Abstract
More than 20% of approximately 35,000 patients filling a diuretic prescription had no potassium blood test recorded within the previous year. A laboratory reporting system used throughout Israel by Maccabi Healthcare Services physicians was modified to provide physician alerts regarding potassium testing. The physicians were experienced users of a computerized medical record (CMR) that provided online laboratory test results. A nightly batch file checked pharmacy diuretic purchases against the patient's potassium blood test status. On-screen computer-generated reminders were sent to physicians of patients lacking a recent potassium test. Reminders to clinicians increased potassium testing by 9.8% (p < 0.001). Physician age and gender played a small part in predicting compliance to the alert, but specialty and practice size did not. The time delay between the date a reminder was sent and the potassium test date decreased steadily during the intervention. The success of this reminder system encourages expansion to include more drug–laboratory interactions. Furthermore, direct alerts to patients at multiple organization/patient contact points are planned.
Adverse drug events (ADEs) play a significant role in iatrogenic morbidity and mortality. Maccabi Healthcare Services has developed a computer alert system using existing computer databases and communications network to reduce ADEs among our members. This alert system generated physician reminders for potassium blood testing in patients taking diuretics. In this article, we describe the design, process, and results of this intervention.
Background
Organizational Information
Maccabi Healthcare Services is the second largest nonprofit integrated health care provider in Israel. It includes 3,000 physicians providing care for over 1.6 million members who have access to services throughout Israel. Nationwide, 10% of our physicians are salaried employees of Maccabi, while the remaining 90% are independent contractors providing medical services to health plan members. Salaried physicians see Maccabi patients exclusively, whereas independent contractors often have other health plan subscribers in their practice. The organization maintains its own laboratory and pharmacy services, and members may also obtain their medications from independent affiliated pharmacies throughout the country.
Preventing Adverse Drug Events
Adverse drug events are relatively common in patients receiving prescription drugs. A cohort study of older adults in a multispecialty group practice found an overall ADE rate of 50.1 per 1,000 person-years.1 In a recent survey of ambulatory patients, using a broad definition of what constitutes an ADE, one in four patients was reported to suffer symptoms or injury as a result of taking prescription drugs.2 Computer-based alert systems in the outpatient setting can identify ADEs3 and are effective in modifying physician behavior in medication management.4
Targeted computer reminders generally are accepted by physicians.5 Simple alerts, such as those that change text color on the computer screen to emphasize abnormal laboratory values, have become widespread in CMRs.6 More complex reminders that recommend an action to the physician to promote health care, such as preventive services, have proven useful.7
Diuretics and ADEs
Diuretics are a common yet potentially hazardous medication widely used by primary care physicians for commonly occurring diseases. Thiazide and similar diuretics may enhance renal excretion of potassium causing hypokalemia, while potassium-sparing diuretics can have the opposite effect.8 Hypokalemia can contribute to a wide variety of disorders, including atrial and ventricular arrhythmias, muscle weakness, constipation, nausea, and vomiting. Dose-related hypokalemia is not uncommon in hypertensive patients treated with thiazide diuretics.9 An abnormal potassium level can cause pathology by itself if sufficiently abnormal, although problems are more likely when other drugs, such as digoxin, are present.
An initial review of Maccabi potassium testing rates in patients taking diuretics was conducted by matching pharmacy records with laboratory records for a one-month period. More than 20% of patients receiving diuretics had no potassium blood level measured within the previous 12 months. We reviewed several pharmaceutical companies' prescribing information for drugs containing diuretics and found no instance in which a potassium testing frequency was specifically recommended. Guidelines suggested that electrolyte levels be monitored at appropriate intervals to detect any possible imbalance.10,11,12
We deemed that an annual blood test for potassium was a reasonable minimal testing frequency in patients receiving diuretics, and alerting the physician was warranted in cases in which this deadline was exceeded. We constructed a reminder subsystem for potassium testing by augmenting an existing laboratory reporting system.
Design Objectives
The aim of this project was to create a model that uses existing computer resources to improve patient care by alerting physicians to situations in which the patient may be at risk. The model was designed using the case of potassium testing for patients taking diuretic medication. The target population was all Maccabi physicians prescribing diuretics. The outcome measured was the proportion of patients taking diuretic medications who had a potassium test in the previous 12 months. We defined the following model objectives:
Systematic integration of pharmacy and laboratory records
Identification of eligible patients and their physicians
Generation of computerized reminders to physicians on a daily basis
Facilitation of process evaluation
System Description
Existing System
The Maccabi central data repository retains complete historical records of patient demographic data, physician data, laboratory results, and filled prescriptions information, using the patient's unique national identification number. The Potassium Reminder Project exploits the interconnectivity and robustness of Maccabi Healthcare Service's integrated computer systems. It was developed by linking central repository data with the CMR.
