Abstract
BACKGROUND:
Disadvantaged inner-city populations have significantly higher cardiovascular disease (CVD) mortality rates than the general population. Whether a deficiency in the level of awareness, a prerequisite for change, exists that contributes to this socioeconomic divide has not been well established.
OBJECTIVES:
To address CVD risk by assessing the knowledge of CVD risk factors of an inner-city population and comparing it with that of the general population by establishing determinants of CVD knowledge and identifying potential barriers to CVD risk factor reduction in the inner city.
METHODS:
Cross-sectional survey of 136 consecutive patients 40 years of age and older attending an inner-city community health centre. The comparison group consisted of 807 age-matched respondents from the Canadian Heart Health Study, a random sample survey of the general adult Canadian population. Outcome measures included CVD risk factor knowledge, CVD risk factor prevalence and barriers to reducing CVD risk.
RESULTS:
There was no significant difference between inner-city respondent ability to name five of the seven CVD risk factors compared with the general population. Two CVD risk factors were more readily recalled by the inner-city group (lack of exercise, P<0.001; heredity, P=0.003). The average number of risk factors named by an individual from the inner city was significantly higher than the general population (3.1 versus 2.6; P<0.001). Among the inner-city respondents, socioeconomic factors, including higher education level (OR 5.224; P<0.001) and being married (OR 3.651; P=0.008), were independently related to good CVD knowledge; high CVD risk was not related. Lack of motivation (57%), lack of time (34%) and lack of money (30%) were commonly reported as barriers to addressing CVD risk.
CONCLUSIONS:
Elevated CVD risk in the inner city may not be attributable to a deficiency in the level of awareness. However, the relationship between socioeconomic status and knowledge is maintained within the lowest social class tier. The identification of barriers linked to inner-city life has implications for prevention of CVD in the inner city; results suggest that interventions that combine health education with motivational approaches, while necessary, may not be sufficient.
Keywords: Cardiovascular disease risk factors, Coronary artery disease, Health promotion, Population health, Socioeconomic factors
Abstract
HISTORIQUE :
Les populations urbaines défavorisées affichent des taux de mortalité secondaires aux maladies cardiovasculaires (MCV) considérablement supérieures à ceux de la population générale. Il n’est pas établi si c’est à cause d’un manque de sensibilisation, mais il existe une condition préalable au changement qui contribue à cet écart socioéconomique.
OBJECTIFS :
Traiter du risque de MCV en évaluant les connaissances des facteurs de risque de MCV d’une population urbaine défavorisée et le comparer à celui de la population générale en établissant les déterminants des connaissances de MCV et repérer les obstacles possibles à la réduction des facteurs de risque de MCV au sein d’un milieu urbain défavorisé.
MÉTHODOLOGIE :
Les auteurs ont mené une enquête transversale de 136 patients consécutifs de 40 ans et plus fréquentant un centre de santé communautaire d’un milieu urbain défavorisé. Le groupe de comparaison se composait de 807 répondants appariés par l’âge tirés de la Canadian Heart Health Study, une enquête auprès d’un échantillon aléatoire de la population générale d’adultes canadiens. Les mesures d’issue incluaient les connaissances des facteurs de risque de MCV, la prévalence des facteurs de risque de MCV et les obstacles à la diminution du risque de MCV.
RÉSULTATS :
Il n’existait pas de différence significative entre la capacité des répondants du milieu urbain défavorisé à nommer cinq des sept facteurs de risque de MCV et celles de la population générale. Le groupe du milieu urbain défavorisé se rappelait plus rapidement deux facteurs de risque de MCV (manque d’exercice, P<0,001, hérédité, P=0,003). Le nombre moyen de facteurs de risque nommés par une personne d’un milieu urbain défavorisé était sensiblement plus élevé qu’au sein de la population générale (3,1 par rapport à 2,6; P<0,001). Parmi les répondants du milieu urbain défavorisé, des facteurs socioéconomiques, y compris un niveau d’instruction plus élevé (RRR 5,224; P<0,001) et le fait d’être marié (RRR 3,651; P=0,008), étaient indépendamment reliés à de bonnes connaissances des MCV; le risque élevé de MCV n’était pas relié. L’absence de motivation (57 %), le manque de temps (34 %) et le manque d’argent (30 %) étaient souvent invoqués comme des obstacles à tenir compte du risque de MCV.
