Abstract
BACKGROUND:
Many Canadians known to have hypertension remain untreated. To aid in the development of specific programs to improve hypertension management, the present report characterizes Canadians who indicated that they had hypertension but were not taking antihypertensive drug therapy.
METHODS:
The 2005 Canadian Community Health Survey (cycle 3.1) was used to estimate the proportion of Canadians 20 years of age and older who reported having high blood pressure or ever being diagnosed with high blood pressure. Sociodemographic characteristics, reported health, lifestyle factors and health care resource use of those who reported taking or not taking high blood pressure medication in the previous month were described and compared.
RESULTS:
Over one-half of hypertensive respondents 20 to 39 years of age reported no antihypertensive treatment compared with 17% and 5% among those 40 to 59 years and 60 years of age and older, respectively. In most age groups, several factors were associated with the absence of pharmacotherapy (eg, male sex, fewer health care professional consultations, perceived excellent health status and most markers of lower cardiovascular risk, with the exception of daily smoking). The proportion of young hypertensive Canadians not receiving pharmacotherapy remained consistent, regardless of the presence of cardiovascular risk factors.
CONCLUSIONS:
Many hypertensive Canadians, particularly those who are younger than 60 years of age, are not taking antihypertensive drug therapy despite having one or more cardiovascular risks. The increased risk of no drug therapy among smokers warrants special attention.
Keywords: Antihypertensive drugs, Health survey, Increased risk, Patient education
Abstract
HISTORIQUE :
De nombreux Canadiens qu’on sait hypertendus ne sont pas traités. Pour contribuer à l’élaboration de programmes précis en vue d’améliorer la prise en charge de l’hypertension, le présent rapport caractérise les Canadiens qui ont indiqué être hypertendus mais ne pas prendre d’antihypertensifs.
MÉTHODOLOGIE :
Les auteurs ont fait appel à l’Enquête sur la santé dans les collectivités canadiennes (cycle 3.1) de 2005 pour évaluer la proportion de Canadiens de 20 ans et plus qui déclaraient être hypertendus ou avoir déjà reçu un diagnostic d’hypertension. Ils ont décrit et comparé les caractéristiques sociodémographiques, l’état de santé déclaré, les facteurs reliés au mode de vie et l’utilisation des ressources de santé des personnes qui déclaraient prendre ou ne pas prendre de médicaments au cours des mois précédents.
RÉSULTATS :
Plus de la moitié des répondants hypertendus de 20 à 39 ans ont déclaré ne suivre aucun traitement antihypertensif par rapport à 17 % et 5 % de ceux de 40 à 59 ans et de 60 ans et plus, respectivement. Dans la plupart des groupes d’âge, plusieurs facteurs s’associaient à l’absence de pharmacothérapie (p. ex., sexe masculin, moins de consultations auprès d’un professionnel de la santé, perception d’un excellent état de santé et la plupart des marqueurs d’un faible risque cardiovasculaire, à l’exception du tabagisme quotidien). La proportion de jeunes Canadiens hypertendus qui ne prenaient pas d’antihypertensifs demeurait importante, quelle que soit la présence de facteurs de risque cardiovasculaires.
CONCLUSIONS :
De nombreux Canadiens hypertendus, notamment ceux de moins de 60 ans, ne prennent pas d’antihypertensifs même s’ils ont au moins un risque cardiovasculaire. Le risque plus élevé relié à l’absence de pharmacothérapie chez les fumeurs mérite une attention particulière.
Hypertension affects approximately 25% of the adult population worldwide (1). The prevalence of hypertension increases markedly with age, and the lifetime residual risk for developing hypertension is higher than 90% even in people with normal blood pressure at 65 years of age (2). Hypertension is also the leading risk factor for death in the world (3). Despite the availability of effective antihypertensive therapies and evidence that supports the cardiovascular benefit of hypertension management (4), treatment and control rates are still far less than ideal (5).
