Summary
Early diagnosis of the affected side in Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo is important in effectively applying treatment manoeuvres. This study was performed to examine the frequency of a new clinical sign, pseudo-spontaneous nystagmus, in a large cohort of patients with Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo, comparing its efficacy in the identification of the involved side with that of other diagnostic signs, seated supine positioning nystagmus, and the intensity of the nystagmus evoked by the head yaw test in the supine position. Overall, 293 patients affected by Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo (197 geotropic and 96 apogeotropic forms) were examined. Pseudo-spontaneous nystagmus was observed in 222 patients (76%). After a very slow, repeated horizontal rotation of the head, in the seated position, this percentage increased to 96% (281 patients). The pseudo-spontaneous nystagmus and the seated supine positioning nystagmus always beat in the same direction and both were in accordance in identifying the affected side with the nystagmus evoked by the head yaw test. The differential diagnosis between spontaneous nystagmus and pseudo-spontaneous nystagmus is easily achieved with the head pitch test in the sitting position: the pseudo-spontaneous nystagmus disappears with the head bent forward 30° (neutral position), it reverses its direction with the head bent 60° forward, it returns visible bringing the head in axis with the body and increases its intensity extending the head about 30° backwards. Pseudo-spontaneous nystagmus is an important sign for determining the affected ear in Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo. Early identification of the affected side improves efficacy of treatment and compliance of patients.
Keywords: Vertigo, Otoliths, Benign Paroxysmal Positional Vertigo, Lateral Semicircular Canal, Liberatory Manoeuvre
Riassunto
La diagnosi immediata del lato affetto nella Vertigine Parossistica Posizionale Benigna del Canale Semicircolare Laterale è importante al fine di praticare in maniera corretta ed efficace il trattamento riabilitativo. Questo studio è stato condotto al fine di verificare l’incidenza di un nuovo segno clinico, il Nistagmo Pseudo-Spontaneo, in un ampio campione di pazienti affetti da Vertigine Parossistica Posizionale Benigna del Canale Semicircolare Laterale, confrontandone l’efficacia nel diagnosticare il lato affetto con quella di altri indicatori diagnostici di lato: il nistagmo evocato nel passaggio rapido da seduto a supino e l’intensità del nistagmo evocato con il test di latero-rotazione del capo a paziente supino. Sono stati esaminati 293 pazienti affetti da Vertigine Parossistica Posizionale Benigna del Canale Semicircolare Laterale, 197 forme geotrope e 96 apogeotrope. Il Nistagmo Pseudo-Spontaneo è stato osservato in 222 pazienti (76%). Tale percentuale saliva al 96% (281 pazienti) dopo aver ripetutamente ruotato il capo del paziente in posizione seduta molto lentamente. Il Nistagmo Pseudo-Spontaneo ed il Nistagmo evocato con posizionamento rapido seduto/supino, quando presenti entrambi nello stesso paziente, battevano sempre nella stessa direzione ed, inoltre, erano sempre in accordo con il terzo indicatore clinico per la diagnosi del lato affetto: l’intensità del nistagmo evocato con il test di latero-rotazione del capo a paziente supino. La diagnosi differenziale fra un Nistagmo Spontaneo (ad es. da neuronite vestibolare) ed un Nistagmo Pseudo-Spontaneo è facilmente eseguibile con il test di flesso/estensione del capo in posizione seduta: con il capo flesso in avanti di 30° il Nistagmo Pseudo-Spontaneo scompare (posizione neutrale), inverte direzione con il capo flesso di 60° in avanti, ritorna visibile riportando il capo in asse con il tronco ed incrementa di intensità estendendo il capo di circa 30° indietro: Head Pitch Test. Il Nistagmo Pseudo-Spontaneo è un importante segno diagnostico per identificare il lato interessato nella Vertigine Parossistica Posizionale Benigna del Canale Semicircolare Laterale. La diagnosi tempestiva del lato affetto ottimizza l’efficacia del trattamento, migliorandone la tollerabilità per il paziente.
Introduction
Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo (LSC-BPPV) is characterized by paroxysmal vertigo and bidirectional/bipositional horizontal nystagmus (Ny) beating to the lowermost ear in the geotropic form and to the uppermost ear in the apogeotropic one. It is provoked by turning the head 180° to either side in the supine position – Head Yaw Test (HYT), Head Yaw Nystagmus (HYN) 1 2.
