Abstract
A patient presented with acute ST segment elevation myocardial infarction following cocaine abuse. He was transferred for primary angioplasty. The emergent coronary angiography revealed acute left main coronary artery occlusion. Recanalization with balloon angioplasty was performed, followed by thrombectomy and stenting of the left main coronary artery with a paclitaxel-eluting stent. The patient recovered with a left ventricular ejection fraction of 35% at discharge. The pathophysiology of cocaine-induced myocardial infarction includes vasospasm, thrombosis and increased myocardial oxygen demand. Primary percutaneous coronary intervention allows local delivery of vasodilators and mechanical reperfusion in a timely manner. The authors argue that it is the best option for cocaine-induced ST segment elevation myocardial infarction. Recent data from randomized trials comparing bare metal and drug-eluting stents for primary percutaneous coronary intervention are discussed, as is the lack of evidence supporting the use of thrombectomy devices in acute myocardial infarction. The authors believe that primary percutaneous coronary intervention should be considered early for a patient presenting with cocaine-induced ST segment elevation myocardial infarction.
Keywords: Angiography, Angioplasty, Cocaine, Drug-eluting stent, Myocardial infarction, Stents
Abstract
Un patient s’est présenté avec un infarctus du myocarde avec élévation aiguë du segment ST après la consommation de cocaïne. Il a été transféré en angioplastie primaire. L’angiographie coronaire émergente a révélé une occlusion aiguë de la principale artère coronaire gauche. Les médecins ont procédé à une recanalisation par angioplastie par ballonnet, suivie d’une thrombectomie et de l’installation d’une endoprothèse à élution de paclitaxel dans la principale artère coronaire gauche. Le patient s’est rétabli, avec une fraction d’éjection ventriculaire de 35 % au congé. La physiopathologie de l’infarctus du myocarde induite par l’utilisation de cocaïne inclut des spasmes vasculaires, une thrombose et une augmentation des besoins myocardiques en oxygène. L’intervention coronaire percutanée primaire permet la libération locale de vasodilatateurs et une reperfusion mécanique rapides. Les auteurs postulent qu’il s’agit de la meilleure solution en cas d’infarctus du myocarde induit par l’utilisation de cocaïne. Ils exposent les récentes données tirées d’essais aléatoires comparant les endoprothèses à métal nu aux endoprothèses à élution de médicament en cas d’intervention coronaire percutanée primaire, ainsi que le manque de données probantes en appui à l’utilisation d’instruments de thrombectomie en cas d’infarctus aigu du myocarde. Les auteurs sont d’avis qu’il faudrait envisager rapidement une intervention coronaire percutanée primaire chez un patient qui se présente avec un infarctus du myocarde avec élévation du segment ST induit par la cocaïne.
The present paper describes the case and management of a cocaine user with an occlusion of the left main coronary artery (LMCA) presenting with ST segment elevation myocardial infarction. To our knowledge, this is the second reported case of LMCA occlusion due to cocaine abuse (1) and the first to be associated with a favourable outcome. Acute LMCA stenting using a drug-eluting stent has been reported (2), although not in the context of cocaine abuse. Data show that primary percutaneous coronary intervention (PCI) in acute LMCA occlusion is feasible. Neri et al (3) reported a 91% initial success rate in patients who, for the most part, presented with cardiogenic shock. However, in-hospital (50%) and six-month (59%) mortality remained very high, as did angiographic restenosis (40%).
