Abstract
Inactivated influenza virus vaccines are the primary modality used for prevention of influenza. A system of annual identification of new strains causing illnesses, selections for vaccines, chick embryo growth, inactivation, processing, packaging, distribution and usage has been in place for decades. Current vaccines contain 15 µg of the HA of an A/H1N1, A/H3N2 and B strain and are given parenterally to induce serum anti-HA antibody for prevention of subsequent infection and illness from natural influenza. Reactogenicity is low and protection among healthy older children and adults is good; protection levels are generally lower in young children and the elderly. Needs include ensuring antigenic matches of vaccine and epidemic viruses each season, enhancing immunization rates, and providing new and improved vaccines and immunization approaches for the varied populations and circumstances globally.
1. Introduction
Inactivated influenza virus vaccines (IVV) were first used for preventing influenza in humans over 60 years of age and are currently the principal modality used for that purpose. Shown in Table 1 are some of the major events in the evolution of IVV since discovery of the influenza virus. Notable are the facts that manufacturing methods and using 15 µg of the HA of each virus component in the annual vaccine have not changed in more than 25 years. During that period, the number of doses made and used annually has increased considerably. For many years, manufacturers produced about 20 million doses annually for the USA; in 2007, the number approached 120 million. While the committee for immunization practices in the USA has been particularly aggressive in broadening the recommendations for immunization with IVV, many other countries have also strengthened recommendations and increased usage. Those population groups for whom immunization is currently recommended by public health authorities in the USA are listed in Table 2 [1]. These groups are estimated to comprise about 80% of the US population. Immunization rates among each of these population groups are variable; recent estimates in the USA are 65% of elderly persons, 26 to 46% of younger persons with a high-risk condition, 13% of pregnant women, and 48% of infants [2]. This disparity between recommendations and immunizations is also true for many other countries. Considerable effort is needed before immunization rates will begin to approach immunization recommendations.
Table 1.
Major Events in the Evolution of Inactivated Influenza Virus Vaccines (IVV)
| 1935 | Growth of virus in chick embryos |
| 1937 | Protection of ferrets with IVV |
| 1943 | Protection of humans with IVV |
| 1945 | Purification and concentration |
| 1964 | Virion lysis for reducing reactogenicity |
| 1967 | Purification by zonal centrifugation |
| 1976 | Extensive studies with Swine (H1N1) vaccines |
| 1977 | Standardization for µg of HA |
| 1981 | 15 µg of each HA for inclusion |
| 1980–2008 | Broadening of recommendations and increased usage |
Table 2.
Major Groups for Whom Annual Vaccination with Inactivated Influenza Virus Vaccine is Recommended (Adapted from Ref. 1)
| • | Persons at increased risk for serious disease, hospitalization or death from influenza |
| – The elderly (≥65 years) | |
| – The very young (6–23 months) | |
| – Those with a high risk disease or condition | |
| • | Age groups with an increased likelihood of a high risk disease (ages 50–64) |
| • | Those with an increased need for medical care because of influenza (ages 2–5) |
| • | Those who could transmit influenza to persons with increased risk |
| • | Those with highest illness attack rates and who are thought to be major spreaders of influenza (ages 5–18)* |
Recently added by the USA Committee on Immunization Practices
2. The System
Influenza viruses are continuously changing antigenically. Two subtypes of influenza A (H1N1 and H3N2) have been circulating in human populations for three to four decades. Minor antigenic changes of circulating viruses (including influenza B) occur frequently (antigenic drift). Highest protection is seen when there is an identical antigenic match of the vaccine and epidemic virus HA and NA antigens. For this reason, vaccine strains are updated annually to obtain antigenic matches between the vaccine viruses and the viruses producing the subsequent epidemic. This match is achieved in many years; in many years, it is not.
