Summary
Aim of this study was to compare post-operative recovery over 14 days in children submitted to tonsillectomy using a bipolar radiofrequency-based plasma device (Coblation®, Evac 70, ArthroCare Corp, Sunnyvale, CA, USA) to cold dissection. Paediatric patients (n = 42) aged 5-16 years old with chronic tonsillitis underwent tonsillectomy using cold dissection with suture ligatures or a plasma device (Evac 70, ArthroCare Corp, Sunnyvale, CA, USA). Pain intensity on the first day, use of analgesics, type of diet, and days of pain, fever, nausea, and absence from school were determined. Groups were compared using time-to-event (Kaplan-Meier) curves and statistically evaluated using the Breslow (generalized Wilcoxon) test. Children undergoing plasma tonsillectomy reported significantly less pain on the first post-operative day (1.2 ± 0.9 vs. 3.5 ± 1.5, p < 0.001), fewer days of pain (4.8 ± 1.5 vs. 9.4 ± 1.2, p < 0.001), pain medication withdrawal (2.6 ± 1.3 vs. 4.5 ± 1.3, p < 0.001) and earlier use of liquid diet (5.1 ± 1.4 vs. 8.5 ± 2.1, p < 0.001), and fewer school days lost (5.3 ± 1.7 vs. 8.9 ± 1.5, p < 0.001). After completing this study, plasma tonsillectomy was adopted for the majority of cases. Benefits of the plasma device include the possibility both to excise tissue and coagulate bleeding vessels using the same device whilst improving quality of post-operative recovery over cold dissection with suture ligatures.
Keywords: Tonsillectomy, Radiofrequency, Cold dissection, Coblation
Riassunto
Lo scopo del nostro studio è stato comparare il recupero post-operatorio in 14 giorni su pazienti pediatrici sottoposti a tonsillectomia mediante tecnica a radiofrequenze (COBLATION©, Evac 70, ArthroCare Corp, Sunnyvale, CA, USA) rispetto alla tecnica per dissezione con lama fredda. Pazienti (n. 42) in età pediatrica (5-16 anni) affetti da ton-sillite cronica, divisi in 2 gruppi, sono stati sottoposti in maniera randomizzata a tonsillectomia con tecnica per dissezione con la-ma fredda e fili riassorbibili o con manipolo a radiofrequenze al plasma (Evac 70, ArthroCare Corp, Sunnyvale, CA, USA). Sono stati valutati dolore post-operatorio nella prima giornata, uso di antidolorifici, tipo di dieta, giorni di dolore, febbre, nausea e gior-ni di assenza dalla scuola. I 2 gruppi sono stati comparati con metodo statistico (Kaplan-Meier, Breslow-generalized Wilcoxon). I pazienti sottoposti a tonsillectomia con radiofrequenze hanno riportato una significativa riduzione del dolore in prima giornata post-operatoria (1,2 ± 0,9 vs. 3,5 ± 1,5, p < 0,001), delle giornate di dolore (4,8 ± 1,5 vs. 9,4 ± 1,2, p < 0,001), dell’uso di analgesici (2,6 ± 1,3 vs. 4,5 ± 1,3, p < 0,001), dei giorni di dieta liquida (5,1 ± 1,4 vs. 8,5 ± 2,1, p < 0,001) e dei giorni di scuola persi (5,3 ± 1,7 vs. 8,9 ± 1,5, p < 0,001). Dopo il completamento dello studio abbiamo adottato la tonsillectomia coblator per la maggior parte dei nostri casi di tonsillectomia. Tra i vantaggi del manipolo di radiofrequenze al plasma segnaliamo la possibilità con un unico strumento di ablare il tessuto e coagulare i vasi sanguinanti, con miglioramento della qualità del recupero post-operatorio rispetto alla tecnica classica per dissezione con lacci riassorbibili.