CONCLUSIONS :
Le risque de MCV élevé au sein des milieux urbains défavorisés n’est peut-être pas attribuable à un manque de sensibilisation. Cependant, le lien entre le statut socioéconomique et les connaissances demeure au sein de l’échelon social le plus bas. Le dépistage des obstacles reliés à la vie dans les milieux urbains défavorisés a des répercussions sur la prévention des MCV dans ces milieux. Les résultats laissent supposer que les interventions qui allient de l’éducation sur la santé à des démarches motivationnelles ne suffisent peut-être pas, même si elles sont nécessaires.
Cardiovascular disease (CVD) continues to be the leading health threat and cause of death in North America, accounting for approximately 40% of all deaths in Canada (1,2). The mortality rate from CVD has been declining slightly in North America over the past four decades (3,4) due, in part, to a parallel decrease in the prevalence of major CVD risk factors and improved care of patients with known CVD (2,5). Despite this decline, there are specific segments of the population, such as disadvantaged, urban, inner-city populations in the United States and Canada, that have a significantly higher CVD mortality rate (6) and higher prevalence of CVD risk factors (7–9). The causes for this inequality are not well understood, but may stem in part from the inadequate control of CVD risk factors.
From a prevention standpoint, the management of CVD risk factors plays an essential role in the reduction of CVD mortality, especially in those disadvantaged communities where the mortality from CVD is highest. Many prevention efforts over the past two decades have centred around improving awareness, because knowledge of CVD risk factors has been shown to be a prerequisite for change (10,11). Therefore, effective prevention strategies depend, in part, on the assessment of the knowledge level of the targeted population.
Previous attempts to describe CVD risk factor knowledge of disadvantaged populations include large cross-sectional studies that compared risk factor knowledge across socioeconomic gradients in a general population (12–15) and smaller studies that examined inner city samples alone (16–18). Data from these studies infer lower levels of knowledge in the inner city, but do not provide a direct comparison. However, because inner-city populations are under the influence of intertwined social factors, including crime, poverty, unemployment and social isolation (19), comparisons across socioeconomic gradients may not truly reflect the impact of an inner-city environment on knowledge. Also, aside from several small focus group studies (20,21), there is very little information regarding barriers to lowering CVD risk in the inner city. This information would be useful for the development of CVD prevention programs that target inner-city individuals.
The present study had the following objectives to address these deficiencies. The study aimed to determine the extent to which inner city factors influence awareness by directly comparing CVD risk factor knowledge in an inner city with that of the general population. Second, factors were identified that were associated with knowledge in the inner city. Finally, in an attempt to develop hypotheses for future heart health promotion efforts, potential barriers to reducing CVD risk factors are described.
METHODS
Study population
Study participants were recruited at the Family Practice Unit of the South Riverdale Community Health Centre (Toronto, Ontario) between June and August 2001. The Family Practice Unit employs a multidisciplinary team of health care workers, including five physicians, five nurse practitioners and six social workers. In addition, the health centre also has health promotion print material available to the community members. This unit primarily services South Riverdale, a predominantly low-income community in Toronto. There are 53,705 residents in this neighborhood. Ten per cent of this population arrived in Canada within the preceding five years, 51% of whom have high school education or less, and the area has an unemployment rate of 11.2%. Immigrants comprise 46% of the population, a large percentage of whom are Chinese (32.5%), Vietnamese (3.5%) and Portuguese (0.9%) (22).
Consecutive patients were approached for recruitment into the study on predetermined days. Eligible patients included all those older than 40 years of age who attended the Family Practice Unit. Patients who lived outside the catchment area, who could not respond to an English questionnaire or who had previously participated in the Canadian Heart Health Surveys were excluded.
The control population was a subset of the general population surveyed in the Canadian Heart Health Surveys between 1986 to 1992. This is the largest contemporary dataset available, which includes over 23,000 Canadians, and contains data regarding CVD risk factor prevalence and knowledge. The subset used consisted of all age-matched participants who were residents of Ontario and lived in cities with populations of more than 10,000, and was chosen to control for variations among different regions in Canada, as well as between rural communities and larger urban centres.
The present study was approved by the St Michael’s Hospital (Toronto, Ontario) research ethics board.
Survey development and administration
After informed consent was obtained, participants were administered a 30 min questionnaire. Height, weight and blood pressure measurements were taken, and a chart review for most recent blood pressure, blood glucose, total cholesterol and high-density lipoprotein values was conducted.
