Abstract
Objective
To examine the relationship between type, frequency, and level of disruptiveness of physically aggressive agitated behaviors, physically non-aggressive agitated behaviors, verbally aggressive agitated behaviors, and verbally non-aggressive agitated behaviors in persons with dementia.
Methods
The study was conducted in 11 nursing home buildings in Maryland, one of which housed two participating buildings. Participants were 191 older nursing home residents with dementia. Cohen-Mansfield Agitation Inventory (CMAI) data provided information on frequency and level of disruptiveness of different types of agitated behavior.
Results
The highest overall frequencies were reported for verbal nonaggressive behavior and the highest average disruptiveness for verbal aggression. Frequency and disruptiveness of behaviors were highly correlated. Disruptiveness was highly correlated across shifts for all syndromes; a difference in magnitude of disruptiveness between shifts was only evident for physically nonaggressive behaviors (such as pacing), which were more disruptive on the day shift than on the evening shift. When controlling for frequency of behavior, physically aggressive behaviors were the most disruptive across both shifts.
Conclusion
In understanding the impact of agitated behaviors, it is important to take into account both the type of behavior and its frequency. Overall disruptiveness of a type of behavior is different from disruptiveness when the frequency of the behavior is controlled.
Introduction
Agitation is one of the hallmark symptoms of dementia and is characterized by inappropriate verbal, vocal, or motor activity not judged by an outside observer to result directly from perceptible needs or confusion of the agitated individual (Cohen-Mansfield & Billig, 1986). Agitation in persons with dementia is manifested in a wide variety of verbal and physical behaviors that deviate from social norms, including irrelevant vocalizations, screaming, cursing, restlessness, wandering, strange movements, and handling things inappropriately (De Johnge & Kat, 1996; Schreiner, 2000; Cohen-Mansfield et al., 1995). Such disruptive behaviors often indicate discomfort in the person with dementia, and are a major source of stress, disquiet, and occasionally embarrassment for caregivers and loved ones and can take a significant toll over time (Voyer et al., 2005).
The prevalence and effects of neuropsychiatric symptoms in dementia have been described in several studies. Tan et al. (2005) found that neuropsychiatric symptoms, including delusion, irritability, agitation, anxiety, and disinhibition were common in persons with dementia and were positively correlated with caregiver distress. Kauffer et al. (1998) found such symptoms to be more distressing to caregivers than dealing with the cognitive impairment in the persons they care for. Family and friends of nursing home residents with dementia who exhibit aggressive behaviors can be embarrassed and unsure of how to respond to these aggressive outbursts and may decrease the regularity of visits (Voyer et al., 2005). A study by Sourial et al. (2001) found that 95% of the 56 patients with dementia sampled from St. Mary’s Hospital, Montreal, had at least one agitated behavior, and the frequency of these behaviors did not vary based on time of day. The number of behaviors, their mean frequency, and their mean disruptiveness were all significantly correlated with staff burden.
Previous studies have identified several different types of agitated behaviors, or “syndromes of agitation” (Cohen-Mansfield et al., 1989; Rabinowitz et al., 2005) along two dimensions: aggressive vs. nonaggressive, and physical vs. vocal/verbal. The following syndromes are discussed in this paper: 1) physically non-aggressive (inappropriate dressing and/or disrobing, inappropriate eating or drinking, exit-seeking behaviors, handling things, hiding things, hoarding, pacing, repetitious mannerisms, restlessness); 2) physically aggressive (biting, grabbing, hitting, hurting oneself or others, falling intentionally, kicking, physical sexual advances, pushing, scratching, spitting, tearing things, throwing things); 3) verbally non-aggressive (attention-seeking behaviors, complaining, negativism, repetitive sentences or questions); and 4) verbally aggressive (cursing, making strange noises, screaming, verbal sexual advances). The different syndromes have different correlates, suggesting different etiologies. For example, in an observational study of 175 elderly persons with dementia, Cohen-Mansfield and Libin (2005) found verbally agitated behaviors to be associated with female gender, cognitive decline, poor ADL performance, impaired social functioning, and depressed affect. These findings corroborated those of previous studies (Cariaga et al., 1991; Cohen-Mansfield et al., 1992). Physically non-aggressive behaviors were positively related to cognitive impairment and negatively related to number of concurrent medical diagnoses. This syndrome of agitation was not related to gender or age in the sample studied. Disruptiveness was significantly associated with verbal agitation, and women, who show higher levels of verbal agitation than males, had higher scores on disruptiveness as well. The degree of disruptiveness, rather than the verbal agitation itself, influenced the quality of relationships with staff members and residents. Disruptiveness also correlated with a greater number of medical diagnoses.
