Abstract
OBJECTIVE:
To evaluate survival and readmissions to hospital for cardiac events or coronary revascularization (REVASC) in patients having off-pump (OPCAB) versus conventional on-pump (CCAB) coronary artery bypass graft surgery (CABG).
METHODS:
Of 11,368 consecutive patients undergoing isolated CABG between 1996 and 2002, 514 had OPCAB surgery. Using propensity scores, 503 CCAB patients were randomly matched to 503 OPCAB patients.
RESULTS:
There were no clinical or statistical differences between the two groups for any prognostic variable. However, OPCAB patients received significantly fewer distal anastomoses than the CCAB group (2.6±1.0 versus 3.1±1.0; P<0.001). There was no difference in operative mortality (OPCAB 1.0%, CCAB 1.4%; P=0.6), but the OPCAB group had significantly fewer operative strokes (0.2% versus 1.8%; P=0.01). Follow-up was 99.7% complete at 2.2±1.2 years (range 0 to 6 years). Twice as many OPCAB patients (n=24) required REVASC compared with the CCAB (n=11) group. The following five-year actuarial outcomes are presented for CCAB and OPCAB, respectively: survival: 77±6%, 76±8%, P=0.8; freedom from REVASC: 95±3%, 92±2%, P=0.02; and cardiac event-free survival: 76±5%, 62±8%; P=0.05. Cox regression revealed that OPCAB was a significant independent predictor of poorer freedom from REVASC (RR 2.2, 95% CI 1.0 to 4.6; P=0.04) and cardiac event-free survival (RR 1.6, 95%CI 1.1 to 2.2; P=0.02).
CONCLUSIONS:
The use of OPCAB remains controversial. These results, from this early experience, suggest that despite improved hospital outcomes, the lesser degree of REVASC raises concerns about the need for repeat revascularization in the OPCAB group.
Keywords: Off-pump coronary artery bypass, Survival
Abstract
OBJECTIF:
Évaluer la survie et les réhospitalisations en raison d’événements cardiaques ou d’une revascularisation coronaire (REVASC) chez les patients ayant subi un pontage aortocoronarien (PAC) à cœur battant (PACCB) par rapport à un PAC avec circulation extracorporelle (PACCE) classique.
MÉTHODOLOGIE:
Des 11 368 patients consécutifs ayant subi un PAC isolé entre 1996 et 2002, 514 avaient subi un PACCB. À l’aide des indices de tendances, 503 patients PACCE ont été appariés de manière aléatoire à 503 patients PACCB.
RÉSULTATS:
Les auteurs n’ont observé aucune différence clinique ou statistique entre les deux groupes à l’égard de l’une ou l’autre des variables pronostiques. Cependant, les patients PACCB ont subi beaucoup moins d’anastomoses distales que le groupe PACCE (2,6±1,0 par rapport à 3,1±1,0; P<0,001). Il n’y avait pas de différence de mortalité opératoire (PACCB 1,0 %, PACCE 1,4 %; P=0,6), mais le groupe PACCB avait subi beaucoup moins d’accidents cérébrovasculaires opératoires (0,2 % par rapport à 1,8 %; P=0,01). Le suivi était complet à 99,7 % au bout de 2,2±1,2 ans (fourchette de 0 à 6 ans). Deux fois plus de patients PACCB (n=24) ont eu besoin d’une REVASC que de patients PACCE (n=11). Les issues actuarielles suivantes au bout de cinq ans sont présentées pour le PACCB et le PACCE, respectivement : survie : 77±6 %, 76±8 %, P=0,8; absence de REVASC : 95±3 %, 92±2 %, P=0,02; et survie sans événements cardiaques : 76±5 %, 62±8 %, P=0,05. La régression de Cox a révélé que le PACCB était un prédicteur indépendant significatif de moindre absence de REVASC (RR 2,2, 95 % IC 1,0 à 4,6, P=0,04) et de survie sans événements cardiaques (RR 1,6, 95 % IC 1,1 à 2,2; P=0,02).
CONCLUSIONS:
Le recours au PACCB demeure controversé. Ces résultats, tirés de cette expérience précoce, indiquent que malgré l’amélioration des issues hospitalières, la revascularisation moins marquée soulève des préoccupations quant à la nécessité de reprendre la revascularisation au sein du groupe PACCB.
Coronary artery disease is associated with more death and disabilities than any other disease in industrialized nations. Coronary artery bypass graft surgery (CABG) is one of the most effective methods of treating symptomatic coronary artery disease and is performed in approximately 10,000 patients annually in Ontario.