The questionnaire was developed by the authors to quantitatively measure CVD risk factor knowledge, CVD risk factors, socioeconomic factors and barriers to reducing CVD risk. All questions, except for those regarding barriers, were based on an abridged form of the Canadian Heart Health Surveys (23). The outcome measure regarding the knowledge of a particular CVD risk factor was evaluated using the open-ended question: “Can you tell me the major causes of heart disease or heart problems?”. Not mentioning a particular CVD risk factor was interpreted as not knowing its role in increasing CVD risk.
The exact definitions that were originally used in the Canadian Heart Health Surveys to define CVD risk factors were used to report risk factors to facilitate comparison between groups. The original definitions were previously described (24). For overall CVD risk, the Framingham risk score was calculated (25), and the 10-year risk for CVD was reported. Participants with a 30% or greater 10-year risk for CVD were considered to be at ‘very high’ risk. Individuals with missing data were not included. Participants with a history of diabetes, coronary artery disease (CAD) or stroke were automatically considered to be at ‘very high’ risk, regardless of their other risk factors (26). Socioeconomic variables used as covariates in our analysis included age, sex, marital status, education level, income level and occupational status. Aside from age, each of these variables was expressed categorically as defined by the Canadian Heart Health Surveys, as described elsewhere (13).
Of note, in an attempt to generate hypotheses, questions were created based on an American focus group work (21) to determine barriers to lowering CVD in the inner city.
Statistical analysis
Descriptive statistics (counts and percentages for discrete variables, and mean ± SD for continuous variables) were calculated for demographics, socioeconomic status, individual CVD risk factors, risk factor knowledge, Framingham risk level and barriers to CVD risk factor reduction. Comparison of socioeconomic variables, individual CVD risk factor prevalence and CVD risk factor knowledge between the two study populations was carried out using Pearson χ2 test for difference in proportions of categorical variables and Wilcoxon rank-sum test for differences in median values of continuous variables. Participants with missing data were excluded from the analysis.
Univariate analyses based on logistic regression were performed separately for the South Riverdale and Urban Ontario populations to establish the OR and the significance of the following outcome: good knowledge of CVD risk factors (three or more factors named). Variables identified significant by univariate analysis were selected in multivariate logistic regression using the backward elimination modelling method.
A level of P<0.05 was considered to be statistically significant. Statistical analyses were performed with SPSS version 11.0 (SPSS Inc, USA) under review by a statistician (author AB).
RESULTS
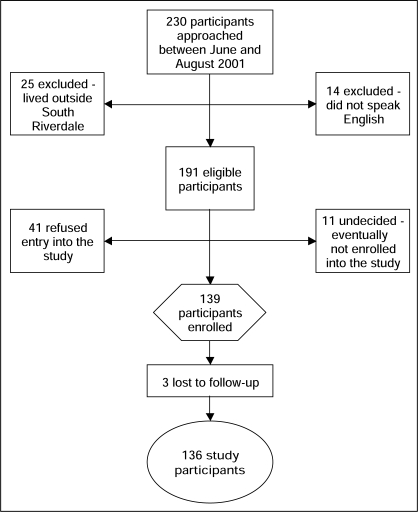
Of the 230 consecutive adults approached at the community health centre, 25 individuals (11%) were excluded because they lived outside of South Riverdale (Figure 1); only 14 (6%) were excluded on account of being unable to speak English. Of the 191 eligible patients, 55 (29%) were undecided or declined entry into the study. One hundred thirty-six patients were enrolled (71% participation rate). The control population (Canadian Heart Health Surveys subset) included 807 participants.
Figure 1).
Recruitment of participants from the South Riverdale community in Toronto, Ontario
The South Riverdale and Urban Ontario populations were comparable in age, sex, occupational status and medical history (Table 1). A greater proportion of the South Riverdale population was low-income, unmarried or had completed secondary school. Regarding CVD risk, the South Riverdale population had a larger proportion of ‘very high’ risk (30% or greater 10-year risk for CVD), overweight and diabetic participants, but a smaller proportion of sedentary individuals.
TABLE 1.