In addition to type of behavior, agitated behaviors can be characterized by the frequency of their manifestation. No study was found on the relationship between frequency, type and disruptiveness of agitated behaviors. The objective of this study was therefore to examine this relationship using four categories of agitated behaviors observed in persons with dementia: physically aggressive behaviors, physically non-aggressive behaviors, verbally aggressive behaviors, and verbally non-aggressive behaviors.
Methods
Participants and Demographic Information
Participants were 149 women (78%) and 42 men (22%) from 11 nursing homes in 12 buildings in Maryland. The primary inclusion criteria were a diagnosis of dementia, claim by the staff that the resident is agitated prior to CMAI administration, and age older than 60. The mean age was 86.6, with a range of 63.2 – 102.9 years. Table 1 provides a summary of participant demographic information. The racial composition of the group was as follows: 11.5% were African-American (not of Hispanic origin), 1.0% Asian/Pacific Islander, 1.0% American Indian/Alaskan native, 3.1% Hispanic, and 83.2% White (not of Hispanic origin) persons. More than half of the participants were widowed (65.9%), 18.1% were married, 6.6% had never been married, 7.1% were divorced, and 2.2% were separated. Regarding level of education, the largest percentage of participants had a high school education (35.9%), followed by those with an 8th grade education or less (16.5%), and those with a bachelor’s degree (14.6%). As can be seen in Table 1, the demographic composition of the sample was similar to the available survey data on the demographic characteristics of nursing home residents. The facilities provided an average of 3.76 total nursing staff hours per resident per day (range 3.11-4.46) which included an average of 0.54 RN hours, 0.66 LPN hours, and 3.16 nursing assistant hours per resident per day.
Table 1.
Background and agitation summary variables (n=191)
| Characteristic | % in our sample | % National survey a | ||
| Age | Mean: 87 years (range 63 - 103) | N/A | ||
| Gender | Female | 78 | 72 | |
| Male | 22 | 28 | ||
| Race | African-American | 11.5 | 11.4 | |
| Asian | 1 | N/A | ||
| Hispanic | 3.1 | 2.8 | ||
| White, non-Hispanic | 83.2 | 85.8 | ||
| Marital status | Never Married | 6.6 | 15.1 | |
| Married | 18.1 | 17.7 | ||
| Widowed | 65.9 | 57.8 | ||
| Divorced/Separated | 9.3 | 8.4 | ||
| Education | No schooling | 1.9 | N/A | |
| 8th grade or less | 16.5 | N/A | ||
| 9-11 grades | 4.9 | N/A | ||
| High School | 35.9 | N/A | ||
| Tech. or trade school | 7.8 | N/A | ||
| Some college | 7.8 | N/A | ||
| Bachelor’s degree | 14.6 | N/A | ||
| Graduate degree | 10.7 | N/A | ||
| Comorbidity | Mean: 5.2 (range 0-14 diagnoses) | N/A | ||
| Agitation | Frequency (n= 191)* | Disruptiveness (n=191)** | ||
| Mean | s.d | mean | s.d | |
| verbal nonaggressive | 2.48 | 1.27 | 1.33 | 0.58 |
| verbal aggressive | 2.22 | 0.91 | 1.37 | 0.50 |
| Physical nonaggressive | 1.91 | 0.77 | 1.20 | 0.34 |
| Physical aggressive | 1.50 | 0.57 | 1.20 | 0.35 |
National Nursing Home Survey: 1999 Summary.
There is significant difference between frequency for the 4 syndromes F(1,190)=46.570, p≤ 0.001.
There is significant difference between disruptiveness means for the 4 syndromes F(1,190)=11.622, p≤ 0.001.