Introduction
Over the last few years, several different techniques for performing tonsillectomy have been proposed in the attempt to lower the morbidity of this surgery. The cold dissection procedure was the standard approach before the ‘Bovie’ electrocautery device was introduced. Electrosurgical methods offered an improved means over cold dissection for controlling intra-operative bleeding and were rapidly adopted as the procedure of choice. During subsequent years, however, several clinical studies showed that electrosurgical tonsillectomy was associated with more painful and extended post-operative recovery 1–3 as well as an increased risk of secondary bleeding compared to cold dissection 4 5. Hence, new devices and methods for performing tonsillectomy continued to be developed and studied.
When radiofrequency-based plasma devices were introduced for tonsillectomy, our hospital still used cold dissection routinely. Investigators comparing plasma devices to electrocautery reported that their use was associated with significantly less damage to tissue underlying the treatment zone 6 and potentially better quality post-operative recovery than electrocautery 7–10. The electrocautery technique was never adopted in our Unit on account, not only of the residue which remained with this procedure, but also because, with this technique, there was the risk of delaying post-operative recovery of our patients. Reports of early research on the plasma device were intriguing and were open to attempting use of a method that, compared with electrocautery, would allow the potential for improved recovery, while providing a mechanism to control intra-operative bleeding without requiring use of sutures.
Aim of the present study was to evaluate the feasibility of using the plasma device, in our clinic, for tonsillectomy. The primary aim was to assess the 14-day post-operative recovery period in paediatric patients who underwent tonsillectomy using the plasma device compared to patients who received cold dissection with suture ligatures.
Material and methods
Patients and study design
The study protocol was approved by the Ethics Committee of the S. Eugenio Hospital in Rome, Italy. The study group consisted of paediatric patients, age range 5-16 years old, who presented symptoms consistent with chronic tonsillitis. After undergoing training to use the plasma device and actually performing, 10 cases were not included in the study, thereafter, the remaining patients were assigned to undergo tonsillectomy using either the plasma device or cold dissection with suture ligatures; patients were assigned to treatment as they were scheduled for surgery, alternating between assignment to one surgical approach and then the other through our first 21 plasma cases. The two surgical groups were statistically similar as far as concerns age and sex, and were similarly distributed in terms of tonsil size and prevalence of associated respiratory conditions (Table I). None of the patients received concurrent adenoidectomy. The same surgical team performed all procedures between September and December 2004.
Table I. Patient demographics.
| Cold dissection (n = 21) | pmRF (n = 21) | p | ||||
| Age (mean ± SD) | 9.3 ± 2.9 | 9.3 ± 3.2 | 0.960 | |||
| Sex (male) | 11 (52%) | 12 (57%) | 0.757 | |||
| Tonsil grade | 0.934 | |||||
| 1 | 1 | 1 | ||||
| 2 | 7 | 9 | ||||
| 3 | 8 | 7 | ||||
| 4 | 5 | 4 | ||||
| Associated conditions | 0.747 | |||||
| Atopic dermatitis | 1 | 2 | ||||
| Allergic rhinitis | 3 | 3 | ||||
| Allergic rhinitis & asthma | 2 | 1 | ||||
| Asthma | 0 | 1 | ||||
| Rheumatic disease | 1 | 1 | ||||
| Total no. cases | 7 | 8 | ||||
Cold dissection tonsillectomy
Cold dissection tonsillectomy was performed, as was standard for our clinic. Using Allis forceps, the tonsil was retracted medially, an incision was made at the anterior pillar near the upper pole of the tonsil which was then excised using a metal snare. Haemostasis was achieved by closing the wound using “slipknot” open ligatures with resorbable suture (Fig. 1).
Fig. 1.
Treatment site immediately after tonsillectomy using cold dissection with ligatures.
Radiofrequency-based plasma tonsillectomy
Plasma tonsillectomy was performed using the Evac 70 Wand (ArthroCare Corporation, Sunnyvale, CA, USA). This device is designed for ablation and dissection of soft tissue and has integrated suction to facilitate removal of debris and variable coagulation settings to allow haemostasis. With this technique, radiofrequency energy is used to excite the electrolytes in a conductive medium, such as saline solution, creating a precisely focused plasma. The energized particles in the plasma have sufficient energy to break molecular bonds 11–13, excising or dissolving soft tissue at relatively low temperatures (typically 40 °C to 70 °C). The same device was used to excise the tonsillar tissue and to perform haemostasis when required.
