Abstract
OBJECTIVE:
It is thought that emphysema patients are at a higher risk of coronary artery disease. The present study is one of very few that evaluated the prevalence of significant coronary artery disease in emphysema patients using coronary artery calcification measured by electron beam computed tomography.
METHODS:
A retrospective chart review evaluated 1720 consecutive patients, some of whom were self-referred. All patients had both heart and lungs imaged with electron beam computed tomography when they were seen at the Inner Imaging Center, a cardiac imaging center affiliated with the Beth Israel Hospital in New York, New York. Multiple logistic regression was performed to determine which factors were independently associated with coronary artery calcification.
RESULTS:
Age, sex, hypertension and smoking were the risk factors independently associated with coronary artery calcification in the population studied. The emphysema group was significantly higher on measures of smoking and hypertension compared with the control group. Comparison of scores between the two groups using different categories for coronary artery calcification scores did not show a statistically significant difference using χ2 analysis (P=0.088). However, there was a significant difference between dichotomized coronary artery calcification scores of lower than 100 and 100 or higher in patients with and without emphysema, respectively (P=0.013). Coexisting smoking and hypertension may contribute to the higher incidence of coronary artery calcfication in emphysema patients. Symptoms of chest pain and shortness of breath were not different between the emphysema and control groups.
CONCLUSION:
Emphysema patients have a higher prevalence of significant coronary artery calcification, defined as a coronary artery calcification score higher than 100.
Keywords: Calcification, Coronary, EBCT, Emphysema
Abstract
OBJECTIF :
On pense que les patients emphysémateux sont plus vulnérables à une coronaropathie. La présente étude fait partie des très rares études à évaluer la prévalence de graves coronaropathies chez les patients emphysémateux au moyen de la calcification artérielle mesurée par tomodensitométrie à faisceau d’électrons.
MÉTHODOLOGIE :
Au moyen d’une analyse rétrospective de dossiers, les auteurs ont évalué 1 720 patients consécutifs, dont certains s’étaient présentés sans recommandation. Tous les patients avaient subi une imagerie des poumons et du cœur par tomodensitométrie à faisceau d’électrons au moment de leur consultation au Inner Imaging Centre, un centre d’imagerie cardiaque affilié au Beth Israel Hospital de New York, à New York. Une régression logistique multiple a permis de déterminer les facteurs associés de manière indépendante à la calcification de l’artère coronaire.
RÉSULTATS :
L’âge, le sexe, l’hypertension et le tabagisme étaient des facteurs de risque associés de manière indépendante à la calcification de l’artère coronaire au sein de la population à l’étude. Le groupe emphysémateux obtenait des résultats beaucoup plus élevés que le groupe témoin à l’égard des mesures de tabagisme et d’hypertension. La comparaison des indices entre les deux groupes au moyen de catégories différentes d’indices de calcification de l’artère coronaire n’ont pas démontré de différence statistiquement significative au moyen de l’analyse χ2 (P=0,088). Cependant, on remarquait une différence considérable entre les indices de calcification de l’artère coronaire dichotomiques de moins de 100 ou d’au moins 100 chez les patients emphysémateux et non emphysémateux, respectivement (P=0,013). La coexistence du tabagisme et de l’hypertension peut contribuer à l’incidence accrue de calcification de l’artère coronaire chez les patients emphysémateux. Les symptômes de douleur thoracique et d’essoufflement ne différaient pas entre le groupe de patients emphysémateux et le groupe témoin.
CONCLUSION :
Les patients emphysémateux avaient une prévalence plus élevée de calcification importante de l’artère coronaire, définie par un indice de calcification de l’artère coronaire supérieur à 100.
It is thought that emphysema patients are at a higher risk of coronary artery disease (CAD).
The present study is one of very few that evaluated the prevalence of significant CAD in emphysema patients using coronary artery calcification (CAC) measured by electron beam computed tomography (EBCT). Emphysema was diagnosed by a lung scan using EBCT.
METHODS
Study population
The present study is a review of 1720 consecutive patients’ charts (629 women, 1091 men) seen at the Inner Imaging Cardiac Imaging Center in New York, New York. Institutional review board approval was obtained before starting the study. All patients who had both lung and heart scans using EBCT between January 2001 and January 2005 were included.
Patients completed a questionnaire before the scans, detailing their cardiovascular risk factors. Patients indicated the presence or absence of a history of hypertension (treated or untreated), diabetes mellitus, current or past smoking, obesity (weight more than 20% over ideal body weight) and a first-degree family history of CAD.