The majority of cardiac operations require the establishment of cardiopulmonary bypass and cardioplegic arrest. However, cardiopulmonary bypass is a well-recognized factor for generating a whole-body inflammatory response, which can contribute to postoperative morbidity including renal, pulmonary, neurological and bleeding complications (1,2). Benetti et al (3) and Buffolo et al (4) reintroduced beating heart surgery almost 20 years ago as a strategy to prevent complications in high-risk patients. Since that time, off-pump coronary artery bypass (OPCAB) surgery has gained increasing popularity and is challenging conventional on-pump coronary artery bypass (CCAB) as the standard of therapy for multivessel disease in many cardiac centres (2).
The benefits of OPCAB remain controversial, despite the publication of numerous studies reporting equivalent or improved hospital outcomes and significantly shorter lengths of hospital stay. Ascione and Angelini (5) discussed the dilemma faced by many cardiac surgeons who perform CABG. On one hand, the literature is replete with studies that emphasize the potential for reducing postoperative morbidity and length of stay with OPCAB surgery (6–24); on the other hand, there is continued concern regarding intraoperative myocardial ischemia, inadequate revascularization and the need for early revascularization (5,8,23,25–29).
Therefore, the purpose of the present study was to evaluate mid-term outcomes of OPCAB versus conventional CCAB in two well-matched cohorts.
METHODS
Patient sample
Between January 1996 and December 2002, 11,368 patients underwent isolated CABG at the University Health Network – Toronto General Hospital (Toronto, Ontario). Of these, 514 patients had surgery performed without cardiopulmonary bypass. All patients had their preoperative, perioperative and hospital clinical outcomes entered prospectively into the cardiac surgery database. The present study was conducted at the Toronto General Hospital and the Institute for Clinical Evaluative Sciences (Toronto), and was approved by the hospital’s institutional research ethics board.
Propensity score matching
Calculation of the propensity score:
A logistic regression analysis was used to develop a propensity score for OPCAB selection (5,30–37). All prognostic variables (Appendix 1), including a temporal marker and coronary systems grafted, were forced into the logistic regression model so that matching with CCAB patients could be accomplished using all measured variables. Only 52 of 11,368 patients were deleted for missing one or more of the data elements.
The propensity score is defined as the predicted probability that any one patient would be selected for OPCAB surgery. It is calculated from the logistic regression coefficients.
Using only the propensity score, off-pump patients were randomly matched to on-pump patients using a greedy matching strategy (38). Initially, matching was performed based on five decimal places of the propensity score, followed by four-, three-, two- and one-decimal point matching. This yielded 503 OPCAB patients matched to 503 CCAB patients.
Late outcomes
Primary outcome:
The primary outcome for the present study was cardiac event-free survival. This was a composite outcome that included any death (including hospital deaths), readmission to hospital for an acute myocardial infarction, readmission to hospital for coronary revascularization (repeat CABG or percutaneous coronary intervention [PCI]) or readmission for stroke.
Administrative data linkage:
The Canadian Institute of Health Information contains the discharge International Classification of Disease 9th and 10th revision (ICD-9 and ICD-10) codes for every patient admitted to a Canadian hospital. Since 1982, the Division of Cardiovascular Surgery at the Toronto General Hospital has maintained a prospective database for every patient undergoing cardiac surgery at this institution (39–41). The medical record number and the health card number were used to link the clinical database with administrative data to follow all study patients for survival and readmission to hospital for cardiac events. All data linkage and analysis took place at the Institute for Clinical Evaluative Sciences. The closing date for late events was March 31, 2003.
Deaths were determined from three sources:
operative mortality, defined as any in-hospital death in the clinical registry during the index admission for CABG;
in-hospital deaths from the Canadian Institute for Health Information database were determined from the discharge exit code; and
out-of-hospital deaths were determined from the Registered Persons Data Base.
Readmissions to hospital for cardiac events occurring after the entry date of operation were determined from the ICD-9 and ICD-10 codes for the most responsible diagnosis and the revised Canadian Classification of Diagnostic procedure codes for the revascularization procedures (42,43).
The first admission for each cardiac event was captured and used in the analysis; therefore, any patient could have had more than one type of cardiac event analyzed. The failure time for freedom from any cardiac event was defined as the earliest readmission date for any cardiac event.
Statistical analysis
SAS 8.2 for Windows (SAS Institute, USA) was used for all data analysis. Results are reported as the mean ± 1 SD in the tables and text, and as the mean ± 1 SEM in the figures. Continuous variables were analyzed by unpaired t tests. Categorical variables are reported as proportions and were analyzed using χ2 or Fisher’s exact test, where appropriate. Time-to-event outcomes were analyzed univariately by the Kaplan-Meier method and multivariably by Cox regression. The P value for significance was 0.05. The present study had 80% power to detect a 20% risk reduction in time-to-event outcomes.