The CMR,13 first used in Maccabi clinics in 1990, is now the sole medical record for 3,000 physicians caring for a population of 1.6 million subscribers. It has completely replaced the paper chart. The program provides full medical record functions, similar to commercial medical charting programs available in the United States. In our CMR, encounter notes are typed in by the physician at the time of the patient visit.
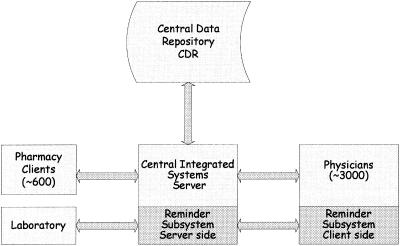
The CMR runs locally on a personal computer located in the doctor's office. It exchanges data with the central data repository using proprietary transactions sent by modem over telephone lines or through a wide area network (WAN) (▶). Laboratory test results, among other data, are downloaded on a daily basis and are reviewed by physicians at their leisure either on screen or in printed form. After being countersigned by the doctor, these laboratory reports become an integral and indelible part of the patient's medical record. The majority of physicians routinely open and acknowledge the test results within a number of days. If the computer system detects a backlog of alerts that have not been viewed, a technician will contact the physician to inform him or her of this.
Figure 1.
System description.
All Maccabi or affiliated pharmacies in Israel (∼600) are connected online by satellite relay or by a WAN to our Centralized Integrated System. Prescriptions written by a Maccabi physician for patients with a chronic condition, such as hypertension, are valid for three months. Prescriptions are filled at participating pharmacies, where relevant patient and drug data are entered into the local pharmacy computer. These data are uploaded to the central integrated system's server for further processing. Eligibility checking, drug interactions, and formulary concordance are performed. Contraindication alerts, if any, are returned in real time to the pharmacist. This completes the transaction and assures the entering of all drug purchase data into the central data repository.
Maccabi uses a central laboratory for all diagnostic testing. The laboratory computer uploads test results daily to the central data repository. These data then are forwarded individually, on a daily basis, to the physician's office computer.
Potassium Reminder Project: System Enhancements
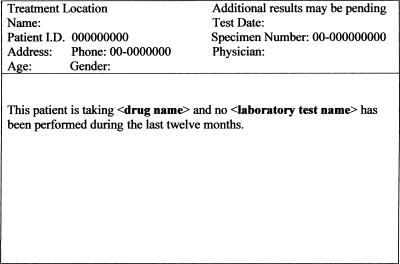
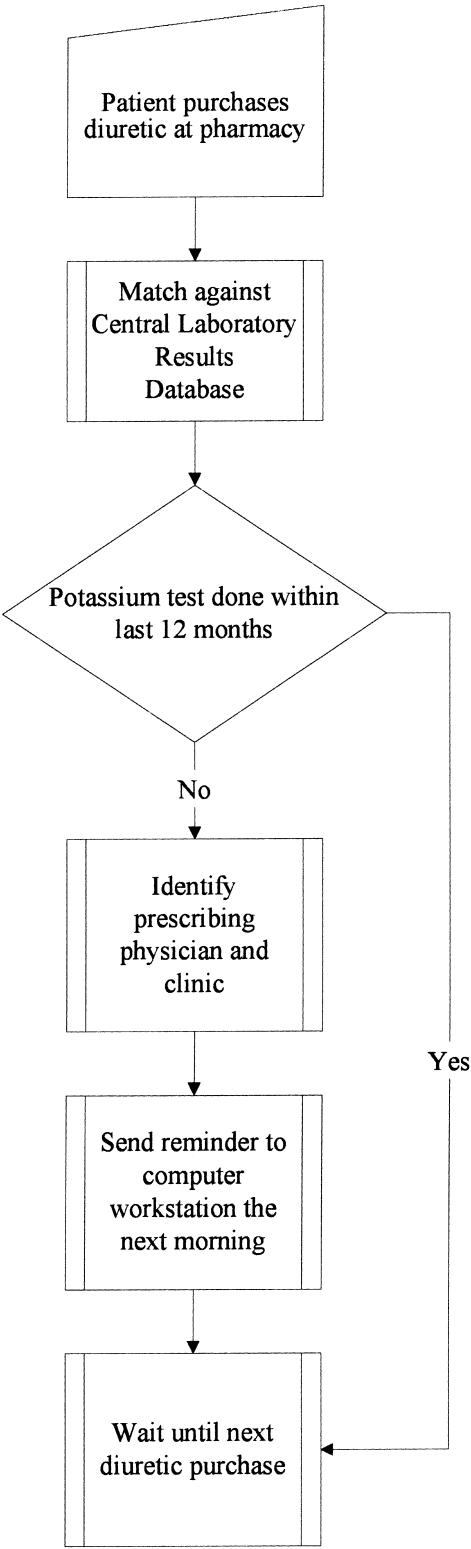
We used a nightly batch process to check all purchased medications containing any of the following diuretics: amiloride, chlorthalidone, furosemide, hydrochlorothiazide, indapamide, and spironolactone. These medication purchases then were compared by patient identification number against historical laboratory data. In every case in which a potassium blood level had not been performed within the previous 12 months, the patient's name and identification number, prescribing physician, medication name, and date of last potassium blood test were recorded. These data then were used to generate alerts (▶), which were downloaded to physician computers the following morning as part of the routine laboratory test results report. Reminder formats used the same header as laboratory reports, but the results format was unique to the alert system. Physicians open reminder mail at their convenience and not necessarily during a patient encounter. Each new diuretic purchase generated a new reminder if no potassium test had yet been done (▶).
