Abstract
BACKGROUND
Hospital discharge data are used extensively in health research. Given the clinical differences between ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI), it is important that these entities be distinguishable in a medical record. The authors sought to determine the extent to which the type of MI is recorded in medical records, as well as the consistency of this designation within individual records.
METHODS
Records of all MI patients admitted to a tertiary care centre in Canada from April 1, 2000, to March 31, 2001, were reviewed. Documentation and consistency of the use of the terms STEMI (Q wave, ST elevation or transmural MI) or NSTEMI (non-Q wave, subendocardial or nontransmural MI) were assessed in the admission history, progress notes, coronary care unit summary and discharge summary sections of each record.
RESULTS
Missing data were common; each chart section mentioned MI type in fewer than one-half of charts. When information was combined, it was possible to determine the type of MI in 81.1% of cases. MI type was consistently described as STEMI in 48.7% of cases, and as NSTEMI in 32.4%. Of concern, MI type was discrepant across sections in 10.5% of cases and missing entirely in 8.4% of cases.
CONCLUSIONS
The designation of MI cases as STEMI or NSTEMI is both incomplete and inconsistent in hospital records. This has implications for health services research conducted retrospectively using medical record data, because it is difficult to comprehensively study processes and outcomes of MI care if the type cannot be retrospectively determined.
Keywords: Diagnosis, Health services research, Myocardial infarction, Population
Abstract
HISTORIQUE
Les données de congé hospitalier sont largement utilisées dans les recherches en santé. Étant donné les différences cliniques entre l’infarctus du myocarde (IM) avec élévation du segment ST (IMAST) et l’IM sans élévation du segment ST (IMSST), il est important de distinguer ces entités dans les dossiers médicaux. Les auteurs ont cherché à déterminer à quel point le type d’IM est précisé dans les dossiers médicaux, de même que l’uniformité de la désignation dans chaque dossier.
MÉTHODOLOGIE
Les auteurs ont examiné les dossiers de tous les patients atteints d’un IM hospitalisés dans un centre de soins tertiaires du Canada entre le 1er avril 2000 et le 31 mars 2001. Ils ont évalué la documentation et l’uniformité d’utilisation des termes IMAST (onde Q, élévation du segment ST ou IM transmurale) ou IMSST (sans onde Q, IM sous-endocardiaque ou non transmurale) dans l’histoire d’admission, les notes des progrès, le résumé de l’unité cardiaque et le résumé du congé de chaque dossier.
RÉSULTATS
Il manquait souvent des données. En effet, le type d’IM était précisé dans chaque partie de moins de la moitié des dossiers. Lorsqu’on combinait l’information, il était possible de déterminer le type d’IM dans 81,1 % des cas. Le type d’IM était uniformément désigné comme un IMAST dans 48,7 % des cas, et comme un IMSST dans 32,4 % des cas. Il est inquiétant de constater que le type d’IM divergeait d’une section à l’autre dans 10,5 % des dossiers et n’était pas du tout précisé dans 8,4 % d’entre eux.
CONCLUSIONS
La désignation des cas d’IM comme un IMAST ou un IMSST est à la fois incomplète et non uniforme dans les dossiers hospitaliers. Ce phénomène a des répercussions sur les recherches rétrospectives en santé faisant appel aux données des dossiers médicaux, car il est difficile d’étudier les processus et les issues de l’IM de manière approfondie s’il est impossible d’en déterminer le type de manière rétrospective.
Major changes have occurred in the definition, diagnosis and management of myocardial infarction (MI). The concept of ‘acute coronary syndrome’, with its subdivisions into ST segment elevation myocardial infarction (STEMI [Q wave, ST elevation or transmural MI]) and non-ST segment elevation myocardial infarction (NSTEMI [non-Q wave, subendocardial or nontransmural MI]) (1), is now widely accepted. Defining the type of MI facilitates treatment, and incorporation of available evidence has now produced separate guidelines for the management of these patients (2,3). Thus, it is important that these two clinical entities be distinguishable in a medical record.
The primary goal of the current study was to determine the extent to which the type of MI (STEMI or NSTEMI) is being recorded in hospital medical records, as well as the consistency of this designation within individual records.
METHODS
A retrospective chart review was performed of all patients with a hospital discharge diagnosis of acute MI at the Foothills Hospital, Calgary, Alberta, from April 1, 2000, to March 31, 2001. This institution is the only tertiary care teaching hospital in Calgary in which interventional cardiology procedures are performed; thus, it also receives patients from other community hospitals. The local pattern of practice is to encourage primary percutaneous coronary intervention as first-line therapy in patients with STEMI.
