Abstract
We conducted a systematic review to evaluate the efficacy and safety of Chinese herbal medicine (CHM) for dysfunctional uterine bleeding (DUB) by performing a meta-analysis. Randomized controlled trials (RCTs) or quasi-RCTs comparing CHM vs no treatment, placebo, conventional western medicine (CWM), or general non-specific surgical treatment for DUB were identified by electronic and manual searches. Trials of CHM treatments with CWM treatments were compared with CWM treatments alone. Jadad scale and allocation concealment were used to assess the quality of included studies. Four RCTs or quasi-RCTs involving 525 patients were included. The methodological quality was poor in all trials except one trial. No serious adverse events were reported in the included studies. With the lack of trials comparing CHM with no treatment or placebo, it is impossible to accurately evaluate the efficacy of CHM. However, CHM in these studies seem to show an encouraging comparative effectiveness with CWM. More RCTs with a higher quality are required.
Keywords: Chinese herbal medicine, dysfunctional uterine bleeding, meta-analysis, randomized controlled trials, systematic review
Background
Dysfunctional uterine bleeding (DUB) is defined as abnormal uterine bleeding without a demonstrable organic cause (1). It is a commonly encountered gynecologic disease. DUB occurs most commonly at the extremes of reproductive age (20% of cases occur in adolescence and 40% in patients over age 40) (2). DUB can be divided into ovulatory and anovulatory. In adolescent and perimenopausal age groups, 90% of DUB is anovulatory (3).
The goals of treatment for DUB are to control acute bleeding, avert future episodes of bleeding, prevent serious long-term consequences of anovulation and endometrial cancer (4). DUB can be treated medically or surgically. Management depends on the age and needs of the patient.
In China, due to the long co-existence of conventional western medical hospitals and traditional Chinese medical hospitals, people are usually exposed to a combination of western and Chinese therapies. As the communication between China and other countries around the world becomes more interactive and the international policies of herbal medicine are improved step by step, Chinese herbal medicine (CHM) will become more and more available throughout the world.
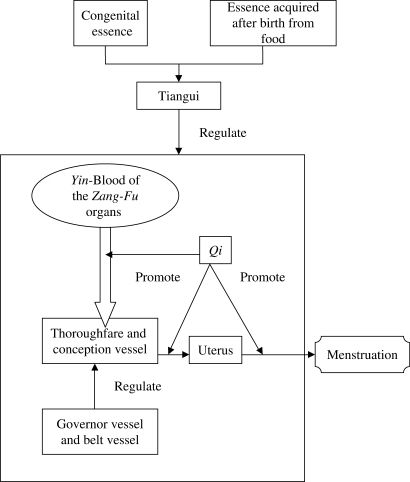
In TCM basic theory, Kidney-Qi is composed of Kidney-yang and Kidney-yin. Kidney-yang warms and promotes the growth of tissues and organs in the human body. Kidney-yin moistens and nourishes the viscera, tissues and organs. The balance of Yin and Yang in Zang-Fu organs is the motive power for the formation of Qi and Blood. Blood is the substantial basis of menstruation and the circulation of blood and menstruation depends on the promotion of Qi. In TCM theory the most important mechanism for the generation of menstruation is the co-ordinative effect of Kidney-Qi, Tiangui, thoroughfare, conception vessels (Chong Channel and Ren meridian) and the uterus. The Tiangui is a kind of substance necessary for promoting the development and maturity of the gonad. This is generated and derived from congenital essence and strengthened by essence acquired after birth from food. Tiangui begins to play its motivational role of generating menstruation, while the thoroughfare (the sea of blood and twelve meridians) and conception vessel (the sea of Yin meridians) are strengthened by the Qi and blood of Zang–Fu organs and adjusted by the governor (Du Channel, the sea of Yang meridians) and belt vessels (Dai Channel). The belt vessel restrains all the up-and-down meridians and the normal physiologic excretions of the uterus, accumulating Yin-Blood of the viscera under the influence of Tiangui. Yin-Blood fills the sea of blood over time, flows into the uterus and changes into menstruation. In TCM, these cycles are the generating mechanism of menstruation (Fig. 1).