RESULTS
Effectiveness of matching
A comparison of the 503 matched pairs is contained in Table 1. Patients were very similar and, unlike previous studies (19), they were matched for major coronary vessels grafted, peripheral vascular disease, previous stroke or transient ischemic attack, and year of operation. However, despite a similar extent of coronary artery disease, OPCAB patients received significantly fewer bypass grafts than CCAB patients.
TABLE 1.
Propensity score, pair-wise-matched sample of patients undergoing isolated off-pump (OPCAB) and on-pump (CCAB) coronary artery bypass graft surgery between 1996 and 2002 at the University Health Network – Toronto General Hospital
| Variable | CCAB (n=503) | OPCAB (n=503) | P |
|---|---|---|---|
| Age, years* | 63±10 | 63±10 | 0.6 |
| Body surface area, m2* | 1.92±0.2 | 1.91±0.2 | 0.3 |
| Body mass index, kg/m2* | 28±7 | 28±5 | 0.8 |
| CBP time, min* | 83±29 | 0 | <0.001 |
| Cross-clamp time, min* | 60±22 | 0 | <0.001 |
| Female sex, % | 23 | 26 | 0.4 |
| Left ventricular grade | |||
| 1 | 45 | 45 | |
| 2 | 35 | 34 | |
| 3 | 18 | 19 | |
| 4 | 2 | 2 | 0.9 |
| Surgical priority | |||
| Elective | 52 | 55 | |
| Urgent | 47 | 45 | |
| Emergent | 0.2 | 0.2 | 0.8 |
| Recent myocardial infarction† | 17 | 18 | 0.6 |
| New York Heart Association classification | |||
| I | 9 | 9 | |
| II | 16 | 18 | |
| III | 18 | 18 | |
| IV | 58 | 56 | 0.8 |
| Number of diseased vessels | |||
| 1 | 14 | 16 | |
| 2 | 29 | 28 | |
| 3 | 57 | 56 | 0.7 |
| Left main disease | 20 | 20 | 1.0 |
| Redo coronary artery bypass graft surgery | 3.6 | 3.6 | 1.0 |
| Renal insufficiency | 6.6 | 6.2 | 0.8 |
| Congestive heart failure | 6.6 | 7.0 | 0.8 |
| Diabetes | 30 | 30 | 1.0 |
| Peripheral vascular disease | 34 | 36 | 0.6 |
| Hypertension | 58 | 56 | 0.4 |
| Chronic obstructive lung disease | 4 | 4 | 1.0 |
| Preoperative stroke/TIA | 9.2 | 10 | 0.7 |
| Year of operation | |||
| 1996–1998 | 9 | 13 | |
| 1999–2000 | 65 | 62 | |
| 2001–2002 | 26 | 26 | 0.1 |
| Number of distal anastomoses | |||
| 1 | 5.2 | 10 | |
| 2 | 23 | 13 | |
| 3 | 36 | 33 | |
| 4 | 29 | 18 | |
| 5 | 6 | 3 | <0.001 |
| Number of grafts* | 3.1±1.0 | 2.6±1.0 | <0.001 |
| Coronary system grafted | |||
| Left anterior descending artery | 97 | 96 | 0.7 |
| Circumflex coronary artery | 62 | 61 | 0.7 |
| Right coronary artery | 38 | 39 | 0.7 |
| Left internal thoracic artery | 89 | 88 | 0.8 |
| RITA | 5.2 | 8.0 | 0.07 |
| LITA + RITA | 4.6 | 7.4 | 0.06 |
*Reported as mean ± SD;
†Within one month before surgery. CBP Cardiopulmonary bypass; LITA Left internal thoracic artery; RITA Right internal thoracic artery; TIA Transient cerebral ischemic attack
Hospital outcomes
OPCAB patients had significantly shorter intensive care unit and total length of hospital stays (Table 2). Hospital mortality was similar between the two groups. However, OPCAB patients had significantly fewer strokes. Reoperation for bleeding was higher in the OPCAB group. The reason for more bleeding in the OPCAB group is unclear from the analysis, but it may be related to a pattern of practice by anesthesiology to avoid giving antifibrinolytics to this group at the time of surgery.
TABLE 2.
