Abstract
BACKGROUND:
In 1999, the Canadian Hypertension Education Program (CHEP) was launched to develop and implement evidence-based hypertension guidelines.
OBJECTIVES:
To determine temporal trends in antihypertensive drug prescribing and physician visits for hypertension in Canada, and correlate these trends with CHEP recommendations.
METHODS:
Longitudinal drug data (Intercontinental Medical Statistics [IMS] CompuScript database; IMS Health Canada) were used to examine prescriptions over an 11-year period (1996 to 2006) for five major cardiovascular drug classes. The IMS Canadian Disease and Therapeutic Index database was used to determine trends in physician office visits for hypertension.
RESULTS:
Prescriptions for antihypertensive agents increased significantly over the 11-year period (4054% for angiotensin receptor blockers, 127% for thiazide diuretics, 108% for angiotensin-converting enzyme inhibitors, 87% for beta-blockers and 55% for calcium channel blockers). Time series analyses demonstrated increases in the growth rate for all drug classes, with the greatest annual change in prescriptions occurring during the 1999 to 2002 time period (except in angiotensin receptor blockers). An increase in prescriptions for fixed-dose combination products occurred, which was temporally related to the change in CHEP recommendations encouraging their use in 2001. The proportion of physician office visits for hypertension increased significantly from 4.9% in 1995 to 6.8% in 2005 (P<0.001).
CONCLUSIONS:
The largest increase in antihypertensive drug prescribing occurred in the period immediately following implementation of CHEP (1999 to 2002). Although prescribing rates are still increasing, the rate of change has decreased, suggesting that the treatment market for hypertension may be becoming saturated. The impact of these changes on blood pressure control and clinical outcomes remains to be determined.
Keywords: Drug therapy, Hypertension
Abstract
HISTORIQUE :
En 1999, le Programme éducatif canadien sur l’hypertension (PECH) était créé pour élaborer et implanter des lignes directrices probantes sur l’hypertension.
OBJECTIFS :
Déterminer les tendances temporelles de prescription d’antihypertenseurs et de consultations chez les médecins au Canada et les corréler avec les recommandations du PECH.
MÉTHODOLOGIE :
Les données longitudinales sur les médicaments (bases de données CompuScript d’IMS, IMS Health Canada) ont permis d’examiner les prescriptions sur une période de 11 ans (de 1996 à 2006) à l’égard de cinq grandes catégories de médicaments cardiovasculaires. La base de données de l’IMS Canadian Disease and Therapeutic Index a été utilisée pour déterminer les tendances des consultations au cabinet du médecin en raison de l’hypertension.
RÉSULTATS :
Les prescriptions d’antihypertenseurs ont augmenté considérablement au cours de la période de 11 ans (4 054 % pour les antagonistes des récepteurs de l’angiotensine, 127 % pour les diurétiques thiazidiques, 108 % pour les inhibiteurs de l’enzyme de conversion de l’angiotensine, 87 % pour les bétabloquants et 55 % pour les inhibiteurs calciques). Des analyses de séries chronologiques ont démontré des augmentations du taux de croissance de toutes les classes de médicaments, le changement annuel le plus important en matière de prescription s’étant observé entre 1999 et 2002 (sauf pour les antagonistes des récepteurs de l’angiotensine). On a constaté une augmentation des prescriptions de polythérapies à dose fixe, reliée dans le temps à la modification des recommandations du PECH favorisant leur utilisation en 2001. La proportion de consultations au cabinet du médecin en raison de l’hypertension a connu une hausse significative de 4,9 % en 1995 à 6,8 % en 2005 (P<0,001).
CONCLUSIONS :
La plus forte augmentation de prescription d’antihypertenseurs s’est produite pendant la période suivant immédiatement l’implantation du PECH (1999 à 2002). Bien que les taux de prescription augmentent encore, le taux de modification a diminué, ce qui laisse supposer la saturation du marché des traitements de l’hypertension. Il reste à déterminer les répercussions de ces changements sur le contrôle de la tension artérielle et les issues cliniques.