Figure 1.
Generating mechanism of menstruation in TCM.
According to clinical manifestations, DUB is similar to other aspects of irregular menstruation such as metrorrhagia, metrostasis and intermenstrual bleeding in Traditional Chinese Medicine (TCM) (5). In TCM theory, DUB is usually caused by the following: insufficiency of qi, blood heat, blood stasis due to insufficiency of kidney-qi or kidney-yin, insufficiency of spleen, or weakness of the thoroughfare and conception vessels. The therapeutic methods vary according to different manifestations. Three therapeutic principles most often used to treat metrorrhagia and metrostasis are: to stop bleeding, determine the cause and deal with the principal aspect and most importantly, restore normal menstruation.
Rats injected with androgen became anovulia. Chinese herbal medicinal compound prescriptions were given to the rats which increased the weight of the ovaries and uterus and thickened the endometria. The herbal compounds could also increase the quantity of glands in the endometrium, folliculi and corpus luteum and make the interstitial glands to become prosperous (6). The herbal compounds can also ameliorate the morphosis of the adenohypophysis and adjust the endocrine function of the adenohypophysis. Hence, they can promote ovarian follicle growth, corpus luteum formation and ovulation (7).
CHM has been widely used to treat DUB in China and many clinical trials have been conducted to investigate their efficacy. These trials, however, could not provide evidence because of the poor quality of their methodology. Thus, it is necessary to assess CHM in terms of no treatment or placebo and also to compare CHM with conventional western medicine (CWM). Furthermore, it should be determined by systematic review whether CHM offers any advantage when combined with conventional western therapies for the treatment of DUB.
Methods
Truly or quasi-randomized controlled trials (RCTs) of CHM for DUB were included, regardless of whether the intervention was blinded to patients, clinicians or researchers after randomization was done. Trials that compared CWM with CHM in the control arm were also included. Trials using animals or their processed products were excluded. To keep the integrity of TCM, processed products from minerals and animal excretions were permitted to be used as adjunct drugs in this review. All eligible literature was included regardless of language. In accordance with our main purpose outlined above, the trials that used CHM in both the treatment and control groups were excluded, as well as the trials that did not report diagnostic criteria.
Participants
DUB diagnosis was based on ruling out organic causes classified into three categories: pelvic pathology, systemic diseases and iatrogenic causes for abnormal bleeding (excluding pregnancy) (8). Only patients with histories, clinical symptoms, physical examinations and supplementary test data that showed no organic disorder with any type of DUB were eligible. Patients suffering from bleeding due to pregnancy, use of an intrauterine contraceptive device (IUD) or systemic disease or disorder were excluded.
Interventions
Experimental treatment included CHM (different agents, doses and routes of administration). Control treatment included no intervention, placebo, CWM or general non-specific surgery. The treatment group received CHM in conjunction with western medical treatment. The control group received the same western medical treatment with no adjunct therapies. Three conventional western medical treatments were used. The first treatment included a treatment for anemia secondary to DUB, the second was a hemostat agent treatment and the third was hormonal therapy. General non-specific surgery was defined as dilatation and curettage (D&C), hysterectomy and endometrial ablation.
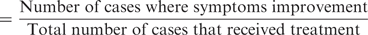
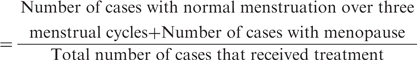
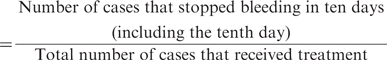
Outcome Measures
Considering that the outcome measures of most TCM studies are based on clinical research guidelines invented by the Chinese State Administration of TCM, six main outcomes were considered:
-
Total effect rate
-
Normalization rate of menstruation
-
Hemostasis rate
The amount of menstrual blood loss.