Characteristics of participants in South Riverdale and Urban Ontario study populations
| South Riverdale (n=136) | Urban Ontario (n=807) | P | |
|---|---|---|---|
| Socioeconomic factors | |||
| Age, years (mean ± SD) | 58.2±12.4 | 59.9±11.1 | 0.054 |
| Male sex, n (%) | 54 (40) | 384 (48) | 0.088 |
| Not married, n (%)* | 89 (66) | 217 (27) | <0.001 |
| Less than secondary school, n (%) | 38 (28) | 320 (40) | 0.009 |
| Low income, n (%)† | 36 (29) | 86 (11) | <0.001 |
| Unemployed, n (%)‡ | 74 (55) | 478 (59) | 0.335 |
| Born outside Canada, n (%) | 48 (35) | N/A | |
| CVD risk factors, n (%) | |||
| Smoking§ | 30 (22) | 144 (18) | 0.278 |
| Lack of exercise¶ | 27 (20) | 300 (37) | <0.001 |
| Obesity** | 82 (60) | 274 (41) | <0.001 |
| High blood pressure†† | 63 (46) | 376 (47) | 0.954 |
| Elevated cholesterol‡‡ | 65 (54) | 360 (59) | 0.315 |
| Diabetes§§ | 28 (21) | 70 (9) | <0.001 |
| Medical history, n (%) | |||
| History of myocardial infarction | 14 (10) | 83 (10) | 0.995 |
| History of stroke | 8 (6) | 29 (4) | 0.208 |
| Framingham risk level, n (%) ≥30% 10-year CVD risk | 42 (39) | 180 (28) | 0.020 |
*Widowed, never married, separated or divorced;
†1 to 2 people with income <$12,000 or 3+ people with income <$25,000;
‡Unemployed, retired, laid off, student or homemaker;
§Smoking at least one cigarette per day;
¶No leisure time physical activity at least once per week during the previous month;
**Body mass index ≥27 kg/m2;
††Systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg or treatment for hypertension;
‡‡Total fasting plasma cholesterol ≥5.2 mmol/L;
§§Self-reported history of diabetes, or oral hypoglycemic or insulin use. CVD Cardiovascular disease; N/A Not applicable
The ‘very high’ risk subgroups from each cohort were compared in a similar fashion. This subgroup from South Riverdale was significantly younger and had a greater proportion of unmarried, low-income, overweight and diabetic individuals compared with the ‘very high’ risk subgroup from Urban Ontario.
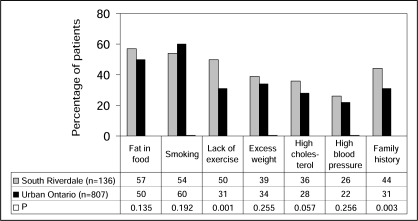
CVD risk factor knowledge was mostly similar in the South Riverdale and Urban Ontario populations (Figure 2), with a greater percentage identifying sedentary lifestyle and heredity in South Riverdale. Awareness of the ‘very high’ risk subgroups was also similar for most risk factors, with elevated cholesterol more readily identified by the South Riverdale subgroup. Overall, behavioural risk factors, such as smoking and fat in food, were more commonly identified than physiological risk factors, such as hypertension and dyslipidemia. The average number of risk factors named was higher in South Riverdale than in Urban Ontario (3.1 versus 2.6; P<0.001).
Figure 2).
Percentage of people who named specific risk factors for cardiovascular disease in South Riverdale compared with Urban Ontario (Canadian Heart Health Surveys)
Among participants with specific risk factors, there were few differences between groups regarding an at-risk participant’s ability to identify that particular factor (Table 2). A greater proportion of South Riverdale participants with sedentary lifestyles mentioned the lack of exercise being a factor. Overall, smokers were most aware of their risk behaviour, whereas patients with hypertension and dyslipidemia were least likely to be aware of their risk for CVD. Patients with a particular risk factor were equally able to identify that risk factor compared with those without that risk factor.
TABLE 2.
Ability of individuals with a specific risk factor to identify that risk factor as increasing cardiovascular disease risk
| Specific risk factor | South Riverdale | Urban Ontario | P |
|---|---|---|---|
| Hypertensive patients who mentioned hypertension | 23 (37) | 99 (26) | 0.09 |
| Overweight patients who mentioned obesity | 37 (45) | 113 (41) | 0.532 |
| Dyslipidemic patients who mentioned high cholesterol | 23 (35) | 107 (30) | 0.362 |
| Smoking patients who mentioned smoking | 22 (73) | 110 (76) | 0.722 |
| Patients with a sedentary lifestyle who mentioned lack of exercise | 13 (48) | 74 (25) | 0.008 |
Values are presented as n (%)
Univariate logistic regression analysis determined that correlates of good CVD risk factor knowledge (ie, three or more risk factors named) in South Riverdale included being married, having completed secondary school, having a higher income, being employed and not having diabetes (Table 3). For the Urban Ontario population, good knowledge of CVD risk factors was related to younger age, secondary school completion, higher income, employment, regular exercise, normal cholesterol level and a lower than 30% 10-year risk for CVD (Table 4).