CASE PRESENTATION
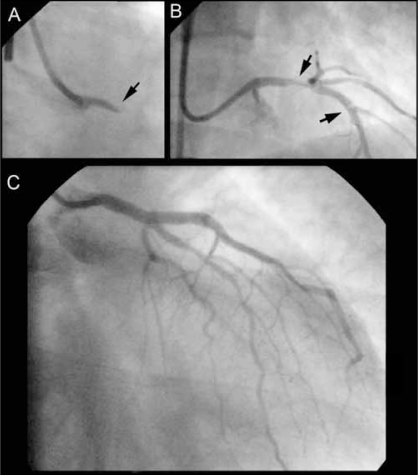
A 42-year-old man proceeded to a nearby community hospital after experiencing several hours of chest pain following heavy cocaine use. His electrocardiogram at admission showed diffuse ST segment depression. Despite administration of nitroglycerine and heparin, subsequent electrocardiograms showed anterolateral ST segment elevation. He was transferred to the Centre Hospitalier de l’Université de Montreal (Montreal, Quebec) for primary PCI approximately 6 h after the onset of symptoms. He received intravenous eptifibatide and a loading dose of clopidogrel before arrival in the catheterization laboratory. Emergent coronary angiography revealed acute LMCA occlusion (Figure 1A). The patient quickly became hypotensive. Vasopressors were started and an intra-aortic balloon pump was inserted. Balloon angioplasty was performed, restoring Thrombolysis In Myocardial Infarction (TIMI) grade 2 flow in the left coronary artery and revealing a severe plaque burden at the distal bifurcation of the LMCA (Figure 1B) with a distal embolized thrombus and residual vasospasm. Thrombectomy was achieved with an aspiration catheter (Export; Medtronic, USA). A 4.5 mm × 20 mm paclitaxel-eluting stent (TAXUS; Boston Scientific, USA) was deployed in the LMCA across the circumflex artery. TIMI grade 3 flow was shown to be restored in the left coronary artery on final angiography (Figure 1C). Endotracheal intubation was required during the procedure. His stay in the coronary care unit was complicated by nosocomial pneumonia. At discharge, he had a left ventricular ejection fraction of 35%. Two months later, he was referred for repeat angiography because of recurrent atypical chest pain. This examination revealed a widely patent LMCA stent with TIMI 3 flow. The ostium of the circumflex artery was not compromised. No other lesions could be visualized in his left or right coronary artery systems.
Figure 1).
Left coronary artery angiogram showing left main coronary artery (LMCA) occlusion (arrow in A). After balloon angioplasty, Thrombolysis In Myocardial Infarction (TIMI) grade 2 flow was restored in the left coronary artery, revealing a severe plaque at the distal bifurcation of the LMCA (top arrow in B) with a distal embolized thrombus (bottom arrow in B). C Final angiography after LMCA stenting with TIMI grade 3 flow in the left coronary artery
DISCUSSION
According to the American College of Cardiology and American Heart Association guidelines for ST segment elevation myocardial infarction management published in 2004 (4), LMCA occlusion with shock is a class IA indication for acute surgical reperfusion. However, necessary logistics for surgery introduce considerable time delays. Primary PCI with stenting offers rapid reperfusion, but it is limited by subacute stent thrombosis and late in-stent restenosis. The first report (2) of LMCA PCI in acute myocardial infarction suggested that it be used for prompt reperfusion in patients awaiting definitive revascularization with coronary artery bypass graft surgery. Bush et al (2) reported the first use of a sirolimus-eluting stent for definitive revascularization following LMCA occlusion. Of the recent randomized controlled trials of drug-eluting stents in primary PCI, only one (5) included LMCA lesions and lesions with thrombus. This study found no difference between paclitaxel-eluting stents and bare metal stents for target vessel revascularization, recurrent myocardial infarction or death (5).
In the present case, cocaine was presumed to be instrumental in provoking the acute myocardial infarction, although there was a significant amount of underlying atherosclerotic plaque. Cocaine causes myocardial ischemia by increasing myocardial oxygen demand. It also causes coronary vasoconstriction, and accelerated atherosclerosis and thrombosis. Treatment success depends on which mechanism is predominant. Fibrinolysis is likely to work if a thrombus has formed, but vasodilators and, ultimately, angioplasty are most useful if spasm is predominant, especially in the presence of an underlying significant plaque. Our patient had diffuse spasm that was resolved with intra-coronary nitroglycerine, a thrombus that was aspirated and a plaque in the LMCA that had ruptured. This combination accounts for the dramatic course of events and was illustrated in a case presented by Pavón-Jiménez et al (1). Primary PCI is the only modality that can address both spasm and coronary thrombosis in a timely manner. Moreover, it allows local delivery of vasodilators when systemic administration is limited by the shock state, which occurs in many patients. We believe that this accounts for the successful short-term outcome in our patient and that it presents a strong argument for primary PCI over fibrinolysis in cocaine-induced myocardial infarction.
