among retirees and workers: Findings from the Normative Aging Study. Psychology and Aging. 1987;2:383–389. doi: 10.1037//0882-7974.2.4.383. [DOI] [PubMed] [Google Scholar]
- Bosse' R, Ekerdt D, Silbert J. The Veterans Administration Normative Aging Study. In: Mednick SA, Harway M, Finello KM, editors. Handbook of longitudinal research: Vol. 2. Teenage and adult cohorts. Praeger; New York: 1984. pp. 273–289. [Google Scholar]
- Christensen AJ, Ehlers SL, Wiebe JS, Moran PJ, Raichle K, Ferneyhough K, Lawton WJ. Patient personality and mortality: A 4-year prospective examination of chronic renal insufficiency. Health Psychology. 2002;21:315–320. doi: 10.1037//0278-6133.21.4.315. [DOI] [PubMed] [Google Scholar]
- Danner DD, Snowdon DA, Friesen WV. Positive emotions in early life and longevity: Findings from the Nun Study. Journal of Personality and Social Psychology. 2001;80:804–813. [PubMed] [Google Scholar]
- Derogatis L. SCL-90 revised manual. Johns Hopkins University School of Medicine; Baltimore: 1983. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual for the Eysenck Personality Inventory. Educational and Industrial Testing Service; San Diego, CA: 1968. [Google Scholar]
- Floderus B. Psychosocial factors in relation to coronary heart disease and associated risk factors. Nordisk Hygienisk Tidskrift. 1974;(Supplementum 6) [Google Scholar]
- Friedman HS. Long-term relations of personality and health: Dynamisms, mechanisms, tropisms. Journal of Personality. 2000;68:1089–1108. doi: 10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- Friedman HS, Tucker JS, Tomlinson-Keasey C, Schwartz JE, Wingard DL, Criqui MH. Does childhood personality predict longevity? Journal of Personality and Social Psychology. 1993;65:176–185. doi: 10.1037//0022-3514.65.1.176. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Ketelaar T. Personality and susceptibility to positive and negative emotional states. Journal of Personality and Social Psychology. 1991;61:132–140. doi: 10.1037//0022-3514.61.1.132. [DOI] [PubMed] [Google Scholar]
- Little RJA. Modeling the drop-out mechanism in longitudinal studies. Journal of the American Statistical Association. 1995;90:1112–1121. [Google Scholar]
- Maier H, Smith J. Psychological predictors of mortality in old age. Journal of Gerontology: Psychological Sciences. 1999;54B:P44–P54. doi: 10.1093/geronb/54b.1.p44. [DOI] [PubMed] [Google Scholar]
- Maruta T, Colligan RC, Malinchoc M, Offord KP. Optimists vs. pessimists: Survival rate among medical patients over a 30-year period. Mayo Clinic Proceedings. 2000;75:140–143. doi: 10.4065/75.2.140. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Almeida DM. The effects of daily stress, age, and personality on daily negative affect. Journal of Personality. 2004;72:354–378. doi: 10.1111/j.0022-3506.2004.00265.x. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A., III Modeling intraindividual change in personality traits: Findings from the Normative Aging Study. Journal of Gerontology: Psychological Sciences. 2003;58B:P153–P165. doi: 10.1093/geronb/58.3.p153. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Roberts BW, Bogg T. A longitudinal study of the relationships between conscientiousness and the social-environmental factors and substance-use behaviors that influence health. Journal of Personality. 2004;72:325–353. doi: 10.1111/j.0022-3506.2004.00264.x. [DOI] [PubMed] [Google Scholar]
- Small BJ, Hertzog C, Hultsch DF, Dixon RA. Stability and change in adult personality over 6 years: Findings from the Victoria Longitudinal Study. Journal of Gerontology: Psychological Sciences. 2003;58B:P166–P176. doi: 10.1093/geronb/58.3.p166. [DOI] [PubMed] [Google Scholar]
- Sugisawa H, Liang J, Liu X. Social networks, social support, and mortality among older people in Japan. Journal of Gerontology: Social Sciences. 1994;49B:S3–S13. doi: 10.1093/geronj/49.1.s3. [DOI] [PubMed] [Google Scholar]
- Suls J, Green P, Hillis S. Emotional reactivity to everyday problems, affective inertia, and neuroticism. Personality and Social Psychology Bulletin. 1998;24:127–136. [Google Scholar]
- Watson D, Clark LA. The vicissitudes of mood: A schematic model. In: Ekman P, Davidson RJ, editors. The nature of emotion: Fundamental questions. Oxford University Press; New York: 1994. pp. 400–405. [Google Scholar]
- Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: More than one culprit at work. Journal of the American Medical Association. 2003;290:2190–2192. doi: 10.1001/jama.290.16.2190. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Bienas JL, Mendes de Leon CF, Evans DA, Bennett DA. Negative affect and mortality in older persons. American Journal of Epidemiology. 2003;158:827–835. doi: 10.1093/aje/kwg224. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Bienas JL, Evans DA, Bennett DA. Personality and mortality in old age. Journal of Gerontology: Psychological Sciences. 2004;59B:P110–P116. doi: 10.1093/geronb/59.3.p110. [DOI] [PubMed] [Google Scholar]
- Wyler AR, Masuda M, Holmes TH. The Seriousness of Illness Rating Scale. Journal of Psychosomatic Research. 1968;11:363–374. doi: 10.1016/0022-3999(68)90033-0. [DOI] [PubMed] [Google Scholar]