Using Allis forceps, the tonsil was retracted infero-medially and an incision was made at the anterior portion of the tonsil pillar. Care was taken to keep the dissection within the peritonsillar space and avoid penetrating the tonsil capsule. Once the tonsil plane was identified, the tip of the device was swept gently over the tonsillar tissue in a superior to inferior direction to remove it. Minimal pressure was applied, since this aided dissection of tissue and decreased the likelihood of excised tissue fragments clogging the device. While completing the tonsil excision, bleeding was controlled by switching to the coagulation setting and pressing the device tip directly onto the bleeder for 2-3 seconds. After achieving haemostasis, tonsil ablation was resumed. The fossa was completely cleared of tonsillar tissue while preserving the capsular plane and pillar (Fig. 2).
Fig. 2.
Treatment site immediately after pmRF tonsillectomy.
Clinical outcome measures
After surgery, all patients and parents were given a post-operative recovery diary to complete daily for 14 days; parents were asked to complete the form at home together with their children. The symptoms and pain parameters collected during the 14-day period included use of analgesics (paracetamol), diet type (e.g. liquid, solid) the child had followed that day, absence from school, and presence of pain, fever (> 37), and nausea. The parents recorded diary questions daily using a ‘yes’ or ‘no’ response. Pain intensity on the first day was graded using a 5-cm visual analogue scale, where ‘0’ represented ‘no pain’ and ‘5’ represented ‘maximum pain’. Parents were also asked to record occurrence of any bleeding episodes during this period and to call the hospital if the episode was worrisome. During surgery, intra-operative bleeding was measured collecting blood by means of suction tube.
Statistical Analysis
Inferences about means from continuous data were based on standard parametric statistics. Comparisons based on non-ordered categorical data were evaluated using the chi-square test or Fisher’s exact test and ordered categorical data were examined using the Mann-Whitney U two-sample rank test. Surgical groups were compared using time-to-event (Kaplan-Meier) curves, which were statistically evaluated using the Breslow (generalized Wilcoxon) test. Two-tailed p < 0.05 was considered statistically significant. Statistical analyses were performed using the SPSS for Windows, version 14.0 software.
Results
Surgery time ranged from 25-30 minutes for cold dissection and 30-35 minutes for the plasma device. When performing tonsillectomy using cold dissection, the procedure required 12-15 surgical instruments and three suture packs. In contrast, with the plasma device, 3 or 4 surgical instruments were used, including the Allis and/or Blumke forceps, pillar retractor, and Kelly forceps. Intra-operative bleeding, during the plasma procedure, tended to be half (~10 ml per case) that generally experienced using cold dissection (~20-25 ml per case).
No abnormal findings were observed, post-operatively, in any of the cases and physical examination findings were similar for both treatment groups. Patients in both groups reported some minor sputum bleeding when sneezing or coughing. No patient experienced a post-operative bleeding episode requiring clinical examination or readmission.