Hypertension affects approximately 25% of adult Canadians (1) and remains the most important modifiable risk factor for vascular morbidity and mortality (2–4). Pharmacotherapy is an important aspect of hypertension management. The Canadian Hypertension Education Program (CHEP) is a national knowledge translation strategy that provides physicians with annual evidence-based recommendations on the diagnosis and treatment of hypertension, with the goal of improving hypertension treatment and control (5). CHEP also provides a comprehensive dissemination and implementation program for these recommendations.
Since CHEP’s inception in 1999, its recommendations have evolved over time as new evidence has become available. For example, with the realization that almost two-thirds of patients in antihypertensive trials required multiple agents to achieve blood pressure targets (6–8) and the evidence that combination tablets improved patient adherence to therapy, the use of combination drugs in the management of hypertension was first recommended by CHEP in 2001 (9). The intent of CHEP recommendations is to guide hypertension therapy. However, an important component of CHEP includes an evaluation of the impact and uptake of their recommendations.
Using a national database of prescription drugs and physician office visits, we sought to determine temporal trends in antihypertensive drug prescribing and office visits for hypertension in Canada over an 11-year period, and to correlate these trends with the CHEP recommendations. In addition to examining total antihypertensive drugs and each of the five major classes, we also examined trends in the prescribing of combination medications, both before and after their use was recommended by CHEP.
METHODS
Data sources
The Intercontinental Medical Statistics (IMS) CompuScript database (IMS Health, Canada) was used to obtain cardiovascular drug dispensing information from January 1, 1996, to December 31, 2006. IMS Health Canada compiles monthly dispensing records from a nationally representative sample of over 4700 pharmacies (two-thirds of all Canadian retail pharmacies). Pharmacies (the ‘sample’) are stratified by province, the type of outlet (independent of affiliation with a chain) and size (small or large). Based on standardized sampling weights, monthly estimates for the dispensing of individual drugs are calculated for each province, with provincial totals combined to provide national estimates.
IMS CompuScript data are not patient-specific; however, the data provided on prescription volume and class can be used to estimate trends in drug use at a provincial and national level. It also has the advantage over most provincial medication databases in that it is not restricted to patients older than 65 years of age. IMS CompuScript data have been used in the past as a valuable source of information for describing trends in drug use over time (10,11).
Drug use and physician visits for hypertension
The numbers of prescriptions dispensed for all antihypertensive agents between January 1, 1996, and December 31, 2006, for each of the five major drug classes (thiazide diuretics, beta-blockers, calcium channel blockers, angiotensin-converting enzyme [ACE] inhibitors and angiotensin receptor blockers [ARBs]) were examined (Table 1). All fixed-dose combinations were included in each of the relevant classes when class-specific rates were calculated, but they were counted only once for estimates of total antihypertensive prescribing. For example, a fixed-dose combination containing a thiazide and an ACE inhibitor were included in both the thiazide and the ACE inhibitor classes for class-specific rates, but were counted only once when ‘total’ antihypertensive prescribing rates were examined. Nitrate formulations were used as ‘control’ drugs to examine trends in the use of other cardiovascular treatments for conditions other than hypertension.
TABLE 1.
List of drugs contained within each class
| Class | Drugs |
|---|---|
| Thiazide diuretics | Hydrochlorothiazide, metolazone, chlorthalidone, bendroflumethiazide, indapamide, and combinations with potassium-sparing diuretics, angiotensin-converting enzyme inhibitors, beta-blockers and angiotensin receptor blockers |
| Beta-blockers | Metoprolol, atenolol, bisoprolol, acebutolol, propranolol, sotalol, nadolol, pindolol, labetalol, timolol, oxprenolol and combinations with thiazide diuretics |
| Angiotensin-converting enzyme inhibitors | Ramipril, enalapril, lisinopril, fosinopril, quinapril, perindopril, cilazapril, captopril, benazepril, trandolapril, and combinations with thiazide diuretics and calcium channel blockers |
| Calcium channel blockers | Amlodipine, nifedipine, felodipine, nimodipine, nicardipine, diltiazem and verapamil |
| Angiotensin receptor blockers | Irbesartan, candesartan, losartan, valsartan, telmisartan, eprosartan and combinations with thiazide diuretics |
| Combination drugs | Potassium-sparing (triamterene, amiloride, spironolactone), beta-blockers (atenolol, pindolol, propranolol, timolol), all angiotensin receptor blockers (valsartan, irbesartan, losartan, candesartan, cilexetil, telmisartan, eprosartan) and angiotensin-converting enzyme inhibitors (lisinopril, quinapril, perindopril, cilazapril, enalapril, ramipril) combined with any thiazide diuretic |
| Nitrate preparations | Nitroglycerine, isosorbide-5-mononitrate, isosorbide dinitrate, pentaerythrityl tetranitrate, amyl nitrite |
The IMS Canadian Disease and Therapeutic Index database was used to determine trends in physician office visits for hypertension from January 1, 1995, to December 31, 2005. Similar to the IMS CompuScript database, the IMS Canadian Disease and Therapeutic Index database compiles quarterly records of the primary indication for an office visit from a nationally representative random sample of Canadian office-based physicians, stratified by geographic region and representing all major specialties. Based on standardized sampling weights, yearly estimates for the number of physician office visits for hypertension are calculated to obtain national estimates.