Recent Canadian data have shown significant increases in the diagnosis of hypertension and increased prescriptions of antihypertensive therapy (6,7). The increase in antihypertensive prescriptions represents a combination of more people being prescribed antihypertensive drugs, increased use of more than one hypertensive drug and reduction in discontinuing of antihypertensive therapy (6,8–10). However, even after nine years of an extensive health care professional education program on hypertension management, many people with hypertension are still not being treated with antihypertensive therapy (6,9,11). Developing interventions to further improve the treatment of hypertension would be facilitated by an understanding of the characteristics of hypertensive Canadians not receiving antihypertensive drugs. The present study analyzed data from a representative sample of adult Canadians participating in the 2005 Canadian Community Health Survey (CCHS) cycle 3.1 to identify sociodemographic, health and lifestyle characteristics associated with having a diagnosis of hypertension but not receiving drug treatment.
METHODS
Study population
The study population was derived from the 2005 CCHS. The CCHS is a cross-sectional survey of a representative sample of household residents 12 years of age and older in all Canadian provinces and territories. The survey excluded populations on Native reserves, Canadian Forces bases and some remote areas. Hypertension was defined as being present among respondents who reported currently or ever having high blood pressure lasting six months or longer and diagnosed by a health care professional. Antihypertensive treatment status was determined by responses to the survey question, “In the past month, have you taken any medicine for high blood pressure?”. Because treatment was defined in relation to recent use, patients who were diagnosed with hypertension in the past but reported that they did not currently have hypertension and had not used medication in the previous month were excluded from the analyses (3.8% of the overall CCHS sample). In addition, respondents who were younger than 20 years of age (0.2%), pregnant (0.1%) or those with missing values for the study variables (1.4%) were excluded.
Study variables
The covariates examined included respondents’ sociodemographic characteristics, reported health status, lifestyle factors and health care resource use. The sociodemographic characteristics included age, sex, marital status, household income, household size and immigration status. The reported health characteristics included self-rated health and number of comorbid chronic health conditions. The lifestyle factors examined included body mass index, smoking status and level of physical activity. The reported number of consultations with a physician in the previous year was used to reflect health care resource use.
Statistical analysis
In the CCHS, household residents are identified across 126 health regions using multistage sampling methodology (a detailed description of the sampling frame and design methodology can be found at www.statcan.ca/english/concepts/health/cycle3_1/index.htm). The sampling method required reweighting the health regions to recover unbiased estimates and correct standard errors.
Because the associations between selected covariates and receipt of antihypertensive medication are likely to vary by age, the study population was divided into three age-based strata: 20 to 39 years, 40 to 59 years, and 60 years and older. A structural break test, the Chow test, confirmed the differences between age groups. Descriptive statistics for the study variables were calculated to describe the hypertensive population according to the presence or absence of antihypertensive therapy. Variations in the proportion of hypertensive respondents not receiving pharmacotherapy by selected covariates of interest, including age, sex, physician consultations and cardiovascular risk were examined. Characteristics depicting a high cardiovascular risk included diabetes, a body mass index greater than 30 kg/m2, physical inactivity and daily smoking. Statistical differences were calculated with χ2 tests. Multivariable logistic regression was used to examine the independent associations between selected covariates and the absence of antihypertensive therapy. All frequencies and OR were weighted to account for Statistics Canada multistage sampling methodology.
RESULTS
Overall, 12.7% of aware adult hypertensive Canadians reported that they were not taking antihypertensive drug treatment. The proportion of aware hypertensive respondents who reported not receiving antihypertensive drug treatment was highest among those 20 to 39 years of age (54.9%), and lower among those 40 to 59 years and 60 years of age and older (17.3% and 4.6%, respectively).
The distribution of sociodemographic and health characteristics among hypertensive respondents by age is shown in Table 1. Relative to those 60 years of age and older, younger respondents were more likely to be male, married, in higher income groups and have larger household sizes. They were also more likely to report having few or no chronic health conditions, good to very good health, higher body mass index values and being current smokers.
TABLE 1.