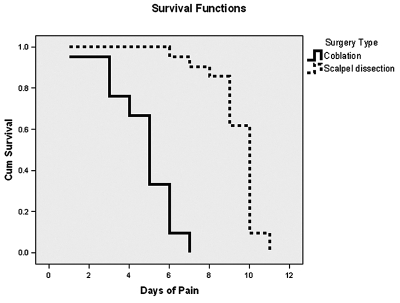
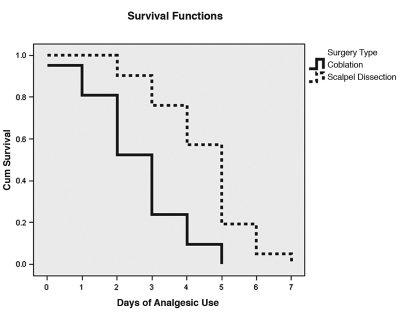
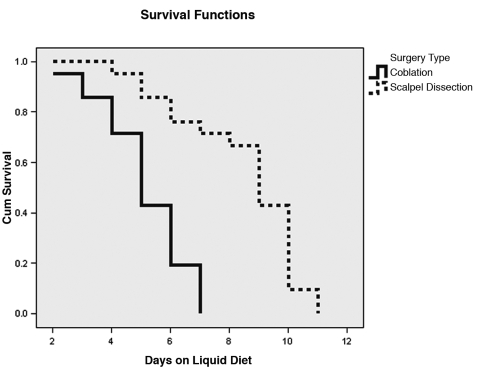
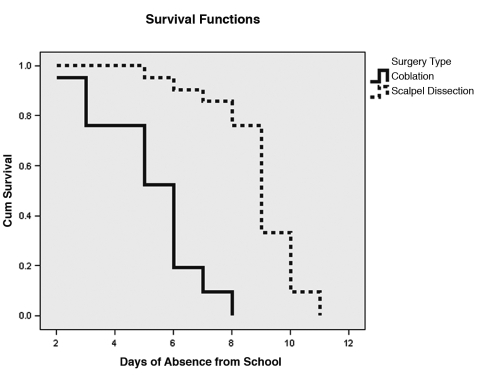
Children undergoing plasma tonsillectomy reported significantly less pain on the first post-operative day compared to children receiving cold dissection (Tables II, III); a pain score of ‘1’ or ‘0’ was reported by 14 (67%) plasma device-treated patients and by 3 (14%) cold patients submitted to dissection. The mean (± SD) number of pain days reported by children in the “plasma” group was 4.8 ± 1.5 days compared to 9.4 ± 1.2 days for children submitted to cold dissection (Fig. 3). The patients receiving plasma tonsillectomy also ceased use of analgesics sooner (Fig. 4), stopped liquid diet sooner (Fig. 5), and lost fewer school days (Fig. 6) than those submitted to cold dissection. Tonsillectomy groups did not differ significantly as far as concerns the number of days with fever or number of days with nausea.
Table II. Summary of statistics for diary data.
| Cold dissection (n = 21) | pmRF (n = 21) | p | |
| Pain score on first day | 3.5 ± 1.5A | 1.2 ± 0.9 | < 0.001 |
| VASB score for pain = | |||
| ‘0’ | 1C | 4 | |
| ‘1’ | 2 | 10 | |
| ‘2’ | 1 | 5 | |
| ‘3’ | 4 | 2 | |
| ‘4’ | 7 | 0 | |
| ‘5’ | 6 | 0 |
= mean ± standard deviation;
= visual analogue scale;
= number of patients;
Table III. Summary of statistics for diary data.
| Cold dissection (n = 21) | pmRF (n = 21) | p | |
| Days reporting pain | 9.4 ± 1.2 | 4.8 ± 1.5 | < 0.001 |
| AnalgesicD days | 4.5 ± 1.3 | 2.6 ± 1.3 | < 0.001 |
| Liquid diet days | 8.5 ± 2.1 | 5.1 ± 1.4 | < 0.001 |
| Absent school days | 8.9 ± 1.5 | 5.3 ± 1.7 | < 0.001 |
| Pain score (days with pain only) | 3.6 ± 1.4 | 2.5 ± 1.1 | 0.006 |
| Days with nausea | 0.245 | ||
| 0 | 1 | 2 | |
| 1 | 3 | 8 | |
| 2 | 10 | 4 | |
| 3 | 5 | 6 | |
| 4 | 2 | 1 | |
| Days with fever | 0.253 | ||
| 0 | 1 | 2 | |
| 1-3 | 5 | 11 | |
| 4-6 | 12 | 3 | |
| 7-9 | 3 | 5 |
= all patients were recommended to take paracetamol.
Fig. 3.
Pain resolution for the two treatment groups over the 14-day diary collection period. Median days to resolution was 5 (95% confidence interval = 4.4-5.6) days for pmRF patients and 10 (9.8-10.2) days for cold dissection patients.
Fig. 4.