-
Recurrence rate
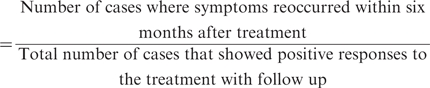
Adverse effects during treatment period that were recorded.
Search Strategy for Identification of Studies
Following databases were searched for relevant studies: PubMed, CBM disk (Chinese Biomedical Disk), CJFD (Chinese Journal Full-text Database), DOCFT (Dissertation of China, full-text), CSTJ (Chinese Scientific and Technological Journals Database). Every database was searched from its starting date to 2006 in Chinese and English. The search strategy on CBM disk is illustrated in Table 1. Thirty-two Chinese professional journals were manually searched (Table 2).
Table 1.
Search strategy on CBM disk
| 1 Explode ‘Functional Uterine Bleeding’/all subheadings |
| 2 Dysfunctional Uterine Bleeding |
| 3 1 OR 2 |
| 4 Explode ‘Drugs, Chinese Herbal’/all subheadings |
| 5 Chinese Herbal Drugs |
| 6 Medicinal Herbs |
| 7 Traditional Chinese Medicine |
| 8 4 OR 5 OR 6 OR 7 |
| 9 3 AND 8 |
Table 2.
Hand searching Chinese professional journals (1980.1–2006.1)
| Acta Chinese Medicine and Pharmacology; Beijing Journal of Traditional Chinese Medicine; Chinese Journal of Basic Medicine in Traditional Chinese Medicine; Chinese Journal of integrated traditional and western medicine; Chinese Traditional and Herbal Drugs; Chinese Traditional Patent Medicine; China Journal of Chinese Materia Medica; Chinese Journal of Information on Traditional Chinese Medicine; Chinese Journal of Obstetrics and Gynecology; Chinese Journal of Traditional Medical Science And Technology; Forum on Traditional Chinese Medicine; Fujian Journal of Traditional Chinese Medicine; Guangming Journal of Chinese Medicine; Hubei Journal of Traditional Chinese Medicine; Heilongjiang Journal of Traditional Chinese Medicine; International Journal of Traditional Chinese Medicine; Journal of Beijing University of Traditional Chinese Medicine; Journal of Traditional Chinese Medicine University of Hunan; Journal of Shanxi College of Traditional Chinese Medicine; Journal of Emergency in Traditional Chinese Medicine; Jiangsu Journal of Traditional Chinese Medicine; Journal of Gansu college of Traditional Chinese Medicine; Journal of Traditional Chinese Medicinal Literature; Journal of Traditional Chinese Medicine; Journal of Nanjing University of Traditional Chinese Medicine; Jilin Journal of Traditional Chinese Medicine; New Journal of Traditional Chinese Medicine; Shandong Journal of Traditional Chinese Medicine; Shanghai Journal of Traditional Chinese Medicine; Shanxi Journal of Traditional Chinese Medicine; Traditional Chinese Medicinal Research; Zhejiang Journal of Traditional Chinese Medicine. |
Data Collection
Data were collected independently by two reviewers. Reviewers should solve discrepancies between them by discussion if some discrepancies exist. If they were unable to solve the disagreement through discussion, authors were contacted to clarify the details.
Quality Assessment
Jadad scale and allocation concealment were used to score the quality of the included studies. Based on scores, we broadly subdivided them into the following two categories: the total score is 5; those scoring below 3 classified as low quality and 3–5 as high quality. Allocation concealment was assessed according to Revman 4.2.7 User Guide. A, B, C, D was used to indicate the quality of concealment: A indicates adequate concealment of the allocation; B indicates uncertainty that concealment was adequate; C indicates inadequate concealment; D indicates the score was not assigned (9).
Data Analysis
Data were analyzed using Revman 4.2.7 downloaded from the website of Cochrane collaboration. Meta-analysis was performed for the data. The dichotomous data were expressed as odds ratio (OR) with corresponding 95% confidence interval (95%CI). For continuous data, weighted mean difference (WMD) and 95%CI were calculated. Heterogeneity was tested by χ2 test.