Characteristics of adult hypertensive respondents (Canadian Community Health Survey, 2005)
| Characteristic | Age 20–39 years, n (%) | Age 40–59 years, n (%) | Age 60+ years, n (%) | |
|---|---|---|---|---|
| Region | Atlantic | 179 (8.6) | 1179 (10.5) | 2292 (8.9) |
| Quebec | 236 (17.9) | 1690 (24.3) | 3443 (24.6) | |
| Ontario | 451 (45.5) | 2320 (39.2) | 5185 (38.7) | |
| Prairie | 366 (27.6) | 2113 (25.8) | 4947 (27.8) | |
| Northern regions | 32 (0.4) | 130 (0.2) | 107 (0.1) | |
| Sex | Male | 681 (58.0) | 3499 (52.1) | 5955 (42.6) |
| Female | 583 (42.1) | 3933 (47.9) | 10,019 (57.4) | |
| Marital status* | Married/common law | 723 (65.2) | 4786 (78.0) | 7944 (64.3) |
| Widowed/separated/divorced | 92 (5.6) | 1558 (13.2) | 7098 (31.1) | |
| Single, never married | 449 (29.2) | 1088 (8.8) | 932 (4.6) | |
| Household income† | <$30,000 | 219 (13.0) | 1385 (11.8) | 5746 (27.3) |
| $30,000–$49,999 | 214 (14.3) | 1257 (13.5) | 2796 (19.1) | |
| $50,000–$79,999 | 285 (22.7) | 1576 (22.6) | 1657 (13.2) | |
| $80,000+ | 297 (28.7) | 1653 (31.3) | 757 (8.3) | |
| Missing | 249 (21.4) | 1561 (20.7) | 5018 (32.1) | |
| Household size | 1 | 253 (9.5) | 2163 (12.5) | 7529 (28.0) |
| 2 | 309 (22.5) | 3635 (39.6) | 7673 (58.1) | |
| 3 | 307 (26.8) | 845 (19.8) | 556 (8.5) | |
| 4+ | 395 (41.2) | 789 (28.1) | 216 (5.4) | |
| Immigration status | Born in Canada | 1134 (79.7) | 6469 (77.3) | 13,281 (75.1) |
| <9 years in Canada | 54 (10.3) | 103 (3.7) | 43 (0.7) | |
| 10+ years in Canada | 76 (10.1) | 860 (19.0) | 2650 (24.2) | |
| Number of physician consultations in previous year | 0 | 199 (17.2) | 709 (9.4) | 1141 (7.8) |
| 1 | 161 (12.4) | 995 (14.5) | 1682 (10.8) | |
| 2 | 199 (15.0) | 1228 (17.2) | 2350 (15.3) | |
| 3 | 147 (12.4) | 911 (13.3) | 1982 (12.4) | |
| 4 | 132 (9.6) | 1232 (16.4) | 3471 (21.0) | |
| 5+ | 426 (33.4) | 2357 (29.2) | 5348 (32.8) | |
| Number of chronic health conditions | 0 | 848 (71.2) | 3240 (49.6) | 3747 (26.1) |
| 1 | 309 (21.6) | 2416 (31.2) | 5754 (37.3) | |
| 2 | 84 (5.9) | 1163 (12.9) | 3810 (22.2) | |
| 3+ | 23 (1.3) | 613 (6.3) | 2663 (14.4) | |
| Perceived health | Excellent | 103 (8.7) | 531 (7.5) | 1049 (7.2) |
| Very good | 401 (35.4) | 2131 (31.0) | 4112 (26.4) | |
| Good | 529 (39.4) | 2812 (39.0) | 5960 (37.4) | |
| Fair | 184 (13.0) | 1427 (17.5) | 3617 (21.9) | |
| Poor | 47 (3.4) | 531 (5.6) | 1236 (7.1) | |
| Body mass index†, kg/m2 | <25 | 330 (27.8) | 1626 (23.5) | 5411 (33.5) |
| 25–30 | 432 (37.9) | 2760 (39.5) | 6417 (41.5) | |
| >30 | 474 (32.8) | 2852 (34.7) | 3751 (23.0) | |
| Missing | 28 (1.5) | 194 (2.4) | 395 (2.0) | |
| Smoking | Not at all | 841 (68.7) | 5515 (76.6) | 14,135 (89.3) |
| Occasionally | 66 (5.4) | 262 (3.8) | 299 (1.9) | |
| Daily | 357 (25.9) | 1655 (19.6) | 1540 (8.9) | |
| Physical activity | Active | 301 (23.6) | 1350 (18.7) | 2567 (16.8) |
| Moderate | 298 (23.7) | 1853 (24.5) | 3648 (24.5) | |
| Inactive | 665 (52.8) | 4229 (56.9) | 9759 (58.7) |
All percentages were weighted using Statistics Canada’s bootstrap method, and frequencies were not weighted.
