Abstract
The majority of adults sleep with a partner, and for a significant proportion of couples, sleep problems and relationship problems co-occur, yet there has been little systematic study of the association between close relationships and sleep. The association between sleep and relationships is likely to be bi-directional and reciprocal—the quality of close relationships influences sleep and sleep disturbances or sleep disorders influence close relationship quality. Therefore, the purpose of the present review is to summarize the extant research on 1) the impact of co-sleeping on bed partner's sleep; 2) the impact of sleep disturbance or sleep disorders on relationship functioning; and 3) the impact of close personal relationship quality on sleep. In addition, we provide a conceptual model of biopsychosocial pathways to account for the covariation between relationship functioning and sleep. Recognizing the dyadic nature of sleep and incorporating such knowledge into both clinical practice and research in sleep medicine may elucidate key mechanisms in the etiology and maintenance of both sleep disorders and relationship problems and may ultimately inform novel treatments.
Keywords: Marital quality, close relationships, sleep, sleep disorders
Sleep is both a shared human biological universal and a time of social interaction… (p. 240; (1))
Sleep is a vulnerable physiological state that optimally occurs when one feels sufficiently safe and secure to down-regulate vigilance and alertness. Across the lifespan, such feelings of safety and security are largely derived from the social environment (2). Conversely, impaired sleep adversely affects the ability to regulate emotions (3) and behavioral responses to interpersonal situations (4), suggesting a bi-directional association between sleep and the social environment. Given that the marital relationship is the primary social context for most adults and that most married adults sleep with their spouse, marriage may have important implications for sleep. Indeed, a substantial body of evidence suggests that marital status is associated with sleep outcomes, with the divorced typically having more sleep problems compared to their married or single counter-parts (5). However, all relationships are not equal. Marital role occupancy (i.e., married/ divorced/ single) reveals little about the qualitative aspects of close relationships that may influence sleep. For instance, amongst the divorced, Cartwright and Wood demonstrated significant reductions in the percentage of Delta sle ep between participants currently undergoing a divorce versus those for whom the divorce was complete (6). These results suggest that the stress of ongoing conflict in the midst of the divorce process reduces deep, restorative sleep. However, divorce is an imperfect proxy for how individuals perceive the quality of their relationship. In the close relationship literature, the subjective experience of the marriage (or other close relationship) is typically referred to as “marital/ relationship quality” or “marital/ relationship functioning” (7). Given the dyadic (pairing of two individuals) nature of sleep for most adults, there has been surprisingly little investigation of the influence of close relationship quality on sleep or conversely, the impact of sleep disturbance on close relationship quality.
Evaluating sleep and sleep disorders from a dyadic perspective is important for several reasons. First, according to the 2005 National Sleep Foundation poll, 61% of adults sleep with a significant other, and one-quarter to one-third of married or cohabitating adults report that their intimate relationships are adversely affected by their own or their spouse's excessive sleepiness or sleep problems. Recent qualitative studies from interview data suggest that sleep problems in one or both partners, including insomnia symptoms and sleep-disordered breathing, contribute to marital problems (8). In addition, Ulfberg and colleagues (9) found that women living with snorers were three times as likely to report symptoms of insomnia compared to women living with nonsnorers, suggesting that a sleep disorder in one spouse may increase risk for a sleep disorder in the other spouse, perhaps leading to additive or synergistic effects on the relationship quality.
Second, spouses or intimate partners are a primary source of social control; i.e., they exert a powerful influence on their partner's adherence or compliance to medical regimens, including treatment for sleep disorders, such as obstructive sleep apnea (OSA;(10)). Indeed, bed-partners play a prominent role in the diagnosis of sleep disorders, including OSA, which has been referred to as “a disease of listeners” (11). Such a label connotes not only the importance of including the bed-partner as an important source of corroborating data in the initial sleep evaluation, but also suggests that OSA is a disease that exacts a toll on the dyad, not just the patient. Therefore, including partners as active participants in sleep medicine interventions may improve compliance and cost-effectiveness of sleep treatments.
Third, life events such as the transition to parenthood (12) or adjustment to illness (e.g., (13, 14), are known to cause sleep impairments and precipitous declines in marital quality, suggesting that sleep quality may play a critical role in the trajectory of marital functioning. Despite the temporal concordance between life events associated with sleep disturbance and declines in marital quality, there has been scant study of the degree to which sleep disturbance precipitates changes in marital functioning following such life transitions (for an exception see (15)).
Finally, consideration of sleep may elucidate key pathways through which close relationships ultimately influence physical health and well-being. Marital quality predicts a diverse array of physical health outcomes, including cardiovascular diseases, chronic pain, and infectious illnesses (16). The potential mechanisms linking marital quality with health include behavioral (e.g., exercise, adherence to medical regimens), neuroendocrine, cardiovascular, and immune pathways. These traditional biopsychosocial mechanisms account for some, but not all of the association between marital quality and health. However, sleep is rarely investigated as a potential mediator of the marital quality-health relationship, despite well-documented health consequences of sleep disturbances (e.g., (17)) and the fact that most couples engage in this health behavior together.
In summary, most adults sleep with a partner, and for some, sleep problems and relationship problems co-occur, yet we know relatively little about the connections between close relationships and sleep. Therefore, the purpose of the present review is to summarize the extant research on 1) the impact of co-sleeping on bed partner's sleep; 2) the impact of sleep disturbance or sleep disorders on relationship functioning; and 3) the impact of close personal relationship quality and sleep.
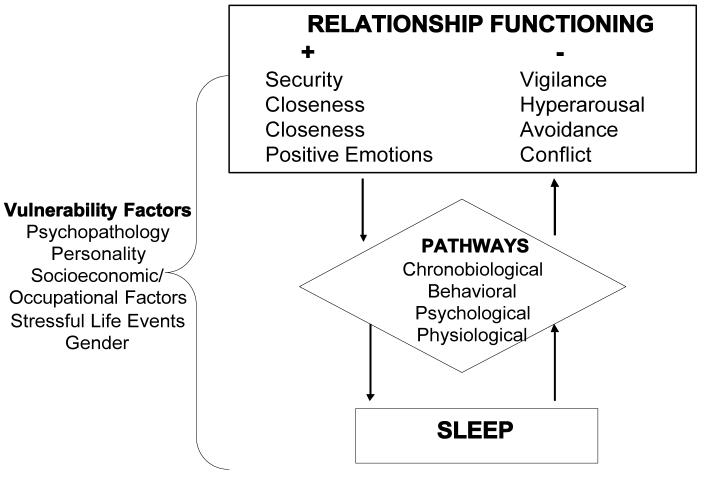
In order to provide a conceptual background to guide the literature review we present a model of biopsychosocial pathways to account for the covariation between relationship functioning and sleep, shown in Figure 1. The model depicts several direct and indirect pathways through which relationship quality may impact sleep and through which sleep disturbances may affect relationships. At the first level of the model we distinguish between “healthy” and “unhealthy” relationships. In the close relationships literature, a “healthy” relationship is typically defined by one or both partners reporting average to high ratings of relationship satisfaction or quality and/ or low levels of marital conflict, while “unhealthy” relationships are defined by low ratings of relationship satisfaction or quality and/or high levels of conflict (7). Our model suggests that, relationships that provide a sense of security and belonging are hypothesized to be health-promoting by reducing physiological responses to stress and promoting sleep. In contrast, relationships that are conflict-ridden and hostile may contribute to impaired sleep by increasing vigilance and hyperarousal, disturbing mood, and contributing to health behaviors that impair sleep. An exhaustive review of each of the proposed pathways in the model is beyond the scope of this paper. Rather, we use the model as a framework for integrating the reviewed literature. After summarizing the available data, we will return to the model in greater detail and use it as a heuristic to guide future research aimed at understanding how close relationship quality and sleep dynamically and reciprocally influence each other, and in whom such links are most likely to be evident.