TABLE 3.
Correlates of good cardiovascular disease risk factor knowledge in South Riverdale respondents
| Good knowledge (≥3 risk factors named, n=91) | Poor knowledge (<3 risk factors named, n=45) | OR (95% CI) | P | |
|---|---|---|---|---|
| Socioeconomic factors | ||||
| Secondary school completed, n (%) | 76 (84) | 21 (48) | 5.5 (2.5 to 12.5) | <0.001 |
| Married, n (%) | 39 (43) | 7 (16) | 4.0 (1.6 to 9.8) | 0.003 |
| Middle to high income, n (%)*† | 69 (79) | 21 (54) | 3.3 (1.5 to 7.4) | 0.004 |
| Employed, n (%)‡ | 49 (54) | 12 (27) | 3.1 (1.4 to 6.8) | 0.004 |
| Age, years (mean ± SD) | 57.3±11.4 | 59.9±14.2 | 1.2 (0.9 to 1.5)§ | 0.303 |
| Female sex, n (%) | 52 (57) | 30 (67) | 0.7 (0.3 to 1.4) | 0.287 |
| Cardiovascular disease risk factor, n (%) | ||||
| No diabetes | 77 (85) | 31 (69) | 2.5 (1.1 to 5.8) | 0.036 |
| No smoking | 75 (82) | 31 (69) | 2.1 (0.9 to 4.9) | 0.077 |
| Regular exercise | 75 (82) | 34 (76) | 1.5 (0.6 to 3.6) | 0.347 |
| Normal blood pressure | 51 (56) | 22 (49) | 1.3 (0.7 to 2.7) | 0.432 |
| Normal weight | 37 (41) | 17 (38) | 1.1 (0.5 to 2.4) | 0.747 |
| Normal cholesterol | 35 (43) | 20 (53) | 0.7 (0.3 to 1.5) | 0.310 |
| Framingham risk level, n (%) | ||||
| <30% 10-year cardiovascular disease risk | 47 (67) | 18 (49) | 2.2 (1.0 to 4.9) | 0.065 |
*Middle income defined as 1 person with income $12,000 to $24,999, 2 people with income $12,000 to $49,999 or 3+ people with income <$25,000;
†High income defined as 1 person with income ≥$25,000 or 2+ people with income ≥$50,000;
‡Full-time and part-time employment;
§OR for every decrease in 10 years of age
TABLE 4.
Correlates of good cardiovascular disease risk factor knowledge in Urban Ontario respondents
| Good knowledge (≥3 risk factors named, n=416) | Poor knowledge (<3 risk factors named, n=391) | OR (95% CI) | P | |
|---|---|---|---|---|
| Socioeconomic factors | ||||
| Employed, n (%)* | 212 (51) | 117 (30) | 2.4 (1.8 to 3.3) | <0.001 |
| Middle to high income, n (%)†‡ | 386 (93) | 335 (86) | 2.2 (1.3 to 3.4) | 0.001 |
| Secondary school completed, n (%) | 286 (69) | 196 (51) | 2.1 (1.6 to 2.8) | <0.001 |
| Age, years (mean ± SD) | 56.9±11.3 | 63.1±9.9 | 1.7 (1.5 to 1.9)§ | <0.001 |
| Married, n (%) | 310 (75) | 280 (72) | 1.2 (0.8 to 1.6) | 0.352 |
| Female sex, n (%) | 218 (52) | 205 (52) | 1.0 (0.8 to 1.3) | 0.994 |
| Cardiovascular disease risk factor, n (%) | ||||
| Regular exercise | 277 (67) | 230 (59) | 1.4 (1.0 to 1.9) | 0.023 |
| Normal cholesterol | 152 (44) | 97 (36) | 1.4 (1.0 to 1.9) | 0.044 |
| No diabetes | 385 (93) | 352 (90) | 1.4 (0.8 to 2.3) | 0.205 |
| Normal weight | 224 (61) | 167 (56) | 1.3 (0.9 to 1.7) | 0.137 |
| Normal blood pressure | 232 (56) | 199 (51) | 1.2 (0.9 to 1.6) | 0.166 |
| No smoking | 331 (82) | 319 (82) | 1.0 (0.7 to 1.4) | 0.801 |
| Framingham risk level, n (%) | ||||
| <30% 10-year cardiovascular disease risk | 269 (78) | 191 (65) | 1.9 (1.4 to 2.7) | <0.001 |
*Full-time and part-time employment;
†Middle income defined as 1 person with income $12,000 to $24,999, 2 people with income $12,000 to $49,999 or 3+ people with income <$25,000;
‡High income defined as 1 person with income ≥$25,000 or 2+ people with income ≥$50,000;
§OR for every decrease in 10 years of age
Multivariate logistic regression analysis showed that in South Riverdale, being married (OR 3.65, 95% CI 1.40 to 9.51; P=0.008) and having completed secondary school (OR 14.92, 95% CI 2.26 to 12.09; P<0.001) were independently related to good knowledge of CVD risk factors. In Urban Ontario, younger age (OR 1.62, 95% CI 1.41 to 1.86; P<0.001), secondary school completion (OR 1.755, 95% CI 1.30 to 2.37; P<0.001) and partaking in regular exercise (OR 1.417, 95% CI 1.05 to 1.92; P=0.024) were independently related to good knowledge of CVD risk factors.
