Abstract
The present report describes the case of an elderly woman who was admitted to the hospital with sepsis and subsequently developed a transient 2:1 atrioventricular block following administration of a low-ionic strength contrast agent for computed tomography. The block resolved after approximately 24 h and did not require a temporary pacemaker. The case identifies an unusual consequence following an anaphylactic reaction to a low-ionic strength computed tomography contrast agent and suggests the potential role of histamine release as a mechanism underlying this reaction.
Keywords: Anaphylaxis, Atrioventricular block, Computed tomography, Contrast
Abstract
Le présent rapport décrit le cas d’une dame âgée qui a été hospitalisée à cause d’une septicémie et qui a présenté un bloc auriculoventriculaire transitoire 2:1 après l’administration d’un agent de contraste à faible concentration ionique en prévision d’une tomodensitométrie. Le bloc s’est résorbé au bout d’environ 24 heures et n’a pas nécessité l’installation d’un stimulateur cardiaque temporaire. Le cas fait état d’une conséquence inhabituelle après une réaction anaphylactique à un agent de contraste à faible concentration ionique en prévision d’une tomodensitométrie et laisse supposer le rôle de la libération d’histamine comme mécanisme sousjacent de cette réaction.
The present report describes a unique response following an anaphylactic reaction to a low-ionic contrast dye used for computed tomography (CT) in a patient admitted to the hospital with sepsis. A description of the case and review of the literature is presented.
CASE PRESENTATION
A 75-year-old woman with a history of chronic obstructive pulmonary disease (COPD) was admitted to the hospital following three days of pleuritic chest pain, cough and intermittent fevers. Her baseline medications included salbutamol and ipatropium. She had had a previous skin reaction to latex but had no known drug allergies.
The initial examination revealed a febrile elderly woman in moderate respiratory distress. Respiratory examination demonstrated coarse crackles to the right base. Laboratory investigations confirmed mild leukocytosis with a predominance of neutrophils. Arterial blood gases demonstrated moderate hypoxia. Baseline cardiac enzymes were normal and her initial electrocardiogram showed normal sinus rhythm at 70 beats/min. A chest x-ray confirmed right lower-lobe pneumonia and the patient began treatment with intravenous moxifloxacin and vancomycin. She was admitted to the general medicine ward with a diagnosis of COPD exacerbation with community-acquired pneumonia.
During the next 72 h, despite administration of intravenous (IV) antibiotics, the patient continued to have intermittent fevers. Blood cultures confirmed the presence of methacillin-sensitive staphylococcus aureus and the patient was switched to IV cloxicillin and continued on moxifloxacin. A number of investigations were performed to identify the source of sepsis. Ultimately, a bone scan identified a large paraspinal abscess from T5 to T7, and a confirmatory contrast CT of the thoracic spine was recommended to identify whether the abscess was amenable to percutaneous drainage.
Unfortunately, immediately following administration of the contrast dye for the CT scan, the patient developed marked hypotension (blood pressure 80/60 mmHg), bradycardia (heart rate 40 to 45 beats/min) and laryngeal edema. She was resuscitated with IV diphenhydramine, epinephrine and methylprednisolone sodium succinate, as well as crystalloid fluids. She was intubated and transferred to the intensive care unit.
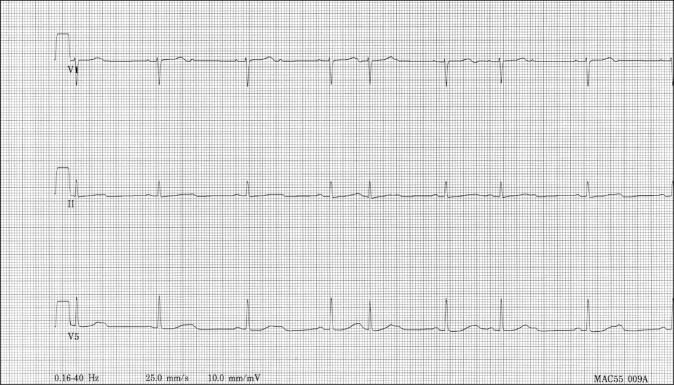
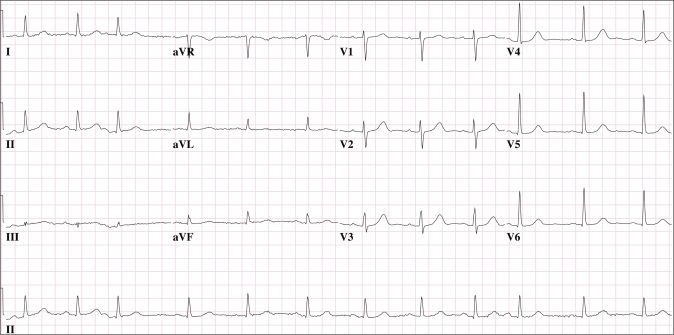
Approximately 2 h after her episode, she had an abrupt rhythm change that was noted on the cardiac monitor. Rhythm strips and a 12-lead electrocardiogram revealed a 2:1 atrioventricular block (AVB) with narrow QRS complexes and a prolonged QT interval (Figure 1). Atropine was given without an effective change in her heart rhythm. She was hemodynamically stable and, therefore, temporary pacing was deemed not necessary. The patient gradually reverted back to sinus rhythm during the next 24 h (Figure 2). She was extubated and transferred to the coronary care unit for further observation. No further episodes of AVB were noted. She completed treatment for her pneumonia and paraspinal abscess, and the rest of her hospitalization was uneventful.