Fig. 1.
Model of Dynamic Association Between Relationship Functioning and Sleep
Literature Review
We conducted an extensive search of Medline and PsychInfo databases to ascertain articles for inclusion. The following keywords were used in the literature search: relationships, relationship quality, marital quality, marital functioning, marital satisfaction, marriage, bed-partner, sleep, sleep disturbance, sleep disorders, sleep apnea, insomnia. The ancestry method of reviewing reference lists from relevant manuscripts was used to identify additional articles. English-language articles were included if they had an assessment of close relationship quality and a measure of sleep, sleep disturbance, or response to treatment for a sleep disorder. Although our primary interest is in the dynamics between sleep and relationship functioning, due to the limited evidence on the effects of co-sleeping more generally, we also included studies examining the impact of co-sleeping on the bed-partner's sleep. We did not include a small number of studies examining the impact of the patient's sleep on the partner's overall quality of life, as the primary outcome variables of interest were sleep and close relationship functioning. Case reports and dissertation studies were also excluded. Given the limited existing data, both cross-sectional and longitudinal studies were included. The review is divided into three sections of studies that examine: 1) the impact of co-sleeping on bed partner's sleep; 2) the impact of sleep disturbance on relationship functioning and 3) the impact of relationship functioning on sleep.
Section 1: Review of Studies Examining the Impact of Co-sleeping on Bed-Partner's Sleep
Given the dyadic nature of sleep for most adults, it is notable that our review uncovered only five studies that investigated how sleeping arrangement (i.e., with or without the bed partner) affects objective sleep parameters. Notably, all of these studies showed significant effects of co-sleeping arrangement on either polysomnographically- or actigraphically- assessed sleep measures (18-22). For example, in a study of fourteen married couples who slept in a sleep laboratory for three consecutive nights, Monroe (1969) found that on nights when participants slept alone, they showed a significant increase in Stage 4 and a concomitant decrease in REM sleep compared to nights when they slept with their partner. Despite the apparent objective costs to sleep architecture when sleeping with the partner, participants reported being less satisfied with their sleep on nights spent without their spouse. Consistent with Monroe's (1969) findings, Pankhurst and Horne (22) found that couples generally reported better sleep quality when they slept with the partner despite the objective evidence (using actigraphy) showing more movements when participants slept with their partner. Women preferred co-sleeping because they reported feeling more “secure” with the partner present, whereas men preferred co-sleeping out of habit.
To our knowledge, only one study has investigated the sleep effects of co-sleeping with a partner who has OSA (18). In this study, ten patients with suspected OSA and their spouses underwent simultaneous PSG studies for one night. Midway through the sleep study, patients received CPAP with the pressure adjusted to eliminate snoring and obstructive breathing events. As expected, during the CPAP trial, patients' apnea-hypopnea indices (AHI) significantly decreased. In addition, spouses showed a significant decrease in arousals and a significant increase in sleep efficiency during the treatment trial.
Section 2: Review of Studies Examining the Impact of Sleep Disturbance and Sleep Disorders on Couple's Relationship Functioning
The majority of studies (12 out of 21) included in this review investigated the influence of sleep disturbance or a sleep disorder on relationship functioning. More specifically, ten out of these twelve studies concerned the impact of OSA or sleep-disordered breathing (SDB) on relationship quality as reported by the patient and/or the bed partner (23-32). Of the ten studies concerning the dyadic impact of OSA or SDB, seven were cross-sectional (23-26, 30-32) and three were prospective (27-29). Four out of seven cross-sectional studies showed adverse associations between OSA and marital satisfaction (23, 25, 31, 32). In contrast, Scott (2003) reported no differences between snorers and controls on marital satisfaction. Billman and Ware (2002) similarly found that wives of severe and mild apneic men were comparable to primary care patient controls (without SDB) on marital satisfaction, but wives of apneics were less satisfied with their husbands' sleeping behaviors and more likely to sleep apart from their husbands. Izci and colleagues (2005) also reported no improvements in marital satisfaction following implementation of mandibular repositioning splints (MRSs) in the treatment of patients with non-apneic snoring to severe OSA; however, frequency of sleeping with the partner and “cuddling” increased with MRS usage. Thus, although some cross-sectional studies report null effects of OSA on marital satisfaction, cumulatively, the increased frequency in intimate behaviors following treatment for snoring may have a positive impact on relationship functioning over time.
Findings from longitudinal studies of the impact of OSA and its treatment on marital functioning are limited and equivocal. For instance, McArdle and colleagues (2001) conducted a cros sover trial in which 22 OSA patients and their partners reported marital satisfaction using the ENRICH questionnaire (33) before and after one-month of CPAP treatment or placebo capsule. In addition, partners' sleep was monitored using in-home PSG following the treatment phase. There were no differences in PSG-assessed sleep quality or self -reported marital quality between partners in the CPAP-limb versus those in the placebo-limb of the trial. Several caveats temper these null findings, including limited power to detect significant differences between the treatment limbs and the relatively short follow-up period, particularly given the use a global measure of marital satisfaction, which is unlikely to show substantial fluctuations in one month.
In another prospective study, McFadyen and group (2001) assigned 44 patients to CPAP and 25 patients to “conservative” treatment (i.e., advic e on sleeping posture, weight loss, and avoidance of evening alcohol consumption). Prior to treatment and 3-months following CPAP or conservative treatment, patients and their partners completed the ENRICH marital satisfaction questionnaire and an in-house measure of frequency of bed-sharing, cuddling, and number of disagreements/ arguments in the past week. CPAP therapy improved marital satisfaction, for both patients and partners. Both patients and partners in the CPAP group reported a decrease in disagreements per week, whereas patients and partners in the conservative treatment group reported an increase in disagreements. Baseline marital satisfaction scores were not related to adherence to CPAP in this sample.
Finally, Prasad and colleagues (2003) examined partners' satisfaction following laser-assisted uvulopalatoplasty (LAUP; n = 50) or uvulopalatopharyngoplasty (UVPP; n = 41). After UVPP, significantly more partners reported improvement in “quality of marital life,” sleep quality, and overall quality of life, as compared to partners of patients who underwent LAUP. Findings from this study are tempered by the very limited statistics, the unclear operationalization of “quality of marital life,” and the lack of a control group.
Aside from the influence of OSA on marital functioning, surprisingly few studies have investigated the association between other sleep disorders or sleep disturbances and marital quality. A notable exception is a large population-based study of 405 couples derived from the Alameda County Study which examined the association between the participant's own and their spouse's sleep problems and marital happiness (34). The results showed that spouses' sleep problems were associated with higher levels of marital unhappiness, even after controlling for one's own sleep problems. An important caveat to this study, however, is that a single -item measure of marital happiness was used to assess the multi-dimensional construct of marital quality.
As indicated by our model, couples dealing with other types of illness in the family are also a particularly important population to consider in the context of sleep and marital quality, given their vulnerability to both sleep problems and relationship distress. For instance, Cottrell and Kahn (35) reported findings from 50 parents of children (ages 5 years old and younger) diagnosed with epilepsy. Parents' nighttime awakenings and poorer sleep quality (as assessed by the PSQI; (36)) were associated with lower marital satisfaction on a widely -used measure of marital satisfaction, the Dyadic Adjustment Scale (DAS; (37)).
