Abstract
Iatrogenic acute dissection of the ascending aorta during percutaneous coronary intervention occurs rarely. Localized aortic dissections may be treated by sealing the entry with a coronary stent. However, extensive dissections may require a surgical intervention. A case of iatrogenic coronary dissection with extensive propagation into the ascending aorta during angioplasty of the right coronary artery is presented. The aortic dissection was successfully treated by stenting at the right coronary artery ostium. Follow-up computed tomography and coronary angiography showed complete resolution of aortic dissection.
Keywords: Aortic dissection, Complication, Percutaneous coronary intervention
Abstract
Une dissection iatrogène aiguë de l’aorte ascendante durant une intervention coronarienne percutanée est un événement rare. Les dissections aortiques localisées peuvent être traitées en obturant le point d’entrée au moyen d’une endoprothèse coronarienne. Toutefois, les dissections importantes peuvent nécessiter une intervention chirurgicale. On présente ici un cas de dissection coronarienne iatrogène avec propagation dans toute l’aorte ascendante durant une angiographie de la coronaire droite. La dissection aortique a été réalisée avec succès par endoprothèse à l’embouchure de la coronaire droite. La tomographie et la coronarographie de suivi ont montré une résolution complète de la dissection aortique.
Coronary artery dissection is a well-known complication of coronary angiography and angioplasty. Infrequently, iatrogenic coronary dissection may result in retrograde extension into the ascending aorta and further (1–3). Iatrogenic aortic dissections (ADs) that are localized a few centimetres beyond the aortic valve may be treated by sealing the entry point by means of coronary stenting (4). However, an extensive dissection involving the ascending aorta may be life-threatening and often requires urgent surgical intervention (3,5). We report a case of iatrogenic coronary dissection extending into the entire ascending aorta that was successfully resolved by coronary stenting at the entry point.
CASE PRESENTATION
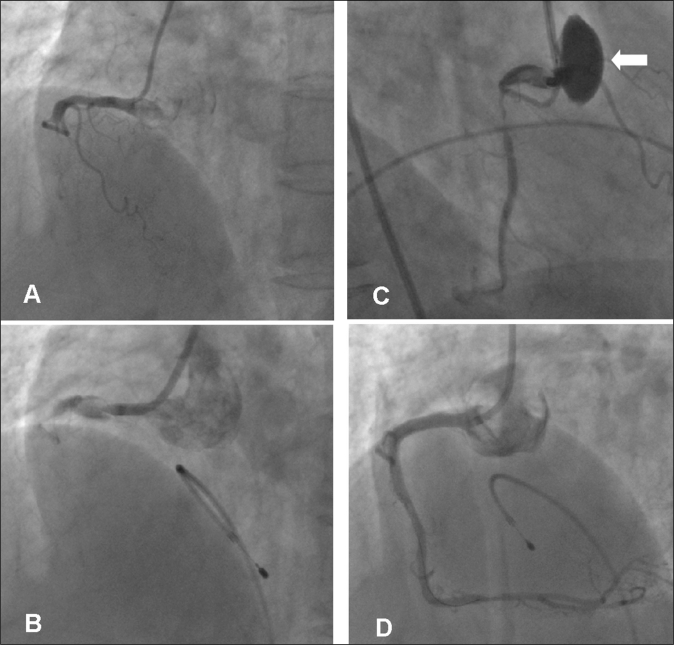
A 68-year-old woman with hypertension, diabetes and dyslipidemia was admitted for effort angina for four months. She was taking acetylsalicylic acid, amlodipine, carvedilol, atorvastatin and glimepiride. The technetium-99m sestamibi scan showed severe reversible ischemia at the inferior and posterolateral wall. Coronary angiography via the femoral approach revealed chronic total occlusion (CTO) in the mid-portion of the right coronary artery (RCA) (Figure 1A). There were other significant stenoses without occlusions in the mid-portion of the left anterior descending artery and the distal site in the left circumflex artery. The left anterior descending artery and left circumflex artery supplied good collateral flow to the occluded RCA.
Figure 1).