Data analysis
Population-adjusted prescription rates were calculated separately for the five antihypertensive drug classes, as well as for total antihypertensive prescriptions, using the Canadian population 20 years of age and older from Statistics Canada’s census data, with quarterly population estimates as the standard. Time series models were applied to logarithmically transformed prescription numbers to derive the smooth curves on the graphs, as well as the annualized prescription changes. Three time periods were constructed for comparison of the annualized prescription changes, corresponding to the time period before the introduction of CHEP (1996 to 1998) and the two time periods after the introduction of CHEP (1999 to 2002 and 2003 to 2006). The curves in the graphs represent the predicted values from the model. The annualized prescription changes were calculated from linear combinations of the model parameters. All of the models included systematic components for periodic calendar variation plus a segmented ‘switching’ linear regression (switching at January 1999). Residual errors were modelled as autoregressive moving average processes. Graphical inspection of residuals revealed no systematic departures from assumptions except for prescriptions for ARBs. A similar analysis was conducted to examine trends in prescriptions specifically for fixed-dose combination drugs. In the present analysis, the time periods for comparison included 1996 to 2000 and 2001 to 2006 to correspond with the change in the CHEP recommendations as of January 2001 endorsing the use of combination antihypertensive tablets.
Trends in physician office-based visits for hypertension for all ages from January 1, 1995, to December 31, 2005, were also examined. The proportion of physician office-based visits for hypertension was calculated by dividing the number of physician office-based visits for hypertension by the total number of physician office-based visits. All analyses were conducted using SAS (version 9.1; SAS Institute, USA).
RESULTS
Between January 1996 and December 2006, an estimated 540 million antihypertensive prescriptions were filled in Canada. After adjusting for increases in the population 20 years of age and older, the rate of antihypertensive prescriptions per 10,000 Canadian adults increased by 106.8% in all classes of drugs over this 11-year period, with class-specific annual increases of 4054% for ARBs, 127% for thiazide diuretics, 108% for ACE inhibitors, 87% for beta-blockers and 55% for calcium channel blockers.