The comparison (Tables 6–7) was split into two parts: first comparing CHM with CWM and second, comparing CHM plus CWM to CWM alone. Although the constituents of the compounds were different in each investigation, the whole compounds of CHM had to exhibit some of the following benefits of nourishing kidney and qi, strengthening spleen and clearing away heat, or invigorate the thoroughfare and conception vessels and stop bleeding. A process was designed to combine across studies to perform a meta-analysis. If the main effects of the whole compound in the studies were similar, the data was combined. The fixed-effect mode was used to combine dichotomous data if homogeneity was found. If heterogeneity was found, the random effect mode was alternatively used. To make the meta-analysis more clinically meaningful, trials with different hormonal therapies involving a combination with necessary hemostat agent treatment for anemia secondary to DUB were lumped together. In the treatment of DUB, if one kind of hormone is not so effective, another kind of hormone may be alternatively used. Publication bias would be examined by the funnel plot.
Table 6.
Chinese herbal medicine vs conventional western medicine
| Outcome measures | Trials | Participants |
Statistical method | Odds ratio (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| CHM group | CWM group | |||||
| Total effect rate | ||||||
| Du (12) | 123/174 | 100/142 | OR(fixed) | 1.01(0.62,1.65) | ||
| Xie (13) | 51/60 | 22/30 | OR(fixed) | 2.06(0.70,6.04) | ||
| Overall effect | OR(fixed) | 1.14(0.73,1.77) | 0.57 | |||
| Normalization rate of menstruation | ||||||
| Du (12) | 40/174 | 16/142 | OR(fixed) | 2.35(1.25,4.41) | ||
| Xie (13) | 18/60 | 9/30 | OR(fixed) | 1.00(0.38,2.60) | ||
| Overall effect | OR(fixed) | 1.83(1.09,3.09) | 0.02 | |||
| Hemostasis rate | ||||||
| Du (12) | 170/174 | 136/142 | OR(fixed) | 1.88(0.52,6.78) | ||
| Xie (13) | 51/60 | 22/30 | OR(fixed) | 2.06(0.70,6.04) | ||
| Overall effect | OR(fixed) | 1.98(0.87,4.52) | 0.11 | |||
| Recurrence rate | ||||||
| Xie (13) | 3/31 | 9/17 | OR(fixed) | 0.10(0.02,0.44) | 0.003 | |
Table 7.
Chinese herbal medicine plus conventional western medicine vs conventional western medicine
| Outcome measures | Sub-category | Trials | Participants |
Statistical method | Odds ratio (95% CI) | P value | |
|---|---|---|---|---|---|---|---|
| CHM& CWM group | CWM group | ||||||
| Total effect rate | |||||||
| Chinese herbal medicine nourishing Qi and stopping bleeding | Cheng (11) | 41/42 | 33/42 | OR(fixed) | 11.18(1.35,92.81) | 0.03 | |
| Chinese herbal medicine stopping bleeding | He (10) | 17/18 | 9/17 | OR(fixed) | 15.11(1.62,140.58) | 0.02 | |
| Overall effect | OR(fixed) | 12.74(2.72,59.72) | 0.001 | ||||
| Normalization rate of menstruation | |||||||
| Chinese herbal medicine nourishing Qi and stopping bleeding | Cheng (11) | 32/42 | 12/42 | OR(fixed) | 8.00(3.01,21.23) | <0.0001 | |
| Chinese herbal medicine stopping bleeding | He (10) | 8/18 | 2/17 | OR(fixed) | 6.00(1.05,34.32) | 0.04 | |
| Overall effect | OR(fixed) | 7.43(3.16,17.44) | <0.00001 | ||||
Results
Four RCTs Met Inclusion Criteria
Four Chinese RCTs or quasi-RCTs (10–13) that met the inclusion criteria were included (Table 3). The main reasons for exclusion are as follows: (i) it was confirmed that animals or processed animal products were used in the TCM formulas, (ii) the treatment in the control group was different from what was given to the treatment group except CHM, (iii) trials had statistical errors and (iv) trials that did not report diagnostic criteria definitely. (v)Trials where is a big gap between the sample size of the experimental group and the control group (experimental group cases: control group cases >2:1). While imbalanced random allocation was not mentioned in these trials or (vi) those trials whose authors failed to describe the randomization process correctly when they were required to clarify details. (vii) As well as trials whose author could not be contacted, (viii) trials not able to obtain the full-text and (ix) trials used CHM both in the treatment and control group.