Coronary angiogram. A Left anterior oblique view showing total occlusion in the mid-portion of the right coronary artery (RCA). B After engagement of the guiding catheter, a dissection of the proximal RCA was developed. C Right anterior oblique view showing progression of the dissection into the sinus of Valsalva (arrow). D Follow-up angiogram after coronary stenting demonstrating no residual stenosis in the stented segment, with good distal flow
Percutaneous coronary intervention (PCI) to the CTO of the RCA was planned. A loading dose of clopidogrel (300 mg) was given orally and an intravenous bolus of heparin (10,000 IU) was administered. A 7 Fr JR4 guiding catheter was engaged in the ostium of the RCA. Before attempting to pass the wire, contrast medium was injected; this revealed a dissection of the proximal RCA (Figure 1B). A 0.014 in guidewire (Whisper; Guidant Corporation, USA) was successfully passed down into the distal RCA across the total occlusion. However, a follow-up angiogram showed progression of the dissection into the sinus of Valsalva (Figure 1C), and the patient suddenly complained of anterior chest pain and back pain without ST segment change on the electrocardiogram. Hemodynamic conditions were stable. After predilation with a 1.5 mm balloon, a 3.0 mm × 18 mm Driver stent (Medtronic Inc, USA) was implanted in the CTO lesion. A second Driver stent (3.5 mm × 24 mm) was implanted in the ostium of the RCA to seal off the entry point of the dissection, proximally to the first stent. A follow-up angiogram demonstrated no residual stenosis in the stented segment with good distal flow and no further extravasation of contrast medium (Figure 1D). However, persistent contrast staining was observed along the aortic wall of the ascending aorta up to the aortic arch on the final angiogram (Figure 2). Because the patient was stabilized after stent implantation and the AD was stable, apparently with no progression, conservative management was decided.
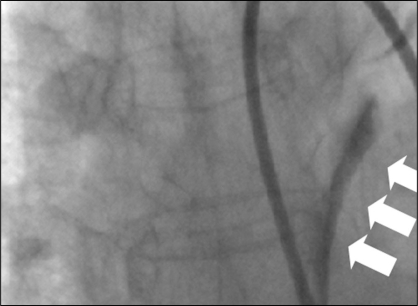
Figure 2).
Persistent contrast staining was observed along the aortic wall of the ascending aorta up to the aortic arch (arrows) on the final cineradiography after percutaneous coronary intervention
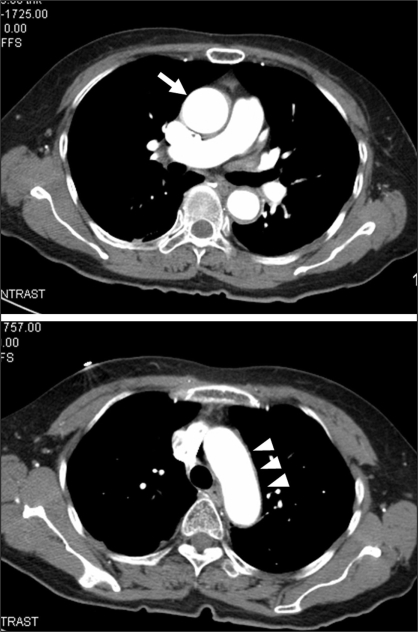
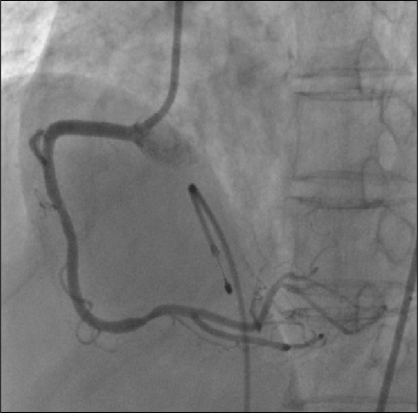
A computed tomography scan performed immediately after the PCI demonstrated complete resolution of the dissection without an intimal flap (Figure 3). A follow-up angiography was performed the next day and it revealed patent stents without residual contrast staining of the aortic wall (Figure 4). The patient was discharged four days after the PCI and remained asymptomatic for one year without any clinical event.