Hospital outcomes
| CCAB | OPCAB | P | |
|---|---|---|---|
| Ventilation time, h* | 14±30 | 10±23 | 0.036 |
| Intensive care unit stay, days* | 2.0±3.4 | 1.7±2.2 | 0.052 |
| Total length of stay, days* | 7.7±6.2 | 6.8±5.5 | 0.017 |
| Hospital mortality, % | 1.4 | 1.0 | 0.6 |
| Myocardial infarction, % | 2.2 | 3.6 | 0.2 |
| Low cardiac output syndrome, % | 4.8 | 3.4 | 0.3 |
| Stroke, % | 1.8 | 0.2 | 0.011 |
| Postoperative renal failure, % | 0.8 | 0.8 | 0.6 |
| Reopened for bleeding, % | 1.8 | 4.6 | 0.012 |
*Reported as mean ± SD. CCAB On-pump coronary artery bypass; OPCAB Off-pump coronary artery bypass
Late outcomes
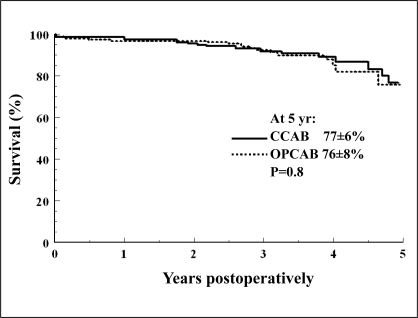
Three out-of-province patients were lost to follow-up. The length of follow-up was similar in both groups: CCAB 2.2±1.2 years, OPCAB 2.2±1.3 years (P=0.4). The range of follow-up was zero to six years. Seventy patients died (35 in each group). The five-year survival (Figure 1) was 77±6% in the CCAB group and 76±8% in the OPCAB group (P=0.8).
Figure 1).
Survival estimates for conventional coronary artery bypass (CCAB) depicted by the solid line and off-pump coronary artery bypass (OPCAB) depicted by the dashed line. Patients at risk at one, three and five years (yr), respectively, for CCAB: 397, 118 and 17; and OPCAB: 404, 116 and 12
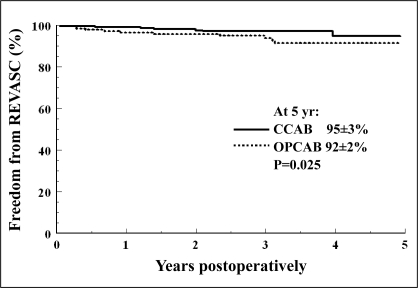
Twice as many OPCAB patients required coronary revascularization (n=24; CABG n=12, PCI n=16) compared with the CCAB group (n=11; CABG n=4, PCI n=8). Some patients required both PCI and repeat CABG. The five-year freedom from repeat coronary revascularization (Figure 2) was 95±3% in the CCAB group and 92±2% in the OPCAB group (P=0.025). OPCAB was a significant independent predictor of the need for repeat revascularization (RR 2.2; 95% CI 1.0 to 4.6; P=0.038).
Figure 2).
Freedom from coronary revascularization (REVASC) (defined as repeat coronary artery bypass or percutaneous coronary intervention). CCAB Conventional coronary artery bypass; OPCAB Off-pump coronary artery bypass; yr Years
There was a similar number of readmissions for acute myocardial infarction (CCAB n=14, OPCAB n=12). Freedom from acute myocardial infarction at five years was 90±5% in the CCAB group and 87±7% in the OPCAB group (P=0.8). There was no significant difference between the two groups for stroke readmissions: five-year estimates were 98±1% in the CCAB group and 94±2% in the OPCAB group (P=0.2).
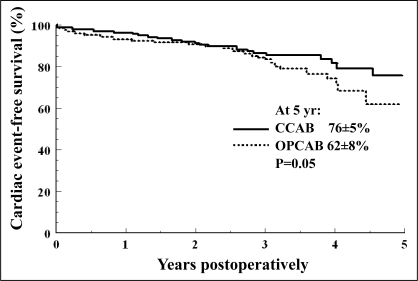
There was a significant difference in cardiac event-free survival between the two groups (CCAB n=50, OPCAB n=65) (Figure 3). Five-year cardiac event-free survival was 76±5% in the CCAB group and 62±8% in the OPCAB group (P=0.05). OPCAB was a significant independent predictor of death or readmission for a cardiac event (RR 1.55; 95% CI 1.1 to 2.2; P=0.05).
Figure 3).
Cardiac event-free survival (defined as freedom from death or readmission to hospital for acute myocardial infarction, repeat coronary intervention or stroke). CCAB Conventional coronary artery bypass; OPCAB Off-pump coronary artery bypass; yr Years
DISCUSSION
The level of existing evidence regarding the benefits of off-pump CABG is controversial. There are several small randomized trials (6–12) that reported less operative morbidity, shorter lengths of hospital stay and reduced costs with OPCAB. In a meta-analysis of nine randomized controlled trials, Parolari et al (2) evaluated a composite hospital end point (death, stroke or myocardial infarction) in 532 patients randomly assigned to OPCAB and 558 patients randomly assigned to CCAB. They found a trend toward a risk reduction associated with OPCAB for the composite outcome (OR 0.48; 95% CI 0.21 to 1.09; P=0.08). However, a more recent randomized controlled trial by Legare et al (44) failed to demonstrate any short-term advantage to OPCAB.