Table 3.
The characteristics of trials
| Trials | Participants (T/C) | Ranges of age(y) (T/C) | Duration of symptoms (m) (T/C) | Treatment | Control | Treatment duration (menstrual cycles) |
|---|---|---|---|---|---|---|
| He (10) | 18/17 | Unclear | Unclear | Oral Tiaojing hao, progesterone im | Progesterone im | 3–6 |
| Cheng (11) | 42/42 | 14–above 40/14–above 40 | 4–33/5–36 | Oral Bazhen Tang, DES, MPA | Oral DES, MPA | 3 |
| Du (12) | 174/142 | 12–50/14–50 | 2–84/2–120 | Oral Bushen Tiaojing Fang | Oral norethindrone, conjugated estrogens, MPA | 3 |
| Xie (13) | 60/30 | 11–21/11–20 | 1–24/20d–24 | Oral Fufang ShuDi capsule | Oral DES, MPA | 3 |
DES indicates diethylstilbestrol; MPA, medroxyprogesterone acetate.
Methodological Quality Varied From High to Low
Table 4 illustrates the quality of the trials with one classified as high and the rest low. All claimed ‘randomization’. One author (13) provided additional information that imbalanced random allocation information (2:1) was used in his trial. One trial (12) randomly allocated patients with random digit tables and another trial (10) allocated patients by patients’ medical record numbers. Details that patients were randomly allocated by random digit tables in one trial (13) were clarified thanks to the kindness of the author. No studies mentioned the use of allocation concealment and blindness. All trials gave baseline characteristics in terms of age and duration of symptoms. One trial (10) simply stated the baseline characteristics of all the patients. Three trials (11–13) compared characteristics of each group and claimed ‘no significant differences were identified’ and two trials (11–13) reported the P-value (P > 0.05). Information about withdrawal and failure to follow-up was provided in only one trial (13). In (13) four cases withdrew during treatment and two patients in the control group failed to follow-up. Arrays of herbal medicines were used in the four trials (Table 5).
Table 4.
The methodologic qualities of trials
Table 5.
The herbal medicines used in the trials
| Trials | Medicinal herbs used in the trials |
|---|---|
| He and Li, (10) | Typha angustifolia Typhaceae, Trogopterus xanthipes Petauristidae, Prunella vulgaris Labiatae. |
| Cheng, (11) | Angelica sinensis Umbelliferae, Ligusticum chuanxiong Umbelliferae, Rehmannia glutinosa Scrophulariaceae, Paeonia lactiflora Ranunculaceae, Codonopsis pilosula Campanulaceae, Atractylodes macrocephala Compositae, Poria cocos Polyporaceae, Glycyrrhiza uralensis Leguminosae, Lycium barbarum Solanaceae, Custuta chinensis Convolvulaceae, Rubus chiagii Rosaceae, Polygonum multiflorum Polygonaceae. |
| Du et al., (12) | Psoralea corylifolia Papilionaceae, Dipsacus asper Dipsacaceae, Codonopsis pilosula Campanulaceae, Cimicifuga heracleifolia Ranunculaceae, Typha angustifolia Typhaceae, Rubia cordifloia Rubiaceae, Halloysite, Ligustrum lucidum Oleaceae, Lycium barbarum Solanaceae, Angelica sinensis Umbelliferae, Paeonia lactiflora Ranunculaceae, Dioscorea opposita Dioscoreaceae, Curculigo orchioides Amaryllidaceae, Custuta chinensis Convolvulaceae, Rubus chiagii Rosaceae, Carthamus tinctorius Compositae. |
| Xie et al., (13) | Rehmannia glutinosa Scrophulariaceae, Custuta chinensis Convolvulaceae, Coix lacryma-jobi ma-yuan Gramineae, Dipsacus asper Dipsacaceae, Eclipta prostrata Compositae, Ligustrum lucidum Oleaceae, Epimedium brevicornum Berberidaceae, Cornus officinalis Cornaceae, Dioscorea opposita Dioscoreaceae, Paeonia lactiflora Ranunculaceae, Leonurus heterophyllus Labiatae, Typha angustifolia Typhaceae, Trogopterus xanthipes Petauristidae, Arnebia euchroma Boraginaceae. |
Results of meta-analysis
We found no trials compared CHM with no treatment or placebo.