Married/common law and widowed/separated/divorced were combined;
A ‘missing’ category was added for the income and body mass index variables
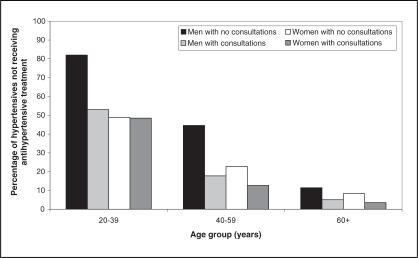
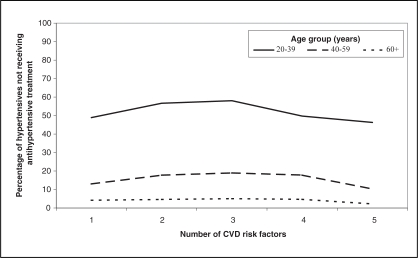
The proportion of hypertensive respondents (by age and drug treatment status) with specific cardiovascular risk factors is shown in Table 2. Consistently in all age categories, the proportion of those with diabetes, physical inactivity and obesity were taking antihypertensive drug therapy was higher than those not taking drug therapy, except for inactive Canadians older than 60 years of age. Conversely, across all ages, treatment was less likely among those reporting daily smoking. In addition, male (all age groups) and female (40 years of age and older) respondents with no physician consultations in the previous year were less likely to receive antihypertensive treatment (Figure 1). Approximately 50% of hypertensive Canadians 20 to 39 years of age were not taking antihypertensive therapy, regardless of the number of other risk factors they had (Figure 2).
TABLE 2.
The proportion of adult hypertensive respondents with cardiovascular risk factors by antihypertensive treatment status (Canadian Community Health Survey, 2005)
| Not treated, n (%)
|
Treated, n (%)
|
||
|---|---|---|---|
| Age 20–39 years | (n=650) | (n=614) | P |
| Diabetes | 25 (3.5) | 81 (11.6) | <0.0001 |
| Physical inactivity | 307 (48.1) | 358 (58.5) | <0.0001 |
| Obesity (BMI >30 kg/m2) | 221 (27.4) | 253 (39.4) | <0.0001 |
| Daily smoking | 220 (32.6) | 137 (17.7) | <0.0001 |
| Age 40–59 years | (n=1192) | (n=6240) | |
| Diabetes | 64 (4.3) | 1138 (17.1) | <0.0001 |
| Physical inactivity | 645 (52.9) | 3584 (57.7) | <0.0001 |
| Obesity (BMI >30 kg/m2) | 376 (29.0) | 2476 (35.9) | <0.0001 |
| Daily smoking | 367 (25.7) | 1288 (18.3) | <0.0001 |
| Age >60 years | (n=666) | (n=15,308) | |
| Diabetes | 80 (11.3) | 3125 (19.7) | <0.0001 |
| Physical inactivity | 394 (59.0) | 9365 (58.7) | 0.30 |
| Obesity (BMI >30 kg/m2) | 135 (20.2) | 3616 (23.1) | <0.0001 |
| Daily smoking | 88 (10.0) | 1452 (8.2) | <0.0001 |
All percentages were weighted using Statistics Canada’s bootstrap method, and frequencies were not weighted. BMI Body mass index
Figure 1.
The proportion of aware adult hypertensive respondents not receiving antihypertensive treatment by age, sex and number of physician consultations in the previous year (Canadian Community Health Survey, 2005)
Figure 2.
The proportion of aware adult hypertensive respondents not receiving antihypertensive treatment by number of cardiovascular disease (CVD) risk factors (ie, male sex, daily or occasional smoking, obesity [body mass index >30 kg/m2], diabetes and physical inactivity) and age
After adjustment for selected covariates (Table 3), the likelihood of not reporting antihypertensive treatment was significantly higher in male respondents and those who reported no physician consultations in the previous year, excellent self-rated health and daily smoking. Many of the other sociodemographic and health characteristics associated with the absence of drug therapy differed across the age groups. In respondents 60 years of age and older, being married, having a higher income, coming from a smaller household size, being an immigrant, having no other medical conditions, being overweight but not obese and being physically inactive were significantly associated with reports of no antihypertensive therapy. In respondents younger than 60 years of age, among whom a higher proportion were untreated, being single, having a low income, coming from a large household size and having a normal body mass index were significantly associated with the absence of antihypertensive treatment.
TABLE 3.