In the geotropic forms 1 2, after performing the HYT towards the impaired side, the otoliths settle along the canal, towards the ampulla, due to gravity, generating an excitatory, ampullopetal, endolymphatic current, and the consequent geotropic Ny beating to the impaired ear. If the patient’s head is turned on the healthy side, the otoliths float towards the utricular orifice generating an inhibitory, ampullofugal, endolymphatic current. Consequently, the Ny will once again be geotropic and, therefore, beat to the healthy side.
In the apogeotropic forms 2 3, after performing the HYT on the impaired side, the debris staying in the ampullary segment of the LSC, close to the cupula, will move away from the ampulla, resulting in an inhibitory, ampullofugal, endolymphatic current, causing apogeotropic paroxysmal positional Ny, beating to the healthy ear. Turning the head on the opposite side, the otoliths will drop towards the ampulla, with an excitatory discharge, and an apogeotropic paroxysmal positional Ny beating to the affected side will be observed.
The HYN beating towards the affected ear is stronger than the HYN beating on the healthy one, according to Ewald’s second law 4, which postulates that the response to an excitatory stimulus is always more intense than that following an inhibitory stimulus.
Another sign to diagnose the affected side is the direction of the Ny when the patient is briskly brought from the seated position to the supine position: Seated Supine Positioning Test (SSPT) 5 6. When the patient lies supine, having the head flexed 30°, the LSC is on a vertical plane; therefore, due to both gravity and the brisk deceleration caused by this manoeuvre, the otoliths are pushed downwards: when they are in the posterior arm they float towards the utricle, and when they are near the cupula they float towards the ampulla (Fig. 1). Therefore, the SSPT evokes a Ny beating towards the healthy side in the geotropic forms and towards the affected side in the apogeotropic forms: Seated Supine Positioning Nystagmus (SSPN).
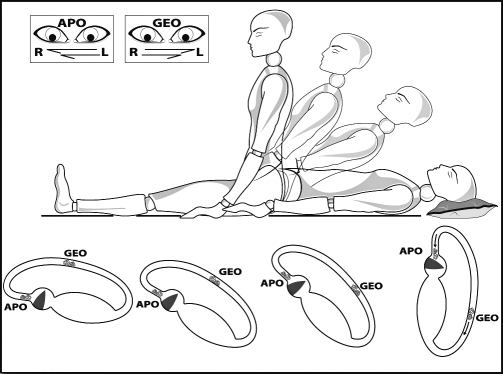
Fig. 1.
Seated Supine Positioning Test in right LSC-BPPV: when patient lies supine, with head flexed 30°, LSC is on a vertical plane; therefore, due to both gravity and the brisk deceleration caused by this manoeuvre, the otoliths are pushed downwards: when in the posterior arm they float towards the utricle, and when close to the cupula they float towards the ampulla. Therefore, SSPT evokes a Ny beating towards the healthy side in geotropic forms (GEO) and towards the affected side in apogeotropic forms (APO): Seated Supine Positioning Nystagmus (SSPN).
Several therapeutic techniques have demonstrated their effectiveness in treating LSC-BPPV: Forced Prolonged Position (Vannucchi Technique), Barbecue Rotation (Lempert Manoeuvre, Vannucchi-Asprella Manoeuvre), Gufoni Manoeuvre 7–9. As manoeuvres should be performed toward the healthy side, the identification of the involved side is crucial in choosing the most suitable therapeutic programme.
The Pseudo-Spontaneous Nystagmus (PSN) is a new clinical sign to diagnose the impaired side of LSC-BPPV described, for the first time, in 2005 6.
The Author examined the occurrence of the PSN in a large cohort of patients, evaluating its efficacy in the identification of the affected side.
Materials and methods
A total of 1643 patients affected by BPPV were observed from January 2005 to October 2007. Of these, 293 were due to LSC-BPPV, out of which 197 were geotropic and 96 apogeotropic.