EBCT
EBCT is an accessible, accurate and noninvasive test for the detection of preclinical CAD. EBCT can rapidly and noninvasively detect and quantify calcified atherosclerotic plaque in the coronary arteries. A higher quantity of coronary artery calcium is associated with the likelihood of obstructive lesions by angiography.
CAC is also associated with an increased risk of future cardiovascular disease (CVD) in middle-aged populations (1–4).
EBCT was performed with an Imatron C-150 scanner (Imatron Inc, USA).
Heart images were obtained using a 40 to 50 slice (3 mm thickness) protocol with image acquisition gated to 70% to 80% of the electrocardiographic RR interval. Exposure time was 0.1 s per image and the radiation dose was 50 mrem. Scans with at least four contiguous pixels greater than 130 HU were considered to be positive for CAC.
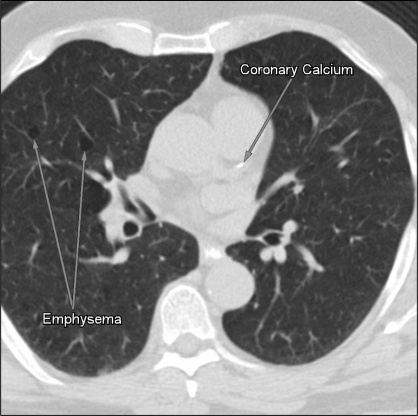
One radiologist, who was blinded to the questionnaire, determined the presence of emphysema based on typical bilateral bullous changes on the lung scan. CAC scores were determined using the Agatston scoring method (5). Lung images were obtained using a 120 contiguous slice (5 mm thickness) protocol, with an exposure time of 0.1 s per image and radiation dose of 150 mrem. One experienced radiologist interpreted all scans (Figure 1).
Figure 1).
Electron beam computed tomography showing bullous changes and coronary calcification, indicating emphysema, in one patient
Statistical analysis
Summary statistics were generated for all variables (Table 1). All predictor variables were compared between the emphysema and control groups using t tests for continuous variables and χ2 tests for categorical variables.
TABLE 1.
Demographic characteristics of patients with cardiovascular risk factors and symptoms
| Variable | Emphysema group (n=78) | Control group (n=1642) | P |
|---|---|---|---|
| Age, years (mean ± SD) | 54.2±10.5 | 53.1±10.6 | 0.469 |
| Sex, n (%) | 0.414 | ||
| Male | 47 (60.3) | 1044 (63.6) | |
| Female | 31 (39.7) | 598 (36.4) | |
| Ethnicity, n (%) | 0.652 | ||
| Caucasian | 68 (87.2) | 1406 (85.6) | |
| African-American | 2 (2.6) | 79 (4.8) | |
| Other | 8 (10.3) | 157 (9.6) | |
| Diabetes, n (%) | 0.639 | ||
| Yes | 3 (3.8) | 48 (2.9) | |
| No | 75 (96.2) | 1594 (97.1) | |
| Hypertension, n (%) | 0.033 | ||
| Yes | 20 (25.6) | 269 (16.4) | |
| No | 58 (74.4) | 1373 (83.6) | |
| Smoking, n (%) | <0.001 | ||
| Yes | 74 (94.9) | 428 (26.1) | |
| No | 4 (5.1) | 1214 (73.9) | |
| BMI*, kg/m2 (mean ± SD) | 26.9±4.8 | 26.9±4.8 | 0.134 |
| Family history of cardiovascular disease, n (%) | |||
| Reported by parents | 0.129 | ||
| Yes | 15 (19.2) | 217 (13.2) | |
| No | 63 (80.8) | 1425 (86.8) | |
| Reported by siblings | 0.664 | ||
| Yes | 3 (3.8) | 49 (3.0) | |
| No | 75 (96.2) | 1593 (97.0) | |
| Chest pain, n (%) | 0.643 | ||
| Yes | 12 (15.4) | 286 (17.4) | |
| No | 66 (84.6) | 1356 (82.6) | |
| Shortness of breath, n(%) | 0.12 | ||
| Yes | 15 (19.2) | 215 (13.1) | |
| No | 63 (80.8) | 1427 (86.9) | |
n=1376 in the control group. BMI Body mass index
Multiple logistic regression was performed to determine which factors were independently associated with CAC.
RESULTS
Approximately 5% of patients (78 of 1720) had significant emphysema, characterized by typical bilateral bullous changes on the lung scan. Demographic characteristics and CVD risk factors of patients are shown in Table 1.
Forty-five per cent of patients (763 of 1720) exhibited CAC. Fifty per cent of patients (39 of 78) with emphysema were positive for CAC.
