Abstract
Objectives
To confirm the feasibility of nurse practitioner interventionin non-high-risk patients with recent myocardial infarction (MI).
Design
Observational study.
Setting
Acute coronary care unit in a teaching hospital.
Methods
We performed an open-label feasibility
study to identify non-high-risk MI patients and evaluate the outcome of a new nurse practitioner intervention programme. The initial pilot phase served to identify the non-high-risk population. In the subsequent confirmation phase, 500 consecutive non-high-risk post-MI patients with preserved LV function without heart failure were included to receive nurse practitioner management. The nurse practitioner intervention started on transfer from the coronary care unit to the cardiology ward and continued thereafter for up to 30 days.
Main outcome measures
Time to first event analysis of death from all causes or repeat myocardial infarction.
Results
500 Patients without signs of heart failure or depressed LV function were identified as nonhigh- risk and eligible for inclusion in the nurse practitioner intervention programme. In the implementation phase, none of the patients died and 0.9% developed a repeat myocardial infarction after 30 days of follow-up. Compared with the pilot phase, patients in the implementation phase spent fewer days in hospital (mean 11.1 versus 6.2 days; p<0.001).
Conclusion
It is feasible to identify non-high-risk post-MI patients, who can be managed adequately by a nurse practitioner. Embedding experienced nurse practitioners within critical care pathways may result in significant decreases in length of hospital stay. (Neth Heart J 2009;17:61-7.Neth Heart J 2009;17:61-7.)
Keywords: myocardial infarction, nurse practitioner, post-infarction management
Cardiovascular diseases remain a major health care problem and consume large amounts of public health resources.1 Over the past few decades, better treatment options and strategies for cardiovascular diseases have improved the quality and length of life of cardiac patients.2 The improved prognosis and life expectancy of cardiac patients calls for more intensive and expedient attention of cardiac health care workers. Medical specialists are frequently confronted with elderly patients with multiple pathologies within a single organ system, such as myocardial infarction in heart failure patients, as well as multiple comorbidities of multiple organ systems.2-6Therefore, new and more efficient treatment strategies are needed. The involvement of specialised nurses in the medical care of preselected patient groups could become one such strategy.7,8 This was developed in the Anglo-American health care system and is also becoming a reality on the European continent. Nurse specialists/practitioners can play an intermediate role between the attending consultants, nurses and patients. Nurse practitioner care in the Medical Centre Alkmaar has been embedded for several years. The nurse practitioners on the cardiology ward are well trained; they work with multidisciplinary evidence-based protocols and work independently for the most part, supervised by a cardiologist.9 Earlier we demonstrated the safety of patient management by a nurse practitioner for stable patients after a recent myocardial infarction.10 However, it is known that implementation of results from highly controlled research projects in daily practice is not easy and is often not done.11
The aim of the present study is to identify non-highrisk post MI patients and confirm the feasibility of clinical and outpatient treatment by a nurse practitioner in this patient group with respect to reducing length of stay while maintaining good clinical outcomes in a large unselected stable population.
Patients and methods
All consecutive patients admitted to the coronary care unit at the Medical Centre Alkmaar with an acute myocardial infarction, chest pain, ECG changes and CK-MB level >20 U/l, were eligible for this study. Patients were recruited betweenNovember 2001 and November 2006 and followed for 30 days.
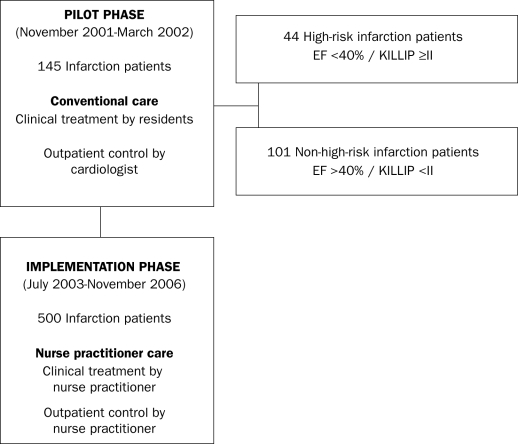
The pilot phase (November 2001 to March 2002) was designed to explore whether a stable post-MI group could be identified to be included in a nurse practitioner interventionstudy. In this phase, 145 consecutive patients were assessed and multivariate analysis was performed to reveal clinical parameters which could be predictive of post-MI complications. Only stable, non-high-risk MI patients were managed by a nurse practitioner.