Section 3: Review of Studies Examining the Impact of Relationship Quality on Sleep
We began this review by stating that sleep optimally occurs when one feels sufficiently secure to down-regulate vigilance and alertness—an affective experience that stems in large part from the quality of the social environment (2). Clearly, not all close relationships are equal. Subsequently, differences in close relationship quality may have significant consequences for sleep.
One of the most influential theoretical frameworks used to characterize both adult and early childhood close relationships is attachment theory. Given that three of the four studies on relationship quality and sleep focus on attachment security, we provide a brief summary of the basic premise of the theory and why it may be implicated in self-regulatory processes, such as sleep. Briefly, attachment theory posits that early interactions with primary caregivers lead to the development of “internal working models” that guide one's cognitions, behaviors, and affect within subsequent relationships. These schema also contribute to one's sense of self, self-image, and one's ability to “down-regulate” physiological and psychological arousal in the face of stressful or threatening situations (2, 38). While interest in attachment theory originated in research on infants' relationships to their parents or caregivers, more recently, researchers have utilized an attachment framework to characterize adult romantic relationships (39). There has been a burgeoning interest in attachment theory in the field of psychosomatic medicine because of the implications for the different attachment patterns (i.e., secure, anxious or preoccupied, dismissing-avoidant, and fearful- avoidant) on differential patterns of stress-responsivity and subsequent physical health risk (e.g., (40)). Specifically, secure relationships are hypothesized to be health-promoting by providing a sense of security and belonging which in turn, fosters effective coping skills and reduces physiological and psychological stress responses (38). In contrast, individuals in insecure relationships, particularly those characterized by an anxious or preoccupied attachment style, may be particularly vulnerable to stress due to their tendency towards vigilance in relationships and relative inability to derive the stress-attenuating benefits of social support.
Consistent with this perspective, three studies have investigated the association between attachment security and sleep—all of which showed significant associations between measures of attachment insecurity (particularly attachment anxiety) and various dimensions of subjective sleep quality (41-43). For instance, Carmichael and Reis (2005) showed that attachment anxiety, but not attachment avoidance, was associated with poorer subjective sleep quality, even after controlling for depressed affect in 78 married couples.
The fourth study investigating the influence of relationship quality on sleep investigated the association between “marital harmony” and self-reported sleep problems (44). In a sample of 927 women drawn from a national probability sample, marital harmony was prospectively linked with fewer sleep problems, even after controlling for baseline sleep problems.
Summary
The majority of studies investigating the influence of sleep disturbance (primarily OSA) on marital functioning showed significant associations between these factors. Moreover, limited evidence suggests that marital quality improves with treatment of sleep disordered breathing. In addition, a small but consistent literature suggests that measures of close relationship quality (i.e., attachment style and marital harmony) are associated with sleep quality. Several qualifications limit the overall conclusions from these studies. First, only four longitudinal studies examined the relationship between OSA and marital quality. The findings from those four studies were equivocal, which precludes definitive conclusions regarding a causal relationship or the directionality of associations between sleep disturbance and relationship quality. Second, the measurement of relationship functioning was highly variable across studies, ranging from unvalidated, single-item assessments to validated, global measures of marital satisfaction.
Notably, most studies concerned the effects of sleep apnea or snoring on relationship functioning. It seems plausible that relationship functioning would also suffer as a result of numerous other sleep disorders, including narcolepsy or insomnia. However, to our knowledge, most research concerning other sleep disorders beyond SDB and psychosocial functioning has not included a specific measure of close relationship functioning, or did not specifically address the association between sleep disturbance per se and relationship functioning.
Conceptualizing sleep disorders from a dyadic perspective is likely to benefit both the patient and the partner, by validating both partners' needs and concerns and providing an even greater incentive to initiate and maintain treatment recommendations. Moreover, the evidence documenting significant effects of co-sleeping arrangements on objective and subjective sleep parameters underscores the importance of considering the patient's usual sleeping arrangements when interpreting data from laboratory sleep studies (in which the patient typically sleep alone).
Finally, as we stated in the introduction and as depicted in our model, the association between sleep and relationship quality is likely to be bi-directional. However, most previous studies hypothesized a uni-directional relationship between sleep disorders and marital dissatisfaction rather than the reverse direction. Evidence for the theoretically plausible pathways in Figure 1 may clarify the complex interplay between relationship quality and sleep. Thus, we now return to our model which provides a conceptual framework for understanding how close relationship functioning and sleep dynamically influence each other (pathways) and in whom such links are likely to be most evident (vulnerability factors).
Revisiting the conceptual model
Our model suggests that positive and negative aspects of relationship functioning are linked with sleep via their influence psychological, behavioral, chronobiological, and physiological mechanisms. In a high functioning relationship, a partner is likely to be a powerful stress-buffer, down-regulating physiological and psychological stress responses, promoting salutary health behaviors, and deterring against health behaviors that could have a negative impact on sleep. In contrast, distressed relationships are a primary source of stress, leading to heightened physiological and emotional arousal, poor health behaviors, and ultimately greater risk for sleep disturbance and sleep disorders. Consistent with the reviewed literature, our model further identifies pathways through which the reciprocal association (i.e., sleep affecting relationship quality) also may occur. Sleep disturbance due to a sleep disorder or temporary perturbations may have adverse effects on marital functioning by influencing emotion regulation and heightening risk for certain psychiatric illnesses, influencing health risk behaviors, and altering physiological responses.
Psychological
People who are in high quality marriages are generally happier and healthier people, as compared to their unmarried or unhappily married counterparts (16), likely due to a number of reasons that are ostensibly linked with sleep. For instance, as the primary social relationship for most adults, marriage protects against social isolation, which by itself is related to sleep disturbance (45). Feelings of safety and security in the relationship may lead to decreased loneliness or negative emotions and increases in positive emotions, which may lead to better sleep quality. The ritual of going to bed with a trusted and secure partner provides many couples with the opportunity to unwind and digest the stresses of the day prior to falling asleep. Having a supportive confidant may reduce intrusive thoughts that disturb sleep (46). In contrast, marital distress is a cause and consequence of psychological distress and psychiatric conditions, such as depression and anxiety (47), which are risk factors for sleep disturbance. Conversely, sleep deprivation affects emotion regulation, frustration tolerance, and cognitive functioning, which could, in turn, lead to more negative marital interactions (3, 4).
Behavioral/ Chronobiological
Spouses are a powerful source of social control on healthy behaviors, such as maintaining healthy sleep habits, engaging in physical activity, or adhering to sleep treatments (e.g, CPAP, (10). In contrast, in distressed relationships, spouses may engage in unhealthy behaviors, such as alcohol or substance use, which are known to impair sleep. Beyond health behaviors, limited evidence suggests that the patterning of social rhythms between bed partners may link marital quality with sleep by influencing the timing and frequency of positive and negative relational behaviors as well as sleep timing (48, 49). Although exposure to light is the most influential “zeitgeber” that entrains human sleep-wake cycles, other non-photic (or social) zeitgebers also exist, including meal time, and pre-bedtime routines (which typically occur with the bed partner; e.g., (50). Disruption of social rhythms would likely affect sleep by disrupting the regularity of exposure to the more primary zeitgebers, including light, and potentially meals and exercise. For example, members of a couple experiencing high levels of conflict may purposely change their sleep or wake times across the week in order to avoid their partner (49). In contrast, healthy relationship functioning may contribute to greater consistency in daily sleep and wake routines in both members of the dyad. Indeed, although there appear to be objective costs to co-sleeping, the ritual of sleeping together may be a powerful motivating factor that encourages couples to follow relatively consistent bedtime routines.