In contrast, Czerny et al (25) found that 35% of patients (14 of 40) randomly assigned to the OPCAB arm had to be switched to CCAB because of deep myocardial vessels or hemodynamic instability. In addition, 11.5% of the remaining OPCAB patients (three of 26) required percutaneous transluminal angioplasty within three months of surgery versus none in the CCAB group. They concluded that the rate of incomplete revascularization was high and compromised the basic principle of complete revascularization in patients requiring CABG. Although hospital outcomes reported from randomized trials for OPCAB are mostly favourable, the length of follow-up tends to be too short and the sample sizes insufficiently powered to detect differences in late outcomes.
Observational studies generally have much larger sample sizes, and when proper multivariable statistical methods are employed, demonstrate a similar risk reduction for in-hospital outcomes for OPCAB surgery (13–20). However, such studies are frequently limited by the fact that patients who ‘cross over’ to CCAB, usually due to hemodynamic instability or other intraoperative difficulties, are frequently not identified a priori. Such patients represent a very high-risk cohort and invariably result in worse outcomes for the on-pump group. Most larger contemporary observational studies do not report late clinical outcomes. Hence, the dilemma faced by many cardiac surgeons: without clear evidence of late outcomes, it is difficult to weigh the risks and benefits of OPCAB surgery.
The results of the present study were similar to those found in an early small observational study of consecutive patients operated on between 1989 and 1990 by Gundry et al (26). They found that survival was equivalent at seven years, but OPCAB patients were almost three times more likely to require revascularization (20%) compared with CCAB patients (7%; P=0.01). In fact, six of 101 OPCAB patients (5.6%) required repeat CABG compared with none in the CCAB group (P=0.01). There was, on average, one fewer graft per OPCAB patient compared with the CCAB group. A larger observational study by Williams et al (27) also demonstrated an increased risk for repeat revascularization with OPCAB surgery (RR 1.29, P=0.02). Other studies (23,27,28) have reported similar increased need for early revascularization following OPCAB. The increased need for repeat revascularization may outweigh any potential economic benefits of earlier intensive care unit and hospital discharge. This concern may have factored into the results found by Desai et al (29), who conducted a population-based survey of Canadian cardiac surgeons and found that on-pump bypass was still the preferred strategy.
Ascione and Angelini (5) offer a cautionary note in their editorial. They stated that OPCAB is being performed in thousands of patients every year, resulting in a possible reduction in-hospital morbidity and in-hospital costs of up to 25%. However, the evidence regarding long-term outcomes is still inconclusive. They suggested that if the evidence is against OPCAB, those surgeons performing this procedure should stop because they are affecting the quality of care of thousands of patients worldwide. If, on the other hand, the evidence from long-term studies supports OPCAB, training programs should support the implementation of OPCAB.
The issue of a lack of long-term clinical outcomes in OPCAB surgery cannot be overstated. The present study was designed to provide timely information, for a well-matched OPCAB and CCAB patient sample, regarding survival and readmission to hospital for cardiac events, not the least of which is the need for repeat revascularization.
Limitations
The limitations of the present study include those associated with observational studies, in that we can only adjust for those variables measured. In addition, OPCAB was not uniformly applied to a specific patient population; therefore, some selection bias may be present that was not factored into the propensity score-matching procedure. One surgeon at our institution routinely performed off-pump surgery during the study period and accounted for 75% of the total OPCAB patient population. Other surgeons generally performed off-pump surgery only in those patients who were considered to be high-risk for on-pump revascularization (eg, patients with ascending aorta atherosclerosis). It is important to note, however, that patients who required ascending aorta repair were not included in the present study, and that we did not find any surgeon-related effects in our analysis of outcomes.
One potential criticism of our methods may be that we included patients from the ‘learning curve’. While eliminating patients from the learning curve is an acceptable method for randomized controlled trials, it is not, in our opinion, acceptable for observational studies. By definition, observational studies evaluate ‘real-world’ experience: eliminating early patients and their outcomes may potentially introduce another level of bias. Outcomes of CABG have improved nationwide over the past decade; these patients were matched on year of operation, and hopefully this manoeuvre helped to mitigate some of the potential learning curve issues.
CONCLUSION
OPCAB surgery was associated with shorter hospital lengths of stay and fewer operative strokes. However, the issue of incomplete revascularization remains a concern, because OPCAB was associated with a higher rate of repeat revascularization and poorer cardiac event-free survival in these early patients.
