Abstract
Objectives. Using prospectively collected registry data to investigate sick leave (sickness benefit and sickness compensation) over a 7-yr period in patients with AS in comparison with population-based controls matched for age, sex and residential area.
Methods. We investigated 122 (21 women and 101 men) outpatients with AS in South Sweden, born 1942 or later, from rheumatology specialist care for their sick leave during a 7-yr period. Mean (s.d.) age was 43 (11) yrs and mean (s.d.) disease duration was 20 (11) yrs. Two controls per case, matched for age, sex and residential area were selected from the Swedish National Population Register. Data concerning sick leave for cases and controls, based on the subjects’ unique 10-digit personal identification number, were retrieved from the national register of the Swedish Social Insurance Agency.
Results. More AS patients than controls were registered for sickness benefit (52 vs 36%, P < 0.01) and sickness compensation (42 vs 11%, P < 0.001). Cases had an increased risk for sick leave compared with controls with a relative risk of 1.8; 95% CI 1.5, 2.1; and cases had more days with sick leave than controls (median number of more days per year 30; 95% CI 2, 72).
Conclusions. Using the Swedish Social Insurance Agency's registers for sick leave, we found that patients with AS in rheumatology specialist care in South Sweden have an increased level of sick leave compared with controls. These population-based registers have a great potential for studies of the effects of different interventions on sick leave.
Keywords: Ankylosing spondylitis, Sick leave, Work disability, Controlled study, Register
Introduction
AS is a chronic, inflammatory rheumatic disease with an unknown aetiology. Prevalence and incidence in the western world are estimated at 0.2% and 6/100 000 per year, respectively, and the disease is more prevalent among men [1]. The disease usually starts between 15 and 30 yrs of age. Disease manifestations, such as pain and stiffness in the axial skeleton and in some cases also peripheral arthritis, enthesitis and extra-articular manifestations, contribute to impairment, activity limitation, participation restriction and reduced quality of life [2–4]. Reduced work ability leading to sick leave is a common consequence of AS [5, 6] and may contribute to psychosocial and financial (direct and indirect) sequels for the individual as well as for the society [7, 8]. For decades the most common treatment for AS was NSAIDs and physical therapy. The treatment options have recently been broadened by TNF inhibitors with beneficial effect on disease activity, function, sick leave and quality of life [9–11]. Employment status in patients with AS of varying disease duration ranges between 55 and 89% in different countries [12]. Proportion of work-disabled patients with AS is reported to vary between 9 and 36% [12]. Differences seen in employment status and work disability between countries may be partly due to differences in social security systems and different labour markets [12]. The main purpose of this registry-based case–control study was to investigate sick leave over a 7-yr period in a cohort of patients with AS in Malmö, South Sweden, compared with controls matched for age, sex and residential area. The Swedish Social Insurance Agency continuously registers compensation for sick leave paid to all residents by their unique personal identification number, and cross-referencing this registry with a disease cohort may provide the foundation for high-quality research on sick leave and health economics.
Subjects and methods
Definitions
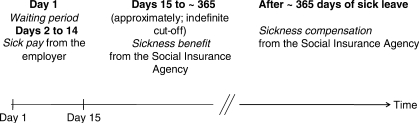
According to the Swedish legislation, all residents aged 16–64 yrs can be granted economic security from the Swedish Social Insurance Agency in the event of work incapacity owing to sickness, disability or injuries [13]. Different forms of benefit are sick pay, sickness benefit and sickness compensation, which are all income-related benefits (Fig. 1).
Fig. 1.
Description of different forms of benefits for individuals with sick leave according to the Swedish Social Insurance system.
The waiting period or the qualifying day is the first day of illness. No benefit is paid for this day.
Sick pay is benefit for the 2nd to the 14th days of illness, and is paid directly from the employer. Sick periods 14 days or shorter are therefore not registered by the Swedish Social Insurance Agency.
Sickness benefit is compensation for illness that reduces work capacity by at least one-quarter for a limited time. It is generally limited to 1 yr, and can be payable as full, three-quarters, half or one-quarter benefit depending on the reduction in work capacity. Sickness benefit may be approved from Day 15 of sick leave.
Sickness compensation (before 2003 referred to as disability pension) can be granted to insured individuals with a permanent or long-term (at least 1 yr) full or partial incapacity for work due to illness or some other impairment of their physical or mental capacity for work. Sickness compensation is paid to insured persons aged 30–64 yrs and can be granted for either an indefinite or a limited period. Sickness compensation is payable as full, three-quarters, half or one-quarter benefit, depending on the extent of the reduction in work capacity.