Physiological
Finally, the interplay between relationship functioning and sleep may be influenced via their effects on several physiological pathways, including the hypothalamic-adrenal-pituitary axis (HPA), autonomic nervous system, inflammatory processes, and more speculatively, through oxytocin-mediated pathways. Several studies have suggested an association between chronic physiological activation and insomnia (51-53). Although we recognize that other systems are also likely to be involved, we limit our discussion to these particular physiological mechanisms that have demonstrated associations with either close relationship quality or to sleep.
HPA
Poor marital functioning contributes to dysregulation of the HPA axis. Wives reporting low relationship quality show flatter diurnal slopes compared to wives reporting high relationship quality (54, 55). HPA dysregulation has also been implicated in the pathophysiology of insomnia (52, 53). Elevated levels of corticotropin-releasing hormone (CRH), the first product in the HPA axis cascade, acts in concert with the brainstem and hypothalamic arousal systems to promote wakefulness, and is associated with decreased SWS and increased wakefulness (56). With this in mind, poor relationship quality may lead to chronic CRH production that contributes to subsequent sleep disturbance. The reciprocal pathway is also plausible; i.e., elevations in HPA activity as a result of sleep disruption may subsequently contribute to decreased relationship quality. In their review of the literature on the HPA axis and sleep, Vgontzas and Chrousos (2002) concluded that sleep has an inhibitory influence on the HPA axis, whereas insomnia has been associated with arousal and increased HPA-axis activity. Shaver et al. (57) reported that midlife women with insomnia scored higher on psychological distress than women without insomnia and women with psychophysiologic type insomnia also had higher levels of urinary cortisol in an early morning sample. These findings are consistent with the hypothesis that cognitive or emotional arousal and the concomitant neuroendocrine activation may underlie chronic insomnia. In turn, such cognitive-affective disturbances and HPA elevations may contribute to relationship dysfunction. Consistent with this hypothesis, elevated ACTH during a conflict discussion in the first year of marriage was related to decreased marital satisfaction 10 years later, and elevated norepinpehrine was related to divorce (58).
Autonomic nervous system
In addition to HPA axis dysregulation, relationship quality may be related to shifts in sympathovagal balance via increased sympathetic or decreased parasympathetic nervous system activation. As reviewed by Kiecolt-Glaser and Newton (2001) hostile behavior during couple discussions is related to elevated blood pressure and plasma catecholamine levels. In unhappy relationships, sympathetic activation may persist into the evening hours, due to increased conflict, hypervigilance, or avoidance, with the potential to disrupt sleep. While no studies directly address this concept, several studies show that shifts in the sympathovagal balance towards sympathetic dominance during sleep may contribute to decreased sleep maintenance and disturbances in sleep architecture in healthy individuals (59) and patients with chronic insomnia (46, 60).
Inflammation
Psychological stress in unhappy relationships may contribute to elevated proinflammatory cytokines. Married couples who demonstrated high levels of hostile behavior during two discussions with their spouse showed larger increases in IL-6, and elevated levels of TNF-α over the 24 hours after a problem-solving discussion compared to couples with low levels of hostile behavior (61). Several proinflammatory cytokines, including IL-6, are considered “sleep modulatory” cytokines (for a review see (62)). IL-1β and TNF-α increase NREM sleep (63), and elevated IL-6 may also be related to daytime fatigue and sleepiness in humans (64). Though there is no direct evidence investigating elevations in proinflammatory cytokines as a mediator of the association between marital functioning and sleep, the available evidence suggests that this may be an important pathway.
Conversely, elevations in proinflammatory cytokines observed after sleep disturbance may contribute to emotional and cognitive disturbances, which in turn, may influence relationship functioning. For instance, decreases in positive mood following inoculation with attenuated bacterial products or active viruses (rhinovirus or influenza) were significantly correlated with elevations in proinflammatory cytokines (65), suggesting a direct relationship between cytokine elevations and mood changes. Similarly, Vgontzas et al. (66) concluded that a good night's sleep is associated with a better sense of well-being and lower circulating levels of IL-6 during the daytime, whereas sleep deprivation is associated with daytime fatigue and increased daytime exposure of tissues to the potentially detrimental effects of IL-6. Such mood or cognitive disturbances related to elevations in proinflammatory cytokines may render couples at higher risk for conflict or may contribute to poor emotion regulation during such conflicts.
Oxytocin
Although speculative at this point due to the lack of human data, some researchers have argued that the neuropeptide oxytocin (OT) may provide the neural substrate linking social relationships with health outcomes (67). OT could plausibly be relevant for sleep as well. OT is produced in the paraventricular nucleus, with neuronal projections throughout many areas of the brain. OT has widespread central nervous system effects and is present in both males and females; however, it is most often associated with its role in promoting maternal (i.e., stimulating contractions during childbirth, lactation) and pair-bonding and sexual behaviors (68). More recent evidence shows that OT has attenuating effects on human cardiovascular stress responses (69) and has anxiolytic effects in rats and humans (70). Taken together, these findings provide suggestive evidence that couples' emotional closeness and physical intimacy during the daytime and prior to bedtime may promote sleep; however, further evidence in humans is needed to confirm such speculations.
Vulnerability Factors
The coupling between relationship quality and sleep may be moderated by several key vulnerability factors, including: personality traits (e.g., hostility), preexisting psychiatric conditions (e.g., depression, anxiety, substance abuse), socioeconomic and occupational factors, life events, and gender. For instance, Brissette and Cohen (2002) found that daily diary reports of interpersonal conflict and negative affect were associated with greater sleep disturbance, particularly amongst individuals characterized by cynical hostility (71). Similarly, links between relationship quality and sleep may be especially pronounced in individuals with pre-existing psychopathology, such as depression, anxiety, or substance abuse, given their heightened risk for affective dysregulation, poorer coping skills, and interpersonal skills deficits (72). For instance, depressed individuals are more vulnerable to sleep disturbance following stressful life events (73). Thus, sleep disturbance may exacerbate symptoms of pre-existing psychopathology, with negative effects on relationships, or psychopathology may contribute to relationship disruption, leading to increases in sleep disturbance.
Socioeconomic status (SES) and occupational factors are also important moderating factors in the context of relationships and sleep. In particular, low SES may exacerbate both relationship and sleep problems, by increasing exposure to psychosocial and environmental stressors (e.g., noise, overcrowding, difficult work conditions) and limiting access to social and material resources (72),. For instance, socioeconomically disadvantaged couples who experience stressful life events, such as the transition to parenthood, and the concomitant sleep disruptions, may be more vulnerable to decrements in marital quality over time, because they lack material and perhaps, social resources to cope with the increased demands and decreased sleep resulting from the birth of the child. Moreover, socioeconomic resources influence couples' options for coping with a sleep disorder or differing sleep patterns, which may further impact the relationship functioning. For instance, couples who have sufficient economic resources to buy a bed with two separate units or who have the option to sleep in a separate bedroom may have greater flexibility and options for coping with sleep disorders which may reduce the degree to which sleep problems influence marital functioning.
Shift work is an important occupational factor that can have negative consequences for both sleep and relationships (74, 75). For instance, for couples in which one or both members of the dyad engage in shift-work, the association between sleep and relationship quality may be particularly strong because of shift-workers heightened risk for sleep deprivation and dysregulated social rhythms which may limit opportunities to engage in pleasurable activities with the spouse.
