Abstract
Behçet’s disease is an autoimmune, multisystem disease presenting with recurrent oral and genital ulceration as well as ocular involvement. Aneurysmal degeneration of coronary arteries remains a rare phenomenon in Behçet’s disease. The case of a patient with Behçet’s disease who presented with severe stenosis of the left anterior descending artery associated with a giant aneurysm of the proximal segment is described. Surgical revascularization was proposed, followed by percutaneous embolization of the aneurysm.
Keywords: Behçet’s disease, Coronary aneurysm management, Interventional cardiology
Abstract
La maladie de Behçet est une maladie auto-immune multisystémique qui se présente avec une ulcération orale et génitale récurrente et une atteinte oculaire. La dégénérescence anévrysmale des artères coronaires demeure un rare phénomène dans cette maladie. Est décrit le cas d’un patient atteint de la maladie de Behçet qui a consulté en raison d’une grave sténose de l’artère descendante antérieure gauche associée à un anévrysme géant du segment proximal. La revascularisation chirurgicale a été proposée, suivie d’une embolisation percutanée de l’anévrysme.
Vascular lesions of Behçet’s disease generally affect both arteries and veins, with coronary involvement remaining a rare complication. Arterial involvement occurs infrequently and presents with aortitis or peripheral arterial aneurysm. We present the case of a giant aneurysm of the left anterior descending (LAD) artery in a patient with Behçet’s disease. Its management was unconventional and consisted of surgical revascularization followed by an endovascular procedure.
CASE PRESENTATION
A 29-year-old man suffering from Behçet’s disease (diagnosed seven years earlier) was hospitalized in the University Hospital of Grenoble (France) intensive care unit for unstable angina, which had commenced four days previously. The initial electrocardiogram showed sinus rhythm with ST segment depression and negative giant T waves in the anterior leads. Troponin increased to 0.34 μg/L. Echocardiography revealed a global decrease in left ventricular function, with an ejection fraction of 50% and anterior akinesis. The coronary angiography (Figure 1) showed a voluminous and partially thrombosed aneurysm of the proximal segment of the LAD (diameter 25 mm × 23 mm), preocclusive stenosis of the middle segment of the LAD and stenosis of the diagonal artery, and low flow in the distal LAD, with slightly impaired left ventricular function of the anterior wall. The severity of the unstable angina led to urgent surgical revascularization. Because percutaneous transfemoral coronary angioplasty would have been hazardous in the present case due to the length of the aneurysm and the high risk of distal embolization, the patient was referred for emergency coronary artery bypass. Surgery was performed via a middle sternotomy using standard cardiopulmonary bypass. No pericardial adherences were encountered. The aneurysm was easily seen through the myocardium, but the superior collar was not isolated. It was connected to the LAD and the diagonal artery, and to several septal arteries; direct access with exclusion of the aneurysm by suture of coronaries and collaterals seemed to be technically risky. The left internal thoracic artery was sutured sequentially to the diagonal artery and to the LAD. The postoperative course was uneventful. The follow-up computed tomography scan and the coronary angiography performed two months later showed permeability of the sequential graft and the persistence of an incomplete thrombosis inside the aneurysm (Figure 2). The coronary angiography confirmed the excellent patency of the graft, and the normal kinetics of the left ventricular anterior wall. The aneurysm was embolized with coils (Boston Scientific/Target, USA; 3 mm × 6 mm), providing a good angiographic result with angiographic exclusion of the aneurysm (Figure 3). The one-year follow-up computed tomography scan showed complete occlusion of the aneurysm. At his 30-month follow-up examination, the patient was doing well and was clinically asymptomatic.
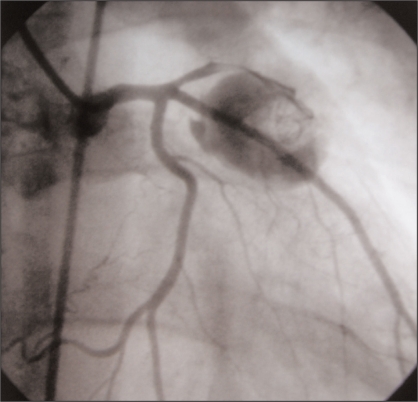
Figure 1).