The proportion and risk-adjusted OR (95% CI)* of aware adult hypertensive respondents not receiving antihypertensive treatment in the previous month (Canadian Community Health Survey, 2005)
| Age 20–39 years
|
Age 40–59 years
|
Age 60+ years
|
|||||
|---|---|---|---|---|---|---|---|
| n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | ||
| Overall | 650 (54.9) | 1192 (17.3) | 666 (4.6) | ||||
| Sex | Male | 376 (59.5) | 687 (20.7) | 296 (5.6) | |||
| Female | 274 (48.5) | 0.83 (0.82–0.85) | 505 (13.5) | 0.64 (0.63–0.65) | 370 (3.9) | 0.79 (0.78–0.8) | |
| Marital status† | Married/common law | 345 (50.7) | 687 (16.2) | 327 (4.8) | |||
| Widowed/separated/divorced | 41 (48.2) | 0.76 (0.73–0.79) | 295 (21.6) | 1.69 (1.66–1.71) | 286 (4.0) | 0.57 (0.56–0.59) | |
| Single, never married | 264 (65.4) | 1.86 (1.82–1.90) | 210 (20.5) | 1.67 (1.64–1.70) | 53 (6.4) | 0.89 (0.86–0.92) | |
| Household income‡ | <$30,000 | 122 (61.7) | 240 (18.4) | 224 (4.0) | |||
| $30,000–$49,999 | 112 (51.1) | 0.79 (0.76–0.82) | 199 (17.9) | 0.92 (0.90–0.94) | 113 (3.9) | 1.03 (1–1.05) | |
| $50,000–$79,999 | 133 (46.8) | 0.56 (0.55–0.58) | 262 (19.4) | 0.87 (0.85–0.88) | 68 (4.8) | 1.22 (1.19–1.25) | |
| $80,000+ | 148 (55.1) | 0.68 (0.66–0.71) | 268 (16.6) | 0.63 (0.62–0.64) | 52 (8.2) | 1.61 (1.57–1.65) | |
| Missing | 135 (61.5) | 0.92 (0.89–0.95) | 223 (14.9) | 0.65 (0.64–0.66) | 209 (4.6) | 1.22 (1.2–1.24) | |
| Household size | 1 | 136 (53.2) | 393 (19.4) | 332 (4.8) | |||
| 2 | 164 (56.0) | 1.56 (1.50–1.62) | 461 (13.4) | 1.12 (1.10–1.15) | 298 (4.0) | 0.45 (0.44–0.46) | |
| 3 | 153 (53.1) | 1.58 (1.52–1.64) | 164 (19.3) | 1.77 (1.73–1.80) | 26 (6.5) | 0.73 (0.71–0.75) | |
| 4+ | 197 (55.8) | 1.67 (1.61–1.73) | 174 (20.2) | 1.84 (1.80–1.87) | 10 (7.2) | 0.58 (0.56–0.6) | |
| Immigration status | Born in Canada | 588 (56.1) | 1027 (17.2) | 524 (4.2) | |||
| <9 years in Canada | 26 (50.8) | 1.08 (1.04–1.11) | 22 (14.8) | 0.78 (0.76–0.80) | 6 (25.6) | 7.03 (6.74–7.34) | |
| 10+ years in Canada | 36 (49.7) | 0.69 (0.67–0.71) | 143 (17.8) | 0.95 (0.94–0.96) | 136 (5.5) | 1.31 (1.29–1.33) | |
| Number of physician consultations in the previous year | 0 | 136 (73.9) | 245 (36.0) | 108 (9.8) | |||
| 1 | 109 (72.1) | 0.98 (0.95–1.02) | 238 (23.7) | 0.56 (0.55–0.57) | 114 (7.6) | 0.69 (0.67–0.7) | |
| 2 | 122 (65.9) | 0.81 (0.78–0.83) | 212 (19.9) | 0.45 (0.44–0.45) | 131 (7.3) | 0.72 (0.71–0.74) | |
| 3 | 73 (55.3) | 0.49 (0.47–0.50) | 120 (13.2) | 0.26 (0.26–0.27) | 76 (3.5) | 0.34 (0.33–0.35) | |
| 4 | 45 (28.6) | 0.15 (0.15–0.16) | 109 (10.4) | 0.19 (0.18–0.19) | 76 (2.3) | 0.22 (0.21–0.22) | |
| 5+ | 165 (41.2) | 0.28 (0.27–0.28) | 268 (12.2) | 0.23 (0.22–0.23) | 161 (3.1) | 0.31 (0.3–0.31) | |
| Number of chronic health conditions | 0 | 451 (56.3) | 631 (20.5) | 219 (6.9) | |||
| 1 | 150 (50.5) | 1.06 (1.03–1.08) | 349 (15.2) | 0.82 (0.81–0.82) | 246 (4.4) | 0.78 (0.77–0.79) | |