Figure 2.
Example of a physician reminder as it appears on the computer screen.
Figure 3.
Computer reminder flow chart.
Physicians received no instruction concerning these reminders and their function, and no announcement regarding the initiation of the new reminder system was made. Patients were unaware that their physicians were receiving reminders regarding their medical care.
Status Report
Lists of eligible patients and their physicians were generated successfully nightly beginning September 1, 2001. Reminders were made available to all relevant physicians each workday morning. For a small number of physicians (∼100), redundant reminders were sent after the patient did have a blood test. This problem was identified and corrected within several weeks. Reminder data were accumulated and used to evaluate the success of the intervention in increasing the proportion of patients who had a potassium blood test after their physician received a computer-generated reminder.
The proportion of patients having blood tests for the months of September 2001 through January 2002 was compared with that in the same time period during the previous year, when no reminders had been issued. Using analysis of variance (ANOVA) in SPSS,14 we examined correlations between physician characteristics (age, gender, specialty, country of origin, and patient load) and the proportion of patients overdue for potassium testing. We also examined the time frame between first reminders and subsequent potassium blood tests.
We identified 1,517 physicians who had prescribed a diuretic for at least one patient during the preintervention periods. However, a great many of these physicians wrote only the occasional diuretic prescription. To focus the trial intervention on physicians who routinely prescribe diuretics, our inclusion criteria included physicians who had written at least 20 diuretic prescriptions over five months. Five hundred fifty-one physicians were included in this intervention. Of these, 504 had both pre- and postintervention data available and were included in the comparison.
Postintervention Change in Proportion of Patients Tested for Potassium
Among all patients taking diuretics, there was an absolute increase of 3% in the proportion of patients who had potassium laboratory tests in the postintervention period (September 2001 to January 2002) compared with the preintervention months (September 2000 to January 2001; ▶). Because only 7,592 of 35,313 patients taking diuretics needed a blood test (21.5%), this represents a relative improvement of 9.8% in this population (p < 0.001).
Table 1.
Increased Potassium Testing after Physician Reminder
| Period | Patients Taking a Diuretic Medication | Mean Proportion Tested | 95% CI | |
|---|---|---|---|---|
| Pre (9/00–1/01) | 34,284 | 78.5 | 77.32 | 79.68 |
| Post (9/01–1/02) | 35,313 | 81.5 | 80.48 | 82.52 |
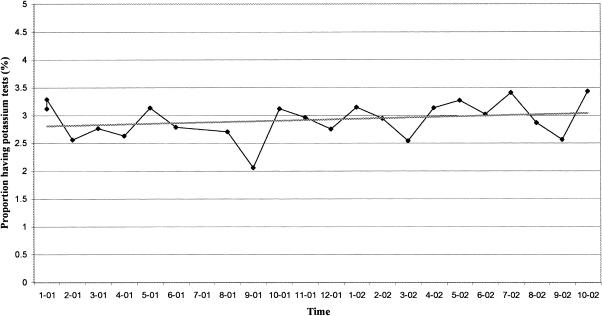
During the pre- and postintervention periods, no statistically significant background change in the level of potassium testing occurred in the general Maccabi population. The mean proportion of potassium tests in the year prior to our intervention was 2.83% (95% CI, 2.63–3.02), compared with 3.04% (95% CI, 2.83–3.23) in the year of the intervention (▶).