Stressful life events, including illness in one of the spousal members or another family member, or normal life course transitions, such as the transition to parenthood, are periods marked by significant sleep disturbance (76) as well as significant fluctuations in the quality of the marital relationship (12). Consistent with diathesis-stress models of stress and coping, Karney and Bradbury (77) argue that the negative effects of stressful life events on both individual and couple functioning are likely to be exacerbated in already distressed marriages, because of the chronic psychological burden of living in unhappy marriage, as well as the concomitant depletion of interpersonal resources to effectively manage the external threat. In a study of the effects of stressful life events on sleep, Morin (78) found that insomniacs perceived their lives as more stressful than good sleeper controls despite having comparable numbers of stressful life events to controls. These findings highlight the importance of the stress appraisal process in connections between stressful life events and sleep. Given that the stress appraisal process is largely determined by the individual's perceived availability of coping resources and given that a supportive spouse can be a powerful stress-buffer, these findings suggest that positive marital functioning may lead to lesser risk for sleep disturbance in part, by mitigating the effects of stressful life events on sleep.
Finally, the magnitude of the association between relationship quality and sleep may differ for men and women. The marital quality and health literature suggests that women are more sensitive to both the positive and negative aspects of the marriage (16). In addition, qualitative data from interview studies suggests that women may be more susceptible to sleep disturbances due to their multiple social roles and responsibilities and relatively greater emotional investment in the health and well-being of their families (79). Gender is also important to consider given gender differences in the prevalence rates of various sleep and psychiatric disorders and the subsequent differential rates of women versus men who experience the “collateral damage” of being the bed partner of a sleep-disordered patient (80). For instance, given the greater prevalence of OSA in men (81), women are more likely to experience the collateral effects of their partner's sleep disorder. On the other hand, it remains to be seen, whether the collateral effects of the partner's sleep disorder are similar for husbands when considering sleep disorders such as insomnia, which show a higher prevalence in women.
Summary
Studies linking relationship functioning and sleep to putative psychological, behavioral, and physiological pathways suggest that relationship quality and sleep may be causally related, but the lack of direct evidence to comprehensively test the pathways proposed in the model, precludes definitive conclusions regarding causality. Healthy relationships may promote healthy sleep, by providing a sense of safety and security, down-regulating vigilance, reducing risk for psychiatric disorders, promoting healthy sleep-related behaviors, reducing physiological responses that disturb sleep, and contributing to physiological responses that promote sleep. In contrast, unhealthy relationships may lead to greater sleep disturbances by increasing vigilance, heightening risk for psychiatric disorders, promoting unhealthy sleep-related behaviors, and augmenting physiological responses that disturb sleep. Our model also proposes a reverse relationship, wherein disturbed sleep due to sleep disorders or prolonged sleep disturbance contributes to unhealthy relationship functioning by impairing emotion regulation and cognitive function and influencing physiological mechanisms. However, given that no studies to date have directly examined any of the proposed pathways as mediators of the relationship quality and sleep connection, these hypothesized pathways await future investigation. Finally, our model suggests several vulnerability factors that may moderate the degree to which relationship quality influences sleep and vice versa. Inconsistencies in the reviewed literature may be attributable, at least in part, to the failure to account for the influence of moderating factors, such as personality, psychopathology, socioeconomic and occupational factors, stressful life events, and gender.
Conclusions
Studying sleep as a dyadic, rather than an individual phenomenon, is clearly in its infancy. This review provides a context for integrating disparate literatures to inform our understanding of how close relationship quality and sleep may be dynamically related. Notwithstanding the methodological limitations of the existing studies, the consistency of the reviewed direct evidence and suggestive evidence from the proposed mediating pathways provides conditional support for the hypothesis that relationship quality is importantly implicated with sleep and vice versa. Recognizing the social context of sleep and incorporating such knowledge into both clinical practice and research in sleep medicine may elucidate key mechanisms in the etiology and maintenance of both sleep disorders and relationship problems and may ultimately inform novel treatments.
Practice Points.
Asking about relationship quality in the diagnosis of sleep disorders may yield important information regarding the etiology or maintenance of the disorder, and may serve as an important motivating factor to initiate and/ or adhere to treatment.
Sleeping apart is not necessarily an indicator of an unhappy or unhealthy relationship. Encouraging patients to discuss difficulties with co-sleeping arrangements with their partner may lead to better sleep and a happier relationship.
If relationship problems are suspected to be a significant factor in the etiology or maintenance of a sleep disorder, referring a patient to couples' counseling may be an important adjunct to treatment.
Sleep hygiene recommendations should take into consideration the dyadic nature of sleep for most adults and should help the patient address potential conflicts (e.g., a comfortable sleep environment for one spouse may be an uncomfortable sleep environment for the other spouse).
Research Agenda.
To avoid systematic bias, laboratory sleep studies should collect information on research participants' habitual sleeping arrangements as a covariate for subsequent analyses.
Home-based PSG studies may shed light on the impact of relationship functioning on sleep continuity and architecture in the couple's natural environment
Behaviorally-oriented assessments of marital functioning, such as daily diaries of marital interactions or shared pleasurable activities with the spouse, may reflect more detailed changes in marital quality over relatively brief assessment periods.
Longitudinal studies that concurrently assess the sleep of both partners as well as their daily marital interactions may elucidate the directionality of the relationship.
Studies employing actigraphy and daily recordings of marital interactions and sleep quality over several nights, would be a relatively low-cost and efficient method of examining the covariation between sleep and relationship functioning.
Statistical analyses for clustered data and intra-individual change (e.g., latent growth curve analysis, mixed models for longitudinal data), will facilitate future investigations of the dynamic relationship between sleep and marital functioning, as well as the potential pathways and vulnerability factors.
Table 1.
Studies examining the effect of co-sleeping arrangement on objective sleep.
| Study/ Design | Sample | Methods | Results | Limitations |
|---|---|---|---|---|
| Beninati et al., 1999 Prospective, 1- night sleep study |
10 OSA a patients and their bed partners |
|
|
|
| Edinger et al., 2001 Prospective, longitudinal, matched-group design |
35 middle-aged “normal” sleepers and 33 age- matched primary insomniacs |
|
|
|
| Meadows et al., 2005 |
22 couples (ages 20-59 years) |
|
|
|
| Monroe, 1969 Prospective, 1- night sleep study |
28 married (i.e., 14 couples) good sleepers |
|
|
|
| Pankhurst & Horne, 1994 Prospective, longitudinal |
Study 1: 46 pairs of bed partners, ages 23-67 years Study 2: 39 sex and age- matched subjects who slept alone were compared to subjects from Study 1 with a bed partner |
|
|
|
Note.
Obstructive sleep apnea
Continuous positive airway pressure
Apnea-Hypopnea Index
Polysomnography
Table 2.