| 2 | 39 (51.8) | 1.32 (1.27–1.37) | 147 (12.6) | 0.74 (0.73–0.75) | 131 (3.7) | 0.74 (0.72–0.75) | |
| 3+ | 10 (62.3) | 4.92 (4.50–5.38) | 65 (11.3) | 0.62 (0.61–0.64) | 70 (2.6) | 0.56 (0.55–0.58) | |
| Perceived health | Excellent | 68 (61.5) | 108 (21.3) | 63 (7.7) | |||
| Very good | 222 (58.8) | 0.91 (0.88–0.94) | 345 (19.4) | 0.98 (0.97–1.00) | 190 (5.1) | 0.78 (0.77–0.8) | |
| Good | 264 (52.7) | 0.77 (0.74–0.80) | 442 (15.6) | 0.83 (0.81–0.84) | 226 (4.4) | 0.72 (0.7–0.74) | |
| Fair | 81 (52.0) | 0.73 (0.70–0.76) | 199 (14.9) | 0.79 (0.77–0.80) | 140 (3.7) | 0.72 (0.7–0.74) | |
| Poor | 15 (34.7) | 0.24 (0.23–0.26) | 98 (19.3) | 1.39 (1.36–1.43) | 47 (3.6) | 0.83 (0.8–0.86) | |
| Body mass index‡, kg/m2 | <25 | 189 (63.9) | 319 (19.9) | 241 (4.4) | |||
| 25–30 | 227 (56.6) | 0.85 (0.83–0.87) | 473 (18.2) | 0.96 (0.95–0.97) | 279 (5.0) | 1.14 (1.12–1.16) | |
| >30 | 221 (45.8) | 0.67 (0.65–0.69) | 376 (14.4) | 0.83 (0.82–0.84) | 135 (4.1) | 0.98 (0.97–1) | |
| Missing | 13 (41.4) | 0.63 (0.59–0.68) | 24 (17.8) | 1.38 (1.34–1.42) | 11 (5.7) | 1.41 (1.35–1.48) | |
| Smoking | Not at all | 401 (50.1) | 773 (15.3) | 562 (4.6) | |||
| Occasionally | 29 (48.1) | 0.91 (0.88–0.95) | 52 (28.0) | 2 (1.96–2.04) | 16 (3.3) | 0.7 (0.66–0.74) | |
| Daily | 220 (69.1) | 2.03 (1.98–2.07) | 367 (22.7) | 1.58 (1.56–1.60) | 88 (5.2) | 1.13 (1.1–1.15) | |
| Physical activity | Active | 188 (66.8) | 256 (19.7) | 128 (5.0) | |||
| Moderate | 155 (54.0) | 0.67 (0.65–0.69) | 291 (18.2) | 1.07 (1.05–1.08) | 144 (4.3) | 0.92 (0.9–0.94) | |
| Inactive | 307 (50.0) | 0.62 (0.60–0.63) | 645 (16.1) | 0.93 (0.92–0.94) | 394 (4.6) | 1.17 (1.15–1.19) | |
All percentages were weighted using Statistics Canada’s bootstrap method, and frequencies were not weighted.
All adjusted OR reflect adjustments for all variables listed in this table and regional residence. 95% CI are not rounded to the first decimal place to show that point estimates are centred in the intervals;
Married/common-law and widowed/separated/divorced were combined, and the reported OR is for the combined group;
A ‘missing’ category was added for the income and body mass index variables
DISCUSSION
Treatment of hypertension is highly effective at preventing cardiovascular events. In the present study, we found that 12.7% of hypertensive adult Canadians were not taking antihypertensive drug therapy. We found several characteristics of those less likely to be taking antihypertensive therapy. In particular, approximately one-half of those younger than 40 years of age were not taking antihypertensive agents. In addition, in all age categories, male respondents and those who reported no physician consultations in the previous year, excellent self-rated health and daily smoking were less likely to report pharmacotherapy. Physicians need to be more alert to hypertensive Canadians with these characteristics to ensure that they are appropriately treated.