Acknowledgments
The authors wish to thank Susan Collins, for database management, and Claus Wall (ret) for data linkage at Institute for Clinical Evaluative Sciences. This study was supported by a Heart and Stroke Foundation of Ontario grant-in-aid (#NA-5481).
APPENDIX 1
Variables forced into the logistic regression model for off-pump coronary artery bypass (OPCAB) selection
| Age at operation (years) |
| Sex: male/female |
| Left ventricular grade |
| 1 – Left ventricular ejection fraction >60%, |
| 2 – Left ventricular ejection fraction 40% to 59% |
| 3 – Left ventricular ejection fraction 20% to 39% |
| 4 – Left ventricular ejection fraction <20% |
| Surgical priority |
| Elective |
| Urgent (same hospitalization as cardiac catheterization or cardiac event) |
| Emergent (within 12 h of cardiac catheterization or a cardiac event) |
| New York Heart Association classification for symptoms (I to IV) |
| Recent myocardial infarction (within one month before surgery) |
| Previous coronary artery bypass graft surgery |
| Number of major coronary artery systems diseased (one, two or three) |
| Left main coronary artery disease (>50% stenosis) |
| Presence of congestive heart failure |
| Renal insufficiency: renal dialysis or serum creatinine >150 μmol/L |
| Diabetes controlled by medication |
| Peripheral vascular disease, including disease of the carotid artery |
| Chronic obstructive pulmonary disease |
| History of hypertension |
| History of a cerebral stroke or transient ischemic attack |
| Vessels grafted: any distal anastomosis to major coronary system (left anterior descending, right coronary artery, circumflex) |
| Year of operation (1996 to 1998, 1999 to 2000, 2001 to 2002) |
These variables were forced into a logistic regression analysis to calculate the predicted probability that any patient would be selected for OPCAB surgery. The predicted probability for OPCAB selection = the propensity score. A group of patients with the same propensity score for OPCAB selection are therefore equally likely to have been assigned to the conventional coronary artery bypass (CCAB; control) group. Each OPCAB patient was randomly matched to a CCAB patient by the propensity score
REFERENCES
- 1.Wan S, LeClerc JL, Vincent JL. Inflammatory response to cardiopulmonary bypass: Mechanisms involved and possible therapeutic strategies. Chest. 1997;112:676–92. doi: 10.1378/chest.112.3.676. [DOI] [PubMed] [Google Scholar]
- 2.Parolari A, Alamanni F, Cannata A, et al. Off-pump versus on-pump coronary artery bypass: Meta-analysis of currently available randomized trials. Ann Thorac Surg. 2003;76:37–40. doi: 10.1016/s0003-4975(03)00183-8. [DOI] [PubMed] [Google Scholar]
- 3.Benetti FJ, Ballester C, Sani G, Doonstra P, Grandjean J. Video assisted coronary bypass surgery. J Cardiac Surg. 1995;10:620–5. doi: 10.1111/j.1540-8191.1995.tb00651.x. [DOI] [PubMed] [Google Scholar]
- 4.Buffolo E, de Andrade CS, Branco JN, Teles CA, Aguiar LF, Gomes WJ. Coronary artery bypass grafting without cardiopulmonary bypass. Ann Thorac Surg. 1996;61:63–6. doi: 10.1016/0003-4975(95)00840-3. [DOI] [PubMed] [Google Scholar]
- 5.Ascione R, Angelini GD. Off-pump coronary artery bypass surgery: The implications of the evidence. J Thorac Cardiovasc Surg. 2003;125:779–81. doi: 10.1067/mtc.2003.11. [DOI] [PubMed] [Google Scholar]
- 6.Ascione R, Lloyd CT, Gomes WJ, Caputo M, Bryan A, Angelini GD. Beating versus arrest heart revascularization: Evaluation of myocardial function in a prospective randomized study. Eur J Cardiothorac Surg. 1999;15:685–90. doi: 10.1016/s1010-7940(99)00072-x. [DOI] [PubMed] [Google Scholar]
- 7.Ascione R, Caputo M, Calori G, Lloyd C, Underwood M, Angelini G. Predictors of atrial fibrillation after conventional and beating heart coronary surgery. A prospective, randomized study. Circulation. 2000;102:1530–5. doi: 10.1161/01.cir.102.13.1530. [DOI] [PubMed] [Google Scholar]
- 8.Angelini GD, Taylor FC, Reeves BC, Ascione R. Early and midterm outcome after off-pump and on-pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): A pooled analysis of two randomised controlled trials. Lancet. 2002;359:1194–9. doi: 10.1016/S0140-6736(02)08216-8. [DOI] [PubMed] [Google Scholar]