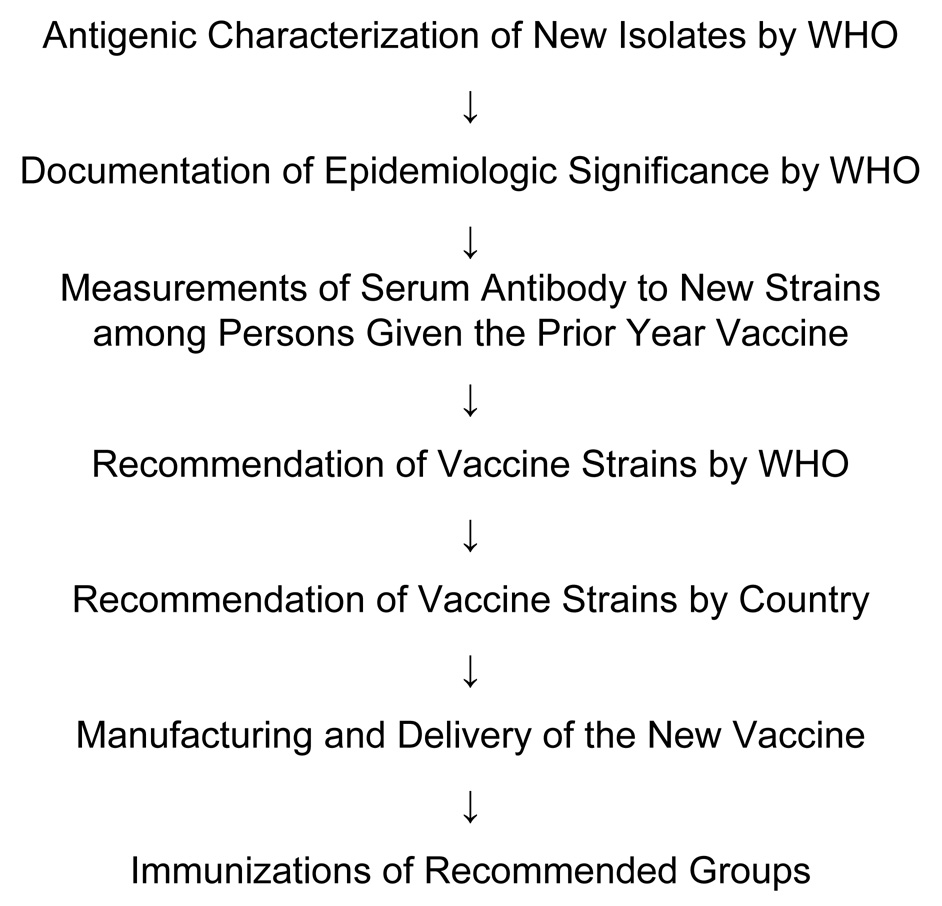
Potential vaccine viruses for a coming season are derived from a continuous worldwide surveillance for influenza viruses conducted by the World Health Organization (WHO). The annual sequence of events leading to pre-epidemic immunizations is shown in Figure 1. Separate recommendations are made annually by the WHO for the Northern Hemisphere and the Southern Hemisphere. Many months are required for manufacturing and delivery to vaccination sites. This requirement impairs selections for an antigenic match of vaccine and epidemic virus; a shortening would improve the likelihood of a perfect match.
Figure 1.
Sequence of Annual Events for Inactivated Influenza Virus Vaccines
3. The Product
The WHO lists more than 30 manufacturers of influenza vaccine globally. Some prepare and distribute whole virus vaccines but the largest quantity for the annual supply is prepared by companies who only make split product or subunit vaccine. Chick embryos are used for virus production; an inactivation process and a degree of purification for removing adventitial egg and virion material are standard. These processes have considerably reduced the reactogenicity of IVV.
A report of arm discomfort, usually mild and of short duration, occurs in 25 to 50% of vaccinated persons given purified vaccine and some will have accompanying erythema and swelling for one to three days. An occasional person will report systemic symptoms after vaccination but frequencies with most vaccines are currently low. Whole virus vaccines are probably more reactogenic than subunit vaccines, particularly among young children, although this is not well documented for vaccines of similar HA content and purity.