The safety phase (March 2002 to July 2003) consisted of a randomised trial of 200 consecutive patients in which the safety of nurse practitioner intervention was compared with conventional care and is described earlier.10
The implementation phase (July 2003 to November 2006) consisted of 500 consecutive stable post- MI patients who were managed by a nurse practitioner (figure 1).
Figure 1.
Patient flowchart.
Patient management
Conventional care
Patients in the pilot phase were managed as usual by the resident and the attending cardiologist, and subsequently at the cardiologist outpatient clinic. They treated the patients within the limits of their medical profession, using the prevailing guidelines. These patients were not seen by the nurse practitioner during or after theirhospitalstay. Patient education and referral to cardiac rehabilitation was performed by nurses of the department of cardiology.
Nurse practitioner care
Nurse practitioner intervention involved daily clinical rounds performed by the nurse practitioner; the necessary clinical decision-making, for example the moment of discharge, was supervised by the attending cardiologist. The nurse practitioner used written protocols for the prescription of medication in acute coronary syndromes and for secondary prevention, in consultation with the cardiologist if needed. Further interventions offered by the nurse practitioner included educating the patient about myocardial infarctionand its treatment, prescribing all appropriate treatment and lifestyle changes (drugs, diet, exercise), teaching selfmonitoring and management (especially the early detection and treatment of chest pain), coordination of care with other health care and physiotherapists as required, and providing rehabilitation support.10
In both groups all participants were given a pocketsized booklet containing an explanation of infarction and its treatment; dietary advice; contact details and a list of their drugs.
Endpoints
The endpoints were death from any cause and reinfarction at 30 days. In the confirmation phase, we evaluated whether the nurse practitioner intervention could reduce the length of hospital stay while the safety was maintained.
Statistics
To reveal clinical parameters which could be predictive of post-MI complications multivariate analysis was performed. We looked at baseline (age, gender) and treatment characteristics, risk factors for cardiovascular disease and diagnosis (e.g. physical signs at admission, left ventricle function, ST deviation at admission ECG, infarct location) in this analysis.
Differences between the two non-high-risk groups were analysed with the t-test and the Χ2 test. A p value smaller than 0.05 was considered statistically significant. All multivariate analyses were performed using ANOVA. We used the Statistical Package for the Social Sciences (SPSS), version 11.5 (SPSS Inc.; Chicago, IL, USA) for the analyses.
Results
Pilot phase
In the pilot phase, 145 consecutive patients were followed. In this phase, 7% of all patients died due to cardiac causes and all within the first 48 hours after admission while still on the coronary care unit (CCU). Independent predictors for death were a lowered left ventricle function and/or signs of pulmonary oedema in the admission phase (Killip class ≥2). The high-risk patients were typically older, had double or triple vessel disease and were less frequently treated by angioplasty (table 1).
Table 1.
Pilot phase: baseline and treatment characteristics.
| High-risk patients | Non-high-risk patients | P value | |
|---|---|---|---|
| Baseline characteristics | |||
| Number of patients | 44 | 101 | |
| Mean age (years) | 73 (SD±12) | 65 (SD±12) | 0.000 |
| Number of men | 26 (59) | 72 (72) | 0.149 |
| Risk factors | |||
| Hypertension | 16 (36) | 35 (35) | 0.843 |
| Hypercholesterolaemia | 14 (32) | 51 (51) | 0.038 |
| Diabetes | 12 (27) | 21 (21) | 0.392 |
| Smoking | 11 (25) | 49 (49) | 0.008 |
| Family history | 10 (23) | 38 (38) | 0.080 |
| Diagnosis | |||
| Anterior infarction | 17 (39) | 37 (37) | 0.819 |
| Inferior infarction | 14 (32) | 35 (35) | 0.740 |
| STEMI | 17 (39) | 61 (60) | 0.802 |
| >1 CAD | 41 (93) | 60 (60) | 0.000 |
| Peak CK-MB mean (U/l) | 134 | 126 | 0.712 |
| Sum ST deviation (mean mm) | 9 (SD±6) | 9 (SD±8) | 0.866 |
| Treatment | |||
| Revascularisation | 15 (34) | 54 (54) | |
| - Primary PCI | 10 (23) | 40 (40) | 0.025 |
| - Thrombolysis | 5 (11) | 14 (14) | 0.682 |
| Medication | 29 (66) | 42 (42) | 0.007 |
Number of patients (%). High-risk patients=heart failure / ejection fraction <40%, non-high-risk patients=no heart failure / ejection fraction >40%, STEMI=STsegment-elevation myocardial infarction, CAD=coronary artery disease, PCI=percutaneous coronary intervention.