Studies examining the effect of sleep disorders or sleep disturbance on relationship quality.
| Study/ Design | Sample | Methods | Primary Findings | Limitations |
|---|---|---|---|---|
| Armstrong et al., 1999 Case-control |
27 untreated snoring patients and their partners; 24 patients who had undergone LAUP j and their partners |
|
|
|
| Billman & Ware, 2002 Sleep Medicine, 3 Cross-sectional |
26 wives of men with severe OSA a, 19 wives of men with mild OSA, and 19 controls |
|
|
|
| Cartwright & Knight, 1987 |
Wives of 10 male OSA patients |
|
|
|
| Cottrell & Khan, 2005 Cross-sectional Izci et al., 2005 Retrospective, questionnaire follow- up study (median 7 month follow-up) |
50 parents of children (= 5 years old) with epilepsy 144 patients referred for intra-oral MRS c devices due to snoring or OSA |
|
|
|
| Kiely & McNicholas, 1997 Cross-sectional |
71 OSA patients prescribed CPAP d and 55 bed partners |
|
|
|
| McArdle et al., 2000 Longitudinal/ crossover |
49 patients with OSA and 46 partners |
|
|
|
| McFadyen et al., 2001 Controlled, prospective trial of CPAP with 3-month follow-up |
44 CPAP patient/ partner couples and 25 patient/ partner couples from a control group |
|
|
|
| Prasad et al., 2003 Longitudinal treatment study |
33 LAUP i patients and 27 UVPP j patients |
|
|
|
| Scott et al., 2002 Cross-sectional |
56 snorers and 63 matched controls |
|
|
|
| Strawbridge et al., 2004 Cross-sectional |
Subset of 405 couples, aged 51-94, from the Alameda County Study |
|
|
|
| Virkkula et al., 2005 Cross-sectional |
37 SDB patients and their partners |
|
|
|
Note.
Obstructive sleep apnea
Dyadic Adjustment Scale
Mandibular repositioning splints
Continuous positive airway pressure
Quality of life
Morningness-Eveningness Questionnaire
Polysomnography
Evaluation and nurturing relationship issues, communication and happiness scale
Laser-assisted uvulopalatoplasty
Uvulopalatopharyngoplasty
Table 3.
Studies examining the effect of relationship quality on sleep.
| Study/ Design | Sample | Methods | Primary Findings | Limitations |
|---|---|---|---|---|
| Carmichael & Reis, 2005 Cross-sectional |
78 married adults |
|
|
|
| McNamara et al., 2001 Cross-sectional |
Study 1: 300 college students Study 2: 76 elderly volunteers |
|
|
|
| Prigerson et al., 1999 Longitudinal, community-based study |
927 married women |
|
|
|
| Scharfe & Eldredge, 2001 |
203 college students |
|
|
|
Note.
Pittsburgh Sleep Quality IndexNote.
Obstructive sleep apnea
Continuous positive airway pressure
Polysomnography
Acknowledgements
This research was supported by the following grants: T32 MH016804, MH 24652, AG20677, HL076852 and RR024153.
Nomenclature
- ACTH
adrenocorticotropic hormone
- AHI
apnea-hypopnea index
- CPAP
continuous positive airway pressure
- CRH
corticotrophin-releasing hormone
- DAS
Dyadic Adjustment Scale
- HPA
hypothalamic-pituitary-adrenal axis
- LAUP
laser-assisted uvulopalatoplasty
- NREM
non-rapid eye movement
- OSA
obstructive sleep apnea
- OT
oxytocin
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- QOL
quality of life
- REM
rapid eye movement
- SDB
sleep-disordered breathing
- UVPP
uvulopalatopharyngoplasty
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Meadows R. The ‘negotiated night’: an embodied conceptual framework for the sociological study of sleep. The Sociological Review. 2005 [Google Scholar]
- 2.Dahl RE, El-Sheikh M. Considering Sleep in a Family Context: Introduction to the Special Issue. Journal of Family Psychology. 2007;21(1):1–3. doi: 10.1037/0893-3200.21.1.1. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin DC, Jr., Daugherty SR. Sleep deprivation and fatigue in residency training: Results of a national survey of first- and second-year residents. Sleep. 2004;27:217–223. doi: 10.1093/sleep/27.2.217. [DOI] [PubMed] [Google Scholar]
- 4.Kahn-Greene ET, Lipizzi EL, Conrad AK, Kamimori GH, Killgore WDS. Sleep deprivation adversely affects interpersonal responses to frustration. Personality and Individual Differences. 2006;41:1433–1443. [Google Scholar]
- 5.Hale L. Who has time to sleep? Journal of Public Health. 2005;27(2):205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 6.Cartwright RD, Wood E. Adjustment disorders of sleep: the sleep effects of a major stressful event and its resolution. Psychiatry Research. 1991;39(3):199–209. doi: 10.1016/0165-1781(91)90088-7. [DOI] [PubMed] [Google Scholar]
- 7.Snyder DK, Heyman RE, Haynes SN. Evidence-based approaches to assessing couple distress. Psychological Assessment. 2005;17(3):288–307. doi: 10.1037/1040-3590.17.3.288. [DOI] [PubMed] [Google Scholar]
- *8.Rosenblatt PC. Two in a bed: The social system of couple bed-sharing. University of New York Press; Albany, NY: 2006. [Google Scholar]
- 9.Ulfberg J, Carter N, Talback M, Edling C. Adverse health effects among women living with heavy snorers. Health Care for Women International. 2000;21:81–90. doi: 10.1080/073993300245311. [DOI] [PubMed] [Google Scholar]
- 10.Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Israel Medical Association Journal: Imaj. 2005;7(1):13–8. [PubMed] [Google Scholar]
- 11.Schmaling KB, Afari N. Couples coping with respiratory illness. In: Schmaling KB, Scher TG, editors. The psychology of couples and illness: Theory, research, and practice. American Psychological Association; Washington, D.C.: 2000. pp. 71–104. [Google Scholar]
- 12.Shapiro AF, Gottman JM, et al. The baby and the marriage: identifying factors that buffer against decline in marital satisfaction after the first baby arrives. Journal of Family Psychology. 2000;14(1):59–70. doi: 10.1037//0893-3200.14.1.59. [DOI] [PubMed] [Google Scholar]
- 13.Brostrom A, Stromberg A, Dahlstrom U, Fridlund B. Congestive heart failure, spouses' support and the couple's sleep situation: a critical incident technique analysis. Journal of Clinical Nursing. 2003;12(2):223–33. doi: 10.1046/j.1365-2702.2003.00692.x. [DOI] [PubMed] [Google Scholar]
- 14.Mitropoulos D, Anastasiou I, Giannopoulou C, Nikolopoulos P, Alamanis C, Zervas A, Dimopoulos C. Symptomatic benign prostate hyperplasia: Impact on partners' quality of life. European Urology. 2002;41:240–245. doi: 10.1016/s0302-2838(02)00041-6. [DOI] [PubMed] [Google Scholar]
- 15.Meijer AM, van den Wittenboer GL. Contribution of Infants' Sleep and Crying to Marital Relationship of First-Time Parent Couples in the 1st Year After Childbirth. Journal of Family Psychology. 2007;21(1):49–57. doi: 10.1037/0893-3200.21.1.49. [DOI] [PubMed] [Google Scholar]
- *16.Kiecolt-Glaser J,K, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 17.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- *18.Beninati W, Harris CD, Herold DL, Shepard JW. The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clinic Proceedings. 1999;74:955–958. doi: 10.4065/74.10.955. [DOI] [PubMed] [Google Scholar]