The diagnosis of LSC-BPPV was made on the basis of the following characteristics:
a brief and intense vertigo induced by rotating the head in the supine position, which very often abruptly wakes the patient up during the night, and which reappears every time the patient turns the head from side to side while supine;
a typical bidirectional/bipositional horizontal paroxysmal Ny beating to the lowermost ear in the geotropic form and to the uppermost ear in the apogeotropic form, which is provoked by turning the head 180° to either side in the supine position performing the HYT;
diagnosis of the affected side was based on the Ny evoked by the HYT which beats with more intensity towards the impaired ear, and on the SSPN which beats towards the healthy ear in the geotropic form and towards the impaired ear in the apogeotropic form. In addition, all the patients were checked for the PSN and its beating direction;
all patients with neurological or other vestibular identifiable disorders were excluded.
All patients were examined by using an infrared videonystagmoscopy system (IR-VNS), with three video cameras, one for each eye and one for monitoring the position of the patient. Almost all examinations were recorded on DVD.
The patients underwent the following strategy of approach: first, spontaneous Ny in seated position was investigated, the patients then underwent the SSPT, and, thereafter, the HYT was performed.
When a spontaneous Ny was observed, the direction was first analysed with the head in axis with the body, then with the head bent 30° and 60° forwards and, finally, with the head bent 30° backwards in the seated position.
An evocative manoeuvre was used in the patients without spontaneous Ny: a very slow repeated horizontal rotation of the head, in the seated position, after that a spontaneous Ny appeared in some patients.
When a SSPN was evoked by the SSPT, the head was turned in the same direction the Ny was beating, with the patient supine, then if the Ny persisted or increased in intensity, the diagnosis of a geotropic form of LSC BPPV was confirmed; conversely, if the Ny decreased, stopped and then reversed its direction, an apogeotropic form was diagnosed.
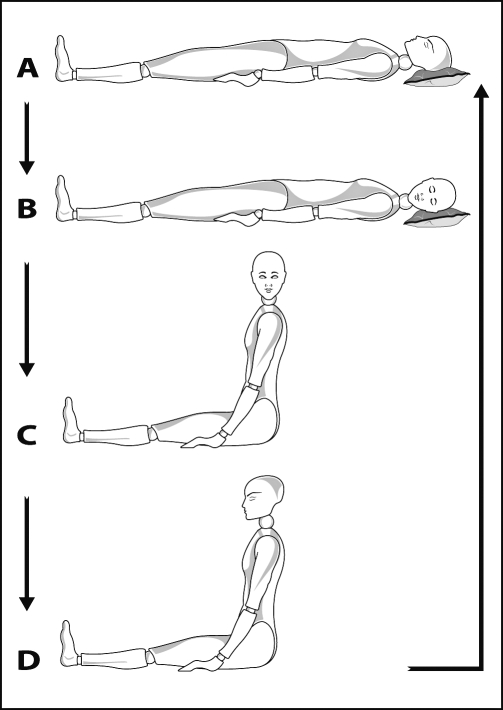
Immediately after both the diagnosis of the affected side and of the geotropic or apogeotropic form were completed, treatment was performed in the same session. A variant of the barbecue rotation manoeuvres was preferred: the Vannucchi-Asprella manoeuvre (Fig. 2), which combines very good patient compliance and high effectiveness, both in geotropic and apogeotropic forms. As in the typical barbecue manoeuvre the patient, in the supine position, quickly rotates the head 90° towards the healthy side; keeping the head turned in this way, he/she sits and slowly brings the head back in line with the body. This sequence of movements is repeated five times or more, as long as it does not provoke nystagmus or vertigo.
Fig. 2.
Vannucchi-Asprella manoeuvre in right LSC-BPPV: A. Patient lies in supine position; B. Head is briskly turned 90° towards the healthy side; C. while keeping head turned, patient is returned to the seated position; D. Head is slowly brought back in axis with body; A. Patient is returned to the supine position. This sequence of movements is repeated five times or more, if necessary, as long as no Ny or vertigo appears.
In the apogeotropic form, first of all, the transformation into a geotropic form was attempted, by doing a very brisk 180° rotation of the patient’s head towards the healthy side in the supine position, then the treatment was continued with the Vannucchi-Asprella manoeuvre.
Treatment was always carried out under IR-VNS control, in order to monitor the effective migration of the otolithic mass in an ampullofugal direction, which is confirmed by a Ny beating to the healthy side, that is inhibitory, due to the ampullofugal deflection of the cupula when carrying out the single steps of the manoeuvre.
The effectiveness of treatment was checked by repeating the SSPT and the HYT after one hour, and after three days.