4. Immune Responses
A recent example of serum hemagglutination-inhibition antibody (HAI) responses to the vaccine virus among three major age groups is shown in Table 3. Responses are generally good but are frequently lower among the elderly and young children. A number of variables affect serum antibody responses including vaccine formulation, subject age, immunocompetence, prior antigenic priming and assay method used. Considerable variation in test results occurs between vaccines, years, different populations and laboratories; nevertheless, patterns of responses tend to be similar.
Table 3.
Serum Hemagglutination-Inhibition Antibody Responses to Inactivated Influenza Virus Vaccines by Age of Vaccinees*
| GMTa | % ≥40b | |||||
|---|---|---|---|---|---|---|
| Vaccine Virus | Age Gp (N) | % Rise | PreVac | PostVac | PreVac | PostVac |
| A/Soloman Islands/03/06 (H1N1) | Adults (24) | 52 | 92 | 1248 | 81 | 100 |
| Elderly (24) | 92 | 14 | 279 | 38 | 100 | |
| Children (29)c | 96 | 6 | 129 | 8 | 63 | |
| A/Wisconsin/67/05 (H3N2) | Adults | 50 | 95 | 457 | 79 | 100 |
| Elderly | 54 | 66 | 267 | 58 | 100 | |
| Children | 86 | 8 | 48 | 17 | 69 | |
| B/Malaysia/2506/04 | Adults | 54 | 27 | 220 | 46 | 100 |
| Elderly | 42 | 30 | 82 | 54 | 88 | |
| Children | 72 | 8 | 65 | 14 | 72 | |
Reciprocal of geometric mean titer pre and postvaccination
Percent with titer ≥1:40 pre and postvaccination
Result after two doses a month apart
Data from Vaccine Responses, Zhiping Ye, M.D., Ph.D., FDA, http://www.fda.gov/ohrms/dockets/ac/08/slides/2008-4348S1and2-00-index.html
There is no serum antibody level for a vaccine to induce that will ensure protective immunity but regulatory authorities have established guidelines of response “acceptability.” Those most commonly used are the European guidelines for response frequencies, mean response titers, and percent ≥1:40 in serum HAI tests for adults and the elderly [3]. The basis for using HAI results in this way comes from repeated demonstrations that the serum HAI titer correlates inversely with frequency of influenza illnesses among vaccinated persons [4].
Limited assessments of T cell mediated immune (CMI) responses in humans have been made but induction of CMI responses by IVV have been clearly documented and data supporting a value for humans of these responses is emerging [5].
5. Efficacy and Effectiveness
Protective efficacy of IVV against infection-proven illnesses has been confirmed in numerous studies of both older and newer vaccines. Efficacy has varied between epidemics as determined by antigenic match of vaccine and epidemic viruses, attack rate in the epidemic and methods used for assessing protection. Studies in the American military over decades have regularly confirmed protection by IVV [6]. These and similar studies in other healthy adult populations are the source of the frequent statement that IVV prevents 70 to 90% of influenza-specific illnesses when the vaccine and epidemic viral antigens match and that protection is lower when there is a mismatch. Although induction of protection by IVV has been clearly documented among vaccinated young children and the elderly, the level of protection tends to be lower than among healthy adults [7–12]. This is considered to be at least partly because of lower immune responses in these groups. The only randomized controlled study among older persons (≥60 years) reported a 33% reduction in influenza-like illness and a 56% reduction in serologically-confirmed illness [8].
Effectiveness assessments for IVV employ database analyses of outcomes thought to be attributable to influenza. These studies have regularly shown reductions among vaccinated persons that include respiratory illness, absenteeism, physician visits due to respiratory illness, hospitalizations for influenza-pneumonia and death. The level of protection induced by IVV tends to be less than for studies of efficacy because other infections and other life events are causing the same outcomes during the influenza epidemic period and IVV only prevents the portion caused by an influenza virus. A recent controversy regarding mortality benefits of IVV among the elderly has emerged where benefits for mortality reported in some effectiveness studies is reportedly biased in favor of IVV because of exclusion of frail elderly [13]. Some examples of both efficacy and effectiveness of IVV are shown in Table 4.