Sick leave is in the present study defined as days with sickness benefit and days with sickness compensation registered at the Swedish Social Insurance Agency. The first 14 days of illness (waiting period/qualifying day and sick pay period) are not included in the sick leave.
Study sample
Entry criteria for the patients included in this study were: men and women born 1942 or later (⩽65 yrs in 2007), living in the region of Skåne in South Sweden, and registered for consultation at a doctor in the rheumatology specialist care in Malmö between 1993 and 2006 with diagnosis of AS according to the New York criteria [14] verified in the patient records. Malmö is a city in Skåne with a population of 230 000 individuals over the age of 15 yrs. At the time of inclusion, the rheumatology specialist care in Malmö comprised of the Rheumatology Department of the University Hospital in Malmö and three rheumatologists practicing privately in the city. These rheumatology specialists were connected to the hospital clinic by a special contract and were an integrated part of the rheumatology service and the rheumatology team in Malmö [15].
Patients were identified from the outpatient registers of the Rheumatology Department of the University Hospital and the three rheumatologists practicing privately. Patients were included if they had AS according to ICD-9 (720A) or ICD-10 (M45) or, when no code was available (in two of the private practices’ registers), a written diagnosis of AS, pelvospondylitis or Mb Bechterew was present. A total of 158 patients, 120 men and 38 women, were identified. To verify the diagnosis, one of the authors (B.S.) examined their medical records and found that 36 patients, 19 men and 17 women, did not fulfil the New York criteria for diagnosis and were excluded. Thus, in all 122 patients, 101 men and 21 women were included in the study. To further validate and characterize the study sample the prevalence of uveitis was registered from the medical records and information of treatment with TNF-inhibitors was collected from the South Swedish Arthritis Treatment Group (SSATG) register [16]. Using the National Population Register, we selected two controls per case matched for age (the same birth date or as close as possible to the same birth date), sex and residential area (zip code).
For 61 of the 122 patients with AS included in the present study, disease activity and functional status were assessed in 2004 (a time-point which is included in the follow-up time of the present study) in an earlier separate project concerning health-related quality of life in patients with AS (data not published). These 61 patients were included in a post hoc correlation analysis in the present study (see below).
Sick leave data
Based on the subjects’ unique 10-digit personal identification number we retrieved data concerning sick leave (number of days with sickness benefit and number of days with sickness compensation) for cases and controls from the Swedish Social Insurance Agency. The data included all sick leave for both cases and controls, i.e. for the cases, sick leave was both related and unrelated to the diagnosis of AS. Data contained dates of sick leave and degree of sick leave (25, 50, 75 or 100% of the day). The follow-up time for sick leave of cases and controls was from 1 January 2000 until 31 January 2007. When the follow-up time was interrupted (e.g. due to death or relocation out of the region) for either a case or any of its controls, the follow-up time was interrupted for all three of them, i.e. a case and its two controls always had the same length of follow-up time.
Correlations
For a post hoc evaluation of the correlation between sick leave and disease activity and sick leave and functional status, respectively, we used data from an earlier project for a subgroup (n = 61, see above) of the 122 patients with AS included in the present study. The well-validated instruments Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [17, 18] and Bath Ankylosing Spondylitis Functional Index (BASFI) [19, 20] were used for assessment of disease activity and functional status.
Statistical methods
We used the Cochran–Mantel–Haenszel test to evaluate differences in frequencies of sick leave. For risk analysis of being on sick leave stratified Cox regression with equal follow up times for patients and controls and robust variance estimator was used. As secondary analysis the median of the difference in number of days on sick leave between patients and controls was counted. The 95% CI for the median was evaluated using the bootstrapping method with respect to matching [21]. Due to the small number of women included in the study, the results for men and women are presented together. Correlations were performed by using the Spearman rank correlation coefficient (rs). All P-values were two-tailed and we considered a P-value of 0.05 or less as statistically significant. Analyses were done using SAS software 9.1, Copyright 2002–03, SAS Institute Inc. and R 2.5.1 (http://www.r-project.org/).
Ethical approval
The regional ethics board of the University of Lund approved the study (No. 514/2007).
Results
Characteristics
Mean (s.d.) age for cases and controls was 43 (11) yrs and mean (s.d.) disease duration (time since debut) for the cases were 20 (11) yrs. The mean (s.d.) follow-up time for sick leave was 6.4 (1.6) yrs for both cases and controls. Forty patients (33%) had ever been treated for uveitis and 26 patients (21%) had been treated with TNF-inhibitors (Table 1).
Table 1.