Figure 1).
Rhythm strips revealing a 2:1 atrioventricular block (AVB) with narrow QRS complexes and a prolonged QT interval
Figure 2).
A 12-lead electrocardiogram showing that the patient gradually reverted back to sinus rhythm within 24 h of her episode
DISCUSSION
We describe a case of transient 2:1 AVB following an anaphylactic reaction to a low-ionic CT contrast agent. Second-degree AVBs are divided into atrioventricular nodal blocks and infranodal blocks. The two types of second-degree AVBs can be differentiated by their response to atropine, which blocks vagal stimulation. If the block resolves following atropine administration, it is more suggestive of an atrioventricular nodal block, which is more sensitive to vagal stimulation. In the present case, the lack of response to atropine was more suggestive of an infranodal block.
Previous generations of ionized contrast material have been found to exert direct inhibitory action on sinoatrial automaticity and atrioventricular conductivity. This effect has been attributed to the ionic strength of the contrast material. High-osmolality compounds, such as diatrizoate, are known to increase sinus cycle length and prolong atrioventricular nodal conduction (1). In the modern era of low-osmolality radiocontrast material use, there has been only one described case (2) of transient third-degree AVB following contrast material injection. The patient had confirmed Wenckebach rhythm before the injection and the authors attributed the etiology of the abrupt rhythm change to contrast material-induced vasospasm resulting in transitory ischemia and a localized increase in endogenous adenosine.
Transient 2:1 AVBs have not been described clinically following an anaphylactic reaction to a low-ionic strength CT contrast agent. Histamine release following introduction of radiocontrast material is a well-described phenomenon that has been postulated as a possible trigger for the AVB. Heller et al (3) noted a transient release in histamine levels following antigen challenge in partially sensitized guinea pig hearts. The group was able to produce transient AVBs in six of 17 sensitized hearts. This was later supported by Felix et al (4), who produced variable AVBs in sensitized guinea pigs through direct stimulation of H1 histamine receptors. Patterson and Milne (5) described a transient 3:1 AVB in a patient who was treated with ranitidine, a known H2 histamine-receptor antagonist, following an anaphylactic reaction to latex. Other mediators such as adenosine, thromboxane A2 and leukotrienes have also been implicated, but their exact role in the production of atrioventricular blockade following anaphylaxis is unclear (3,4). The transient prolonged QT interval was also a unique finding in our patient. Possible explanations include transitory ischemia through adenosine-mediated vasospasm or a possible histamine-mediated process. It is unlikely that our patient’s flouroquinolone use was the causative agent because serial electrocardiograms before the anaphylactic event had not demonstrated any QT prolongation.
The present case highlights a unique event following an anaphylactic reaction to a CT contrast agent. It demonstrates some diagnostic tools that can be used to differentiate the types of second-degree AVBs, and supports the role of histamine as a key player in the pathway that leads to transient AVBs following anaphylaxis.
References
- 1.Niccoli L, Bellandi M, Benedini G, Cuccia C, Petroboni V, Visioli O. Iopamidol: A new contrast medium in coronary angiography. Comparison, on electrophysiological changes in man, with a commonly used contrast medium. Eur Heart J. 1983;4:280–5. doi: 10.1093/oxfordjournals.eurheartj.a061460. [DOI] [PubMed] [Google Scholar]
- 2.Brodmann M, Seinost G, Stark G, Pilger E. Aggravation of pre-existing atrioventricular block, Wenckebach type, provoked by application of x-ray contrast medium. Cardiovasc Intervent Radiol. 2006;29:1114–6. doi: 10.1007/s00270-005-0133-x. [DOI] [PubMed] [Google Scholar]
- 3.Heller LJ, Regel JE. Effect of adenosine on histamine release and atrioventricular conduction during guinea pig cardiac anaphylaxis. Circ Res. 1998;62:1147–58. doi: 10.1161/01.res.62.6.1147. [DOI] [PubMed] [Google Scholar]
- 4.Felix SB, Baumann G, Niemczyk M, et al. Effects of histamine H1- and H2-receptor antagonists on cardiovascular function during systemic anaphylaxis in guinea pigs. Agents Actions. 1991;32:245–52. doi: 10.1007/BF01980881. [DOI] [PubMed] [Google Scholar]
- 5.Patterson LJ, Milne B. Latex anaphylaxis causing heart block: Role of ranitidine. Can J Anaesth. 1999;46:776–8. doi: 10.1007/BF03013914. [DOI] [PubMed] [Google Scholar]