After treatment, all patients were instructed to lie in bed, at night, on the healthy ear, for three nights, until the next vestibular control.
Results
Of the 293 patients affected by LSC-BPPV, 187 were female and 106 were male, age range 9-86 years (mean 54, median 57 years).
Six patients had a bi-canalar BPPV with a concomitant involvement of the lateral and posterior canals, and another two patients had a three-canalar BPPV involving also the anterior canal. All the pluri-canalar forms were post head traumas BPPV.
The onset of the symptom before the patients underwent vestibular examination varied from 2 hours to 4 months, with a mean of 7 days.
A stationary spontaneous horizontal Ny was observed in the seated position with the patient’s head in axis with the body in 76% (222 patients) (Table I).
Table I. Clinical signs for affected side diagnosis in LSC BPPV.
| Clinical sign | Incidence % |
| SSPN | 96 |
| PSN | 76 |
| PSN after head horizontal rotation | 96 |
| HYN intensity | 97 |
SSPN = Seated Supine Positioning Nystagmus; PSN = Pseudo-Spontaneous Nystagmus; HYN = Head Yaw Nystagmus.
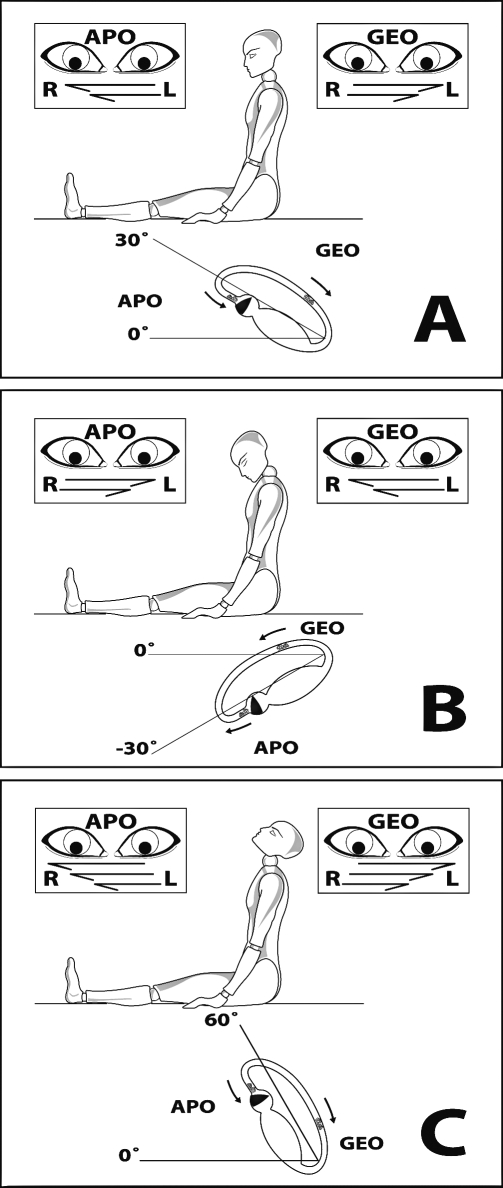
A slow, repeated, horizontal rotation of the head, in the seated position, increased the percentage of PSN to 96% (281 patients) (Table I). Furthermore, in all these patients the PSN disappeared with the head bent 30° forward (neutral position), it reversed direction with the head bent 60° forward, it beat again in the initial direction when the head was returned in axis with the body and it increased in intensity extending the head about 30° backwards: Head Pitch Test (HPT) (Fig. 3).
Fig. 3.
Pseudo-Spontaneous Nystagmus: (A) LSC is bent 30° compared to horizontal plane, in patient seated with head in axis with the body, it works as an inclined plane where otoliths can slowly float. PSN beats towards healthy ear in geotropic forms (GEO), whereas it beats towards affected ear in apogeotropic forms (APO). (B) When patient’s head is bent forwards, pseudo-spontaneous Ny inverts its direction, (A) when head is returned in axis with body or (C) is bent backwards it beats again in the initial direction. Changing LSC bending angle, otoliths change direction and velocity, settling along the canal, consequently, PSN increases intensity when head is bent backwards and LSC is approximately bent 60° on horizontal plane (C).
In all these patients, the PSN disappeared after successful rehabilitation treatment.
