Abstract
Two cases of torsade de pointes associated with bradycardia and takotsubo cardiomyopathy are reported. In both cases, atrioventricular block preceded the occurrence of takotsubo cardiomyopathy. Bradycardia-induced QT interval prolongation seemed to be amplified by the occurrence of takotsubo cardiomyopathy, resulting in torsade de pointes. Temporary ventricular pacing at a high rate decreased the QT interval and prevented the recurrence of torsade de pointes. Because atrioventricular block recurred or persisted even after the resolution of takotsubo cardiomyopathy, the patients received permanent pacemakers.
Keywords: Atrioventricular block, Takotsubo cardiomyopathy, Torsade de pointes
Abstract
Deux cas de torsade de pointe associés à une bradycardie et à une myocardiopathie takotsubo sont présentés. Dans les deux cas, un bloc auriculoventriculaire a précédé l’occurrence de myocardiopathie takotsubo. Une prolongation de l’intervalle QT induite par une bradycardie semblait amplifiée par l’occurrence de myocardiopathie takotsubo, entraînant une torsade de pointe. Un entraînement ventriculaire temporaire à rythme élevé a réduit l’intervalle QT et prévenu la récurrence de torsades de pointe. Puisque le bloc auriculoventriculaire était récurrent ou persistant même après la résolution de la myocardiopathie takotsubo, les patients ont reçu des stimulateurs cardiaques permanents.
A novel cardiac syndrome exhibiting transient left ventricular apical wall motion abnormalities without obstructive epicardial coronary artery disease has been recognized worldwide (1–4). This disorder has widely been called takotsubo cardiomyopathy because the end-systolic left ventriculogram looks like a tako-tsubo, used for trapping octopuses.
We report two cases of torsade de pointes associated with bradycardia and takotsubo cardiomyopathy.
CASE PRESENTATIONS
Patient 1
An 87-year-old woman with a history of syncope was admitted to her local hospital due to dyspnea. An electrocardiogram (ECG) on admission showed right bundle branch block during 2:1 atrioventricular block with a ventricular rate of 46 beats/min, but did not show ST segment or T wave change. She had worsening dyspnea and was referred to the Hiroshima City Hospital (Hiroshima, Japan) six days later.
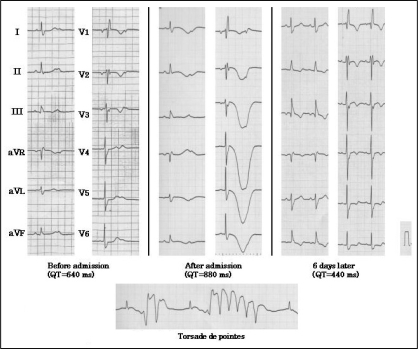
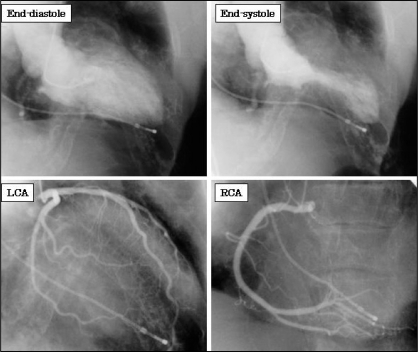
On admission, the patient had no chest pain but had orthopnea. She was fully conscious, and her blood pressure was 130/80 mmHg. Her hematological test results were normal. A chest x-ray showed bilateral pleural effusion and cardiac enlargement. An ECG showed right bundle branch block during 2:1 atrioventricular block with a ventricular rate of 42 beats/min, T wave inversion in leads I, II, aVL, aVF and V1 to V6, as well as excessive QT interval prolongation (880 ms) (Figure 1). Immediately after the admission, torsade de pointes occurred. Temporary ventricular pacing, which was performed at a rate of 80 beats/min, decreased the QT interval to 640 ms and prevented the recurrence of torsade de points. Emergency coronary angiography showed no significant coronary artery disease, but left ventriculography showed akinesia of the distal portion of the left ventricular chamber (ejection fraction of 62%) (Figure 2). The patient was diagnosed as having takotsubo cardiomyopathy. Her QT interval gradually improved and torsade de pointes never recurred, even after discontinuation of temporary ventricular pacing. Serial measurements of creatine kinase were normal. Follow-up echocardiography eight days later showed normal left ventricular wall motion. Because atri-oventricular block recurred transiently, the patient received a single-chamber pacemaker 10 days after admission.