In contrast, patients admitted without heart failure or pre-existent depressed LV function proved to be a stable group. This patient group was more frequently treated by (primary) angioplasty. Therefore, these criteria were added to the earlier assigned infarction criteria and the nurse practitioner intervention started on the moment the patients were transferred from the CCU to the ward.
Implementation phase
Clinical and infarction characteristics of the non-highrisk patients in the pilot and implementation phase are comparable (table 2). The mean age was over 60 years and over 70% were men. Risk factors for cardiovascular disease were comparable, except that in the pilot phase there was a significantly higher occurrence of diabetes compared with the nurse practitioner group: 21 versus 12%.
Table 2.
Non-high-risk groups: baseline and treatment characteristics.
| Pilot phase | Implementation phase | P value | |
|---|---|---|---|
| (Conventional care) | (Nurse practitioner care) | ||
| Baseline characteristics | |||
| Number of patients | 101 | 500 | |
| Mean age (years) | 65 (SD±12) | 63 (SD±13) | 0.883 |
| Number of men | 72 (72) | 372 (74) | 0.509 |
| Risk factors | |||
| Hypertension | 35 (35) | 199 (40) | 0.341 |
| Hypercholesterolaemia | 51 (51) | 219 (44) | 0.211 |
| Diabetes | 21 (21) | 60 (12) | 0.018 |
| Smoking | 49 (49) | 229 (45) | 0.632 |
| Family history | 38 (38) | 199 (40) | 0.667 |
| Diagnosis | |||
| Anterior infarction | 37 (37) | 147 (29) | 0.147 |
| Inferior infarction | 35 (35) | 205 (41) | 0.221 |
| STEMI | 61 (60) | 347 (69) | 0.021 |
| > 1 CAD | 60 (60) | 203 (41) | 0.006 |
| Peak CK-MB mean (U/l) | 126 | 126 | 0.975 |
| Sum ST deviation (mean mm) | 9 (SD±8) | 9 (SD±7) | 0.833 |
| Treatment | |||
| Revascularisation | 54 (54) | 319 (64) | |
| - Primary PCI | 40 (40) | 317 (64) | 0.000 |
| - Thrombolysis | 14 (14) | 2 (0) | 0.000 |
| Medication | 42 (42) | 180 (36) | 0.287 |
Number of patients (%). STEMI=ST-segment-elevation myocardial infarction, CAD=coronary artery disease, PCI=percutaneous coronary intervention.
At hospital admission, 37% of the patients suffered from an inferior myocardial infarction. There were more multi-vessel disease patients in the pilot phase, 60% compared with 41% in the nurse practitioner phase. The mean CK-MB level and the sum ST deviation on the admission ECG were comparable. Of the patients, 56% were eligible for revascularisation therapy, 97% of whom were treated by primary PCI.
Clinical outcome
Two patients in this study died, both in the pilot phase in the 30-day follow-up. Re-infarction rates were comparable in the phases; 1% in each phase. There were no significant differences between the groups (table 3).
Table 3.