Table 4.
Efficacy and Effectiveness of Inactivated Influenza Virus Vaccines
| Age Group | Study Type (Ref) | N | Percent Reduction | |
|---|---|---|---|---|
| Adults | Efficacy (R,DB,PC)a (14) | ~2000/yr (~80% adult) | Culture pos illness | |
| A/H1N1 yrs | 79,74 | |||
| A/H3N2 yrs | 71,79 | |||
| Seroconversion | ||||
| A/H1N1 yrs | 55,79 | |||
| A/H3N2 yrs | 71.75 | |||
| Effectiveness (R,DB,PC)a (15) | 849 | URIb | 25 | |
| URI Absenteeism | 43 | |||
| URI Physician Visits | 44 | |||
| Elderly | Efficacy (R,PC)a (8) | 1838 | Influenza & Seroconversion | 58 |
| Effectiveness (database source) (16) | 713, 872 (person seasons over 10 yrs) | P-I Hospitalizations | 27 | |
| All Causes Deaths | 48 | |||
| Children | Efficacyc (11) | 1325 | Influenza A or B infection or illness | 63 |
R = randomized, DB = double blind, PC = placebo controlled
URI = Upper respiratory illness
Mean of five studies for <9 years
6. Problems and Prospects
There is a need to improve IVV and vaccinations. Some prospects for improvement are shown in Table 5. Alternative substrates and methods of production may contribute to shortening the time from strain selection to vaccine availability; they are not constrained by egg production and availability. This will be true for cell culture and rDNA-produced vaccines which focus on eliciting serum anti-HA antibody, the current required response from vaccination. While HA peptide epitope and DNA vaccines have been developed to induce anti-HA responses, none are currently slated for production on a global scale; however, each may be of value for inducing alternative immune responses.
Table 5.
Prospects for Improvement of Inactivated Influenza Virus Vaccines & Vaccinations
| • | Alternative Production Methods |
| – Cell-culture based vaccines | |
| – rDNA-produced vaccines | |
| – Peptide epitope and DNA vaccines | |
| • | Increased Immune Responses (anti-HA) |
| – Increased dosage | |
| – Adjuvant addition | |
| – Mucosal administration for increased antibody in secretions | |
| • | Broadened Immune Responses |
| – Ensure anti-NA antibody (serum and secretions) | |
| – Ensure induction and maintenance of CMI | |
| – Induce anti-M2 antibody | |
| • | Improve acceptability/delivery |
| – Intranasal/aerosol delivery | |
| – Transdermal, sublingual | |
| – Other methods | |
| • | Population-specific vaccines/regimens |
| – The very young and elderly | |
| – The immunocompromised | |
| – Vaccine combined with other preventives |
6.1 Immune Responses
The numerous and varied studies of influenza viruses, antigens and immune responses to infection and vaccinations in animals and humans have provided an information base for rational development of improved immune responses to improve protection against influenza. While this is a need for some populations, particularly the elderly, improvement is desirable for all persons. The varied, and sometimes low, efficacy from IVV indicates deficiencies in current vaccines and their usage. The need for an antigenic match of vaccine and epidemic strains has been noted earlier. Many other variables influence the degree of efficacy in a given study, including the attack rate, clinical definition of influenza, and the varying sensitivity of the methods used for identifying infection and illness.