Cessation of analgesic use for the two treatment groups over the 14-day diary collection period. Median days to cessation was 3 (95% confidence interval = 2.4-3.6) days for pmRF patients and 5 (4.6-5.4) days for cold dissection patients.
Fig. 5.
Days until cessation of liquid diet for the two treatment groups over the 14-day diary collection period. Median days to cessation was 5 (95% confidence interval = 4.3-5.7) days for pmRF patients and 9 (8.1-9.9) days for cold dissection patients.
Fig. 6.
Days until return to school for the two treatment groups over the 14-day diary collection period. Median days to return was 6 (95% confidence interval = 5.1-6.7) days for pmRF patients and 9 (8.5-9.5) days for cold dissection patients.
A significant linear relationship was observed between pain days and 1) use of analgesics (Pearson correlation = 0.422; p = 0.005), 2) school days lost (Pearson correlation = 0.650; p < 0.001), and 3) days on liquid diet (Pearson correlation = 0.811; p < 0.001).
Discussion
Several studies have shown the potential for significantly improved recovery with the plasma tonsillectomy compared to that following electrocautery 7–10 14 but research comparisons of plasma tonsillectomy and cold dissection are more limited in number. In a prospective, randomized, single-blind study conducted at UCLA, Shapiro et al. compared the intra-operative efficiency and post-operative recovery between cold dissection adeno-tonsillectomy (CDA) and Coblation-assisted adeno-tonsillectomy (CAA). It was shown that CAA offers better operative time and intra-operative haemostasis as compared with CDA. However, CAA does not result in lower post-operative pain scores or recoveries despite these intra-operative advantages 15. Polites et al. observed that adult patients who received Coblation tonsillectomy, on one side, and conventional cold steel tonsillectomy, on the other, reported that the Coblation side was significantly less painful on post-operative days 1, 2, and 3 than the cold dissection side 16. Zhong et al. reported a significantly earlier return to a normal diet and significantly reduced pain with the plasma tonsillectomy compared to blunt dissection 17. In contrast, Philpott et al. who evaluated post-operative pain, otalgia, swallowing and use of analgesics, at selected time points over a 14-day period, showed no significant benefits for plasma tonsillectomy with regard to cold dissection in adults 18. However, in that report, the cold dissection technique used was not clearly described, nor was the method used to control intra-operative bleeding specified. In our study, children who underwent, plasma tonsillectomy reported freedom from pain, ceased liquid-only diet, and returned to school significantly earlier than children who underwent cold dissection.
Electrocautery for haemostasis after removing the tonsils using cold dissection will undoubtedly increase recovery time compared to cold dissection with suture closing. The cold dissection technique is associated with less histological damage to surrounding tissue than electrocautery 19. This may, in part, explain why patients submitted to cold dissection generally have a less painful post-operative recovery than those who undergo electrocautery tonsillectomy 1–3. Conventional electrocautery systems ablate or coagulate tissue by applying a voltage across the tissue to be treated. This difference in voltage causes an arc to form across the physical gap between the active electrode and the target tissue. Usually, this gap is filled with an electrically insulating gas (air, or carbon dioxide in laparoscopic procedures) or an electrically non-conductive liquid (distilled water, or glycine, etc.). The temperature of this spark has been reported 20 to be > 1600 °C. In contrast, plasma devices use a lower voltage Radio Frequency signal (100-350 Volts at 100-500 kHz), which is applied through an electrically conductive medium, usually water based. In the ionized vapour layer formed around the electrode, the low temperate (40-90 °C) plasma contains radicals which are chemically very active. These radicals chemically disintegrate tissue 13. This activity is a chemical etching process with some heat dissipated as a controlled by-product allowing control of haemostasis, as opposed to conventional electrocautery, which is a purely thermally driven process.
Less pain and faster recovery were observed in the patients submitted to plasma tonsillectomy compared to those who underwent cold dissection, a possible explanation being that the surrounding tissue is less traumatized using the plasma device. During cold dissection, the tissue around the treatment site is manipulated using forceps and other instruments; in addition, suturing may be associated with localized pain. In contrast, when using the plasma device, the tonsil is excised without grasping, pulling, or tearing the adjacent tissue.