Coronary angiogram showing a giant aneurysm of the left anterior descending artery. The aneurysm is partially thrombosed and the distal arteries are small
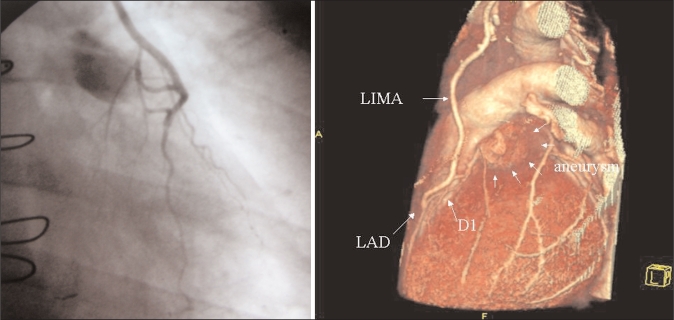
Figure 2).
Left Postoperative angiogram showing the coronary artery bypass and the aneurysm. Right Computed tomography scan reconstruction showing the aneurysm located in the left anterior descending (LAD) artery and the coronary artery bypass graft. D1 First diagonal branch; LIMA Left internal mammary artery
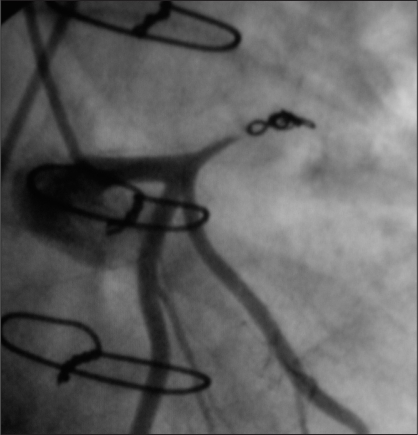
Figure 3).
Final result, after transfemoral embolization of the aneurysm
DISCUSSION
Behçet’s disease is an autoimmune, multisystem disease involving arteries and veins (1). Arterial involvement is more frequent, presenting with peripheral arterial aneurysm, aortitis or thrombosis. Aneurysmal degeneration of the coronary arteries is rare, occurring in approximately 0.5% of cases (2). Surgical treatment remains reserved for critical vascular lesions because of the high risk of anastomotic complications (3). To limit this risk, endovascular therapy is employed (4) and the stenting of coronary stenosis in Behçet’s disease has been described (5). Surgery has been performed when restenosis occurred or in the case of a very severe lesion. To our knowledge, the present case of a combined endovascular and surgical approach for the management of a coronary artery aneurysm is the first to be published. Because local anatomical conditions were not favourable for direct access to the aneurysm and knowing the risk of anastomotic complications in such patients, we preferred not to open the aneurysm wall. Spontaneous thrombosis could have been a possible complication because of the slow blood flow inside the aneurysm and the presence of mural thrombi, with a relatively low risk of distal emboli due to distal coronary artery bypass flow. Second, keeping in mind the possibility of interventional cardiology, we decided to use a secondary endovascular coil occlusion. This combined approach may occasionally be used to minimize the surgical aggression during the management of such life-threatening lesions when local anatomical conditions are not favourable.
REFERENCES
- 1.James DG, Thomson A. Recognition of the diverse cardiovascular manifestation in Behçet’s disease. Am Heart J. 1982;103:457–8. doi: 10.1016/0002-8703(82)90298-8. [DOI] [PubMed] [Google Scholar]
- 2.Ozeren M, Dogan OV, Dogan S, Yucel E. True and pseudo aneurysms of coronary arteries in a patient with Behçet’s disease. Eur J Cardiothorac Surg. 2004;25:465–7. doi: 10.1016/j.ejcts.2003.11.040. [DOI] [PubMed] [Google Scholar]
- 3.Schneider F, Gouny P, Van Laere O, Duedal V, Nussaume O. Vascular complications after surgical repair of aneurysms in Behçet’s disease. J Cardiovasc Surg (Torino) 2002;43:501–5. [PubMed] [Google Scholar]
- 4.Silistreli E, Karabay O, Erdal C, et al. Behçet’s disease: Treatment of popliteal pseudoaneurysm by an endovascular stent graft implantation. Ann Vasc Surg. 2004;18:118–20. doi: 10.1007/s10016-003-0107-x. [DOI] [PubMed] [Google Scholar]
- 5.Putini RL, Natale E, Di Marcotullio G, De Felice F, Vajola SF. Acute coronary syndrome and late stent failure in a patient with Behçet’s syndrome. Ital Heart J. 2003;4:281–4. [PubMed] [Google Scholar]