A description of potential barriers to reducing CVD risk is summarized in Table 5. Lack of motivation (57%), lack of time (34%) and lack of money (30%) were the most common barriers mentioned. Subjective lack of knowledge was not believed to be an important factor.
TABLE 5.
Barriers to cardiovascular disease risk reduction mentioned by South Riverdale population
| Barrier mentioned | Participants, n (%) |
|---|---|
| Lack of motivation | 78 (57) |
| Lack of time | 46 (34) |
| Lack of money | 41 (30) |
| A chronic disease or physical disability | 35 (26) |
| Limited access to health resources | 31 (23) |
| Lack of energy | 26 (19) |
| Subjective lack of knowledge | 17 (13) |
| Lack of safe areas to exercise | 9 (7) |
DISCUSSION
Despite the fact that inner-city populations experience higher mortality rates from CVD (6) and have higher levels of CVD risk factors (7,8), to our knowledge, the present study is one of the first to directly compare CVD risk factor knowledge between an inner-city and a general adult population in Canada. Our results demonstrate that individuals in the inner city are equally aware, if not more aware, of the causes of CVD as the general population. Our study also suggests that a deficiency in knowledge does not account for the disparity seen in inner-city individuals at very high risk for CVD.
These findings were somewhat surprising, given that previous studies have linked low socioeconomic status to low levels of awareness (12–15). However, those results may not apply to inner-city populations; participants who are assigned low socioeconomic status based on income, education or occupation in those studies do not necessarily live in inner-city areas. Our results provide a unique viewpoint, because we have isolated an inner-city population to measure awareness. Our data demonstrate that although the relationship between socioeconomic status and knowledge exists within the lowest tier of social class, the impact of an inner-city environment on awareness does not appear to be significant.
While knowledge in the Canadian inner-city population is similar to the general population, the actual level of awareness in both populations is strikingly low. This was especially true for physiological CVD risk factors (hypertension, dyslipidemia), a trend that has been similarly described in other series (12,13). More concerning is the lack of awareness seen in patients with specific risk factors. The ability to identify a specific risk factor that one possesses is necessary for behaviour modification and has been widely accepted as an important first step by health education programs (10,11).
Despite the generally low level of awareness, there was no relationship between existing knowledge and CVD risk in South Riverdale. While this has been shown previously in a predominantly Caucasian, middle-class population (12) and was confirmed in our Urban Ontario population, it has not been shown to date in the inner city. Our results suggest that the lack of correlation between knowledge and CVD risk extends to include inner-city populations, and may explain why previous attempts at community-based cardiac prevention programs in disadvantaged areas that focused on improving awareness may have had limited success (27–29). Given the lack of association between knowledge and CVD risk, future evaluation of heart health promotion efforts aimed at improving awareness should also include health outcome measures.
In evaluating additional factors that lead to an increased risk of CVD in the inner city, some smaller studies have qualitatively reported barriers to reducing CVD risk in nonhomeless, inner-city populations (16,21). To our knowledge, there are few other studies that have attempted to quantitatively describe barriers to reducing CVD risk. We found that in this inner-city population, the most commonly reported barriers were lack of motivation, lack of time and lack of money. The overwhelming lack of motivation may explain why community-based CVD prevention programs directed at the needs of disadvantaged neighbourhoods reported low levels of program participation (27).
Regarding other barriers, the competing priority to meet subsistence needs is an important barrier to medical care in the homeless population (30). Inner-city individuals have similar concerns, making time constraint a significant barrier to addressing behaviour change. Financial burden, clearly a major concern in all areas of inner-city life, makes certain health choices such as registering at a gym or purchasing healthy food difficult.