Non-high-risk groups: 30-day follow-up aand admission time.
| Pilot phase | Implementation phase | P value | |
|---|---|---|---|
| (Conventional care) | (Nurse practitioner care) | ||
| Number of patients | 101 | 500 | |
| During admission | |||
| Event-free | 98 (97) | 497 (99) | |
| Death | 2 (2) | 0 | 0.002 |
| Re-infarction | 1 (1) | 3 (0.6) | 0.659 |
| 30 days after discharge | |||
| Event-free | 98 (97) | 496 (99) | |
| Death | 2 (2) | 0 | |
| Re-infarction | 1 (1) | 4 (0.9) | 0.653 |
| Length of stay | |||
| Total (days) | 11.1 (SD±10) | 6.2 (SD±6) | 0.000 |
Number of patients (%).
Efficacy outcome
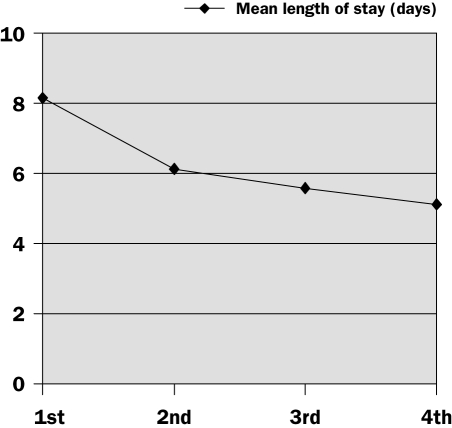
The mean length of stay was significantly longer in the pilot phase: 11.1 days compared with 6.2 days in the nurse practitioner phase. Multivariate analyses showed that independent predictors for length of stay included age, multi-vessel disease and the need for coronary artery bypass grafting.
In the nurse practitioner phase, the length of hospital stay for these stable post-infarction patients was 4.9 days shorter (11.1 vs. 6.2 days; p=0.000) compared with the non-high-risk patients in the pilot phase. This reduction in hospital stay was achieved gradually. The overall length of stay decreased from 8.1 days in the first quarter (SD±4) to 5.1 days in the fourth quarter (figure 2). If we combine the length of stay with the initial infarction therapy, for example primary PCI, or with additional treatment such as a CABG we see a wider length of stay range between 4 and 23 days. The improved efficacy was not accompanied by any increase in 30-day clinical complication rates.
Figure 2.
Mean length of stay for nurse practitioner care (per quartile).
Discussion
This study confirms the safety and feasibility of clinical and outpatient treatment of non-high-risk post-MI patients by a nurse practitioner in a general cardiology clinical practice. Following our previous experience, it also shows the efficacy of a nurse-led infarction unit with a 56% decrease in length of hospital stay. The identification of a non-high-risk post-infarction patient group is of imminent importance in selecting eligible patients for this approach of task shifting.
Quality and education
Our results indicate that treatment by a nurse practitioner achieves comparable clinical outcomes when compared with conventional care. This supports the role of nurse practitioner intervention in the secondary and tertiary health care of stable non-high-risk patients after acute myocardial infarction. Randomised trials have evaluated such interventions12-17 and several trials have also supported the concept of nurse-led interventions and most studies showed improved patient satisfaction and a high level quality of care.
In our opinion the most important contributors to this success are the clinical training of nurse practitioners and adequate patient selection. The training programme in the Netherlands consists of a two-year theoretical training at master level and a clinical hands-on training on a specific cardiology ward. Only experienced registered nurses are allowed to participate in this training programme. This leads to an advanced practice nurse who can act at an expert level for a particular patient group and specialism. The practical training of the nurse practitioner in the hospital should preferably be integrated into an existing training structure such as a programme for fellows and residents. A dedicated and homogeneous group of specialists is the basis of a good ‘teaching on the job’ principle.
Patient selection
Careful identification of well-described stable patients diagnosed with a recent myocardial infarction is the second important contributor to success. To identify stable and non-high-risk MI patients, valid risk stratification tools are available. These tools are very useful in acute MI patients treated with primary PCI,18,19 or in patients with specific ECG deviations.20 In the pilot phase of our study all infarction patients (chest pain, ECG changes and CK-MB level >20 U/l), independent of their treatment, were included. In this phase we evaluated the clinical outcome and investigated when these patients could be marked as ‘stable’ as an important starting point for nurse practitioner care. In this group we found a 7% mortality rate. All patients who died were still on the CCU suffering from acute heart failure or had a reduced left ventricular function (ejection fraction <40%). These local findings in a small group (145 patients) were added to the earlier criteria. Therefore, recent MI patients without signs of heart failure and transferred to the ward were selected for inclusion in this protocol.