Characteristics of the patients with AS (the main group, n = 122) the controls (n = 366) and the subgroup of patients with AS (n = 61) with BASDAI and BASFI data available
| Characteristics | AS patients n = 122 | Controls n = 366 | AS patients (subgroup) n = 61 |
|---|---|---|---|
| Women, n (%) | 21 (17) | 44 (17) | 10 (16) |
| Age, mean (s.d.)a, years | 43 (11) | 43 (11) | 44 (11) |
| Disease duration, mean (s.d.)a, years | 20 (11) | – | 20 (13) |
| Follow-up time, mean (s.d.), years | 6.4 (1.6) | 6.4 (1.6) | 6.8 (0.7) |
| HLA-B27, n (%) | |||
| Positive | 67 (55) | – | 29 (48) |
| Negative | 5 (4) | – | 3 (4) |
| Not tested | 50 (41) | – | 29 (48) |
| Uveitis, n (%) | 40 (33) | – | 21 (34) |
| Treated with TNF-inhibitors, n (%) | 26 (21) | – | NA |
| BASDAI, mean (s.d.) | NA | – | 4 (2.4) |
| BASFI, mean (s.d.) | NA | – | 3.7 (2.4) |
aAt start of follow-up. NA = not assessed.
Sick leave
During the follow-up period there were more AS cases than controls that were registered for sickness benefit (52 vs 36%, P < 0.01) and sickness compensation (42 vs 11%, P < 0.001). Thirty percent of the cases and 58% of the controls had no registered sick leave days at all during the follow-up period. AS patients had an increased risk for sick leave (i.e. either sickness benefit and/or sickness compensation) compared with controls with a relative risk of 1.8; 95% CI 1.5, 2.1 over the 7-yr period.
The increased risk for sick leave for patients younger than 45 yrs was 2.1; 95% CI 1.6, 2.8, and for patients older than 45 yrs 1.6; 95% CI 1.3, 2 (P-value for difference = 0.07). This indicates that age tends to weaken the effect of the AS disease on sick leave. AS patients had more days of sick leave than controls. Median [quartile (Q) 1, Q3] value for number of days with sick leave of any rate (25, 50, 75 and 100%) per year was 50 (0, 317) for cases and 0 (0, 11) for controls. Median (Q1, Q3) value for sick leave rate adjusted to number of days with 100% sick leave per year was 43 (0, 199) for cases and 0 (0, 10) for controls. The difference in number of days with sick leave (days with sickness benefit or sickness compensation of any degree) per year between patients and controls was median 30 days; 95% CI 2, 72.
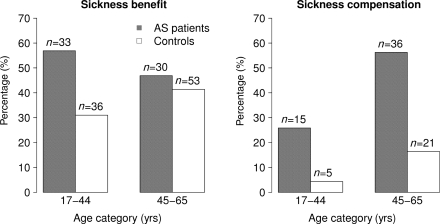
The proportion of persons with sick leave increased with age— persons 45 yrs and older had a higher level of sick leave than persons younger than 45 yrs (Fig. 2).
Fig. 2.
Proportions of patients with AS and controls with sickness benefit and sickness compensation of any extent (25, 50, 75 and 100%) during the follow-up period. Groups are divided based on the individuals being younger than 45 yrs and 45 yrs or older at the time of the investigation.
Post hoc analysis
The characteristics of the subgroup of patients with AS (n = 61) with BASDAI and BASFI data available did not substantially differ from the subjects without such data (Table 1). Mean BASDAI and BASFI was 4 and 3.7, respectively. Median (Q1, Q3) value for number of days with sick leave of any rate (25, 50, 75 and 100%) per year was 49 (0, 307) and median (Q1, Q3) value for sick leave rate adjusted to number of days with 100% sick leave per year was 38 (0, 232).
There was no statistically significant correlation between number of sick leave days and BASDAI (rs = 0.15) or BASFI (rs = 0.18), respectively.
Discussion
In contrast to what many clinicians assume, patients with AS have increased sick leave. Our population-based case–control study, which is to the best of our knowledge the first study presenting Swedish sick leave data for this patient category, shows an 80% increased risk of sick leave over a 7-yr period. The sick leave data were collected from an independent, reliable and identical source for both cases and controls as sick leave over 14 days for all residents leading to compensation is continuously registered by the Swedish Social Insurance Agency.
Our findings are in concordance with earlier reports, [7, 8, 12, 22] and some of these have presented data allowing interpretation of work participation in relation to the general population. Boonen et al. [7] described that the risk for withdrawal from work in the Netherlands was about 3-times higher in patients with AS, and that work disability in three European countries was higher than expected in the general population [8]. Mau et al. [22] compared employment rates in different rheumatic diseases with the general German population and found that there were differences, but smaller than expected, especially in AS. However, the differences increased with longer disease duration [22]. The employment rate in patients with AS was higher than in patients with RA from the German rheumatological database [23]. Due to heterogeneity of populations studied, differences in definitions of end-points and methodology used, as well as in labour markets and social security systems, comparisons between countries may be difficult to interpret.