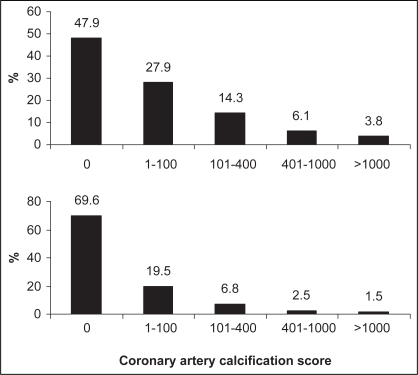
There was a significant difference between sex and the polychotomized CAC scores (P<0.0001) (Figure 2).
Figure 2).
Distribution of coronary artery calcification scores in men (top) and women (bottom)
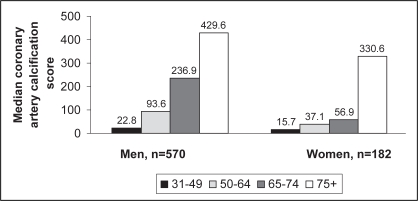
In patients with CAC, age across groups significantly differed with sex (P<0.0001) (Figure 3).
Figure 3).
Median coronary artery calcification scores in men and women by age group
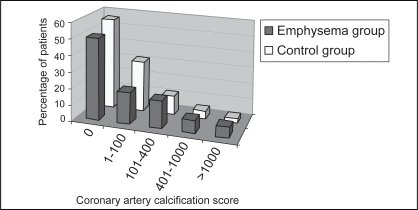
Comparison of CAC scores between the two groups using different categories for CAC scores did not show statistically significant difference using χ2 analysis (P=0.088) (Table 2, Figure 4).
TABLE 2.
Comparison of coronary artery calcification (CAC) scores between groups using different cut-offs
| CAC score | Emphysema group (n=78), n (%) | Control group (n=1642), n (%) | Overall P* |
|---|---|---|---|
| 0 | 39 (50) | 919 (56) | 0.088 |
| 1–100 | 15 (19) | 413 (25) | |
| 101–400 | 13 (17) | 188 (11) | |
| 401–1000 | 6 (8) | 77 (5) | |
| >1000 | 5 (6) | 45 (3) |
P determined using χ2
Figure 4).
Comparison of coronary artery calcification scores between emphysema and control groups
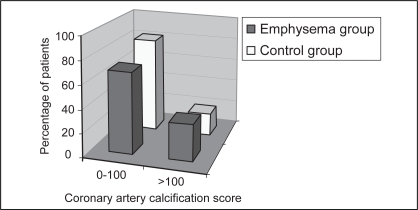
The aim of the present study was to determine the difference between the group with emphysema and the group without emphysema using dichotomized scores with a cut-off value of 100, believed to indicate clinically significant disease (6–7). It was found that 19% of patients (310 of 1642) without emphysema had CAC scores of 100 or higher compared with 31% of patients (24 of 78) with emphysema. This difference was statistically significant (P=0.013) (Figure 5).
Figure 5).
Comparison of coronary artery calcification scores between emphysema and control groups using 100 as the cut-off
Logistic regression analysis using the backward limitation-of-risks method showed that age, sex, hypertension and smoking significantly and independently contributed to CAC (Table 3).
TABLE 3.
Multiple logistic regression: factors independently associated with coronary artery calcification
| Variable included | β (SE) | 95% CI for exp b
|
||
|---|---|---|---|---|
| Lower | Exp b | Upper | ||
| Constant | −3.812 (0.329)* | – | 0.022 | – |
| Age | 0.096 (0.006)* | 1.087 | 1.101 | 1.115 |
| Sex (male†) | −1.527 (0.132)* | 0.168 | 0.217 | 0.282 |
| Hypertension (yes†) | −0.572 (0.153)* | 1.312 | 1.772 | 2.394 |
| Smoking | 1.051 (0.120)* | 2.261 | 2.861 | 3.619 |
R2=0.346 (Nagelkerke), model χ2 (4)=505.56;
P<0.0001.
Reference variables. exp b Exponential of regression coefficient (b)
DISCUSSION
One of the most commonly encountered comorbidities in emphysema patients is CAD. The direct relationship between chronic lung disease such as emphysema and the incidence of CVD has been known for many years (8–12).
The studies that assessed the prevalence of CAD in this population of patients were limited, and very few used CAC as a marker for atherosclerosis.
Using CAC, Newman et al (11) demonstrated that emphysema, among other variables, including age, sex, race, clinical CVD, triglyceride level and pack-years of smoking were independently associated with CAC scores in the highest quartile (defined as a CAC score higher than 918) compared with the other lower quartiles.
