Abstract
There is currently no promising interventional solution for in-stent stenosis in previously stented bifurcation lesions, even with drug-eluting stents. Rather than being restricted to stent struts, catheter-based local antiproliferative therapy offers the advantage of homogenous drug transfer to the whole vessel wall, and thereby allows for intracoronary pharmacotherapy without adding additional layers of metal into an already stented lesion. The newly developed GENIE catheter (Acrostak Corp, Switzerland), applied in the kissing balloon technique, allows for delivery of liquid paclitaxel into whole bifurcation lesions without repeat stent implantation. After conventional percutaneous transluminal coronary angioplasty, local delivery of paclitaxel using two GENIE catheters in the kissing balloon technique was performed in three patients (left anterior descending, left circumflex and right coronary arteries) with highly symptomatic in-stent bifurcation stenoses. The intervention was feasible and safe in all coronary arteries. Final angiography and control angiography after six months showed good results. No major adverse cardiac events occurred 30 days and six months after intervention. The patients, who represent a group at high risk of recurrent instent restenosis, remained asymptomatic since the local drug delivery. They did not require insertion of a drug-eluting stent or crossover to coronary artery bypass surgery. In conclusion, this new treatment strategy proved to be safe and effective in this first human experience and offers a promising alternative to surgery or implantation of additional stents in these patients.
Keywords: Angioplasty, Bifurcation, Local drug delivery, Paclitaxel, Restenosis
Abstract
Il n’existe pas d’intervention prometteuse en cas de sténose de l’endoprothèse aux lésions de bifurcation, même avec des endoprothèses à élution de médicament. Plutôt qu’être restreinte aux treillis de l’endoprothèse, la thérapie antiproliférative locale par cathéter offre l’avantage d’un transfert homogène du médicament à toute la paroi du vaisseau et assure donc une pharmacothérapie intracoronaire sans l’ajout d’une couche supplémentaire de métal dans une lésion déjà pourvue d’une endoprothèse. Le nouveau cathéter GENIE (Acrostak Crop, Suisse), appliqué par la technique de contact par ballonnet, permet de dispenser du paclitaxel liquide dans l’ensemble des lésions de bifurcation sans implanter une autre endoprothèse. Après une angioplastie coronarienne transluminale percutanée classique, on a administré du paclitaxel au moyen de deux cathéters GENIE par technique de contact par ballonnet chez trois patients (artère interventriculaire antérieure, artère auriculoventriculaire, artère coronaire droite) très symptomatiques en raison d’une sténose dans l’endoprothèse de la bifurcation. L’intervention était faisable et sécuritaire dans les trois artères coronaires. L’angiographie finale et l’angiographie de contrôle au bout de six mois ont révélé de bons résultats. Aucun événement cardiaque grave ne s’était produit 30 jours et six mois après l’intervention. Les patients, qui représentent un groupe très vulnérable aux récurrences de sténose de l’endoprothèse, sont demeurés asymptomatiques depuis l’administration locale du médicament. Ils n’ont pas eu besoin de se faire installer une endoprothèse à élution de médicament ou de subir un pontage aortocoronarien. Pour terminer, cette nouvelle stratégie thérapeutique s’est révélée sécuritaire et efficace dans le cadre de cette première expérience chez des humains, et elle représente une solution prometteuse par rapport à l’opération ou à l’implantation d’endoprothèses supplémentaires chez ces patients.
Treatment of coronary artery bifurcation lesions is still a major problem in interventional cardiology. A variety of different stent implantation techniques have failed to show satisfactory long-term results. For in-stent stenosis in previously stented bifurcation lesions, there is currently no promising solution, even with drug-eluting stents (1–3). Rather than being restricted to stent struts, catheter-based local antiproliferative therapy offers the advantage of homogenous drug transfer to the whole vessel wall, and thereby allows for intracoronary pharmacotherapy without adding additional layers of metal into an already stented bifurcation lesion (4).
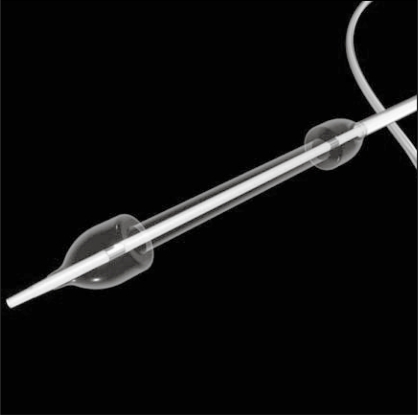
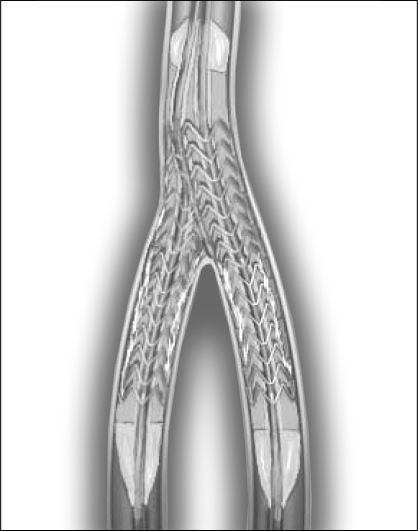
We performed local delivery of paclitaxel for treatment of in-stent restenosis in bifurcation lesions using the newly developed GENIE application device (Acrostak Corp, Switzerland). This catheter consists of a percutaneous balloon having a distal and proximal segment with occlusive function, and a central segment that allows for homogenous transfer of paclitaxel to the vessel wall (Figure 1). Three holes in the distal ramp fill the drug depot without additional trauma or hydrojets. A similar inflation of two catheters in the kissing balloon technique allows for local antiproliferative pharmacotherapy of the whole bifurcation lesion, even beyond the margins of previously implanted stents (Figure 2).