Increased risk of delayed post-operative bleeding has been reported in the literature as a significant problem when using a plasma device 21. During the present study, no secondary re-bleed cases occurred, however the relatively small sample size used does not allow us to conclude that it is not a risk. In our opinion, the plasma device may be associated with a slightly higher re-bleed rate than cold dissection but as the literature suggests, it may not be any higher than it is when using electrocautery. In cold dissection cases, we cut less and dissect more; therefore, there may be less risk of subsequent bleeding.
In our experience, plasma technology was found to be sufficient for performing intra-operative haemostasis in the majority of cases (99%). In the three cases requiring additional haemostasis, not part of the present study, suture ties were successfully used. However, we suggest that the surgeon be proficient with at least one other surgical technique, when using the plasma device (e.g. dissection and haemostasis with ligatures, stitches, or electrocautery), in order to be able to complete any procedure in which an unexpected event may occur, such as massive haemorrhage or device failure. When using this device, we found it beneficial to adopt some of the same surgical pearls we used with cold dissection, including paying particular attention to performing spot haemostasis, as necessary, while removing the tonsil, preserving the capsular plane and pillar, and avoiding leaving tonsillar tissue in situ. Proceeding in a meticulous fashion, allowed us to maintain a clean operative field and avoid carrying out extensive haemostasis at the end of the procedure. We used the plasma device to conduct haemostasis and, therefore, did not need to use either sutures or electrocautery. However, in order to achieve effective haemostasis with the plasma device, it was necessary to ensure that the entire tonsillar fossa was covered in saline solution before gently brushing the device over the bleeder.
Compared to cold dissection, the most significant disadvantages found with the plasma device were the need to go through a learning curve, although it was relatively short, and the expense of the wand. Costs of coblation tonsillectomy include a wand for each patient and, most of all, a plasma generator; but surgeons could reduce overall expenses using coblation technology also to perform reduction of turbinates, palatoplasty, adenoidectomy, tongue base reduction with the same coblator generator and by sharing it with other colleagues. In addition, this tool is substantially more costly than that used to perform cold dissection. However, we found that the total number of instruments required for performing the procedure, when using the plasma device, was substantially less than the number required for cold dissection. It may be useful to conduct a formal cost effectiveness study to evaluate the overall costs of using this device for tonsillectomy. At the end of this study, we completely switched to using the plasma device for performing tonsillectomy.
Conclusion
Since completing the present study, the plasma device has been adopted for performing tonsillectomy in the majority of cases. However, performing tonsillectomy with this procedure should not be approached by simply using the same technique as would be followed when doing any other more conventional procedure; it should be considered a completely new surgical method. After appropriate training, plasma tonsillectomy represents an innovation that provides benefits for both the surgeon and patient, including the possibility both to excise tissue and to coagulate bleeding vessels with the same device and whilst, moreover, improving the quality of post-operative recovery compared to that following the cold dissection technique.
Acknowledgements
Authors thank Debby Holmes-Higgin, MS, MPH for assistance with statistical analyses and editing of manuscript.