Figure 3).
Computed tomography performed after the coronary intervention showing complete resolution of the dissection. No intimal flap was observed in the ascending aorta (arrow) or aortic arch (arrowheads)
Figure 4).
Follow-up angiogram performed the next day, demonstrating no residual contrast staining of the aortic wall and no further extravasations of contrast medium
DISCUSSION
Iatrogenic AD is an uncommon and severe complication during cardiac catheterization, with an incidence of 0.02% (3). In many cases, the entry site is located in the coronary artery where a dissection occurs following trauma caused by the tip of the guiding catheter or balloon dilation. A vigorous manual injection of contrast medium into the subintimal space appears to play a major role in extending the dissection retrogradely to the aortic root. In the present case, the trigger for the AD was thought to be a coronary dissection caused by the tip of the guiding catheter, which damaged the ostium of the RCA. Extension of the coronary dissection to the Valsalva sinus and the ascending aorta was possibly the result of raised coronary flow pressure from the contrast injection (1,2).
If a dissection is limited to the aortic sinus of Valsalva, it will resolve with conservative treatment only. However, when it extends over the aortic sinus of Valsalva, the treatment of an iatrogenic AD is still controversial. Dunning et al (3) retrospectively reviewed nine coronary artery-ADs and reported that patients with limited aortic involvement were successfully managed with stenting of the entry point of the coronary dissection, whereas ADs extending more than 40 mm in length required surgical intervention (3). However, in some cases, excluding the entry point from the bloodstream by coronary stenting was sufficient to prevent extension of the AD. In addition, this conservative management, defined as the ‘watchful waiting’ strategy, showed a favourable evolution and constituted the definitive therapy (6).
In our case, an extensive iatrogenic AD extending up to the entire ascending aorta without hemodynamic compromise had been effectively treated by coronary stent implantation. Stenting of the ostium of the RCA sealed the entry point of the dissection, preventing its further progression. The present case report suggests that if the patient is hemodynamically stable, sealing the coronary entry door with a coronary stent and excluding dissection progression with computed tomography surveillance can be a reasonable strategy even in the case of an extensive dissection of the ascending aorta, reserving surgery for cases with documented progression of the dissection.
REFERENCES
- 1.Moles VP, Chappuis F, Simonet F, et al. Aortic dissection as complication of percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn. 1992;26:8–11. doi: 10.1002/ccd.1810260103. [DOI] [PubMed] [Google Scholar]
- 2.Perez-Castellano N, Garcia-Fernandez MA, Garcia EJ, Delcan JL. Dissection of the aortic sinus of Valsalva complicating coronary catheterization: Cause, mechanism, evolution, and management. Cathet Cardiovasc Diagn. 1998;43:273–9. doi: 10.1002/(sici)1097-0304(199803)43:3<273::aid-ccd7>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 3.Dunning DW, Kahn JK, Hawkins ET, O’Neill WW. Iatrogenic coronary artery dissections extending into and involving the aortic root. Catheter Cardiovasc Interv. 2000;51:387–93. doi: 10.1002/1522-726x(200012)51:4<387::aid-ccd3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 4.Al-Saif SM, Liu MW, Al-Mubarak N, Agrawal S, Dean LS.Percutaneous treatment of catheter-induced dissection of the left main coronary artery and adjacent aortic wall: A case report Catheter Cardiovasc Interv 20004986–9.discussion 90. [DOI] [PubMed] [Google Scholar]
- 5.Yip HK, Wu CJ, Yeh KH, et al. Unusual complication of retrograde dissection to the coronary sinus of valsalva during percutaneous revascularization: A single-center experience and literature review. Chest. 2001;119:493–501. doi: 10.1378/chest.119.2.493. [DOI] [PubMed] [Google Scholar]
- 6.Maiello L, La Marchesina U, Presbitero P, Faletra F. Iatrogenic aortic dissection during coronary intervention. Ital Heart J. 2003;4:419–22. [PubMed] [Google Scholar]