Assessments
The Cohen-Mansfield Agitation Inventory (CMAI) is a caregiver-rated questionnaire that examines 29 agitated behaviors. The CMAI quantifies the frequency of agitated behaviors exhibited by a resident on a 7-point scale from never (1) to several times an hour (7) throughout the preceding 2 weeks (Cohen-Mansfield et al., 1989). Each agitated behavior that is exhibited is then rated on a 5-point disruptiveness scale (possible answer choices are “not at all,” “a little,” “moderately,” “very much,” and “extremely”) to determine the degree to which the behavior affects caregivers and others who come into contact with an individual. The CMAI was independently completed for each resident by nursing staff members of the day and the evening shift. These ratings were averaged to form frequency and disruptiveness means for the four different types of agitation: physically aggressive behaviors, physically non-aggressive behaviors, verbally aggressive behaviors, and verbally non-aggressive behaviors (Table 1).
Procedure
Eleven nursing homes were recruited for an intervention study described elsewhere (Cohen-Mansfield, J., Libin, A & Marx, M.S, in press). The data used in this study are from the baseline evaluations. Nursing staff from each unit identified agitated residents with dementia, and the responsible party was then approached for informed consent. After receiving consent, demographic and medical data from residents’ charts were collected by a research assistant. Subsequently, research assistants administered the CMAI to both the morning and evening nurses of each participant. When the frequency of behavior was never, disruptiveness was coded as not at all disruptive.
The following analyses were conducted:
The correlation between frequency and disruptiveness within each syndrome of agitation was evaluated by calculating an average syndrome frequency (i.e., across all the behaviors that comprise the syndrome and across the two shifts) and an average syndrome disruptiveness score (again, across all behaviors that comprise the syndrome and across the two shifts) for each of the 4 syndromes for each participant and correlating the results;
The relationship between frequency of behaviors across the morning and the evening shifts was evaluated by calculating each individual’s mean frequency score for each syndrome for each shift. Pearson correlations and paired t-tests were used to compare frequency within persons across shifts. Similar analyses were done for disruptiveness
In order to describe the relationship between type of behavior, frequency of behavior and disruptiveness, the following process was undertaken: For each behavior, persons were aggregated according to the level of frequency of the behavior. All behaviors in each syndrome were then aggregated, the corresponding disruptiveness ratings for each behavior at each specific frequency were averaged, and the mean disruptiveness of each individual behavior for each level of frequency was calculated. The syndromes’ disruptiveness for each level of frequency was calculated as the mean disruptiveness of all the behaviors that compose this syndrome at that frequency. In this way, each level of frequency for each syndrome had an average disruptiveness rating, which corresponds to the average disruptiveness of all behaviors within the syndrome that occurred at that frequency. This procedure was conducted for the morning and the evening shifts separately and for both shifts together.
In this analysis we performed a regression to explain disruptiveness behavior by its frequency and type of syndrome. Because each person has a score on all 4 syndromes, which are therefore not independent, the sample was randomly divided into 4 subsets of equal size. For each subset we used one of the four syndromes. We then conducted a regression of disruptiveness with the following independent variables: 1) the corresponding frequency, 2) aggression (no=0, yes=1), 3) type (verbal =0 physical =1), and 4) demographic variables (age, gender, marital status, race).
Results
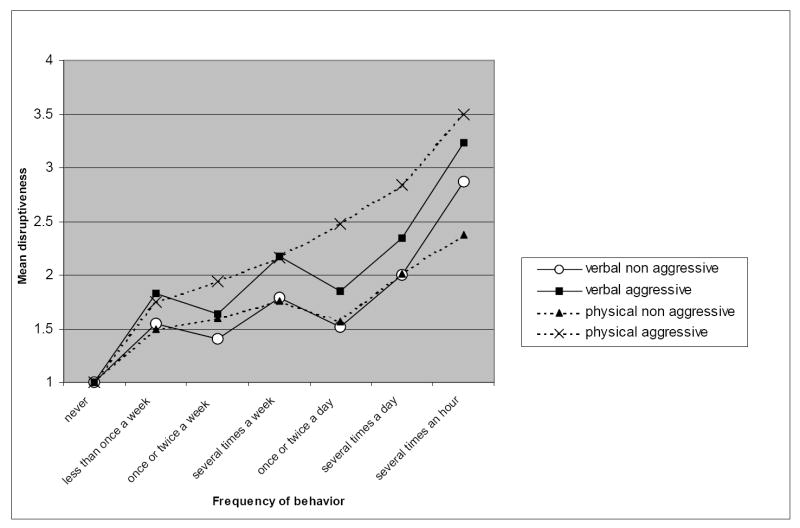
The highest overall frequencies were reported for verbal nonaggressive behaviors and the highest average disruptiveness ratings were for verbal aggression (Table 1). Frequency and disruptiveness of behaviors were highly correlated (Table 2). The frequency of each type of behavior in the day shift was highly correlated with its frequency on the evening shift and, although the mean frequencies were slightly higher during the day shift for all types of behavior in comparison to the evening shift report, none of the differences were statistically significant (Table 3). Similarly, disruptiveness was highly correlated across shifts for all syndromes (Table 3), and a difference in magnitude of disruptiveness was only evident for physically nonaggressive behaviors (such as pacing), which were more disruptive in the day shift than in the evening shift. (Table 3). When controlling for frequency of behavior, physically aggressive behaviors were the most disruptive across both shifts (Table 4 and Figure 1). Verbal aggression was also highly disruptive, at some points of frequency equaling or surpassing physical aggression (figure1).