Since patients in our study were recruited from rheumatological specialist care they can be expected to have a higher disease activity and to be more severely affected and as all the included patients fulfilled the New York criteria for the diagnosis of AS, early disease might not be included. The sick leave may therefore not be representative for the whole spectrum of disease [24].
The mechanisms causing the increased sick leave are multiple, with contribution by disease-related factors, work-related factors, sociodemographic factors, mental factors as well as coping styles [7, 12, 25–29]. In our study, sick leave was not associated with disease activity or function, which could indicate that other, not evaluated, factors influence the degree of sick leave [25, 27–29]. During recent years effective anti-inflammatory and disease-modifying treatment with TNF inhibitors have become increasingly available. In fact, 21% of our patients had received such therapy, which may have affected their sick leave. However, serving as a limitation, our study sample was too small to evaluate if TNF inhibitor treatment was associated with work disability. Also, our data do not include shorter periods (up to 14 days) of sick leave as these periods are directly compensated by the employer and never get registered by the Swedish Social Security Agency. It is possible that AS patients also have an increase of such brief periods of sick leave compared with controls, and therefore our estimates of increased risk may be biased towards the null.
To sum up, we have demonstrated that AS patients in Sweden have an increased sick leave level, despite the introduction of TNF inhibitors in the treatment arsenal. We also demonstrate the large potential for work disability studies that is possible by using the Swedish population-based registers for health care and social insurance benefits [30, 31]. These registers form an exciting possibility for evaluation of treatment interventions, such as team-based rehabilitation [32] and biologic pharmacological treatment [16].
Acknowledgements
We thank Gunnel Henriksson, Thor Lithman and Dennis Noréen for help with data retrieval and management and excellent technical support.
Funding: The project was funded by a grant from the Regional Health Service Authorities in Skåne (Region Skåne) and the Swedish Social Insurance Agency (Försäkringskassan). Funding to pay the Open Access publication charges for this article was provided by the Musculoskeletal Research Center, University Hospital, Lund, Sweden.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Silman A. Ankylosing spondylitis and spondylarthropathies. In: Silman AJHM, editor. Epidemiology of the rheumatic diseases. Oxford: University Press; 2001. pp. 100–11. [Google Scholar]
- 2.Boonen A. A review of work-participation, cost-of-illness and cost-effectiveness studies in ankylosing spondylitis. Nat Clin Pract Rheumatol. 2006;2:546–53. doi: 10.1038/ncprheum0297. [DOI] [PubMed] [Google Scholar]
- 3.Dagfinrud H, Mengshoel AM, Hagen KB, Loge JH, Kvien TK. Health status of patients with ankylosing spondylitis: a comparison with the general population. Ann Rheum Dis. 2004;63:1605–10. doi: 10.1136/ard.2003.019224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Echteld I, Cieza A, Boonen A, et al. Identification of the most common problems by patients with ankylosing spondylitis using the international classification of functioning, disability and health. J Rheumatol. 2006;33:2475–83. [PubMed] [Google Scholar]
- 5.Boonen A, Chorus A, Miedema H, van der Heijde D, van der Tempel H, van der Linden S. Employment, work disability, and work days lost in patients with ankylosing spondylitis: a cross sectional study of Dutch patients. Ann Rheum Dis. 2001;60:353–8. doi: 10.1136/ard.60.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gran JT, Skomsvoll JF. The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol. 1997;36:766–71. doi: 10.1093/rheumatology/36.7.766. [DOI] [PubMed] [Google Scholar]
- 7.Boonen A, Chorus A, Miedema H, et al. Withdrawal from labour force due to work disability in patients with ankylosing spondylitis. Ann Rheum Dis. 2001;60:1033–9. doi: 10.1136/ard.60.11.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boonen A, van der Heijde D, Landewe R, et al. Work status and productivity costs due to ankylosing spondylitis: comparison of three European countries. Ann Rheum Dis. 2002;61:429–37. doi: 10.1136/ard.61.5.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braun J, Brandt J, Listing J, et al. Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. Lancet. 2002;359:1187–93. doi: 10.1016/s0140-6736(02)08215-6. [DOI] [PubMed] [Google Scholar]
- 10.Listing J, Brandt J, Rudwaleit M, Zink A, Sieper J, Braun J. Impact of anti-tumour necrosis factor alpha treatment on admissions to hospital and days of sick leave in patients with ankylosing spondylitis. Ann Rheum Dis. 2004;63:1670–2. doi: 10.1136/ard.2003.017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Heijde D, Dijkmans B, Geusens P, et al. Efficacy and safety of infliximab in patients with ankylosing spondylitis: results of a randomized, placebo-controlled trial (ASSERT) Arthritis Rheum. 2005;52:582–91. doi: 10.1002/art.20852. [DOI] [PubMed] [Google Scholar]
- 12.Boonen A, van der Linden SM. The burden of ankylosing spondylitis. J Rheumatol. 2006;78:4–11. [PubMed] [Google Scholar]
- 13.Swedish Social Insurance Agency. [(27 March 2008, date last accessed)]; www.forsakringskassan.se/sprak/eng.