A paclitaxel-eluting stent was chosen to reduce the risk of restenosis because of the critical location of the occlusion. In recent trials, there were no increases of stent thrombosis in acute myocardial infarction patients treated with drug-eluting stents compared with bare metal stents (4). However, the choice of the best stent for primary PCI and PCI of the LMCA remains a matter of debate; the alleged benefit of drug-eluting stents over bare metal stents has been challenged (6). Concerns have been raised about the occurrence of late stent thrombosis with drug-eluting stents, which may offset their benefit of reducing restenosis. Stent thrombosis in the LMCA is a dramatic complication, while restenosis is less likely in a vessel larger than 4 mm and is usually not life-threatening. Hence, a word of caution is appropriate with regard to the presumed advantage of drug-eluting stents over bare metal stents for LMCA stenting, especially in a drug user. The bare metal stent may have a better long-term safety profile if, for example, a patient does not optimally adhere to the dual antiplatelet therapy or if those medications need to be stopped.
Finally, we elected to use thrombectomy with an aspiration catheter (Export; Medtronic, USA) based on visual assessment that a thrombus was present in the LMCA. Angiographic criteria for the use of a thrombectomy device are scarce, with the decision left to the experience of the operator. To our knowledge, outcomes of aspiration thrombectomy with the Export catheter in acute myocardial infarction have not been published yet. Subgroups of patients who would benefit from the use of this device should be identified in appropriate trials.
CONCLUSION
We have presented the first successful primary PCI with a drug-eluting stent for anterior myocardial infarction caused by LMCA occlusion secondary to cocaine use. Several characteristics in this case made transfer from a community hospital to our centre for primary PCI the ideal treatment. First, the patient went into shock shortly after convincing electrocardiographic evidence of acute anterior ST segment elevation myocardial infarction. Second, once LMCA occlusion was identified, additional delays would have been expected if an acute surgical revascularization procedure had been chosen. Third, the response to fibrinolysis might have been incomplete because of the angiographic findings of significant plaque, thrombosis and spasm caused by cocaine use.
The present case illustrates the rapid evolution from a cocaine-induced non-ST segment elevation acute coronary syndrome to a life-threatening ST segment elevation myocardial infarction. Cocaine creates a milieu that is particularly favourable to thrombosis, and only PCI can address all the components of the coronary occlusion. Hence, if available within acceptable delays, strong consideration should be given to PCI over thrombolysis in cocaine-induced myocardial infarction.
REFERENCES
- 1.Pavón-Jiménez R, García-Rubira JC, Calderón-Leal J. Total occlusion of the left main coronary artery in a young cocaine user. Int J Cardiol. 1999;70:87–90. doi: 10.1016/s0167-5273(99)00050-9. [DOI] [PubMed] [Google Scholar]
- 2.Bush HS, Strong DE, Novaro GM. Successful use of sirolimus-eluting stents for treatment of ST-elevation acute myocardial infarction caused by left main coronary artery occlusion. Tex Heart Inst J. 2005;32:421–3. [PMC free article] [PubMed] [Google Scholar]
- 3.Neri R, Migliorini A, Moschi G, Valenti R, Dovellini EV, Antoniucci D. Percutaneous reperfusion of left main coronary disease complicated by acute myocardial infarction. Catheter Cardiovasc Interv. 2002;56:31–4. doi: 10.1002/ccd.10168. [DOI] [PubMed] [Google Scholar]
- 4.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Laarman GJ, Suttorp MJ, Dirksen MT, et al. Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention. N Engl J Med. 2006;355:1105–13. doi: 10.1056/NEJMoa062598. [DOI] [PubMed] [Google Scholar]
- 6.Tung R, Kaul S, Diamond GA, Shah PK. Narrative review: Drug-eluting stents for the management of restenosis: A critical appraisal of the evidence. Ann Intern Med. 2006;144:913–9. doi: 10.7326/0003-4819-144-12-200606200-00009. [DOI] [PubMed] [Google Scholar]