A trained nurse/coder with extensive medical record and cardiology research experience examined all the retrieved charts. The nurse filled out a 52-item chart review form, on which one of the items of query was, “Is MI explicitly listed as STEMI (Q wave, ST elevation, transmural) or NSTEMI (non-Q wave, subendocardial, nontransmural) or not documented?” in each admission history, coronary care unit (CCU) progress notes, transfer notes and discharge summary section.
The percentage of STEMI and NSTEMI cases was reported for each admission history, CCU progress reports, transfer notes and discharge summary section. Patient records were categorized into four groups: consistently STEMI (STEMI documented in at least one of the four areas, with no contradictions elsewhere), consistently NSTEMI (NSTEMI documented in at least one area, with no contradictions), not stated (documented as unknown or missing in all four areas) and ‘discrepancy’ (both terms, STEMI and NSTEMI, were used in the chart).
The protocol also included electrocardiogram (ECG) interpretation by the nurse/coder, who had received previous training from an internist and a cardiologist, which is not typically done in health record reviews. Using the additional ECG data, a sensitivity analysis was performed to determine whether the availability of ECG data increased the ability to accurately classify MI cases.
RESULTS
The study population consisted of 581 acute MI patients, 71.1% of whom were male, with a mean age of 64.2 years.
Table 1 shows the usage of the terms STEMI (Q wave, ST elevation or transmural MI), NSTEMI (non-Q wave, subendocardial or nontransmural MI) or neither, as documented in the four specified areas of the hospital chart (admission history, CCU progress notes, transfer notes and discharge summary). For example, the admission history clearly used the term STEMI in 47.2% of cases, but the discharge summary noted this in only 11.2% of cases.
TABLE 1.
Type of myocardial infarction as documented in four areas of the hospital chart (n=581)
| Chart area | STEMI, n (%) | NSTEMI, n (%) | Neither, n (%) |
|---|---|---|---|
| Admission history | 274 (47.2) | 105 (18.1) | 202 (34.7) |
| CCU progress notes | 124 (21.3) | 173 (29.8) | 284 (48.9) |
| Transfer notes | 132 (22.7) | 133 (22.9) | 316 (54.4) |
| Discharge summary | 65 (11.2) | 141 (24.3) | 375 (64.5) |
CCU Coronary care unit; NSTEMI Non-ST segment elevation myocardial infarction; STEMI ST segment elevation myocardial infarction
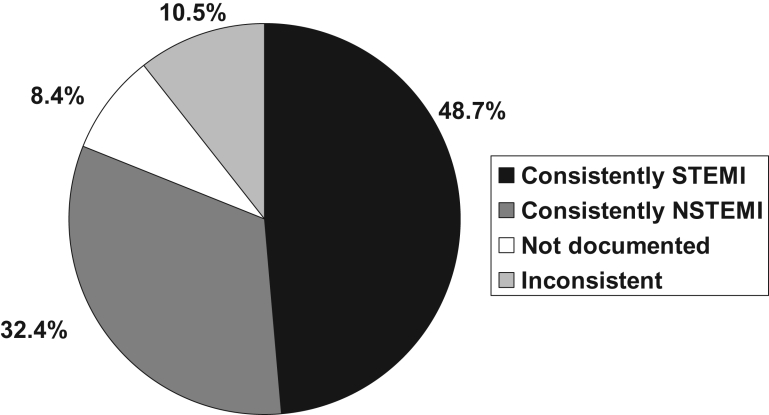
A diagnosis was considered to be ‘consistent’ if either STEMI or NSTEMI was designated in any one or more of the four areas of the chart, and not contradicted later in the documentation. In nine patients (1.6% of all cases) with STEMI and 38 patients (6.5% of all cases) with NSTEMI, the same designation was seen throughout all four areas of documentation. The remainder of the consistent cases used either STEMI (n=274 [47.2%]) or NSTEMI (n=150 [25.8%]) once throughout the documentation. As shown in Figure 1, consistent terminology for STEMI was used in 48.7% of all cases and consistent terminology for NSTEMI in 32.4%. However, in 18.9% of cases, it was impossible to determine MI type, with discrepancy across sections in 10.5% of cases, and MI type missing entirely in 8.4% of cases.
Figure 1.
Myocardial infarction type as documented in four areas of the medical records reviewed. NSTEMI Non-ST segment elevation myocardial infarction; STEMI ST segment elevation myocardial infarction
When ECG interpretation was added, STEMI and NSTEMI designations were possible in 42 of the 49 charts in which MI type was missing entirely from other parts of the chart. As shown in Table 2, this gain in ability to classify MI cases came at the cost of introducing confusion in 12 cases (2.1% of all patients), in which the ECG interpretation conflicted with otherwise consistent documentation.
TABLE 2.