CHM vs Conventional Medicine
Two studies compared CHM with CWM. Since they nourished the kidneys and stopping bleeding, we combined data across two studies (Table 6).
Notably, the meta-analysis of the high quality trial (13) demonstrated that there was no significant difference in normalization rate of menstruation.
CHM and Conventional Medicine vs Conventional Medicine Alone
Two studies compared CHM and CWM vs CWM alone in the treatment of DUB (Table 7). The compound in one study is used to nourish qi and stop bleeding while the other is only to stop bleeding. No serious adverse events were reported. With fewer than five trials to compare, we did not use a funnel plot to examine publication bias.
Discussion
The women's ages ranged from 11 to 50 and the duration of symptoms varied from 20 days to 120 months, demonstrating the scope of CHM for DUB. No group scientifically described the severity of symptoms before the patients entered the trials. Only 31 patients were followed-up in (13), which makes it difficult to accurately evaluate these terms.
We found only a few trials that compared CHM with surgery. John Bonnar and Brian L Sheppard (14) recommended that patients with DUB should be offered effective drug treatment with tranexamic acid before considering surgical treatment. Hysterectomies have been the traditional surgical procedure used to treat menorrhagia secondary to DUB. The systematic review of Neil Johnson and David Barlow et al. (15) found no important disadvantages of vaginal hysterectomy compared with other surgical approaches, such as avoiding abdominal hysterectomy accelerates recovery, diminishes post-operative pain and avoids abdominal wall infections and general post-operative febrile illness. Laparoscopic hysterectomy may help to avoid a laparotomy, but urinary tract injury is a genuine concern.
Over the past 10 years there has been an international upsurge of interest in decreasing hysterectomy rates in the gynecologic community. Some less complicated methods of endometrial ablation, like NovaSure system have been developed and offer the gynecologist excellent alternatives in the treatment of DUB so that hysterectomy can be avoided (16). S. B. Pinion et al. (17) demonstrated that hysteroscopic surgery could be recommended and should be encouraged as an alternative for the majority of women when more conservative treatment had failed. Interestingly, hysteroscopic surgery and hysterectomy have a similar effect on psychiatric and psychosocial outcomes (18). Neither treatment affected marital relationships nor both treatments had a similar influence on sexual relationships. Trials comparing CHM with surgery should be conducted to comprehensively assess the benefits of CHM in the treatment of DUB. Deciding which treatment is best is complex. All these options should be discussed with patients, considering the relative advantages and disadvantages before making a decision on treatment.
Herbal medicine, including Chinese herbs, is gaining popularity as an alternative therapy all over the world. For instance, spending on herbal products in the United Kingdom is over £40 m a year, mainly from self prescription of over the counter products (19). Originally confined to health food shops, herbal remedies are now marketed in many conventional pharmacies. On the other hand, there are still some hurdles, which are partly caused by the lack of strong evidence from reputable medical sources and this slows the spread of herbal medicine. For example, in one review article, the author stated that clinicians should prescribe or recommend herbal remedies only if their use had been proved effective by rigorous study and only a small fraction of the thousands of medicinal plants used worldwide have been tested rigorously in randomized, controlled trials (20).