References
- 1.Wexler DB. Recovery after tonsillectomy: electrodissection vs. sharp dissection techniques. Otolaryngol Head Neck Surg 1996;114:576-81. [DOI] [PubMed] [Google Scholar]
- 2.MacGregor FB, Albert DM, Bhattacharyya AK. Post-operative morbidity following paediatric tonsillectomy; a comparison of bipolar diathermy dissection and blunt dissection. Int J Pediatr Otorhinolaryngol 1995;31:1-6. [DOI] [PubMed] [Google Scholar]
- 3.Nunez DA, Provan J, Crawford M. Postoperative tonsillectomy pain in pediatric patients: electrocautery (hot) vs. cold dissection and snare tonsillectomy – a randomized trial. Arch Otolaryngol Head Neck Surg 2000;126:837-41. [DOI] [PubMed] [Google Scholar]
- 4.Mowatt G, Cook JA, Fraser C, McKerrow WS, Burr JM. Systematic review of the safety of electrosurgery for tonsillectomy. Clin Otolaryngol 2006;31:95-102. [DOI] [PubMed] [Google Scholar]
- 5.Lee MS, Montague ML, Hussain SS. Post-tonsillectomy hemorrhage: cold vs. hot dissection. Otolaryngol Head Neck Surg 2004;131:833-6. [DOI] [PubMed] [Google Scholar]
- 6.Chinpairoj S, Feldman MD, Saunders JC, Thaler ER. A comparison of monopolar electrosurgery to a new multipolar electrosurgical system in a rat model. Laryngoscope 2001;111:213-7. [DOI] [PubMed] [Google Scholar]
- 7.Stoker KE, Don DM, Kang DR, Haupert MS, Magit A, Madgy DN. Pediatric total tonsillectomy using coblation electrosurgery compared to conventional electrosurgery: A prospective, controlled single-blind study. Otolaryngol Head Neck Surg 2004;130:666-75. [DOI] [PubMed] [Google Scholar]
- 8.Temple RH, Timms MS. Paediatric coblation tonsillectomy. Int J Pediatr Otorhinolaryngol 2001;61:195-8. [DOI] [PubMed] [Google Scholar]
- 9.Timms MS, Temple RH. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol 2002;116:450-2. [DOI] [PubMed] [Google Scholar]
- 10.Parsons SP, Cordes SR, Comer B. Comparison of posttonsillectomy pain using the ultrasonic scalpel, coblator, and electrocautery. Otolaryngol Head Neck Surg 2006;134:106-13. [DOI] [PubMed] [Google Scholar]
- 11.Stalder KR, Woloszko J, Brown IG, Smith CD. Repetitive plasma discharges in saline solutions. Applied Physics Letters 2001;79:4503-5. [Google Scholar]
- 12.Woloszko J, Stalder KR, Brown IG. Plasma characteristics of repetitively-pulsed electrical discharges in saline solutions used for surgical procedures. IEEE Trans Plasma Sci 2002;30:1376-83. [Google Scholar]
- 13.Stalder KR, McMillen DF, Woloszko J. Electrosurgical plasmas. J Phys Dis Appl Phys 2005;38:1728-38. [Google Scholar]
- 14.Glade RS, Pearson SE, Zalzal GH, Choi SS. Coblation adenotonsillectomy: an improvement over electrocautery technique? Otolaryngol Head Neck Surg 2006;134:852-5. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro NL, Bhattacharyya N. Cold dissection vs. coblation-assisted adenotonsillectomy in children. Laryngoscope 2007;117:406-10. [DOI] [PubMed] [Google Scholar]
- 16.Polites N, Joniau S, Wabnitz D, Fassina R, Smythe C, Varley P, et al. Postoperative pain following coblation tonsillectomy: randomized clinical trial. Aust N Z J Surg 2006;76:226-9. [DOI] [PubMed] [Google Scholar]
- 17.Zhong Z, Xiao S, Wang C, Wang H, Wang G. Coblation tonsillectomy vs. blunt dissection tonsillectomy. Lin Chuang Er Bi Yan Hou Ke Za Zhi 2006;20:391-5. [PubMed] [Google Scholar]
- 18.Philpott CM, Wild DC, Mehta D, Daniel M, Banerjee AR. A double-blinded randomized controlled trial of coblation vs. conventional dissection tonsillectomy on post-operative symptoms. Clin Otolaryngol 2005;30:143-8. [DOI] [PubMed] [Google Scholar]
- 19.Liboon J, Funkhouser W, Terris DJ. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg 1997;116:379-85. [DOI] [PubMed] [Google Scholar]
- 20.Woloszko J, Kwende MM, Stalder KR. Coblation in Otolaryngology. Proceedings of SPIE. Lawrence et al., Editors, NY 2003;4949:341-52. [Google Scholar]
- 21.Lowe D, van der Meulen J. Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet 2004;364:697-702. [DOI] [PubMed] [Google Scholar]