Figure 4.
Proportion of patients in the general population who had potassium tests over the study period.
We used the first five months of our intervention to compare potassium testing with the previous year, as presented. We then continued to monitor the effects of the intervention for a further six months, resulting in a period of 11 months of follow-up. During the 11-month period, a total of 17,486 reminders were sent to physicians of patients meeting the eligibility criteria. Of these, 14,364 were first reminders. The mean number of reminders sent per patient was 1.2 for patients who subsequently had a blood test and 1.25 for those who did not (p < 0.01).
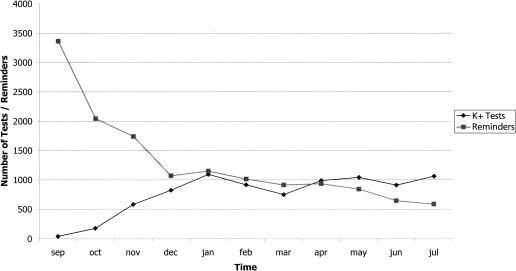
The monthly number of reminders required decreased steadily with time. A simultaneous increase was observed in the number of patients having at least one potassium test (▶). At the eighth month of intervention, the number of tests done exceeded the number of reminders sent out.
Figure 5.
First reminders and potassium tests performed in study population.
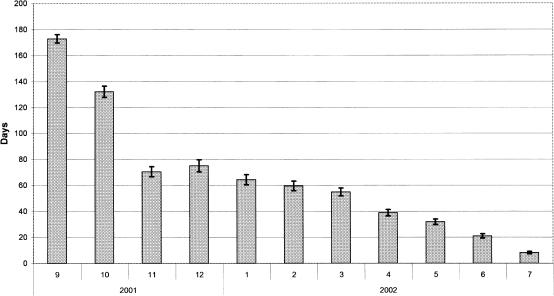
We also investigated the amount of time between the first reminder and the time at which the test was conducted. For the period from September 2001 to December 2001, the mean delay was 125 days (SD 88 days), and for the period January 2002 to July 2002, the mean delay was 46 days (SD 45 days). A steady improvement was observed in the time delay between the first reminder date and when the patient had the subsequent potassium test done (▶) over the period of the study.
Figure 6.
Number of days between reminder and test, mean ( ± ) 95% CI.
The physicians' specialty and country of origin were not associated with the proportion of patients having a potassium test done either before or after the intervention period. Furthermore, no correlation was found between the number of patients prescribed diuretics by a physician and the proportion of his or her patients who had a laboratory test done after the physician received the reminders. Patients of female physicians were more likely to have potassium tests done both before and after the intervention, although this difference was statistically significant only for the period after the intervention (p < 0.001). In addition, patients of younger physicians were significantly more likely to have a potassium test both before (p < 0.05) and after (p < 0.001) the intervention.
Discussion
Computer-generated reminders have been shown to be effective in a number of settings. McDonald,15 in his seminal paper on computer reminders, showed that computer alerts improve the level of patient care in routine tasks and those dependent on physician memory.
In this study, presenting a relevant computer alert to physicians in a format familiar to them led to a clear improvement in the proportion of patients having potassium blood tests. Although the absolute improvement of 3.0% was significant, the effect on patient care is greater when looking at potential improvement. Because only 21.5% of patients taking diuretics lacked a blood test, the relative improvement in this population was 9.8%.
We matched two five-month time periods one year apart to compensate for a recurring seasonal variability in the number of potassium blood tests done during the spring and fall holiday seasons in Israel.
Because reminders could be read by the physician independent of patient encounters, the date the reminder was sent was not necessarily the date the physician read the alert. The time lag between the time the reminder was issued and the time the test was done was dependent on when the physician gave the patient a referral and when the patient had the test done. This intervention influenced only the physician's referral, not the patient's compliance. Furthermore, alerts may have been viewed during chart review, when the patient was not present. There was no record of whether the physician contacted the patient immediately or whether he or she waited until a patient-initiated visit to implement the reminder recommendation. We do not know how many patients were specially asked to come in for a blood test, how many were notified when coming to the clinic for other reasons, and how many blood test orders were deferred by patients. Part of this decrease may be attributed to the small number of tests that would have been done in September or October and were not included in the total. To minimize this effect, we excluded reminders sent from August 2001 onward from this part of the analysis. The observed decrease in the lag time between reminder dates and test dates during the intervention period does indicate that the intervention had some effect on physician response time as well as the proportion of tests performed.