Figure 1).
A serial electrocardiogram of patient 1 showing transient QT interval prolongation (upper panel). Immediately after the admission, torsade de pointes occurred (lower panel) (calibration setting 10 mm = 1.0 mV)
Figure 2).
Left ventriculography of patient 1 showed akinesia of the distal portion of the left ventricular chamber (ejection fraction of 62%) with no significant coronary artery disease. LCA Left coronary angiogram; RCA Right coronary angiogram
Patient 2
A 78-year-old man was admitted to his local hospital due to syncope. An ECG on admission showed left axis deviation and left bundle branch block during complete atrioventricular block with a ventricular rate of 46 beats/min, but did not show ST segment or T wave changes. He had persistent atrioventricular block and was referred to the Hiroshima City Hospital two days later.
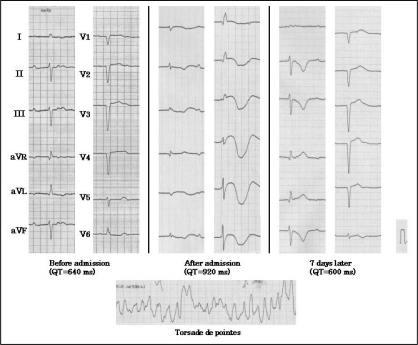
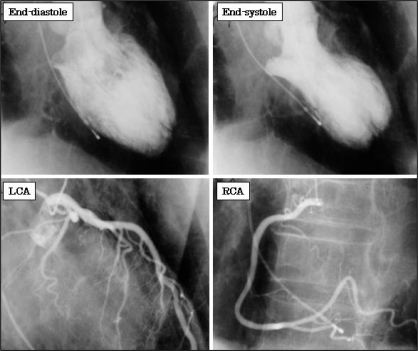
On admission, he had no symptoms. He was fully conscious, and his blood pressure was 120/70 mmHg. His hematological test results were normal. A chest x-ray showed no pulmonary edema or cardiac enlargement. An ECG showed right bundle branch block during complete atri-oventricular block with a ventricular rate of 40 beats/min, ST segment elevation in leads V2 to V6, T wave inversion in leads I, II, III, aVF and V1 to V6, as well as excessive QT interval prolongation (920 ms) (Figure 3). Immediately after the admission, torsade de pointes occurred, which was alleviated with intravenous magnesium sulfate. Temporary ventricular pacing, which was performed at a rate of 90 beats/min, decreased the QT interval to 480 ms and prevented the recurrence of torsade de pointes. Emergency coronary angiography showed no significant coronary artery disease, but left ventriculography showed akinesia of the mid- to distal portion of the left ventricular chamber (ejection fraction of 38%) (Figure 4). He was diagnosed as having takotsubo car-diomyopathy. The QT interval gradually improved and torsade de pointes never recurred, even after discontinuation of temporary ventricular pacing. Serial measurements of creatine kinase were normal. Follow-up echocardiography seven days later showed normal left ventricular wall motion. Because atrioventricular block persisted, he received a dual-chamber pacemaker seven days after the admission.
Figure 3).
Serial electrocardiogram of patient 2 showed transient QT interval prolongation (upper panels). Immediately after the admission, torsade de pointes occurred (lower panel) (calibration setting 10 mm = 1.0 mV)
Figure 4).
Left ventriculography of patient 2 showed akinesia of the mid- to distal portion of the left ventricular chamber (ejection fraction of 38%) with no significant coronary artery disease. LCA Left coronary angiogram; RCA Right coronary angiogram
DISCUSSION
Since Sato et al (1) first reported takotsubo cardiomyopathy in 1990, several clinical features have been revealed (1–3). In general, most patients are elderly women, have emotional or physical stress antecedent to the onset, and have a favourable prognosis. In the present report, we demonstrated two cases of torsade de pointes associated with bradycardia and takotsubo cardiomyopathy.
In both cases, atrioventricular block seemed to precede the occurrence of takotsubo cardiomyopathy; the initial ECGs showed atri-oventricular block without ST segment or T wave change. Moreover, atrioventricular block recurred or persisted even after the resolution of left ventricular dysfunction, suggesting that the atrioventricular block did not result from takotsubo cardiomyopathy. Our patients were not under emotional stress. However, one had dyspnea due to bradycardia-induced heart failure and the other had syncope due to bradycardia. Thus, these physical stresses might have resulted in takotsubo car-diomyopathy.