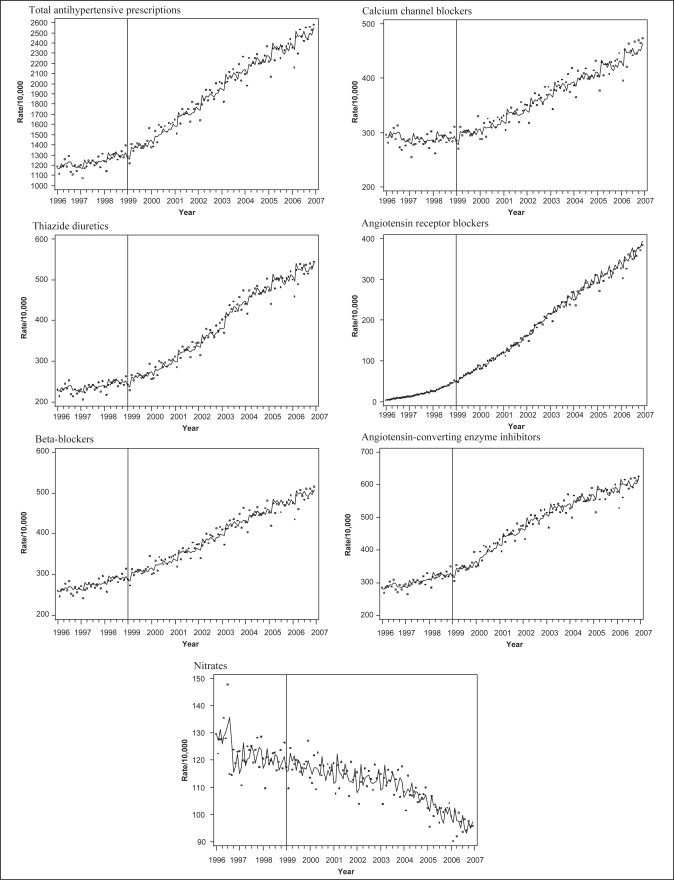
Figure 1 confirms the increase in antihypertensive prescriptions for all classes over the 11-year period. It includes population-adjusted prescription rates presented as monthly data points, as well as a line derived from nonparametric smoothing for all antihypertensive prescriptions and each of the five classes separately. In contrast, prescription rates for nitrates, the ‘control’ drug for comparison, declined by 24% over this time.
Figure 1).
Trends in prescriptions for antihypertensive drugs in Canadians ≥20 years of age, January 1996 to December 2006. Derived from the IMS CompuScript database (IMS Health Canada)
Time series analyses substantiate the statistically significant and considerable increases in the prescription growth rates for all drug classes (Table 2). Except for ARBs (which were introduced into the market in 1995 and, thus, demonstrated very large relative but small absolute changes in prescribing rates in their first few years of availability), the greatest annual change in prescriptions occurred during 1999 to 2002, with approximately a twofold increase for most classes, except for thiazide diuretics, which increased threefold. Although there was an increase in antihypertensive prescribing rates for all drug classes over the entire 11-year study (Figure 1), the rate of annual increase during the last period (2003 to 2006) was less pronounced compared with 1999 to 2002 for all drug classes (Table 3). Of note, the decline in the rate of increase in ARB prescriptions for the study periods was related to the relatively small number of prescriptions in the earlier years and the rapidly changing rates of use over time.
TABLE 2.
Per cent annual changes in prescription rates of antihypertensive drugs, 1996 to 1998, 1999 to 2002 and 2003 to 2006
| Drug | Annualized changes in prescriptions (%)
|
||
|---|---|---|---|
| 1996–1998 | 1999–2002 | 2003–2006 | |
| Total antihypertensive drugs | 4.6 | 10.8 | 6.1 |
| Thiazide diuretics | 3.9 | 12.7 | 7.7 |
| ACE inhibitors | 5.8 | 11.5 | 4.5 |
| Angiotensin receptor blockers | 101.9 | 36.6 | 14.7 |
| Beta-blockers | 4.8 | 8.4 | 5.6 |
| Calcium channel blockers | 0.5 | 6.6 | 5.1 |
ACE Angiotensin-converting enzyme
TABLE 3.