During the entire 11-month follow-up period, new patients meeting the eligibility criteria were added daily as a function of their blood test status when filling a diuretic prescription. Despite the increase in the eligible population, the monthly total of reminders being sent to physicians decreased over this follow-up period. This decrease may indicate increased physician compliance. It appears that, as a result of this intervention, a large backlog of patients had their recommended blood work done per the physicians' request before reminders were issued.
Most physician and practice characteristics examined did not seem to have a large effect on physician compliance. Women and younger physicians were significantly more likely to refer their patients for tests after the intervention. Physicians with very large practices did not respond significantly less than those with small practices to computer-generated alerts.
As previously mentioned, compliance with blood testing recommendations relies on both physician referrals and patient response. There may be a group of patients who, regardless of referrals, will not comply with testing. This issue needs to be addressed. This Potassium Reminder Project increased the proportion of patients taking diuretics who had potassium tests. This was done at minimal cost with a populationwide impact. The limitations of this work are (1) it targets physicians and not patients and therefore does not address the issue of patient noncompliance, (2) the intervention affects mainly the care of patients who see their doctor regularly, and (3) it does not address the values of the tests. Some of these limitations can be addressed by designing interventions targeting patients as well as physicians and linking the reminders to the patient's file as a pop-up message when the patient file is opened at the next visit. We also are examining the issue of test results as part of the expansion of computer-generated reminders at Maccabi.
Building on our present work, physician reminders can be extended to include a variety of medications requiring laboratory investigation of medication level or side effects. This computer-generated alert system can also be used to directly provide patients with appropriate alerts. The reminder module can be modified easily to access several existing organization/patient contact points, such as our members' Web site or our touch-screen information kiosks that are present in all large Maccabi clinics. These additional alerts could magnify the positive effect of the physician reminder.
Although Maccabi has a unique enabling infrastructure that includes complete capture and control of laboratory results and pharmacy data within one organization (much like that of Veterans Affairs in the United States) it could be possible for health care organizations that use computerized records but lack drug purchase data to generate reminders using prescription data instead. The principle of modifying an existing reporting system to generate physician reminders to prevent ADEs may be applied to various patient care settings at minimal cost.
The authors thank Mila Wasbih and Vladimir Galinkin for their kind assistance in data collection and processing.
References
- 1.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. [DOI] [PubMed] [Google Scholar]
- 3.Honigman B, Lee J, Rothschild J, et al. Using computerized data to identify adverse drug events in outpatients. J Am Med Inform Assoc. 2001;8:254–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennett JW, Glasziou PP. Computerised reminders and feedback in medication management: a systematic review of randomised controlled trials. Med J Aust. 2003;178:217–22. [DOI] [PubMed] [Google Scholar]
- 5.Kuperman GJ, Teich JM, Tanasijevic MJ, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial. J Am Med Inform Assoc. 1999;6:512–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradshaw KE, Gardner RM, Pryor TA. Development of a computerized laboratory alerting system. Comput Biomed Res. 1989;22:575–87. [DOI] [PubMed] [Google Scholar]
- 7.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3:399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walters EG, Barnes IC. A survey of hypokalaemia in patients of general practitioners. Br J Clin Pract. 1988;42:192–5. [PubMed] [Google Scholar]
- 9.Hollifield JW. Thiazide treatment of hypertension. Effects of thiazide diuretics on serum potassium, magnesium, and ventricular ectopy. Am J Med. 1986;80:8–12. [DOI] [PubMed] [Google Scholar]
- 10.Merck. HYZAAR® 50-12.5 Prescribing Information. Whitehouse Station, NJ, 2001.
- 11.SmithKline-Beecham. DYAZIDE® capsules Prescribing Information. Philadelphia, PA, 1999.
- 12.Aventis Lasix (furosemide) Prescribing Information. Bridgewater, NJ: Aventis Pharmaceuticals, 2003.
- 13.Roshtov Software L. Clicks Medical Record. Omer, Israel, 1995.
- 14.SPSS Inc. SPSS for Windows. Chicago IL, 2001.
- 15.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med. 1976;295:1351–5. [DOI] [PubMed] [Google Scholar]