Comparison of nurse electrocardiogram interpretation with chart-reported diagnosis (n=581)
| Chart-reported diagnosis, n
|
||||
|---|---|---|---|---|
| Electrocardiogram | STEMI | NSTEMI | Neither | Both |
| Interpretation, n | ||||
| STEMI | 276 | 6 | 28 | 47 |
| NSTEMI | 6 | 164 | 14 | 14 |
| Uninterpretable, n | 1 | 18 | 7 | 0 |
NSTEMI Non-ST segment elevation myocardial infarction; STEMI ST segment elevation myocardial infarction
DISCUSSION
We have found evidence of incomplete and inconsistent documentation of MI type in medical records. Indeed, almost 20% of our patient population could not be used for retrospectively conducted health services research on type-specific assessment of MI management, due to contradictory terminology or the absence of MI descriptors altogether.
To our knowledge, the accuracy of using the newer designations of NSTEMI and STEMI in hospital records has not been systematically studied. The Global Registry of Acute Coronary Events (GRACE) (4) describes the global epidemiology, management and outcomes of acute coronary syndromes. Information is captured using a case report form, which includes clear definitions for STEMI and NSTEMI. Despite this, investigators found that establishing a clear-cut admission diagnosis was difficult because a large proportion of patients did not have a working diagnosis that matched their final diagnosis. Indeed, at admission, only 30% of NSTEMI patients had a working diagnosis of MI – the remainder were admitted with diagnoses that included unstable angina, ruling out of MI, chest pain and others (5). Our work expands this important finding from Global Registry of Acute Coronary Events (GRACE) (5), demonstrating inconsistency in the use of the diagnostic terms STEMI (Q wave, ST elevation or transmural MI) and NSTEMI (non-Q wave, subendocardial or nontransmural MI) in various areas of the hospital chart in a large Canadian tertiary care centre.
Hospital discharge coding data are used extensively, and are dependent on trained individuals obtaining data from information documented in patient medical records. While the accuracy of hospital discharge diagnosis coding for MI has been questioned by some (6), other investigators have shown that coding for acute MI is accurate, with high specificity, sensitivity and positive predictive value (7–16). Most of these studies used administrative data coded as per the International Classification of Disease, 9th edition (ICD-9). Currently, ICD-10 is being used internationally (17). The ICD-10 contains the following categories for acute MI: 121.0 – acute transmural MI of anterior wall, 121.1 – acute transmural MI of inferior wall, 121.2 –acute transmural MI of other sites, 121.3 – acute transmural MI of unspecified site, 121.4 – acute subendocardial MI and 121.9 – acute MI, unspecified. Institutions therefore equate transmural infarction with STEMI and subendocardial infarction with NSTEMI. Our findings are relevant to future coding practice, because the coders will require a chart review to decide on whether the MI is a STEMI or NSTEMI. In conducting these reviews, coders will likely encounter the same MI type inconsistency dilemma that we have demonstrated here. Given the interest in measuring door-to-needle and door-to-balloon times as quality indicators for STEMI, accurate coding of MI would make chart reviews for these indicators more efficient.
We expanded our classification attempts by including ECG interpretation in our review, which is not traditionally done with administrative data coding. Although this provided additional data in 42 of the 49 cases that lacked a declaration of MI type in the chart, it also had the detrimental effect of introducing new contradictions regarding MI type in 12 cases. In addition, when discrepancy already existed in various areas of the chart, the ECG interpretation of a nurse/coder was not enough to clarify the diagnosis.
The reasons for discrepant and missing documentation are not clear. The present chart review was conducted at an academic tertiary care training centre. Therefore, most documentation was performed by junior house staff, with variable understanding of the important differences between the clinical entities of STEMI and NSTEMI, coupled with relatively immature ECG interpretative skills. For example, a STEMI patient who received successful reperfusion therapy might have subsequently been misclassified as having had NSTEMI. Indeed, Iezzoni et al (18) have demonstrated inappropriateness in diagnostic coding of MI in teaching hospitals.
Limitations
There are limitations to the present study. We assessed data from a single tertiary care centre in Canada over a one-year period, shortly after the consensus redefinition of acute MI. However, we did consider this by also including older terminology, such as Q wave and non-Q wave MI, in our assessment. In addition, the chart reviews were not conducted by a physician. It is possible that some of the discrepant cases or those missing MI type completely might have been retrospectively adjudicated by a physician who can interpret clinical information at a higher level and arrive at the correct diagnosis. However, this is not typically done in health record assessments.
CONCLUSIONS
The designation of MI cases as STEMI or NSTEMI in hospital records is both incomplete and inconsistent. The addition of nurse/coder ECG interpretation provided additional information in some cases, but introduced discrepancy in others, and almost 20% of charts would be excluded in a retrospective analysis. This has implications for health services research conducted using medical record data, because it is difficult to comprehensively study processes and outcomes of MI care if the MI type can not be retrospectively determined. Our findings suggest an urgent need for improved education and documentation of STEMI and NSTEMI in medical records by physicians.