Although several surveys have examined respondent characteristics associated with lack of treatment or control of hypertension, there are no consistent predictors of a lack of treatment other than age, sex and region of the world studied (12–16). The inconsistent findings may relate to unique aspects of health systems and hypertension programs in different countries. In the Canadian Heart Health Surveys (1985 to 1992) and in surveys from other countries, younger, aware hypertensive adults were also less likely to be treated than those who were older. There was also a sex-related ‘gap’, with fewer men being aware of the diagnosis or being treated for hypertension (17–19). Since the Canadian Heart Health Surveys, there have been large increases in the diagnosis and treatment of hypertension and a closing of the sex-related ‘gap’ in Canada (6). Similar to Canada, national programs implemented in other countries to improve hypertension treatment and control have resulted in changes in the characteristics of respondents who are being treated (18,19). A particular strength of our study is that it provides contemporary Canadian data on which to develop interventions to improve treatment.
Limitations
There are some limitations to the present study. The hypertension diagnosis and treatment measures were self-reported and not verified. Thus, there is likely to be some misclassification of both the presence of hypertension and drug treatment. Furthermore, certain groups, such as military personnel, those living on a reserve and who are institutionalized were not sampled by the CCHS, and, thus, our results may not pertain to these groups. Nevertheless, the results of the present study are likely to be representative of aware hypertensive Canadians, because the CCHS is specifically designed to provide data that are representative of the Canadian population. It is also not possible to determine the appropriateness of antihypertensive drug therapy in this database. Some patients may have hypertension treated with lifestyle modification rather than with drug therapy. However, few hypertensive Canadians have indicated that they are making or have made lifestyle changes in past surveys (20,21), and the use of pharmacotherapy remains a key predictor of blood pressure control (22).
Because it is possible that a proportion of those with a previous diagnosis of hypertension no longer have the condition (and, thus, are not in need of drug therapy), respondents who reported that they had a previous diagnosis of hypertension but no current diagnosis and no current drug treatment were excluded from our analysis. It is also likely that drug therapy is not being prescribed to some hypertensive Canadians who are at low overall cardiovascular risk (23). Low cardiovascular risk is associated with younger age and excellent health, both of which were associated with a reduced likelihood of reporting antihypertensive therapy in our study. Nevertheless, a large proportion of hypertensive Canadians younger than 40 years of age who reported one or more other cardiovascular risk were not treated with antihypertensive drugs. Continued smoking is one of the most significant of cardiovascular risks and was associated with a reduced likelihood of antihypertensive therapy, regardless of age. The lack of increased drug treatment with the number of cardiovascular risks is of particular concern. It is essential that future research and surveys in this area incorporate blood pressure measurements, the assessment of lifestyle changes and indexes of cardiovascular risk to permit a more comprehensive assessment of the appropriateness of not taking antihypertensive therapy among selected patients with high blood pressure.
CONCLUSIONS
Based on our results, educational programs aimed at patients with hypertension and highlighting the importance of regular physician assessments may result in more patients being treated with drug therapy. It is recommended that even hypertensive patients who are making lifestyle changes have regular follow-up (23), because they may be in need of pharmacotherapy. However, the increasing shortage of family physicians may increase the problem of hypertensive Canadians not having regular visits to assess blood pressure. This is an issue the provincial governments need to address. Finally, based on our results, education programs to emphasize the need for pharmacological therapy of hypertension in higher-risk younger Canadians may also be warranted.