Serum anti-HA antibody is the most consistent correlate of immunity to influenza; moreover, available information indicates it is the primary mediator of immunity to infection [4]. While there is no level of antibody that ensures protection, the higher the titer, the greater the protection; therefore, improving the magnitude and duration of this response is desirable. It is established that increasing vaccine dosage increases the serum anti-HA antibody response. While the current 15 µg per HA dosage induces responses in most persons, it has been shown that further increases in dosage will induce further increases in responses; moreover, increases have occurred without a significant increase in reactogenicity. A remarkable demonstration of this was provided with a zonal centrifuged whole virus vaccine of an A/H2N2 strain 40 years ago. An increase in antigen dosage from 300 to 4800 CCA1 in healthy primed adults increased serum HAI antibody increases from seven to 35 fold [17]. Notable is that no plateau of the antibody response was reached. A later study with a purified HA vaccine from an A/H1N1 virus given over a range of 15 to 405 µg of the HA found an increase of 16 to 35 fold in serum HAI titers for subjects with a low prevaccination titer and 3 to 7 fold among those with high pretiters [18]. Neutralizing antibody (neut) titers increased from 67 to 399 fold among those with low and three to 16 fold among those with high pretiters. A plateau for serum HAI titer occurred at about 1:250 but no plateau was seen in neut titers. The same vaccine given as 15 to 135 µg HA to elderly persons increased serum HAI titers 1.1 to 5.3 fold and neut titers 1.2 to 6.1 fold [19]. As noted recently, a Sigmoid curve with a plateau seems likely for serum anti-HA responses to increasing dosages of HA; however, the variables that define the maximal response plateau for different vaccines in different populations using different antibody test procedures have not been identified [20]. While such data could aid our understanding, it is more important to determine the consistency of increasing protection against influenza with increasing anti-HA antibody titers. In an efficacy trial with an A/H3N2 zonal centrifuged vaccine, an unprimed adult population developed a 14 fold increase in HAI titers from a 300 CCA dosage and a 25 fold increase from 3000 CCA. The 300 CCA vaccine prevented 24% of cases of febrile respiratory illness during the subsequent epidemic while the 3000 CCA vaccine prevented 71% [21,22].
An alternative to dosage for increasing serum anti-HA responses is use of adjuvants. Mineral oil adjuvants were very well established as a means for increasing responses to vaccines in the 1950s and 1960s [23]. Usage ceased because of reactogenicity and concern for cancer induction. Alum adjuvants have been variable in value but MF59 adjuvant has regularly induced increases in antibody tiers and still newer adjuvants are promising [24].
While induction of serum anti-HA is the primary goal of vaccination with IVV, other modalities for mediating immunity are desirable for induction and can increase the immunity to vaccine-related strains as well as broaden the immunity to antigenic variants. These modalities include optimizing anti-HA antibody in respiratory secretions by enhancing IgA antibody concentrations, optimizing anti-NA antibody in serum and secretions, optimizing CMI, and inducing anti-M2 antibody. All of these modalities have been shown to convey a degree of immunity to influenza in animals or humans and M2 antibody and CMI are cross-reactive to all type A and all type B virus strains.
6.2 Population-Specific Vaccinations
While better induction of immune responses than has occurred with current IVV is highly desirable, a focus on improved delivery and population-specific vaccines is also highly desirable. Parenteral delivery by needle and syringe is a significant impairment to increased immunizations with IVV. Alternative methods for parenteral delivery such as new devices and transdermal delivery could improve parenteral delivery. Adding intranasal or aerosol administration could ensure optimal immune responses at the respiratory mucosal surface where infection occurs: moreover, the route could provide the potential for full vaccination without using the parenteral route. Surveys have indicated a preference by subjects for intranasal immunization when both intranasal and parenteral immunizations were available. Another potential mucosal route proposed recently is sublingual immunization [25].
Only one type of IVV and one dosage is manufactured annually with lower volumes recommended for young children to avoid significant reactogenicity. This “one vaccine fits all” is an outmoded concept. Better and more acceptable vaccines are needed for the very young and the elderly. The addition of the live cold-adapted vaccine given by the nasal route represents one alternative that should facilitate immunizations, particularly among children [26]. The increasing population of frail elderly and immunocompromised persons in western societies needs to be addressed with vaccine development. For each of these needs and opportunities, IVV can theoretically provide a solution.