Footnotes
FUNDING: Analyses for this paper were supported by an operating grant from the Canadian Institutes of Health Research. Collaborations between researchers at the University of Alberta, University of Calgary and University of Toronto are supported through a Canadian Institutes of Health Research Team Grant in Cardiovascular Outcomes Research. Dr William A Ghali is supported by a Health Scholar Award from the Alberta Heritage Foundation for Medical Research, Edmonton, Alberta. Dr Jack V Tu is supported by a Heart and Stroke Foundation of Ontario Career Investigator Award. Both Drs William A Ghali and Jack V Tu are supported by the Government of Canada Research Chair Program in Health Services Research.
REFERENCES
- 1.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. (Erratum in 2001;37:973) [DOI] [PubMed] [Google Scholar]
- 2.Antman EM, Anbe DT, Armstrong PW, et al. American College of Cardiology; American Heart Association; Canadian Cardiovascular Society. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction – executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. (Erratum in 2005;45:1376) [DOI] [PubMed] [Google Scholar]
- 3.Braunwald E, Antman EM, Beasley JW, et al. American College of Cardiology; American Heart Association. Committee on the Management of Patients With Unstable Angina. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction –summary article: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina) J Am Coll Cardiol. 2002;40:1366–74. doi: 10.1016/s0735-1097(02)02336-7. [DOI] [PubMed] [Google Scholar]
- 4.GRACE Investigators. Rationale and design of the GRACE (Global Registry of Acute Coronary Events) Project: A multinational registry of patients hospitalized with acute coronary syndromes. Am Heart J. 2001;141:190–9. doi: 10.1067/mhj.2001.112404. [DOI] [PubMed] [Google Scholar]
- 5.Steg PG, Goldberg RJ, Gore JM, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am J Cardiol. 2002;90:358–63. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 6.Sapsford RJ, Lawrance RA, Dorsch MF, et al. Evaluation of Methods and Management of Acute Coronary Events Study Group. Identifying acute myocardial infarction: Effects on treatment and mortality, and implications for National Service Framework audit. QJM. 2003;96:203–9. doi: 10.1093/qjmed/hcg030. [DOI] [PubMed] [Google Scholar]
- 7.Mähönen M, Miettinen H, Pyörälä K, Molarius A, Salomaa V, Kuulasmaa K. Hospital discharge register data in the assessment of trends in acute myocardial infarction. FINMONICA AMI Register Study Team. Ann Med. 1995;27:547–54. doi: 10.3109/07853899509002467. [DOI] [PubMed] [Google Scholar]
- 8.Meehan TP, Hennen J, Radford MJ, Petrillo MK, Elstein P, Ballard DJ. Process and outcome of care for acute myocardial infarction among Medicare beneficiaries in Connecticut: A quality improvement demonstration project. Ann Intern Med. 1995;122:928–36. doi: 10.7326/0003-4819-122-12-199506150-00007. [DOI] [PubMed] [Google Scholar]
- 9.Mähönen M, Salomaa V, Brommels M, et al. The validity of hospital discharge register data on coronary heart disease in Finland. Eur J Epidemiol. 1997;13:403–15. doi: 10.1023/a:1007306110822. [DOI] [PubMed] [Google Scholar]
- 10.Petersen LA, Wright S, Normand SL, Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999;14:555–8. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA. Coding accuracy of hospital discharge data for elderly survivors of myocardial infarction. Can J Cardiol. 1999;15:1277–82. [PubMed] [Google Scholar]
- 12.Campbell SE, Campbell MK, Grimshaw JM, Walker AE. A systematic review of discharge coding accuracy. J Public Health Med. 2001;23:205–11. doi: 10.1093/pubmed/23.3.205. [DOI] [PubMed] [Google Scholar]
- 13.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–6. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 14.Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The validity of the diagnosis of acute myocardial infarction in routine statistics: A comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol. 2003;56:124–30. doi: 10.1016/s0895-4356(02)00591-7. [DOI] [PubMed] [Google Scholar]
- 15.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: Estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Rosamond WD, Chambless LE, Sorlie PD, et al. Trends in the sensitivity, positive predictive value, false-positive rate, and comparability ratio of hospital discharge diagnosis codes for acute myocardial infarction in four US communities, 1987–2000. Am J Epidemiol. 2004;160:1137–46. doi: 10.1093/aje/kwh341. [DOI] [PubMed] [Google Scholar]
- 17.International Classification of Diseases. < www.who.int/classifications/icd/en> (Version current at December 5, 2007)
- 18.Iezzoni LI, Burnside S, Sickles L, Moskowitz MA, Sawitz E, Levine PA. Coding of acute myocardial infarction. Clinical and policy implications. Ann Intern Med. 1988;109:745–51. doi: 10.7326/0003-4819-109-9-745. [DOI] [PubMed] [Google Scholar]