CHM for the treatment of DUB had different outcomes. Some of the outcome measures regulated by the authorities of TCM are quite specific and that is what TCM clinical studies have to obey. The assessment of menstrual loss may be based on the Chinese participants’ views, but it is never evaluated scientifically and rigidly. A standardized outcome index should be developed to make assessment more scientific and future investigations should adapt objective and quantitative measurements. Few trials have observed the amount of menstrual blood loss, ovulation in women suffering from anovulatory DUB and their quality of life, making it difficult to draw conclusions from these outcomes.
No multi-center, large sample and co-operative studies were found and there were many differences in sample size between treatment groups and control groups in some randomized trials, which were beyond the range of randomized allocation. No trials estimated the sample size. None were strong enough to state conclusively whether there were differences between CHM and other treatments. Although all trials claimed randomization, they failed to provide enough information to judge whether the randomization procedures had been carried out properly. Gynecologists should pay more attention to the safety of CHM for DUB.
The prevalence of poor quality studies calls to TCM clinicians and scientists to improve the quality of TCM investigations not only in gynecologic areas but in all clinical fields.
Conclusion
The results of meta-analysis of clinical practice demonstrated that CHM used under the guidelines of basic TCM theory gained encouraging results in the treatment of DUB, especially when combined with western medicine. Most women in the included trials stopped bleeding and many of them regained normal menstruation in a certain period of time. No adverse events were reported due to (in part) the use of herbs which are mostly not noxious with few side effects. A great deal of emphasis was placed on treatment based on differentiation. Modification of corresponding assistant and adjunctive herbs in formulas according to the accompanying symptoms is very common in these studies. Lumping trials of herbal compounds with the same or similar effects together had not caused heterogeneity, which, perhaps, is a prospective method for TCM formulas varying widely in constituents when performing meta-analysis.
Due to the lack of trials comparing CHM with no treatment or placebo, it is impossible to evaluate the effectiveness of CHM. CHM treatment in these studies seems to show a favorable comparative effect on the control of western medicine. However, the poor methodological quality may weaken the validity of the results. Owing to the lack of RCTs with high methodologic quality, we have to wait. In this case, the waiting period could be a time to develop hypotheses to explain the results that have been achieved in individuals and trials conducted lower on the golden pyramid (21). Performing clinical trials with high methodological quality of TCM for DUB is very helpful to accurately assess the benefits and potential risks in the treatment of DUB. In the future, more rigorously designed, randomized, double-blind, placebo-controlled trials with large sample size are needed to make TCM accepted by more people in the world.
Acknowledgements
We thank Prof Fanrong Liang of Chengdu University of TCM for his suggestions and useful comments for this paper, Lecturer Lishuang Ye for translation. We thank Tarynn Butler and Carrie Brugger, (LAc, USA) for their editing in language.