The group remained representative for Dutch infarction patients. Our observed 2% mortality rate and 2% re-infarction rate were comparable with the literature.21 Our earlier experience was confirmed in a subsequent randomised trial of 200 consecutive patients comparing nurse practitioner intervention with conventional care. This study showed that nurse practitioners can deliver qualitatively equal care to stable patients with a recent myocardial infarction with a higher level of patient satisfaction as compared with conventional care.10
Clinical pathways
Our results confirm the importance of the concept of a nurse practitioner intervention using standardised care embedded in a clinical pathway.22 With increasing experience, the nurse practitioner phase did show a significant decrease in length of stay, and with a similar safety profile at 30-day follow-up. These data confirm the beneficial outcome effects of our newly constructed clinical framework in the care of infarction patients when implemented in daily practice.
The importance of an expedient treatment strategy, including the use of primary angioplasty, for infarction patients at the time of (pre)hospital diagnosis is universally accepted. Correspondingly, it should be similarly important to set up an efficient clinical framework of care for patients who recover from their infarction in order to maintain the initial beneficial effects of expedient therapy. Such clinical frameworks should include standing orders and should use the toolboxes that have been developed for getting guidelines into practice. Nurse practitioners can develop, implement, evaluate and improve such pathways on an evidence-based level. The included nurse intervention protocols may also serve as a platform to gain a higher level of guideline adherence. Hospitals that foster such dedicated nurse intervention projects might easily also serve as an ‘expert centre’ for nurses, residents and other health care workers in the treatment of acute myocardial infarction. Developing a rotational shift programme for young nurses and residents in training to the nurse practitioner-led clinic can quickly familiarise them with the management of acute myocardial infarction and its evidence-based standards of care.
Conclusion
Nurse practitioners can deliver qualitatively equal care to non-high-risk patients with a recent myocardial infarction as compared with conventional care. Embedding experienced nurse practitioners in clinical wards within critical care pathways may result in significant decreases in length of stay.
References
- 1.American Heart Association 2004. Heart disease and stroke statistics – 2004 update. Dallas Texas. Available at www.americanheart.org [Google Scholar]
- 2.Fye WB, Hirshfeld JW. 35th Bethesda conference report: cardiology workforce crisis: a pragmatic approach. JACC 2004;44:215-75 [Google Scholar]
- 3.Escaned J, Rydén L, Zamorano JL, Poole-Wilson P, Fuster V, Gitt A, et al. Trends and contexts in European cardiology practice for the next 15 years: the Madrid Declaration: a report from the European Conference on the Future of Cardiology, Madrid, 2-3 June 2006. Eur Heart J 2007;28:634-7. [DOI] [PubMed] [Google Scholar]
- 4.Lambrew CJ, Dove JT, Friday BA, Lloyd Doherty C, Nocero MA Jr, et al. Working group 5: innovative care team models and processes that might enhance efficiency and productivity. JACC 2004;44:251-6. [DOI] [PubMed] [Google Scholar]
- 5.Mehta RH, Montoye CK, Faul J, Nagle DJ, Kure J, Raj E, et al., for the American College of Cardiology Guidelines Applied in Practice Steering Committee. Enhancing quality of care for acute myocardial infarction : shifting the focus of improvement from key indicators to process of care and tool use. JACC 2004;43:2166-73 [DOI] [PubMed] [Google Scholar]
- 6.Adamson Ph, Abraham W, Love Ch, Reynolds D. The evolving challenge of chronic heart failure management. JACC 2004;44:1354-7 [DOI] [PubMed] [Google Scholar]