Table 2.
The correlation between frequency and disruptiveness within each syndrome of agitation (n= 191)
| Verbal nonaggressive | 0.65*** |
| Verbal aggressive | 0.59*** |
| Physical nonaggressive | 0.65*** |
| Physical aggressive | 0.81*** |
p<.05,
p<.01,
p<.001
Table 3.
| a. The relationship between frequency in the morning vs. the evening shifts (n=169) | ||||||
| Frequency | Morning | Evening | Paired T-test | |||
| mean | Sd | mean | sd | (df=168) | Correlation | |
| Verbal non aggressive | 2.54 | 1.43 | 2.33 | 1.40 | 1.89 | 0.49*** |
| Verbal aggressive | 2.29 | 1.10 | 2.18 | 1.06 | 1.25 | 0.42*** |
| Physical non aggressive | 1.97 | 0.88 | 1.92 | 0.85 | 0.79 | 0.60*** |
| Physical aggressive | 1.52 | 0.65 | 1.46 | 0.66 | 1.13 | 0.38*** |
| b. The relationship between disruptiveness of behavior in the morning vs. the evening shifts (n=169) | ||||||
| Disruptiveness | Morning | Evening | Paired T-test | |||
| mean | Sd | mean | sd | (df=168) | Correlation | |
| Verbal non aggressive | 1.33 | 0.68 | 1.25 | 0.58 | 1.52 | 0.43*** |
| Verbal aggressive | 1.36 | 0.60 | 1.35 | 0.58 | 0.09 | 0.32*** |
| Physical non aggressive | 1.24 | 0.47 | 1.16 | 0.35 | 2.36* | 0.49*** |
| Physical aggressive | 1.21 | 0.42 | 1.17 | 0.37 | 1.11 | 0.36*** |
p<.05,
p<.01,
p<.001
Table 4.
Mean disruptiveness by type of behavior and its frequency, with number of ratings used to calculate each mean
| Shift | Type of behavior | verbal non aggressive | # of ratings for verbal non aggressive behaviors | verbal aggressive | # of ratings for verbal aggressive behaviors | physical non aggressive | # of ratings for physical non aggressive behaviors | physical aggressive | # of ratings for physical aggressive behaviors | |
|---|---|---|---|---|---|---|---|---|---|---|
| Morning | frequency of behavior | Never | 1.00 | 438 | 1.00 | 486 | 1.00 | 1274 | 1.00 | 1851 |
| Less than once a week | 1.78 | 27 | 1.59 | 27 | 1.71 | 34 | 1.89 | 66 | ||
| Once or twice a week | 1.45 | 51 | 1.60 | 50 | 1.64 | 59 | 1.98 | 66 | ||
| several times a week | 2.15 | 33 | 2.38 | 29 | 1.86 | 42 | 2.49 | 81 | ||
| Once or twice a day | 1.55 | 58 | 1.80 | 41 | 1.56 | 50 | 2.46 | 82 | ||
| several times a day | 2.11 | 98 | 2.24 | 79 | 2.30 | 152 | 2.86 | 65 | ||
| several times an hour | 2.71 | 28 | 3.27 | 22 | 2.40 | 47 | 3.17 | 6 | ||
| Evening | frequency of behavior | Never | 1 | 440 | 1 | 469 | 1 | 1199 | 1 | 1770 |
| Less than once a week | 1.32 | 19 | 2.07 | 15 | 1.27 | 22 | 1.60 | 35 | ||
| Once or twice a week | 1.35 | 52 | 1.68 | 38 | 1.56 | 50 | 1.89 | 74 | ||
| several times a week | 1.42 | 24 | 1.97 | 39 | 1.66 | 32 | 1.83 | 46 | ||
| Once or twice a day | 1.48 | 54 | 1.89 | 35 | 1.58 | 52 | 2.47 | 57 | ||
| several times a day | 1.88 | 64 | 2.44 | 72 | 1.72 | 138 | 2.81 | 68 | ||
| several times an hour | 3.03 | 30 | 3.18 | 17 | 2.33 | 48 | 3.83 | 6 |
Figure 1.