Per cent absolute annual changes in prescription rates for antihypertensive drugs, comparison of three time periods
| Drug | Absolute annual changes in prescription rates, % (95% CI)
|
||
|---|---|---|---|
| 1999–2002 versus 1996–1998 | 2003–2006 versus 1996–1998 | 2003–2006 versus 1999–2002 | |
| Total antihypertensive | 6.4 | 1.5 | –4.7 |
| drugs | (4.0 to 8.5) | (–0.9 to 4.0) | (–7.0 to –2.4) |
| Thiazide diuretics | 8.9 | 3.9 | –5.0 |
| (4.3 to 13.5) | (–1.0 to 8.8) | (–9.6 to –0.4) | |
| Angiotensin-converting | 5.7 | –1.3 | –7.0 |
| enzyme inhibitors | (1.9 to 9.6) | (–5.4 to 2.8) | (–10.9 to –3.2) |
| Angiotensin receptor | –65.6 | –66.8 | –21.9 |
| blockers | (–109.9 to –41.4) | (–97.1 to –36.5) | (–34.6 to –13.8) |
| Beta-blockers | 3.6 | 0.8 | –2.8 |
| (1.6 to 5.6) | (–1.3 to 2.9) | (–4.8 to –0.8) | |
| Calcium channel | 6.2 | 4.7 | –1.4 |
| blockers | (3.2 to 9.2) | (1.5 to 7.9) | (–4.4 to 1.5) |
Derived from the IMS CompuScript database (IMS Health Canada)
Fixed-dose combinations
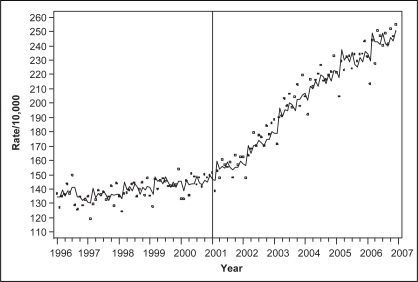
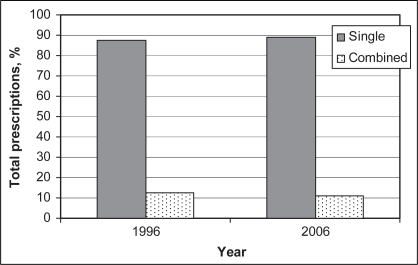
Prescribing rates for antihypertensive fixed-dose combinations also increased over the 11-year study, with an overall increase of 112.8% and an annual increase of 23.7% after adjusting for the population 20 years of age and older. The use of combination antihypertensive drugs was included in the CHEP recommendations in 2001 (12), following which there was a substantial and significant increase in prescriptions for fixed-dose combinations (Figure 2). The annualized per cent changes in prescriptions for fixed-dose combinations were 1.5% (95% CI 1.7 to 4.7) and 9.0% (95% CI 5.5 to 12.5) for the 1996 to 2000 and 2001 to 2006 periods, respectively. Time series analysis also demonstrated a significant increase in fixed-dose combination prescriptions after their use was recommended by CHEP in 2001, with an absolute annual change in prescribing rates of 7.5% (95% CI 1.9 to 11.8) for 2001 to 2006 versus 1996 to 2000. However, fixed-dose combinations still made up a minority of all antihypertensive prescriptions, ranging from 12.6% of all antihypertensive prescriptions in 1996 to 10.9% in 2006 (Figure 3).
Figure 2).
Trends in prescriptions for antihypertensive fixed-dose combinations in Canadians ≥20 years of age, January 1996 to December 2006. Derived from the IMS CompuScript database (IMS Health Canada)
Figure 3).
Proportion of antihypertensive prescriptions for single-dose and fixed-dose combinations for Canadians ≥20 years of age, 1996 and 2006. Derived from the IMS CompuScript database (IMS Health Canada)
Office visits for hypertension
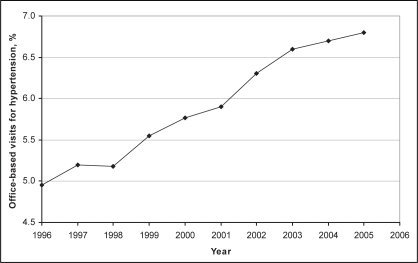
Over the 11-year study, hypertension was the leading diagnosis for physician office-based visits, accounting for 16,030,000 visits in 1999 and 21,956,210 in 2005. The proportion of physician office-based visits for hypertension increased significantly from 4.9% in 1995 to 6.8% in 2005 (χ2 test for trend P<0.001) (Figure 4). Although the proportion of office visits for hypertension increased over time, the per cent annual change in visits followed a pattern similar to that seen for the antihypertensive prescription rates. The per cent annual change in physician visits for hypertension increased after 1999, and decreased slightly in the more recent years, with a per cent annual change of 1.7% for 1995 to 1998, 4.1% for 1999 to 2002 and 2.6% for 2003 to 2005.
Figure 4).