7. Comment
The two major obstacles that IVV face currently as an effective public health preventive are the time required to select, manufacture and deliver vaccine annually and the variable annual immunization rates; innovative solutions are required to correct these deficiencies. Fortunately, the recent increase in population groups for whom vaccine is recommended, the increased utilization and increased cost have served to reawaken industry to a potential for profit. The record of product development of therapeutics by industry when a profit is to be made has been impressive. As the cost of health care continues to escalate, it seems likely that governments will provide incentives for the development and application of preventives. In this regard, prevention of influenza by IVV has repeatedly been shown to be cost effective [9, 27]. The goal for influenza immunization is to reduce annual, seasonal influenza to a minor medical problem. A parallel development of improved vaccines and vaccinations and increased immunization rates is essential to ensure a successful public health policy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CCA = Chick cell agglutinating units, a standard used by the USA for quantitating antigen dosage. Distributed vaccines contained 200 to 400 CCA of each strain.
References
- 1.Centers for Disease Control and Prevention. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices. MMWR. 2007;56(RR06):1–54. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Estimates of influenza vaccination target population sizes in 2006 and recent vaccine uptake levels. 2006 July 17; http://www.cdc.gov/flu/professionals/vaccination/pdf/targetpopchart.pdf.
- 3.Committee for Proprietary Medicinal Products (CPMP) Notes for guidance on harmonization of requirements for influenza vaccines (CPMP/BWP/214/96)
- 4.Couch RB. An Overview of Serum Antibody Responses to Influenza Virus Antigens. In: Brown F, Haaheim LR, Wood JM, Schild GC, editors. Developments in Biologicals: Laboratory Correlates of Immunity to Influenza. Vol. 115. Karger: 2003. pp. 25–30. [PubMed] [Google Scholar]
- 5.McElhaney JE, Xie D, Hager WD, Barry MB, Wang Y, Kleppinger A, Ewen C, Kane KP, Bleackley RC. T cell responses are better correlates of vaccine protection in the elderly. J Immunol. 2006;176:6333–6339. doi: 10.4049/jimmunol.176.10.6333. [DOI] [PubMed] [Google Scholar]
- 6.Meiklejohn G. Viral respiratory disease at Lowry Air Force Base in Denver, 1952–1982. J Infect Dis. 1983;148:775–784. doi: 10.1093/infdis/148.5.775. [DOI] [PubMed] [Google Scholar]
- 7.Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med. 1995;123:518–527. doi: 10.7326/0003-4819-123-7-199510010-00008. [DOI] [PubMed] [Google Scholar]
- 8.Govaert TME, Thijs CTMCN, Masurel N, Sprenger MJW, Dinant GJ, Knottnerus JA. The efficacy of influenza vaccination in elderly individuals. A randomized double-blind placebo-controlled trial. JAMA. 1994;272:1661–1665. [PubMed] [Google Scholar]
- 9.Nichol KL. The efficacy, effectiveness and cost-effectiveness of inactivated influenza virus vaccines. Vaccine. 2003;21:1769–1775. doi: 10.1016/s0264-410x(03)00070-7. [DOI] [PubMed] [Google Scholar]
- 10.Ruben FL. Inactivated influenza virus vaccines in children. Clin Infect Dis. 2004;38:678–688. doi: 10.1086/382883. [DOI] [PubMed] [Google Scholar]
- 11.Zangwill KM, Belshe RB. Safety and efficacy of trivalent inactivated influenza vaccine in young children: a summary for the new era of routine vaccination. Pediatr Infect Dis J. 2004;23:189–200. doi: 10.1097/01.inf.0000116292.46143.d6. [DOI] [PubMed] [Google Scholar]
- 12.Keitel WA, Couch RB. Inactivated Influenza Vaccines. In: Potter DW, editor. Influenza. Amsterdam: Elsevier; 2002. pp. 145–177. [Google Scholar]