- 19.Edinger JD, Glenn DM, Bastian LA, Marsh GR, Daile D, Hope TV, et al. Sleep in the laboratory and sleep at home II: comparisons of middle -aged insomnia sufferers and normal sleepers. Sleep. 2001;24(7):761–70. doi: 10.1093/sleep/24.7.761. [DOI] [PubMed] [Google Scholar]
- 20.Meadows R, Venn S, Hislop J, Stanley N, Arber S. Investigating couples' sleep: An evaluation of actigraphic analysis techniques. Journal of Sleep Research. 2005;14(4):377–386. doi: 10.1111/j.1365-2869.2005.00485.x. [DOI] [PubMed] [Google Scholar]
- 21.Monroe LJ. Transient changes in EEG sleep patterns of married good sleepers: The effects of altering sleeping arrangement. Psychophysiology. 1969;6(3):330–337. doi: 10.1111/j.1469-8986.1969.tb02910.x. [DOI] [PubMed] [Google Scholar]
- 22.Pankhurst FP, Horne JA. The influence of bed partners on movement during sleep. Sleep. 1994;17(4):308–315. doi: 10.1093/sleep/17.4.308. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong MWJ, Wallace CL, Marais J. The effect of surgery upon the quality of life in snoring patients and their partners: a between-subjects case-controlled trial. Clinical Otolaryngology & Allied Sciences. 1999;24(6):510–522. doi: 10.1046/j.1365-2273.1999.00307.x. [DOI] [PubMed] [Google Scholar]
- 24.Billman SJ, Ware JC. Marital satisfaction of wives of untreated sleep apneic men. Sleep Medicine. 2002;3:55–59. doi: 10.1016/s1389-9457(01)00118-6. [DOI] [PubMed] [Google Scholar]
- 25.Cartwright RD, Knight S. Silent partners: the wives of sleep apneic patients. Sleep. 1987;10(3):244–8. doi: 10.1093/sleep/10.3.244. [DOI] [PubMed] [Google Scholar]
- 26.Izci B, McDonald JP, Coleman EL, Mackay TW, Douglas NJ, Engleman HM. Clinical audit of subjects with snoring & sleep apnoea/hypopnoea syndrome fitted with mandibular repositioning splint. Respiratory Medicine. 2005;99(3):337–46. doi: 10.1016/j.rmed.2004.07.007. [DOI] [PubMed] [Google Scholar]
- *27.McArdle N, Kingshott R, Engleman HM, Mackay TW, Douglas NJ. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56(7):513–8. doi: 10.1136/thorax.56.7.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *28.McFadyen TA, Espie CA, McArdle N, Douglas NJ, Engleman HM. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. European Respiratory Journal. 2001;18(6):996–1002. doi: 10.1183/09031936.01.00209301. [DOI] [PubMed] [Google Scholar]
- 29.Prasad KR, Premraj K, Kent SE, Reddy KT. Surgery for snoring: are partners satisfied in the long run? Clinical Otolaryngology & Allied Sciences. 2003;28(6):497–502. doi: 10.1046/j.1365-2273.2003.00765.x. [DOI] [PubMed] [Google Scholar]
- 30.Scott S, Ah-See K, Richardson H, Wilson JA. A comparison of physician and patient perception of the problems of habitual snoring. Clinical Otolaryngology & Allied Sciences. 2003;28(1):18–21. doi: 10.1046/j.1365-2273.2003.00651.x. [DOI] [PubMed] [Google Scholar]
- 31.Virkkula P, Bachour A, Hytonen M, Malmberg H, Salmi T, Maasilta P. Patient- and bed partner-reported symptoms, smoking, and nasal resistance in sleep-disordered breathing. Chest. 2005;128(4):2176–82. doi: 10.1378/chest.128.4.2176. [DOI] [PubMed] [Google Scholar]
- 32.Kiely JL, McNicholas WT. Bed partners' assessment of nasal continuous positive airway pressure therapy in obstructive sleep apnea. Chest. 1997;111(5):1261–5. doi: 10.1378/chest.111.5.1261. [DOI] [PubMed] [Google Scholar]
- 33.Fowers BJ, Olson DH. ENRICH marital satisfaction scale: a brief research and clinical tool. Journal of Family Psychology. 1993;7:176–185. [Google Scholar]
- *34.Strawbridge WJ, Shema SJ, Roberts RE. Impact of spouses' sleep problems on partners. Sleep. 2004;27(3):527–31. doi: 10.1093/sleep/27.3.527. [DOI] [PubMed] [Google Scholar]
- 35.Cottrell L, Khan A. Impact of childhood epilepsy on maternal sleep and socioemotional functioning. Clinical Pediatrics. 2005;44(7):613–6. doi: 10.1177/000992280504400709. [DOI] [PubMed] [Google Scholar]
- 36.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 37.Spanier GB, Thompson LA. A confirmatory analysis of the dyadic adjustment scale. Journal of Marriage and Family. 1982;44:731–738. [Google Scholar]
- 38.Mikulincer M, Shaver PR. Mental Representations of Attachment Security: Theoretical Foundation for a Positive Social Psychology. In: Baldwin Mark W., editor. Interpersonal cognition. Guilford Press; New York, NY, US: 2005. pp. 233–266.pp. xviii, 462 2005. [Google Scholar]
- *39.Hazan C, Shaver PR. Attachment as an organizational framework for research on close relationships. Psychological Inquiry. 1994;5(1):1–22. [Google Scholar]
- 40.Carpenter EM, Kirkpatrick LA. Attachment style and presence of a romantic partner as moderators of psychophysiological responss to a stressful laboratory situation. Personal Relationships. 1996;3:351–367. [Google Scholar]
- 41.Carmichael CL, Reis HT. Attachment, sleep quality, and depressed affect. Health Psychology. 2005;24(5):526–31. doi: 10.1037/0278-6133.24.5.526. [DOI] [PubMed] [Google Scholar]
- 42.McNamara P, Andresen J, Clark J, Zborowski M, Duffy CA. Impact of attachment styles on dream recall and dream content: a test of the attachment hypothesis of REM sleep. Journal of Sleep Research. 2001;10(2):117–27. doi: 10.1046/j.1365-2869.2001.00244.x. [DOI] [PubMed] [Google Scholar]
- 43.Scharfe E, Eldredge D. Associations between attachment representations and health behaviors in late adolescence. Journal of Health Psychology. 2001;6(3):295–307. doi: 10.1177/135910530100600303. [DOI] [PubMed] [Google Scholar]
- 44.Prigerson HG, Maciejewski PK, Rosenheck RA. The effects of marital dissolution and marital quality on health and health service use among women. Medical Care. 1999;37(9):858–73. doi: 10.1097/00005650-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13(4):384–7. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- 46.Hall M, Buysse DJ, Nowell PD, Nofzinger EA, Houck P, Reynolds CF, 3rd, et al. Symptoms of stress and depression as correlates of sleep in primary insomnia. Psychosomatic Medicine. 2000;62(2):227–30. doi: 10.1097/00006842-200003000-00014. [DOI] [PubMed] [Google Scholar]
- 47.Fincham FD, Beach SRH, Harold GT, Osborne LN. Marital satisfaction and depression: Different causal relationships for men and women? Psychological Science. 1997;8(5):351–357. [Google Scholar]
- 48.De Waterman AL, Kerkhof G. Sleep-wake patterns of partners. Perceptual & Motor Skills. 1998;86(3 Pt 2):1141–2. doi: 10.2466/pms.1998.86.3c.1141. [DOI] [PubMed] [Google Scholar]
- *49.Larson JH, Crane D, Smith CW. Morning and night couples: The effect of wake and sleep patterns on marital adjustment. Journal of Marital & Family Therapy. 1991;17(1):53–65. [Google Scholar]
- 50.Mistlberger RE, Skene DJ. Social influences on mammalian circadian rhythms: animal and human studies. Biological Reviews of the Cambridge Philosophical Society. 2004;79(3):533–56. doi: 10.1017/s1464793103006353. [DOI] [PubMed] [Google Scholar]
- 51.Bonnet MH, Arand DL. Heart rate variability in insomniacs and matched normal sleepers. Psychosomatic Medicine. 2003;60(5):610–615. doi: 10.1097/00006842-199809000-00017. [DOI] [PubMed] [Google Scholar]