- 14.van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27:361–8. doi: 10.1002/art.1780270401. [DOI] [PubMed] [Google Scholar]
- 15.Jacobsson L, Lindroth Y, Marsal L, Tejler L. [The Malmo model for private and public rheumatological outpatient care. Cooperation makes it possible to introduce disease modifying treatment quickly] Lakartidningen. 2001;98:4710–6. [PubMed] [Google Scholar]
- 16.Geborek P, Nitelius E, Noltorp S, et al. Population based studies of biological antirheumatic drug use in southern Sweden: comparison with pharmaceutical sales. Ann Rheum Dis. 2005;64:1805–7. doi: 10.1136/ard.2005.036715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21:2286–91. [PubMed] [Google Scholar]
- 18.Waldner A, Cronstedt H, Stenstrom CH. The Swedish version of the Bath Ankylosing Spondylitis Disease Activity Index. Reliability and validity. Scand J Rheumatol. 1999;111:10–6. [PubMed] [Google Scholar]
- 19.Calin A, Garrett S, Whitelock H, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol. 1994;21:2281–5. [PubMed] [Google Scholar]
- 20.Cronstedt H, Waldner A, Stenstrom CH. The Swedish version of the Bath Ankylosing Spondylitis Functional Index. Reliability and validity. Scand J Rheumatol. 1999;111:1–9. [PubMed] [Google Scholar]
- 21.Davidsson ACHD. Cambridge: University Press; 1997. Bootstrap methods and their application. [Google Scholar]
- 22.Mau W, Listing J, Huscher D, Zeidler H, Zink A. Employment across chronic inflammatory rheumatic diseases and comparison with the general population. J Rheumatol. 2005;32:721–8. [PubMed] [Google Scholar]
- 23.Zink A, Braun J, Listing J, Wollenhaupt J. Disability and handicap in rheumatoid arthritis and ankylosing spondylitis–results from the German rheumatological database. German collaborative arthritis centers. J Rheumatol. 2000;27:613–22. [PubMed] [Google Scholar]
- 24.Gran JT, Husby G. Ankylosing spondylitis: a comparative study of patients in an epidemiological survey, and those admitted to a department of rheumatology. J Rheumatol. 1984;11:788–93. [PubMed] [Google Scholar]
- 25.Boonen A, Chorus A, Landewe R, et al. Manual jobs increase the risk of patients with ankylosing spondylitis withdrawing from the labour force, also when adjusted for job related withdrawal in the general population. Ann Rheum Dis. 2002;61:658. doi: 10.1136/ard.61.7.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boonen A, de Vet H, van der Heijde D, van der Linden S. Work status and its determinants among patients with ankylosing spondylitis. A systematic literature review. J Rheumatol. 2001;28:1056–62. [PubMed] [Google Scholar]
- 27.Chorus AM, Boonen A, Miedema HS, van der Linden S. Employment perspectives of patients with ankylosing spondylitis. Ann Rheum Dis. 2002;61:693–9. doi: 10.1136/ard.61.8.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guillemin F, Briancon S, Pourel J, Gaucher A. Long-term disability and prolonged sick leaves as outcome measurements in ankylosing spondylitis. Possible predictive factors. Arthritis Rheum. 1990;33:1001–6. doi: 10.1002/art.1780330712. [DOI] [PubMed] [Google Scholar]
- 29.Ward MM, Kuzis S. Risk factors for work disability in patients with ankylosing spondylitis. J Rheumatol. 2001;28:315–21. [PubMed] [Google Scholar]
- 30.MORSE. [(27 March 2008, date last accessed)]; www.morse.nu.
- 31.NKO. [(27 March 2008, date last accessed)]; www.nko.se/en.
- 32.Iversen MD, Petersson IF. Design issues and priorities in team and nonpharmacological arthritis care research. J Rheumatol. 2006;33:1904–7. [PubMed] [Google Scholar]