Unfortunately, we are unable to make a comparison between the inner city and the general population regarding barriers, because there are limited published, population-based data of global barriers to reducing CVD risk. Current data are more focused on medication compliance (31,32) and access to care (33). We believe, however, that these data provide a quantitative description of important barriers and offer insight into the development of patient-centred heart health promotion interventions in the inner city.
Limitations
The present study has some inherent limitations. The South Riverdale population was sampled through a family practice unit, likely accounting for the greater proportion of individuals who were overweight, had diabetes and who were at very high risk for CVD. However, our results are in keeping with previous studies that reported elevated CVD risk factor levels in the inner city (8,9), and higher mortality rates due to CVD in disadvantaged populations (6). This sample may also be more health conscious, biasing our results toward the overestimation of knowledge level in the inner city sample. Although this may be true, it is this attentive group that is likely to participate in community-based interventions, and so a clear understanding of this group’s knowledge level remains extremely valuable.
There was a high proportion of well-educated people in our inner city population, which is atypical for a traditional inner-city neighbourhood (19). This might have been due to a sampling bias, possibly resulting in the over-representation of the more advantaged segment of our inner-city population. However, 1996 census data for this neighborhood show that our sample is comparable with regard to income, education and occupation level (22). This may reflect an educated immigrant effect seen in the Canadian inner city, so our results may not reflect other inner-city populations with lower levels of education.
Potentially, our data are limited by the temporal gap between comparison groups. Some studies suggest improvement in knowledge over time (14), based on data generated 15 years ago. However, more contemporary data from a Canadian Heart Health Passport study suggest a recent plateau in knowledge levels, finding that overall CVD knowledge remains poor in the general population (34). Nonetheless, this is the most recent complete database containing data regarding CVD risk and CVD risk factor knowledge that was available to us at the time.
CONCLUSIONS
Our results suggest that the level of CVD risk factor knowledge in the inner city, although poor overall, is similar to that of the general population. The degree of risk factor knowledge alone does not appear to be a major determinant of cardiovascular risk reduction in the inner city. However, a number of barriers to reducing CVD risk were identified and quantified. These results have implications for primary prevention of CVD in the inner city and suggest that interventions that combine health education with motivational approaches, while necessary, may not be sufficient. Instead, a broader strategy that addresses barriers associated with inner city life, such as financial limitations and competing priorities, may be more successful.
REFERENCES
- 1.Anderson RN.National Vital Statistics Report. 49(11). 10/12/2001. Hyattsville, National Center for Health Statistics.
- 2.Wielgosz A. The changing face of heart disease and stroke in Canada. Ottawa: Heart and Stroke Foundation of Canada; 1999. [PubMed] [Google Scholar]
- 3.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: Findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102:3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 4.Higgins M, Thom T. Trends in CHD in the United States. Int J Epidemiol. 1989;18:S58–66. [PubMed] [Google Scholar]
- 5.Pater C. The current status of primary prevention in coronary heart disease. Curr Control Trials Cardiovasc Med. 2001;2:24–37. doi: 10.1186/cvm-2-1-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCord C, Freeman HP. Excess mortality in Harlem. N Engl J Med. 1990;322:173–7. doi: 10.1056/NEJM199001183220306. [DOI] [PubMed] [Google Scholar]
- 7.Bartley M, Fitzpatrick R, Firth D, Marmot M. Social distribution of cardiovascular disease risk factors: Change among men in England 1984–1993. J Epidemiol Community Health. 2000;54:806–14. doi: 10.1136/jech.54.11.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szerlip MI, Szerlip HM. Identification of cardiovascular risk factors in homeless adults. Am J Med Sci. 2002;324:243–6. doi: 10.1097/00000441-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Diez-Roux AV, Northridge ME, Morabia A, Bassett MT, Shea S. Prevalence and social correlates of cardiovascular disease risk factors in Harlem. Am J Public Health. 1999;89:302–7. doi: 10.2105/ajph.89.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- 11.Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218. [PubMed] [Google Scholar]