- 13.Simonsen L, Taylor RJ, Viboud C, Miller MA, Jackson LA. Mortality benefits of influenza vaccination in elderly people: an ongoing controversy. Lancet Infect Dis. 2007;7:658–666. doi: 10.1016/S1473-3099(07)70236-0. [DOI] [PubMed] [Google Scholar]
- 14.Edwards KM, Dupont WD, Westrich MK, Plummer WD, Jr, Palmer PS, Wright PF. A randomized controlled trial of cold-adapted and inactivated vaccines for the prevention of influenza A disease. J Infect Dis. 1994;169:68–76. doi: 10.1093/infdis/169.1.68. [DOI] [PubMed] [Google Scholar]
- 15.Nichol KL, Lind A, Margolis KL, Murdoch M, McFadden R, Hauge M, Magnan S, Drake M. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1994;333:889–893. doi: 10.1056/NEJM199510053331401. [DOI] [PubMed] [Google Scholar]
- 16.Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med. 2007;357:1373–1381. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]
- 17.Mostow SR, Schoenbaum SC, Dowdle WR, Coleman MT, Kaye HS, Hierholzer JC. Am J Epidemiol. 1970;92:248–256. doi: 10.1093/oxfordjournals.aje.a121204. [DOI] [PubMed] [Google Scholar]
- 18.Keitel WA, Couch RB, Cate TR, Hess KR, Baxter B, Quarles JM, Atmar RL, Six HR. High doses of purified influenza A virus hemagglutinin significantly augment serum and nasal antibody responses in healthy adults. J Clin Micro. 1994;32:2468–2473. doi: 10.1128/jcm.32.10.2468-2473.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keitel WA, Cate TR, Atmar RL, Turner CS, Niño D, Dukes CM, Six HR, Couch RB. Increasing doses of purified influenza virus hemagglutinin and subvirion vaccines enhance antibody responses in the elderly. Clin and Diag Lab Immunol. 1996;3:507–510. doi: 10.1128/cdli.3.5.507-510.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palache AM, Beyer WEP, Osterhaus ADME. Influenza vaccine dosages. Vaccine. 2008 doi: 10.1016/j.vaccine.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 21.Mostow SR, Schoenbaum SC, Dowdle WR, Coleman MT, Kaye HS Bulletin of the World Health Organization. Studies with inactivated influenza vaccines purified by zonal centrifugation. 1. Adverse reactions and serological responses; International Conference on Hong Kong Influenza; 14–16 October, 1969; Atlanta, GA, USA. 1969. pp. 525–530. [PMC free article] [PubMed] [Google Scholar]
- 22.Schoenbaum SC, Mostow SR, Dowdle WR, Coleman MT, Kaye HS Bulletin of the World Health Organization. Studies with inactivated influenza vaccines purified by zonal centrifugation. 2. Efficacy; International Conference on Hong Kong Influenza; 14–16 October 1969; Atlanta, GA, USA. 1969. pp. 531–535. [PMC free article] [PubMed] [Google Scholar]
- 23.Davenport FM. Seventeen years’ experience with mineral oil adjuvant influenza virus vaccines. Ann Allergy. 1968;26:288–292. [PubMed] [Google Scholar]
- 24.Podda A, Del Giudice G, O’Hagan DT. MF59: a safe and potent adjuvant for human use. In: Schijns VEJC, O’Hagen DT, editors. Immunopotentiators in modern vaccines. Oxford, UK: 2006. pp. 149–159. [Google Scholar]
- 25.Song J-H, Nguyen HH, Cuburu N, Horimoto T, Ko S-Y, Park S-H, Czerkinsky C, Kweon M-N. Sublingual vaccination with influenza virus protects mice against lethal viral infection. PNAS. 2008;105:1644–1649. doi: 10.1073/pnas.0708684105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belshe RB, Edwards KM, Vesikan T, Black SV, Walker RE, Hultquist M, Kemble G, Connor EM. Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med. 2007;356:685–696. doi: 10.1056/NEJMoa065368. [DOI] [PubMed] [Google Scholar]
- 27.Prosser LA, Bridges CB, Uyeki TM, Hinrichsen VL, Meltzer MI, Molinari N-AM, Schwartz B, Thompson WW, Fukuda K, Lieu TA. Health benefits, risks, and cost-effectiveness of influenza vaccination in children. Emerging Infect Dis. 2006;12:1548–1558. doi: 10.3201/eid1210.051015. [DOI] [PMC free article] [PubMed] [Google Scholar]