Disruptiveness by type and frequency of behavior (combining morning and evening shifts)
The regression, which included disruptiveness of the syndrome as the dependent variable and frequency, aggressive vs. nonaggressive, physical vs. verbal, age, gender, married vs. nonmarried, and Caucasian vs. noncaucasian as independent variables, explained 40% of the variance (R2=.4, adjusted R2=.376) with the following significant predictors: frequency of behavior (β=.64, t= 9.42 p<.001), aggressiveness (β= .20, t= 3.28 p=.001), and race ((β= .14, t= 2.29 p<.05). This regression therefore showed increased disruptiveness with increased frequency, more aggressive behavior, and Caucasian race.
Discussion
Agitated behaviors in persons with dementia are often emotionally taxing on caregivers and loved ones and can be a source of embarrassment and anxiety for them as well (Potts et al., 1996). Additionally, agitated behaviors can be detrimental to patient quality of life and interpersonal relations (Chou et al., 1996). Consequently, it is important to identify those behaviors that are most disruptive in order to find effective ways to manage and cope with such behaviors. In this study, we found that verbal nonaggressive behaviors were the most frequently exhibited, while verbal aggression was the most disruptive overall. The main determinants of disruptiveness are the frequency of the behavior and whether or not it is aggressive. Verbal nonaggressive behaviors were least disruptive at the low levels of frequency, and at very high levels of frequency, physical nonaggressive behaviors were the least disruptive. In understanding the impact of agitated behaviors, it is important to take into account both the type of behavior and its frequency. Overall disruptiveness of a type of behavior is different from the disruptiveness of that behavior when controlling for the frequency of its occurrence.
Whereas a study by Sourial et al. (2001) found that the mean frequency of behaviors and their mean disruptiveness were significantly correlated with staff burden, this paper clarifies this finding by examining the relationship between frequency and disruptiveness and by adding the analysis of type of behavior.
The fact that very similar relationships were found in the two shifts, in which we employed independent informants, serves to validate and strengthen the findings. There were minor differences between shifts, i.e. physically nonaggressive behaviors (such as pacing) were more disruptive in the day shift than in the evening shift (Table 3), and verbal aggression received the highest rating of disruptiveness in the highest frequency in the day shift (as well as in some of the lower frequencies in the evening shift (Figure 1). These differences could be explained either by random error or by real differences in behavior and its effect by shift. Future research needs to examine these differences in other samples of persons with dementia.
In addition to frequency and type of behavior there are probably rater variables and patient variables that affect the perception of disruptiveness. Disruptiveness is essentially a subjective evaluation of the impact of behavior and is likely affected by rater’s levels of sensitivity, stress, dedication to the job and other variables. These need to be investigated in future research. Similarly, future research needs to examine the extent to which other qualities of the behavior, such as the quality of sound in verbal agitation (Cohen-Mansfield, Werner, Hammerschmidt, & Newman, 2003) and various qualities of the person with dementia (e.g., general mood or pleasantness) may also affect the perception of disruptiveness of behavior.
The findings of the present study have several important clinical implications. In residential nursing facilities, the ability to measure and anticipate a resident’s levels of disruptiveness can be helpful when determining where he or she should live as well as how to intervene when agitation is exhibited. Nursing home dementia units are typically set up in such a way that the residents live amongst people with whom their behaviors are most compatible, or so that too many disruptive residents are not placed in a single unit, overwhelming staff and adding to already elevated stress levels. However, disruptiveness per se is an insufficient measure of the actual interruption of unit activity. Understanding the type and frequency of behavior are more important measures for planning unit staffing, composition, and interventions. Indeed, disruptiveness can be deduced to a significant extent from the information concerning type and frequency of behavior, and, when resources are limited, the focus of assessment should be on the latter aspects rather than the former.