We used EBCT as a precise tool to diagnose emphysema, which has not been used before. We also aimed to explore the association between CAC and emphysema using different standard categories and then a cut-off of 100, which is known to imply some degree of significant CAD.
We found that emphysema was associated with a higher incidence of significant CAD, defined as a CAC score of 100 or higher; however, we did not elucidate an independent association.
The multivariable regression analysis showed age, sex, hypertension and smoking as independent risk factors for CAC; therefore, we assumed this association with higher scores to be secondary to more smoking and hypertension in the emphysema group. However, other factors cannot be excluded based on this analysis.
Our results confirm the conclusions of other studies that examined the effects of emphysema on different end points diagnosed by other modalities, such as electrocardiogram, angiography, as well as clinical cardiac events, including mortality (8–10).
Sin and Man (8) analyzed data from participants 50 years of age and older (n=6629) in the Third National Health and Nutrition Examination Survey. Chronic obstructive pulmonary disease was found to be associated with electrocardiogram evidence of ischemic heart disease, as assessed by the cardiac infarction injury score.
Using cardiac angiography, Thurnheer et al (9) found a high prevalence of CAD among advanced emphysema patients before lung reduction surgery: 15% of patients (6 of 41) were found to have significant CAD.
Engström et al (10) studied cardiovascular mortality and incidence of myocardial infarction over a mean follow-up of 18.4 years. They determined that chronic obstructive pulmonary disease was associated with an increased incidence of myocardial infarction and cardiovascular mortality.
Our study revealed no significant difference in symptoms of chest pain and shortness of breath between groups. Although the present study was susceptible to some degree of inaccurate data, like any other questionnaire-based study, it still emphasizes the difficulty encountered when screening for CAD in emphysema patients using symptoms alone.
Although our study has the limitations of a retrospective screening nature, lack of accurate quantification of smoking exposure, lack of pulmonary function testing, as well as the use of oximetry, we believe it contributes valuable information to the concept of CAD in emphysema patients, which merits further studies.
REFERENCES
- 1.Rumberger JA, Sheedy PF, II, Breen JF, Fitzpatrick LA, Schwartz RS. Electron beam computed tomography and coronary artery disease: Scanning for coronary artery calcification. Mayo Clin Proc. 1996;71:369–77. doi: 10.4065/71.4.369. [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Georgiou D, Brody A, et al. Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: A multicenter study. Circulation. 1996;93:898–904. doi: 10.1161/01.cir.93.5.898. [DOI] [PubMed] [Google Scholar]
- 3.O’Rourke RA, Brundage BH, Froelicher VF, et al. American College of Cardiology/American Heart Association Expert Consensus Document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. J Am Coll Cardiol. 2000;36:326–40. doi: 10.1016/s0735-1097(00)00831-7. [DOI] [PubMed] [Google Scholar]
- 4.Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–60. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 5.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 6.Keelan PC, Bielak LF, Ashai K, et al. Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation. 2001;104:412–7. doi: 10.1161/hc2901.093112. [DOI] [PubMed] [Google Scholar]
- 7.Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112:572–7. doi: 10.1161/CIRCULATIONAHA.104.488916. [DOI] [PubMed] [Google Scholar]
- 8.Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107:1514–9. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 9.Thurnheer R, Muntwyler J, Stammberger U, et al. Coronary artery disease in patients undergoing lung volume reduction surgery for emphysema. Chest. 1997;112:122–8. doi: 10.1378/chest.112.1.122. [DOI] [PubMed] [Google Scholar]
- 10.Engström G, Lind P, Hedblad B, et al. Lung function and cardiovascular risk: Relationship with inflammation-sensitive plasma proteins. Circulation. 2002;106:2555–60. doi: 10.1161/01.cir.0000037220.00065.0d. [DOI] [PubMed] [Google Scholar]
- 11.Newman AB, Naydeck BL, Sutton-Tyrrell K, Feldman A, Edmundowicz D, Kuller LH. Coronary artery calcification in older adults to age 99: Prevalence and risk factors. Circulation. 2001;104:2679–84. doi: 10.1161/hc4601.099464. [DOI] [PubMed] [Google Scholar]
- 12.Tockman MS, Pearson JD, Fleg JL, et al. Rapid decline in FEV1. A new risk factor for coronary heart disease mortality. Am J Respir Crit Care Med. 1995;151:390–8. doi: 10.1164/ajrccm.151.2.7842197. [DOI] [PubMed] [Google Scholar]