Torsade de pointes denotes a polymorphic ventricular tachycardia associated with a long QT syndrome (LQTS), and is a life-threatening arrhythmia. LQTS is caused by mutations in genes encoding specific channels (congenital LQTS), drugs, metabolic abnormalities or sympathetic imbalance, or by bradyarrhythmias such as atrioventricular block (acquired LQTS). LQTS is also caused by structural heart diseases. Halkin et al (5) demonstrated LQTS following acute myocardial infarction. In their study, QT interval prolongation was significant but transient, reaching a maximal level within days after onset and shortening to the initial values by day 10. Patients had no clinical, ECG or angiographic findings to suggest that either acute ischemia or reinfarction was responsible for these arrhythmias. We also recently demonstrated LQTS following takotsubo cardiomyopa-thy (3). Significant but transient QT interval prolongation occurred twice following takotsubo cardiomyopathy – the first peak occurring at approximately three days and the second peak occurring at approximately two to three weeks. In the current cases, we thought that bradycardia-induced QT interval prolongation might have been augmented by the occurrence of takotsubo cardiomyopathy, resulting in torsade de pointes.
The inverse relationship between heart rate and repolarization time means that faster pacing will give a shorter QT interval. Previous studies (5) have shown that cardiac pacing at a high rate is useful to prevent torsade de pointes in various conditions. In the present report, we demonstrated that this was also applicable to torsade de pointes associated with takotsubo cardiomyopathy. It has recently been demonstrated (6) that ventricular pacing can cause left ventricular mechanical dyssynchrony and subsequent remodelling. Therefore, overdrive ventricular pacing may result in worsening hemodynamics, especially in patients with takotsubo cardiomyopathy and depressed left ventricular function. From this viewpoint, ventricular pacing should be discontinued as soon as possible after the resolution of tor-sade de pointes.
Cardiologists should recognize that torsade de pointes is a possible complication of takotsubo cardiomyopathy, especially during bradycardia. Cardiac pacing at a high rate is useful to prevent torsade de pointes associated with takotsubo cardiomyopathy.
REFERENCES
- 1.Sato H, Tateishi H, Uchida T, Dote K, Ishihara M. Stunned myocardium with specific (tsubo-type) left ventriculographic configuration due to multivessel spasm. In: Kodama K, Haze K, Hori M, editors. Clinical Aspects of Myocardial Injury: From Ischemia to Heart Failure. Kagakuhyouronsya Co: Tokyo; 1990. pp. 56–64. [Google Scholar]
- 2.Kurisu S, Sato H, Kawagoe T, et al. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: A novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J. 2002;143:448–5. doi: 10.1067/mhj.2002.120403. [DOI] [PubMed] [Google Scholar]
- 3.Kurisu S, Sato H, Kawagoe T, et al. Time course of electrocardiographic changes in patients with tako-tsubo syndrome: Comparison with acute myocardial infarction with minimal enzymatic release. Circ J. 2004;68:77–81. doi: 10.1253/circj.68.77. [DOI] [PubMed] [Google Scholar]
- 4.Bybee KA, Kara T, Prasad A, et al. Systematic review: Transient left ventricular apical ballooning: A syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858–65. doi: 10.7326/0003-4819-141-11-200412070-00010. [DOI] [PubMed] [Google Scholar]
- 5.Halkin A, Roth A, Lurie I, Fish R, Belhassen B, Viskin S. Pause-dependent torsade de pointes following acute myocardial infarction: A variant of the acquired long QT syndrome. J Am Coll Cardiol. 2001;38:1168–74. doi: 10.1016/s0735-1097(01)01468-1. [DOI] [PubMed] [Google Scholar]
- 6.Lupi G, Sassone B, Badano L, et al. Ablate and Pace in Atrial Fibrillation (APAF) Pilot Echocardiographic Trial Investigators Effects of right ventricular pacing on intra-left ventricular electromechanical activation in patients with native narrow QRS. Am J Cardiol. 2006;98:219–22. doi: 10.1016/j.amjcard.2006.01.077. [DOI] [PubMed] [Google Scholar]