- 7.Stewart S. Caring for older patients with chronic cardiac disease: an increasing challenge for cardiac nurses in the 21st century. Eur J Cardiovasc Nurs 2002;1:11-3 [DOI] [PubMed] [Google Scholar]
- 8.Luttik ML, Veeger NJ, van Veldhuisen DJ. Design and methodology of the COACH study: a multicenter randomised coordinating study evaluating outcomes of advising and counseling in heart failure. Eur J Heart Fail 2004;6:227-33 [DOI] [PubMed] [Google Scholar]
- 9.Broers C, Umans V. Medisch handelen door de nurse practitioner; introductie en toegevoegde waarde binnen de cardiologie. Zorg en Management 2005;21:10:2-6. [Google Scholar]
- 10.Broers C, Smulders J, van der Ploeg Tj, Arnold A, Umans V. Nurse practitioner: equally as good as a resident in the treatment of stable patients after recent myocardial infarction and more patient satisfaction. NTvG 2006;150:2544-8 [PubMed] [Google Scholar]
- 11.Blomkalns AL, Roe MT, Peterson ED, Ohman EM, Fraulo ES, Gibler WB. Guideline implementation research: exploring the gap between evidence and practice in the CRUSADE Quality Improvement Initiative. Acad Emerg Med 2007;141:949-54 [DOI] [PubMed] [Google Scholar]
- 12.Jaarsma T, Van Der Wal MH, Lesman-Leegte I, Luttik ML, Veeger NJ, Sanderman R, et al., for the COACH investigators. Effect of moderate or intensive disease management program on outcome in patients with heart failure: coordinating study evaluating outcomes of advising and counseling in heart failure (COACH). Arch Intern Med 2008;168:316-24 [DOI] [PubMed] [Google Scholar]
- 13.de la Porte PW, Lok DJ, van Veldhuisen DJ, van Wijngaarden J, Cornel JH, Zuithoff NP, et al. Added value of a physician-andnurse-directed heart failure clinic: results from the Deventer-Alkmaar heart failure study. Heart 2007;93:819-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stables RH, Booth J, Welstand J, Wright A, Ormerod OJ, Hodgson WR. A randomised controlled trial to compare a nurse practitioner to medical staff in the preparation of patients for diagnostic cardiac catheterisation: the study of nursing intervention in practice (SNIP). Eur J Cardiovasc Nurs 2004;3:53-9. [DOI] [PubMed] [Google Scholar]
- 15.Broers C, Hogeling J, Burgersdijk C, Cornel JH, Van der Ploeg Tj, Umans, V. Efficacy of a Nurse led Clinic for post operative Coronary Artery Bypass Grafting Patients. Int J Cardiol 2006;106:111-5. [DOI] [PubMed] [Google Scholar]
- 16.Sakr M Angus J, Perrin J, Nixon C, Nicholl J, Wardrope J. Care of minor injuries by emergency nurse practitioners or junior doctors: a randomised controlled trial. Lancet 1999;354:1321-6. [DOI] [PubMed] [Google Scholar]
- 17.Horrocks S, Anderson E, Salisbury Ch. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324:819-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Luca G, Suryapranata H, Van ’t Hof A, de Boer MJ, Hoorntje J, Dambrink JH, et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty. Circulation 2004;109:2737-43. [DOI] [PubMed] [Google Scholar]
- 19.Kandzari D, Tcheng J, Cohen D, Bakhai A, Grnies C, Cox D, et al., for the CADILLAC investigators: Feasibility and implications of an early discharge strategy after percutaneous intervention with abciximab in acute myocardial infarction (the CADILLAC trial). Am J Cardiol 2003;92:779-84. [DOI] [PubMed] [Google Scholar]
- 20.Morrow D, Antman E, Charlesworth A, Cairns R, Murphy S, de Lemos J, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000;102:2031-7. [DOI] [PubMed] [Google Scholar]
- 21.Zwakhals SL, Giesbers H, Mac Gillavry E, van Boven PF, van der Veen AA. The Dutch National Atlas of Public Health Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2004;47:882-9. [DOI] [PubMed] [Google Scholar]
- 22.De Bleser L, Depreitere R, De Waele K, Vanhaecht K, Vlayen J, Sermeus W. Defining pathways. J Nurs Manag 2006;14:553-63. [DOI] [PubMed] [Google Scholar]