Figure 1).
Schematic drawing of the GENIE catheter (Acrostak Corp, Switzerland)
Figure 2).
Illustration of the kissing balloon technique allowing local application of liquid paclitaxel into the whole bifurcation lesion, even beyond the edges of previously implanted stents
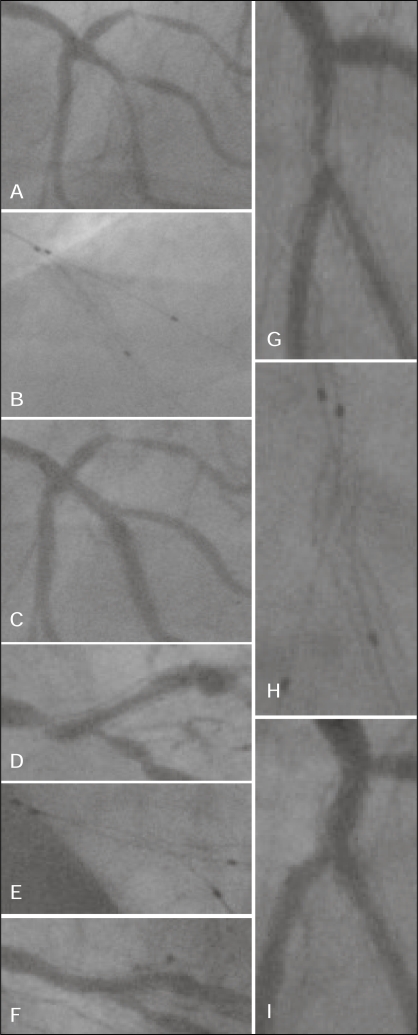
Three patients with in-stent bifurcation stenosis were included in this first human trial. The protocol for local intracoronary paclitaxel delivery was approved by the local ethics committee and the German Federal Institute for Drugs and Medical Devices. Written consent was obtained according to these formalities. Patient A was a 75-year-old man who developed in-stent restenosis six months after bare metal stent implantation in bifurcation stenosis of the left anterior descending (LAD) artery/second diagonal branch (LAD: 3.0 mm/15 mm, second diagonal branch: 2.5 mm/8 mm). Patient B was a 74-year-old man who developed in-stent restenosis five months after implantation of a drug-eluting stent (Endeavor; Medtronic, USA; 3.0 mm/12 mm) into the crux cordis of the right coronary artery (RCA). Patient C was an 81-year-old woman who suffered from in-stent restenosis six years after bare metal stent implantation into segment 13 of the left circumflex artery (3.0 mm/18mm) involving the left posterolateral artery (LAD: Figures 3A to 3C, RCA: Figures 3D to 3F, and left circumflex artery: Figures 3G to 3I).
Figure 3).
Patient A: Bifurcation lesion of the left anterior descending artery (A); two GENIE catheters (Acrostak Corp, Switzerland) in the kissing balloon technique (B); acute result (no dissections or remaining stenosis) (C). Patient B: Bifurcation lesion of the right coronary artery (D); two GENIE catheters in kissing balloon technique (E); acute result (F). Patient C: Bifurcation lesion of the left circumflex artery (G); two GENIE catheters in kissing balloon technique (H); acute result (I)
The intervention, including local drug delivery for treatment of bifurcation in-stent stenosis, was similar in all patients. After conventional percutaneous transluminal coronary angioplasty of both vessels involved in the bifurcation lesion, two GENIE catheters were introduced over a standard 6 Fr guiding catheter and two standard wires into both coronary artery branches. The balloons were inflated simultaneously at a low pressure of 2 atm, which allows for blockage of the blood stream and formation of a central chamber between the two balloon shoulders without causing mechanical trauma. This guarantees one of the key features of our local drug delivery approach – the possibility of performing pharmacotherapy independent of a mechanical, pressure-driven intervention (Figure 2). Paclitaxel was sterile filtered, diluted in 0.9% saline and prepared for application in a final concentration of 10 μM. A total of 15 mL to 20 mL of liquid paclitaxel was applied during each intervention; the inflation time of the GENIE catheters was 120 s. During this time, the drug was released from three holes in the distal balloon shoulder, filling the central drug depot. The lipophilic character of paclitaxel allows for rapid intracellular uptake within the vascular smooth muscle cells. We showed in previous studies (4–6) that even short incubation leads to long-lasting biological effects within the cell by an irreversible alteration of the cytoskeleton. The dose of 10 μM was determined by extensive preclinical testing in cell culture, organ culture and animal studies in different species. In a recent study in the pig coronary stent model (7), paclitaxel treatment via the GENIE catheter led to a significant reduction of neointimal proliferation. All coronary arteries showed complete endothelialization 42 days following treatment in this animal model.