Proportion of physician office-based visits for hypertension in Canada for all ages, January 1995 to December 2005. Derived from the Canadian Disease and Therapeutic Index, IMS Health Canada
DISCUSSION
Consistent with previous reports (13), we found large increases in anti-hypertensive drug therapy in Canada between 1996 and 2006, with the largest increases in the period immediately following the implementation of CHEP (1999 to 2002). In parallel to the increase in antihypertensive prescriptions, we also found an increase in the number of physician office-based visits for hypertension between 1996 and 2006. The greatest rise in office-based visits also coincided with the start of CHEP. Furthermore, we report an increase in prescriptions of combination antihypertensive drug products temporally associated with a change in CHEP recommendations encouraging their use in 2001.
Although clinical practice guidelines generally have a limited impact on clinical management (14), these results suggest sustained changes in clinical management (office visits and drug prescriptions) associated with the CHEP recommendation process. This sustained effect may be related to a unique feature of CHEP: it updates its recommendations on an annual basis and includes an extensive implementation program supported by national organizations representing family physicians, specialists, nurses and pharmacists (15,16).
We found that the greatest increase in prescriptions of antihypertensive drugs was experienced in 1999 to 2003. Although the rate of antihypertensive prescriptions continued to increase over the 2003 to 2006 period, their annual rate of increase has become less pronounced. A similar pattern was evident for physician office-based visits for hypertension. This may be due, in part, to ‘saturation’ of the hypertension market. Between 1999 and 2003, there was a substantial increase in the number of Canadians being treated with drug therapy, and by 2003, 85% of aware hypertensive Canadians were being treated with drug therapy (17). Furthermore, more hypertensive Canadians were being treated with two or more drugs and fewer were stopping their therapy (17,18). Recently, a hypertension survey in Ontario (19) reported that most hypertensive patients were taking antihypertensive therapy and two-thirds had their blood pressure controlled. It is encouraging that prescriptions of antihypertensive drugs continue to increase, implying that further improvements in treatment and control of hypertension are being achieved.
The increases in antihypertensive prescriptions were largest for ACE inhibitors, ARBs, thiazide diuretics and fixed-dose combinations. The increase in beta-blockers was lower than in the other classes, and may be due, in part, to the decreased prescribing of beta-blockers as first-line therapy in elderly patients – another CHEP recommendation that was first produced in 1999 (20). The increase in prescriptions of calcium channel blockers might have been dampened by the recognition of the higher cost of this therapy relative to other antihypertensive drug classes, as well as the potential concerns regarding their safety published in the mid-1990s (21).
Prescription rates for fixed-dose combinations increased substantially after 2001 and mirrored the recommendation for combination drug use in the CHEP recommendations. However, as a proportion of all antihypertensive therapy, fixed-dose combination tablets still have limited use. Prescriptions for combination drug tablets are generally less expensive than the component drugs and can improve adherence to treatment (22). Given that most patients require two or more drugs for blood pressure control, increased use of fixed-dose combinations may improve hypertension treatment and control (a hypothesis that is currently being tested in ongoing trials).
Limitations
Results of the present study should be interpreted in light of its limitations. First, the IMS CompuScript database includes total prescriptions rather than individual patient level data; therefore, it is not possible to assess trends in drug use in different patient subgroups. In addition, the data provided are not disease-specific; therefore, the extent to which changes in the prevalence of disease conditions besides hypertension might have influenced the results is unknown. Finally, while associations between the CHEP guidelines and trends in antihypertensive drug prescribing were considered, given the observational nature of the data, definitive statements about causality cannot be made.
CONCLUSIONS
We found a substantial increase in antihypertensive drug prescribing over the past decade, particularly between 1999 and 2002. Although prescribing rates are still increasing, in more recent years, the rate of change has decreased, suggesting that the treatment market for hypertension may be becoming saturated. This is further supported by recent survey data suggesting improved hypertension treatment and control, at least in Ontario. The impact of these changes in prescribing practices on blood pressure control and hypertension-related clinical outcomes remains to be determined.