- 12.Avis NE, McKinlay JB, Smith KW. Is cardiovascular risk factor knowledge sufficient to influence behavior? Am J Prev Med. 1990;6:137–44. [PubMed] [Google Scholar]
- 13.Potvin L, Richard L, Edwards AC. Knowledge of cardiovascular disease risk factors among the Canadian population: Relationships with indicators of socioeconomic status. CMAJ. 2000;162(Suppl):S5–11. [PMC free article] [PubMed] [Google Scholar]
- 14.Davis SK, Winkleby MA, Farquhar JW. Increasing disparity in knowledge of cardiovascular disease risk factors and risk-reduction strategies by socioeconomic status: Implications for policymakers. Am J Prev Med. 1995;11:318–23. [PubMed] [Google Scholar]
- 15.Gans KM, Assmann SF, Sallar A, Lasater TM. Knowledge of cardiovascular disease prevention: An analysis from two New England communities. Prev Med. 1999;29:229–37. doi: 10.1006/pmed.1999.0532. [DOI] [PubMed] [Google Scholar]
- 16.Behera SK, Winkleby MA, Collins R. Low awareness of cardiovascular disease risk among low-income African-American women. Am J Health Promot. 2000;14:301–5. iii. doi: 10.4278/0890-1171-14.5.301. [DOI] [PubMed] [Google Scholar]
- 17.Hyman DJ, Simons-Morton DG, Dunn JK, Ho K. Smoking, smoking cessation, and understanding of the role of multiple cardiac risk factors among the urban poor. Prev Med. 1996;25:653–9. doi: 10.1006/pmed.1996.0103. [DOI] [PubMed] [Google Scholar]
- 18.Poduri A, Grisso JA. Cardiovascular risk factors in economically disadvantaged women: A study of prevalence and awareness. J Natl Med Assoc. 1998;90:531–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Wasylenki DA. Inner city health. CMAJ. 2001;164:214–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Molokhia M, Oakeshott P. A pilot study of cardiovascular risk assessment in Afro-Caribbean patients attending an inner city general practice. Fam Pract. 2000;17:60–2. doi: 10.1093/fampra/17.1.60. [DOI] [PubMed] [Google Scholar]
- 21.Gettleman L, Winkleby MA. Using focus groups to develop a heart disease prevention program for ethnically diverse, low-income women. J Community Health. 2000;25:439–53. doi: 10.1023/a:1005155329922. [DOI] [PubMed] [Google Scholar]
- 22.City of TorontoWard 30: Broadview-Greenwood Profile. <www.toronto.ca/wards2000/ward30.htm> (Version current at April 24, 2008).
- 23.MacLean DR, Petrasovits A, Nargundkar M, et al. Canadian heart health surveys: A profile of cardiovascular risk. Survey methods and data analysis. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1969–74. [PMC free article] [PubMed] [Google Scholar]
- 24.Choinière R, Lafontaine P, Edwards AC. Distribution of cardiovascular disease risk factors by socioeconomic status among Canadian adults. CMAJ. 2000;162:S13–24. [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 26.Fodor JG, Frohlich JJ, Genest JJ, Jr, McPherson PR. Recommendations for the management and treatment of dyslipidemia. Report of the Working Group on Hypercholesterolemia and Other Dyslipidemias. CMAJ. 2000;162:1441–7. [PMC free article] [PubMed] [Google Scholar]
- 27.O’Loughlin JL, Paradis G, Gray-Donald K, Renaud L. The impact of a community-based heart disease prevention program in a low-income, inner-city neighborhood. Am J Public Health. 1999;89:1819–26. doi: 10.2105/ajph.89.12.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shea S, Basch CE, Wechsler H, Lantigua R. The Washington Heights-Inwood Healthy Heart Program: A 6-year report from a disadvantaged urban setting. Am J Public Health. 1996;86:166–71. doi: 10.2105/ajph.86.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brownson RC, Smith CA, Pratt M, et al. Preventing cardiovascular disease through community-based risk reduction: The Bootheel Heart Health Project. Am J Public Health. 1996;86:206–13. doi: 10.2105/ajph.86.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87:217–20. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson EC, Stason WB, Neutra RR, Solomon HS, McArdle PJ. Impact of patient perceptions on compliance with treatment for hypertension. Med Care. 1978;16:893–906. doi: 10.1097/00005650-197811000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Clark LT. Improving compliance and increasing control of hypertension: Needs of special hypertensive populations. Am Heart J. 1991;121:664–9. doi: 10.1016/0002-8703(91)90443-l. [DOI] [PubMed] [Google Scholar]
- 33.Moy E, Bartman BA, Weir MR. Access to hypertensive care. Effects of income, insurance, and source of care. Arch Intern Med. 1995;155:1497–502. [PubMed] [Google Scholar]
- 34.Heart and Stroke Foundation of Canada. Seven Deadly Myths Threatening Canadians’ Heart Health, says Heart and Stroke Foundation’s Annual Report Card. 1/2/2003.