- 9.van Dijk D, Nierich AP, Jansen EW, et al. Early outcome after off-pump versus on-pump coronary bypass surgery: Eesults from a randomized study. Circulation. 2001;104:1761–6. doi: 10.1161/hc4001.097036. [DOI] [PubMed] [Google Scholar]
- 10.Puskas JD, Williams WH, Duke PG, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: A prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:797–808. doi: 10.1067/mtc.2003.324. [DOI] [PubMed] [Google Scholar]
- 11.Tang AT, Knott J, Nanson J, Hsu J, Haw MP, Ohri SK. A prospective randomized study to evaluate the renoprotective action of beating heart coronary surgery in low risk patients. Eur J Cardiothorac Surg. 2002;22:118–23. doi: 10.1016/s1010-7940(02)00220-8. [DOI] [PubMed] [Google Scholar]
- 12.Lee JD, Lee SJ, Tsushima WT, et al. Benefits of off-pump bypass on neurologic and clinical morbidity: A prospective randomized trial. Ann Thorac Surg. 2003;76:18–26. doi: 10.1016/s0003-4975(03)00342-4. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez F, Cohn WE, Baribeau YR, et al. In-hospital outcomes of off-pump versus on-pump coronary artery bypass procedures: A multicenter experience. Ann Thorac Surg. 2001;72:1528–33. doi: 10.1016/s0003-4975(01)03202-7. [DOI] [PubMed] [Google Scholar]
- 14.Patel NC, Grayson AD, Jackson M, et al. The effect off-pump coronary artery bypass surgery on in-hospital mortality and morbidity. Eur J Cardiothorac Surg. 2002;22:255–60. doi: 10.1016/s1010-7940(02)00301-9. [DOI] [PubMed] [Google Scholar]
- 15.Plomondon ME, Cleveland JC, Jr, Ludwig ST, et al. Off-pump coronary artery bypass is associated with improved risk-adjusted outcomes. Ann Thorac Surg. 2001;72:114–9. doi: 10.1016/s0003-4975(01)02670-4. [DOI] [PubMed] [Google Scholar]
- 16.Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: A risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75:472–8. doi: 10.1016/s0003-4975(02)04370-9. [DOI] [PubMed] [Google Scholar]
- 17.Cleveland JC, Jr, Shroyer AL, Chen AY, Peterson E, Grover FL. Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity. Ann Thorac Surg. 2001;72:1282–8. doi: 10.1016/s0003-4975(01)03006-5. [DOI] [PubMed] [Google Scholar]
- 18.Brown PP, Mack MJ, Simon AW, et al. Outcomes experience with off-pump coronary artery bypass surgery in women. Ann Thorac Surg. 2002;74:2113–9. doi: 10.1016/s0003-4975(02)03988-7. [DOI] [PubMed] [Google Scholar]
- 19.Sabik JF, Gillinov AM, Blackstone EH, et al. Does off-pump coronary surgery reduce morbidity and mortality? J Thorac Cardiovasc Surg. 2002;124:698–707. doi: 10.1067/mtc.2002.121975. [DOI] [PubMed] [Google Scholar]
- 20.Novick RJ, Fox SA, Stitt LW, et al. Effect of off-pump coronary artery bypass grafting on risk-adjusted and cumulative sum failure outcomes after coronary artery surgery. J Card Surg. 2002;17:520–8. doi: 10.1046/j.1540-8191.2002.01008.x. [DOI] [PubMed] [Google Scholar]
- 21.Mishra M, Malhotra R, Karlekar A, Mishra Y, Trehan N. Propensity case-matched analysis of off-pump versus on-pump coronary artery bypass grafting in patients with atheromatous aorta. Ann Thoracic Surg. 2006;82:608–14. doi: 10.1016/j.athoracsur.2006.03.071. [DOI] [PubMed] [Google Scholar]
- 22.Al-Ruzzeh S, George S, Bustami M, et al. Effect of off-pump coronary artery bypass surgery on clinical, angiographic, neurocognitive, and quality of life outcomes: Randomised controlled trial. BMJ. 2006;332:1365. doi: 10.1136/bmj.38852.479907.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wijeysundera D, Scott W, Djaiani G, et al. Off-pump coronary artery surgery for reducing mortality and morbidity: Meta-analysis of randomized and observational studies. J Am Coll Cardiol. 2005;46:872–82. doi: 10.1016/j.jacc.2005.05.064. [DOI] [PubMed] [Google Scholar]
- 24.Mack M, Brown P, Houser F, et al. On-pump versus off-pump coronary artery bypass surgery in a matched sample of women: A comparison of outcomes. Circulation. 2004;110(11 Suppl 1):II1–6. doi: 10.1161/01.CIR.0000138198.62961.41. [DOI] [PubMed] [Google Scholar]