REFERENCES
- 1.Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43:10–7. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB. Blood pressure as a cardiovascular risk factor: Prevention and treatment. JAMA. 1996;275:1571–6. [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies Lancet 20023601903–13.(Erratum in 2003;361:1060). [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 5.McAlister FA. The Canadian Hypertension Education Program –a unique Canadian initiative. Can J Cardiol. 2006;22:559–64. doi: 10.1016/s0828-282x(06)70277-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 7.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) JAMA. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 8.ALLHAT Officers & Coordinators. Major Outcomes in High-Risk Hypertensive Patients Randomized to Angiotensin-Converting Enzyme Inhibitor or Calcium Channel Blocker vs Diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 9.McAlister FA, Zarnke KB, Campbell NR, et al. Canadian Hypertension Recommendations Working Group The 2001 Canadian recommendations for the management of hypertension: Part two – therapy. Can J Cardiol. 2002;18:625–41. [PubMed] [Google Scholar]
- 10.Campbell NR, McAlister FA, Brant R, et al. Canadian Hypertension Education Process and Evaluation Committee Temporal trends in antihypertensive drug prescriptions in Canada before and after introduction of the Canadian Hypertension Education Program. J Hypertens. 2003;21:1591–7. doi: 10.1097/00004872-200308000-00025. [DOI] [PubMed] [Google Scholar]
- 11.Jackevicius CA, Tu K, Filate WA, Brien SE, Tu JV, Canadian Cardiovascular Outcomes Research Team Trends in cardiovascular drug utilization and drug expenditures in Canada between 1996 and 2001. Can J Cardiol. 2003;19:1359–66. [PubMed] [Google Scholar]
- 12.Canadian Hypertension Recommendations Working Group. The 2001 Canadian hypertension recommendations. What is new and what is old but still important. Can J Cardiol. 2002;18:591–603. [PubMed] [Google Scholar]
- 13.Tu K, Campbell NR, Duong-Hua M, McAlister FA. Hypertension management in the elderly has improved: Ontario prescribing trends, 1994 to 2002. Hypertension. 2005;45:1113–8. doi: 10.1161/01.HYP.0000164573.01177.95. [DOI] [PubMed] [Google Scholar]
- 14.Majumdar SR, McAlister FA, Furberg CD. From knowledge to practice in chronic cardiovascular disease: A long and winding road. J Am Coll Cardiol. 2004;43:1738–42. doi: 10.1016/j.jacc.2003.12.043. [DOI] [PubMed] [Google Scholar]
- 15.Drouin D, Campbell NR, Kaczorowski J. Implementation of recommendations on hypertension: The Canadian Hypertension Education Program. Can J Cardiol. 2006;22:595–8. doi: 10.1016/s0828-282x(06)70281-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell N, Onysko J, Canadian Hypertension Education Program; Outcomes Research Task Force The Outcomes Research Task Force and the Canadian Hypertension Education Program. Can J Cardiol. 2006;22:556–8. doi: 10.1016/s0828-282x(06)70276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onysko J, Maxwell C, Eliasziw M, Zhang JX, Johansen H, Campbell NR, Canadian Hypertension Education Program Large increases in hypertension diagnosis and treatment in Canada after a healthcare professional education program. Hypertension. 2006;48:853–60. doi: 10.1161/01.HYP.0000242335.32890.c6. [DOI] [PubMed] [Google Scholar]
- 18.Campbell NR, McAlister FA, Duong-Hua M, Tu K. Polytherapy with two or more antihypertensive drugs to lower blood pressure in elderly Ontarians. Room for improvement. Can J Cardiol. 2007;23:783–7. doi: 10.1016/s0828-282x(07)70827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leenen FH, Nwachuku CE, Black HR, et al. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research Group Clinical events in high-risk hypertensive patients randomly assigned to calcium channel blocker versus angiotensin-converting enzyme inhibitor in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension. 2006;48:374–84. doi: 10.1161/01.HYP.0000231662.77359.de. [DOI] [PubMed] [Google Scholar]
- 20.Campbell NR, Tu K, Brant R, Duong-Hua M, McAlister FA, Canadian Hypertension Education Program Outcomes Research Task Force The impact of the Canadian Hypertension Education Program on antihypertensive prescribing trends. Hypertension. 2006;47:22–8. doi: 10.1161/01.HYP.0000196269.98463.fd. [DOI] [PubMed] [Google Scholar]
- 21.Psaty BM, Heckbert SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA. 1995;274:620–5. [PubMed] [Google Scholar]
- 22.Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: A meta-analysis. Am J Med. 2007;120:713–9. doi: 10.1016/j.amjmed.2006.08.033. [DOI] [PubMed] [Google Scholar]