REFERENCES
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–10. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Geneva, Switzerland: World Health Organization; 2002. The World Health Report 2002. [Google Scholar]
- 4.Smith SC, Jr, Blair SN, Criqui MH, et al. Preventing heart attack and death in patients with coronary disease. Circulation. 1995;92:2–4. [PubMed] [Google Scholar]
- 5.Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–9. doi: 10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- 6.Onysko J, Maxwell C, Eliasziw M, Zhang JX, Johansen H, Campbell NR, Canadian Hypertension Education Program Large increases in hypertension diagnosis and treatment in Canada after a healthcare professional education program. Hypertension. 2006;48:853–60. doi: 10.1161/01.HYP.0000242335.32890.c6. [DOI] [PubMed] [Google Scholar]
- 7.Campbell NR, McAlister FA, Brant R, et al. Canadian Hypertension Education Process and Evaluation Committee Temporal trends in antihypertensive drug prescriptions in Canada before and after introduction of the Canadian Hypertension Education Program. J Hypertens. 2003;21:1591–7. doi: 10.1097/00004872-200308000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Campbell NR, Tu K, Brant R, Duong-Hua M, McAlister FA, Canadian Hypertension Education Program Outcomes Research Task Force The impact of the Canadian Hypertension Education Program on antihypertensive prescribing trends. Hypertension. 2006;47:22–8. doi: 10.1161/01.HYP.0000196269.98463.fd. [DOI] [PubMed] [Google Scholar]
- 9.Neutel CI, Campbell NR. Antihypertensive medication use by recently diagnosed hypertensive Canadians. Can J Cardiol. 2007;23:561–5. doi: 10.1016/s0828-282x(07)70801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tu K, Campbell NR, Duong-Hua M, McAlister FA. Hypertension management in the elderly has improved: Ontario prescribing trends, 1994 to 2002. Hypertension. 2005;45:1113–8. doi: 10.1161/01.HYP.0000164573.01177.95. [DOI] [PubMed] [Google Scholar]
- 11.Tobe SW, Touyz RM, Campbell NR, Canadian Hypertension Education Program The Canadian Hypertension Education Program – a unique Canadian knowledge translation program. Can J Cardiol. 2007;23:551–5. doi: 10.1016/s0828-282x(07)70799-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang YR, Alexander GC, Stafford RS.Outpatient hypertension treatment, treatment intensification, and control in western Europe and the United States Arch Intern Med 2007167141–7.(Erratum in 2007;167:648). [DOI] [PubMed] [Google Scholar]
- 13.Bleich SN, Cutler DM, Adams AS, Lozano R, Murray CJ. Impact of insurance and supply of health professionals on coverage of treatment for hypertension in Mexico: Population based study. BMJ. 2007;335:875–83. doi: 10.1136/bmj.39350.617616.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: A systematic review. J Hypertens. 2004;22:11–9. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Greenberg JD, Tiwari A, Rajan M, Miller D, Natarajan S, Pogach L. Determinants of sustained uncontrolled blood pressure in a national cohort of persons with diabetes. Am J Hypertens. 2006;19:161–9. doi: 10.1016/j.amjhyper.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 16.Agyemang C, van Valkengoed I, Koopmans R, Stronks K. Factors associated with hypertension awareness, treatment and control among ethnic groups in Amsterdam, the Netherlands: The SUNSET study. J Hum Hypertens. 2006;20:874–81. doi: 10.1038/sj.jhh.1002073. [DOI] [PubMed] [Google Scholar]
- 17.Joffres MR, Ghadirian P, Fodor JG, Petrasovits A, Chockalingam A, Hamet P. Awareness, treatment, and control of hypertension in Canada. Am J Hypertens. 1997;10:1097–102. doi: 10.1016/s0895-7061(97)00224-0. [DOI] [PubMed] [Google Scholar]
- 18.Primatesta P, Poulter NR. Improvement in hypertension management in England: Results from the Health Survey for England 2003. J Hypertens. 2006;24:1187–92. doi: 10.1097/01.hjh.0000226210.95936.bc. [DOI] [PubMed] [Google Scholar]
- 19.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 20.Neutel CI, Campbell NR, Canadian Hypertension Society Changes in lifestyle after hypertension diagnosis in Canada. Can J Cardiol. 2008;24:199–204. doi: 10.1016/s0828-282x(08)70584-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G. Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1997–2005. [PMC free article] [PubMed] [Google Scholar]
- 22.Wolf HK, Andreou P, Bata IR, et al. Trends in the prevalence and treatment of hypertension in Halifax County from 1985 to 1995. CMAJ. 1999;161:699–704. [PMC free article] [PubMed] [Google Scholar]
- 23.Khan NA, Hemmelgarn B, Padwal R, et al. Canadian Hypertension Education Program The 2007 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 2 – therapy. Can J Cardiol. 2007;23:539–50. doi: 10.1016/s0828-282x(07)70798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]