In summary, although the average disruptiveness of aggressive and nonaggressive behaviors is similar across all frequencies of the CMAI (identical for physical behaviors in our sample – see Table 1), this similarity is based on the different frequencies at which these behaviors are manifested. An aggressive behavior exhibited at low frequencies is more disruptive than a nonaggressive behavior exhibited more frequently. Generally, aggressive behaviors are more disruptive than nonaggressive behaviors, and although physical aggression is typically the most disruptive of the syndromes, there are cases where verbal aggression can exceed its disruptiveness.
Acknowledgments
This study was supported by National Institutes of Health grant AG 10172. I would like to thank Dr. Maha Dakheel-Ali and Natalie Regier for their help in preparing this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Cariaga J, Burgio L, Flynn W, Martin DA. A controlled study of disruptive vocalizations among geriatric residents in nursing homes. Journal of the American Geriatric Society. 1991;39(5):501–507. doi: 10.1111/j.1532-5415.1991.tb02497.x. [DOI] [PubMed] [Google Scholar]
- Chou K, Kaas M, Richie MF. Assaultive behavior in geriatric patients. Journal of Gerontological Nursing. 1996;22(11):31–38. doi: 10.3928/0098-9134-19961101-09. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Billing N. Agitated behaviors in the elderly: A conceptual review. Journal of the American Geriatric Society. 1986;34:711–21. doi: 10.1111/j.1532-5415.1986.tb04302.x. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Marx MS, Rosenthal AS. A description of agitation in a nursing home. Journal of Gerontology: Medical Sciences. 1989;44(3):M77–M84. doi: 10.1093/geronj/44.3.m77. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Marx MS, Werner P. Agitation in elderly persons: An integrative report of findings in a nursing home. International Psychogeriatrics. 1992;4(Suppl 2):221–240. doi: 10.1017/s1041610292001285. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Libin A. Verbal and physical agitation in cognitively impaired elderly with dementia: robustness of syndromes. Journal of Psychiatric Research. 2005;39:325–332. doi: 10.1016/j.jpsychires.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Werner P, Hammerschmidt K, Newman J. Acoustic properties of vocally disruptive behaviors in the nursing home. Gerontology. 2003;49(3):161–167. doi: 10.1159/000069173. [DOI] [PubMed] [Google Scholar]
- Jones A. The National Nursing Home Survey: 1999 summary. National Center for Health Statistics. Vital Health Statistics. 2002;13(152) [PubMed] [Google Scholar]
- Rabinowitz J, Davidson M, De Deyn PP, Katz I, Brodaty H, Cohen-Mansfield J. Factor analysis of the Cohen-Mansfield Agitation Inventory in three large samples of nursing home patients with dementia and behavioral disturbance. American Journal of Geriatric Psychiatry. 2005;13(11):991–8. doi: 10.1176/appi.ajgp.13.11.991. [DOI] [PubMed] [Google Scholar]
- Potts HW, Richie MF, Kaas MJ. Resistance to care. Journal of Gerontological Nursing. 1996;22(11):11–16. doi: 10.3928/0098-9134-19961101-06. [DOI] [PubMed] [Google Scholar]
- Sourial R, McCusker J, Cole M, Abrahamowicz M. Agitation in demented patients in an acute care hospital: Prevalence, disruptiveness, and staff burden. International Psychogeriatrics. 2001;13(2):183–197. doi: 10.1017/s1041610201007578. [DOI] [PubMed] [Google Scholar]
- Tan LL, Wong HB, Allen H. The impact of neuropsychiatric symptoms of dementia on distress in family and professional caregivers in Singapore. International Psychogeriatrics. 2005;17(2):253–263. doi: 10.1017/s1041610205001523. [DOI] [PubMed] [Google Scholar]
- Voyer P, Verreault R, Azizah GM, Desrosiers J, Champoux N, Bedard A. Prevalence of physical and verbal aggressive behaviours and associated factors among older adults in long-term care facilities. BMC Geriatrics. 2005;5(13):1–13. doi: 10.1186/1471-2318-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]