- 25.Czerny M, Baumer H, Kilo J, et al. Complete revascularization in coronary artery bypass grafting with and without cardiopulmonary bypass. Ann Thorac Surg. 2001;71:165–9. doi: 10.1016/s0003-4975(00)02230-x. [DOI] [PubMed] [Google Scholar]
- 26.Gundry SR, Romano MA, Shattuck OH, Razzouk AJ, Bailey LL. Seven-year follow-up of coronary artery bypasses performed with and without cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1998;115:1273–7. doi: 10.1016/S0022-5223(98)70209-0. [DOI] [PubMed] [Google Scholar]
- 27.Williams ML, Muhlbaier LH, Schroder JN, et al. Risk-adjusted short- and long-term outcomes for on-pump versus off-pump coronary artery bypass surgery. Circulation. 2005;112(9 Suppl):I366–70. doi: 10.1161/CIRCULATIONAHA.104.526012. [DOI] [PubMed] [Google Scholar]
- 28.Widimsky P, Traka Z, Stros P, et al. One-year coronary bypass graft patency: A randomized comparison between off-pump and on-pump surgery angiographic results of the PRAGUE-4 trial. Circulation. 2004;110:3418–23. doi: 10.1161/01.CIR.0000148139.79580.36. [DOI] [PubMed] [Google Scholar]
- 29.Desai N, Pelletier M, Mallidi H, et al. Why is off-pump coronary surgery uncommon in Canada? Results of a population-based survey of Canadian heart surgeons. Circulation. 2004;110(11 Suppl 1):II7–12. doi: 10.1161/01.CIR.0000138978.97207.3e. [DOI] [PubMed] [Google Scholar]
- 30.D’Agostino RB. Tutorial in biostatistics: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statist Med. 1998;17:2265–81. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 31.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 32.Blackstone EH. Comparing apples and oranges. J Thorac Cardiovasc Surg. 2002;123:8–15. doi: 10.1067/mtc.2002.120329. [DOI] [PubMed] [Google Scholar]
- 33.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–8. [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–24. [Google Scholar]
- 35.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 36.Stamou SC, Jablonski KA, Pfister AJ, et al. Stroke after conventional versus minimally invasive coronary artery bypass. Ann Thorac Surg. 2002;74:394–9. doi: 10.1016/s0003-4975(02)03636-6. [DOI] [PubMed] [Google Scholar]
- 37.Grunkemeier GL, Payne N, Jin R, Handy JR., Jr Propensity score analysis of stroke after off-pump coronary artery bypass grafting. Ann Thorac Surg. 2002;74:301–5. doi: 10.1016/s0003-4975(02)03783-9. [DOI] [PubMed] [Google Scholar]
- 38.Parsons LS. Reducing bias in propensity score matched-pair sample using greedy matching techniques. 2001. Cary, NC, SAS Institute Inc. Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference, Long Beach, California, USA.
- 39.Christakis GT, Ivanov J, Weisel RD, Birnbaum PL, David TE, Salerno TA. The changing pattern of coronary artery bypass surgery. Circulation. 1989;80(Suppl I):I151–61. [PubMed] [Google Scholar]
- 40.Rao V, Ivanov J, Weisel RD, Ikonomidis JS, Christakis GT, David TE. Predictors of low cardiac output syndrome after coronary artery bypass. J Thorac Cardiovasc Surg. 1996;112:38–51. doi: 10.1016/s0022-5223(96)70176-9. [DOI] [PubMed] [Google Scholar]
- 41.Ivanov J, Tu JV, Naylor CD. Ready-made, recalibrated, remodelled? Issues in the use of risk indices for assessing mortality after coronary artery bypass graft surgery. Circulation. 1999;99:2098–104. doi: 10.1161/01.cir.99.16.2098. [DOI] [PubMed] [Google Scholar]
- 42.Tu JV, Austin P, Naylor CD, Iron K, Zhang H. Acute myocardial infarction outcomes In Ontario. In: Naylor CD, Slaughter PM, editors. Cardiovascular Health and Services in Ontario: An ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. pp. 83–110. [Google Scholar]
- 43.Alter DA, Austin P, Tu JV. Use of coronary angiography, angioplasty and bypass surgery after acute myocardial infarction in Ontario. In: Naylor CD, Slaughter PM, editors. Cardiovascular Health and Services in Ontario: An ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. pp. 141–64. [Google Scholar]
- 44.Legare J, Buth K, King S, et al. Coronary artery bypass performed off pump does not result in lower in-hospital morbidity than coronary artery bypass performed on pump. Circulation. 2004;109:887–92. doi: 10.1161/01.CIR.0000115943.41814.7D. [DOI] [PubMed] [Google Scholar]