References
- 1.Brandon JB, Amy EH, Nicholas CL, Harold EF, Edward EW. The Johns Hopkins Manual of Gynecology and Obstetrics. 2nd. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 405–11. [Google Scholar]
- 2.Alan HD, Lauren N. Current Obstetric & Gynecologic Diagnosis & Treatment. 9th. New York: McGraw-Hill; 2003. pp. 623–30. [Google Scholar]
- 3.Havens CS, Sullivan ND. Manual of Out-patient Gynecology. 4th. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 119–31. [Google Scholar]
- 4.Steven RB, Alan HD. Clinical Manifestations and Treatment of Dysfunctional Uterine Bleeding. JAMA. 1993;269:1823–8. [PubMed] [Google Scholar]
- 5.Wu KM, Zhang QW. Clinical gynecology and obstetrics in Chinese and western medicine. Beijing: Chinese Medical and Science Press; 2001. pp. 144–54. [Google Scholar]
- 6.Du HL, Song CM, Ma HR, Zhen YJ, Xu JX, Yan Hua, et al. Effect of Effect of Bushen Guchong serial prescriptions on ovary, uterus and microelement in anovulia rats induced by androgen. Chinese J Trad Med Sci Tech. 2002;9:102–3. [Google Scholar]
- 7.Du HL, Song CM, Ma HR, Zhen YJ, Xu JX, Yan Hua, et al. Effect of Bushen Guchong serial prescriptions on pituitary in anovulia rats induced by androgen. Chinese J Trad Med Sci Tech. 2002;9:100–1. [Google Scholar]
- 8.Chen BH, Giudice LC. Dysfunctional Uterine Bleeding. West J Med. 1998;169:280–4. [PMC free article] [PubMed] [Google Scholar]
- 9.Review Manager (RevMan) [Computer program] Version 4.2 for Windows. Oxford, England: The Cochrane Collaboration; 2002. [Google Scholar]
- 10.He YC, Li MR. Clinical efficacy observation on Chinese medicine Tiaojing hao in the treatment of 467 cases of dysfunctional uterine bleeding. J Shanxi Med College. 1993;24:221–3. [Google Scholar]
- 11.Cheng HE. Modified Bazhen Tang plus artificial menstrual cycle in the treatment of 84 cases of anovulatory dysfunctional uterine bleeding. Anhui Clinl J TCM. 1999;11:238–9. [Google Scholar]
- 12.Du HL, Yan Hua, Bai FL, Song CN, Li XF, Zhang JF. Clinical study on effect of cyclic medicated Bushen Tiaojing serial recipe in treating dysfunctional uterine bleeding. Chinese J Integrat Tradl West Med. 2003;23:178–81. [Google Scholar]
- 13.Xie Bo, Chen XP, Zhang YR, Zheng JL. Treatment of hebetic dysfunctional uterine bleeding by Fufang Shudi capsule: a clinical observation of 60 cases. N J TCM. 2003;35:17–8. [Google Scholar]
- 14.Bonnar J, Sheppard BL. Treatment of menorrhagia during menstruation: randomised controlled trial of ethamsylate, mefenamic acid and tranexmic acid. Brit Med J. 1996;313:579–82. doi: 10.1136/bmj.313.7057.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. Brit Med J. 2005;330:1478. doi: 10.1136/bmj.330.7506.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gallinat A. NovaSure impedance controlled system for endometrial ablation: Three-year follow-up on 107 patients. Am J Obstet Gynecol. 2004;191:1585–9. doi: 10.1016/j.ajog.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 17.Pinion SB, Parkin DE, Abramovich DR, Naji A, Alexander DA, Russell IT, et al. Randomised trial of hysterectomy, endometrial laser ablation, and transcervical endometrial resection for dysfunctional uterine bleeding. Brit Med J. 1994;309:979–83. doi: 10.1136/bmj.309.6960.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander D, Naji AA, Pinion SB, Mollison J, Kitchener HC, Parkin DE, et al. Randomised trial comparing hysterectomy with endometrial ablation for dysfunctional uterine bleeding: psychiatric and psychosocial aspects. Brit Med J. 1996;312:280–4. doi: 10.1136/bmj.312.7026.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vickers A, Zollman C. ABC of complementary medicine: Herbal medicine. Brit Med J. 1999;319:1050–3. doi: 10.1136/bmj.319.7216.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Smet PA. Herbal Remedies. N Eng J Med. 2002;347:2046–56. doi: 10.1056/NEJMra020398. [DOI] [PubMed] [Google Scholar]
- 21.Cooper EL. ECAM is waiting for eCAM. Evid Based Complement Alternat med. 2005;2:427–8. doi: 10.1093/ecam/neh135. [DOI] [PMC free article] [PubMed] [Google Scholar]