The intervention was feasible and safe in all patients (representing all three main coronary arteries). Inflation and intervention in the kissing balloon technique, as well as the withdrawal of both drug delivery catheters, were easily performed, even in the distal RCA, and led to no procedural problems. Final angiography showed excellent acute results (no dissections or remaining stenoses) in all cases. No local or systemic side effects were detected after the intracoronary application of paclitaxel by continuous hemodynamic monitoring, repeated electrocardiogram controls and blood samples. Safety and efficacy of a local paclitaxel treatment via the GENIE catheter for preventing in-stent restenosis in de novo lesions is currently also being evaluated in a randomized, prospective clinical trial in more than 200 patients (LOCAL TAX Study; unpublished data).
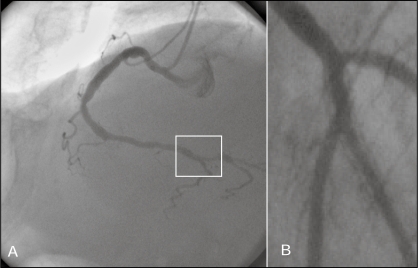
No major adverse cardiac events occurred 30 days and six months after the intervention. The patients, who represent a cohort normally scheduled for coronary artery bypass graft surgery, have stayed asymptomatic. Patients B and C underwent repeat coronary angiography six months after the intervention (Figures 4A and 4B), with excellent long-term results and no restenosis or need for target lesion revascularization. Patient A, who was relieved from angina pectoris, refused repeat angiography while being asymptomatic.
Figure 4).
Patient B: Bifurcation lesion of the right coronary artery six months after intervention. The white box indicates the former intervention area (A). Patient C: The left circumflex artery bifurcation lesion six months after local delivery of paclitaxel, showing a good long-term result with a patent vessel lumen (B)
In conclusion, the use of two GENIE catheters in the kissing balloon technique for local antiproliferative therapy of in-stent stenosis in bifurcation lesions can easily be performed in all coronary arteries without procedural problems, and led to excellent results in the present first human study. This treatment strategy offers considerable conceptual advantages over a repeated stent implantation, because it allows for homogenous local antiproliferative pharmacotherapy of coronary artery bifurcation lesions without the disadvantages of a second stent and its coating material. Thus, local antiproliferative therapy using the GENIE catheter in the kissing balloon technique for therapy of in-stent bifurcation lesions is a completely new and promising therapy for a clinical problem that has been very difficult to treat thus far.
REFERENCES
- 1.Sianos G, Vaina S, Hoye A, Serruys PW. Bifurcation stenting with drug eluting stents: Illustration of the crush technique. Catheter Cardiovasc Interv. 2006;67:839–45. doi: 10.1002/ccd.20742. [DOI] [PubMed] [Google Scholar]
- 2.Shuchman M. Debating the risks of drug-eluting stents. N Engl J Med. 2007;356:325–8. doi: 10.1056/NEJMp068300. [DOI] [PubMed] [Google Scholar]
- 3.Finn AV, Nakazawa G, Joner M, et al. Vascular responses to drug eluting stents: Importance of delayed healing. Arterioscler Thromb Vasc Biol. 2007;27:1500–10. doi: 10.1161/ATVBAHA.107.144220. [DOI] [PubMed] [Google Scholar]
- 4.Herdeg C, Oberhoff M, Baumbach A, et al. Local paclitaxel delivery for the prevention of restenosis: Biological effects and efficacy in vivo. J Am Coll Cardiol. 2000;35:1969–76. doi: 10.1016/s0735-1097(00)00614-8. [DOI] [PubMed] [Google Scholar]
- 5.Axel DI, Kunert W, Göggelmann C, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96:636–45. doi: 10.1161/01.cir.96.2.636. [DOI] [PubMed] [Google Scholar]
- 6.Herdeg C, Oberhoff M, Baumbach A, et al. Visualization and comparison of drug effects after local paclitaxel delivery with different catheter types. Basic Res Cardiol. 1999;94:454–63. doi: 10.1007/s003950050161. [DOI] [PubMed] [Google Scholar]
- 7.Dommke C, Haase KK, Süselbeck T, et al. Local paclitaxel delivery after coronary stenting in an experimental animal model. Thromb Haemost. 2007;98:674–80. [PubMed] [Google Scholar]