- 52.Rodenbeck A, Hajak G. Neuroendocrine dysregulation in primary insomnia. Revue Neurologique. 2001;157(11 Pt 2):S57–61. [PubMed] [Google Scholar]
- 53.Vgontzas AN, Chrousos GP. Sleep, the hypothalamic-pituitary-adrenal axis, and cytokines: multiple interactions and disturbances in sleep disorders. Endocrinology & Metabolism Clinics of North America. 2002;31(1):15–36. doi: 10.1016/s0889-8529(01)00005-6. [DOI] [PubMed] [Google Scholar]
- 54.Adam EK, Gunnar MR. Relationship functioning and home and work demands predict individual differences in diurnal cortisol patterns in women. Psychoneuroendocrinology. 2001;26:189–208. doi: 10.1016/s0306-4530(00)00045-7. [DOI] [PubMed] [Google Scholar]
- 55.Saxbe D, Repetti RL, Nishina AHPip. Marital satisfaction, recovery from work, and diurnal cortisol among men and women. Health Psychology. 2007 doi: 10.1037/0278-6133.27.1.15. in press. [DOI] [PubMed] [Google Scholar]
- 56.Roth T, Roehrs T, Pies R. Insomnia: Pathophysiology and implications for treatment. Sleep Medicine Reviews. 2007;11:71–79. doi: 10.1016/j.smrv.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 57.Shaver JLF, Johnston SK, Lentz MJ, Landis CA. Stress exposure, psychological distress and physiological stress activation in midlife women with insomnia. Psychosomatic Medicine. 2002;64:793–802. doi: 10.1097/01.psy.0000024235.11538.9a. [DOI] [PubMed] [Google Scholar]
- *58.Kiecolt-Glaser JK, Bane C, Glaser R, Malarkey WB. Love, marriage, and divorce: Newlyweds' stress hormones foreshadow relationship changes. Journal of Consulting and Clinical Psychology. 2003;71:176–188. doi: 10.1037//0022-006x.71.1.176. [DOI] [PubMed] [Google Scholar]
- 59.Hall M, Vasko R, Buysse D, Ombao H, Chen Q, Cashmere JD, et al. Acute stress affects heart rate variability during sleep.[see comment] Psychosomatic Medicine. 2004;66(1):56–62. doi: 10.1097/01.psy.0000106884.58744.09. [DOI] [PubMed] [Google Scholar]
- 60.Bonnet MH, Arand DL. Situational insomnia: consistency predictors, and outcomes. Sleep. 2003;15(2):1029–36. doi: 10.1093/sleep/26.8.1029. [DOI] [PubMed] [Google Scholar]
- 61.Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, et al. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry. 2005;62(12):1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- 62.Opp MR. Cytokines and sleep. Sleep Medicine Review. 2005;9:355–64. doi: 10.1016/j.smrv.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 63.Krueger JM, Obal FJ, Fang J, Kubota T, Taishi P. The role of cytokines in physiological sleep regulation. Annals of New York Academy of Sciences. 2001;933:211–21. doi: 10.1111/j.1749-6632.2001.tb05826.x. [DOI] [PubMed] [Google Scholar]
- 64.Vgontzas AN, Bixler EO, Papanicolaou DA, Kales A, Stratakis CA, Vela -Bueno A, et al. Rapid eye movement sleep correlates with the overall activities of the hypothalamic-pituitary-adrenal axis and sympathetic system in healthy humans. Journal of Clinical Endocrinology & Metabolism. 1997;82(10):3278–80. doi: 10.1210/jcem.82.10.4307. [DOI] [PubMed] [Google Scholar]
- 65.Janicki-Deverts D, Cohen S, Doyle WJ, Turner RB, Treanor JJ. Infection-induced proinflammatory cytokines are associated with decreases in positive affect, but not increases in negative affect. Brain Behavior and Immunity. 2007;21(3):301–7. doi: 10.1016/j.bbi.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vgontzas AN, Papanicolaou DA, Bixler EO, Lotsikas A, Zachman K, Kales A, et al. Circadian interleukin-6 secretion and quantity and depth of sleep. Journal of Clinical Endocrinology & Metabolism. 1999;84(8):2603–7. doi: 10.1210/jcem.84.8.5894. [DOI] [PubMed] [Google Scholar]
- 67.Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA. Biobehavioral responses to stress in females: Tend and befriend, not fight or flight. Psychological Review. 2000;107:411–423. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- 68.Carter S. Oxytocin and sexual behavior. Neuroscience and Biobehavioral Review. 1992;16:131–144. doi: 10.1016/s0149-7634(05)80176-9. [DOI] [PubMed] [Google Scholar]
- 69.Light KC, Smith TEJ,JM, Brownley KA, Hofmheimer JA, Amico JA. Oxytocin responsivity in mothers of infants: A preliminary study of relationships with blood pressure during laboratory stress and normal ambulatory activity. Health Psychology. 2000;19:560–7. doi: 10.1037//0278-6133.19.6.560. [DOI] [PubMed] [Google Scholar]
- 70.Uvnas-Moberg K, Ahlenius S, Hillegaart V, Alster P. High doses of oxytocin cause sedation and low doses cause an anxiolytic -like effect in male rats. Pharmacology Biochemistry and Behavior. 1994;49:101–106. doi: 10.1016/0091-3057(94)90462-6. [DOI] [PubMed] [Google Scholar]
- 71.Brissette I, Cohen S. The contribution of individual differences in hostility to the associations between daily interpersonal conflict, affect, and sleep. Personality & Social Psychology Bulletin. 2002;28(9):1265–74. [Google Scholar]
- 72.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 73.Haynes PL, McQuaid JR, Ancoli-Israel S, Martin JL. Disrupting life events and the sleep-wake cycle in depression. Psychological Medicine. 2006;36(10):1363–73. doi: 10.1017/S0033291706008208. [DOI] [PubMed] [Google Scholar]
- 74.Smith L, Folkard S. Determinants of shift-work adjustment for nursing staff: the critical experience of partners. Journal of Professional Nursing. 2004;20(3):187–95. doi: 10.1016/j.profnurs.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 75.Akerstedt T, Fredlund P, Gillberg M, Jansson B. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. Journal of Psychosomatic Research. 2002;53(1):585–8. doi: 10.1016/s0022-3999(02)00447-6. [DOI] [PubMed] [Google Scholar]
- 76.Yamazaki A, Lee KA, Kennedy HP, Weiss SJ. Sleep-wake cycles, social rhythms, and sleeping arrangement during Japanese childbearing family transition. JOGNN - Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2005;34(3):342–8. doi: 10.1177/0884217505276156. [DOI] [PubMed] [Google Scholar]
- 77.Karney BR, Bradbury TN. The longitudinal course of marital quality and stability: A review of theory, method, and research. Psychological Bulletin. 1995;118(1):3–34. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- 78.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic Medicine. 2003;65(2):259–67. doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- *79.Hislop J, Arber S. Sleepers Wake! The gendered nature of sleep disruption among midlife women. Sociology. 2003;37:695–711. [Google Scholar]
- 80.Ashtyani H, Hutter DA. Collateral damage: the effects of obstructive sleep apnea on bed partners.[comment] Chest. 2003;124(3):780–1. doi: 10.1378/chest.124.3.780. [DOI] [PubMed] [Google Scholar]
- 81.Krishnan V, Collop NA. Gender differences in sleep disorders. Current Opinion in Pulmonary Medicine. 2006;12(6):383–9. doi: 10.1097/01.mcp.0000245705.69440.6a. [DOI] [PubMed] [Google Scholar]