The SSPN was evoked by performing the SSPT in 281 patients (96%) (Table I), 189 of which had a geotropic form and 92 an apogeotropic form. In the geotropic forms, the SSPN beats towards the healthy side and in the apogeotropic forms towards the affected side.
Both the SSPN and the PSN, observed in the seated position (with the head in axis with the body), beat always in the same direction. In addition, the PSN increased in intensity after the SSPT in 96% of these patients.
Only 12 patients, 8 with a geotropic, and 4 with an apogeotropic LSC-BPPV, showed neither the spontaneous Ny nor the SSPN. All these patients underwent the LSC-BPPV diagnosis with a delay of 2 to 4 months from the onset of the symptoms. In these patients, the HYT evoked no Ny after the initial rotations of the head, on each side, in the supine position.
Only after the head was turned 4-7 times, did a typical, geotropic or apogeotropic Ny finally appear. Two of these patients revealed a PSN, an SSPN and a typical Ny, evoked by HYT, only after performing a Head Shaking Test.
The affected side was determined by detecting the intensity of the Ny evoked by the HYT and by observing the direction of the PSN and of the SSPN (Table II): in the geotropic LSC-BPPV, the PSN and the SSPN beat to the healthy side and the HYN was more intense on the impaired side, while in the apogeotropic form the PSN and the SSPN beat to the affected side and the HYN was more intense on the healthy side. In all the patients in which the PSN and the SSPN were observed, both these diagnostic signs were in accordance with identifying the affected side, together with the Ny evoked by the HYT.
Table II. Clinical signs to diagnose affected side in LSC-BPPV.
| Direction of the more intense nystagmus in Head Yaw Test is towards affected ear. |
| Direction of both Pseudo Spontaneous Nystagmus and Seated Supine Positioning Nystagmus is towards unaffected ear in geotropic LSC-BPPV. |
| Direction of both Pseudo Spontaneous Nystagmus and Seated Supine Positioning Nystagmus is toward affected ear in apogeotropic LSC-BPPV. |
Only 9 patients, 3 with a geotropic, and 6 with an apogeotropic LSC-BPPV, showed an equal intensity Ny on each side in performing the HYT. In all these patients, the diagnosis of the affected ear was based on the direction of the PSN and of the SSPN and, consequently, they were successfully treated by the Vannucchi-Asprella manoeuvre, performed towards the healthy ear.
Overall, 98% of LSC-BPPV checked after 3-6 hours, recovered during the first treatment session and 2% recovered after 2-6 therapeutic sessions. The PSN and the SSPN always disappeared after resolution of the BPPV, achieved using liberatory manoeuvres.
Discussion
The real challenge in treatment for LSC-BPPV is to identify the affected ear.
The clinical signs currently described to identify the impaired side in LSC-BPPV are (Table II):
the intensity of the Ny evoked by performing the HYT;
the direction of the SSPN.
The affected side of the geotropic form is:
the side on which the HYN is more intense;
the side opposite the direction of the SSPN.
The affected side of the apogeotropic forms is:
the side on which the HYN is less intense;
the side to which the SSPN beats.
The present study confirms the efficacy of both the above-mentioned clinical signs in identifying the impaired ear in LSC-BPPV.
Furthermore, a spontaneous Ny was observed in 76% of the patients enrolled in this study. In my opinion, this spontaneous Ny is a Pseudo-Spontaneous Nystagmus (PSN), it is a particularly long-lasting, non-paroxysmal Ny caused by involuntary, horizontal rotations of the patient’s head just before undergoing the vestibular examination. These rotations cause the slow floating of the otoliths, as the LSC is bent 30° compared to the horizontal plane, in the patient seated with the head in axis with the body.
It is useful to slowly rotate the patient’s head horizontally. In fact, this manoeuvre increases the percentage of PSN to 96%.
The physiopathology of PSN is due to the 30° inclination of the LSC with respect to the horizontal plane. Therefore, it behaves as an inclined plane where otoliths can slowly gravitate, due to unintentional or provoked rotations of the head to both sides around the vertical axis.
Furthermore, when the patient’s head is bent forwards, the pseudo-spontaneous Ny stops, reaching a bending angle of 30°, so that the LSC is perfectly aligned with respect to the horizontal plane, thus no gravity action is effective in moving the otoliths inside the canal (neutral position); the PSN inverts its direction when the patient’s head is bent about 60° forwards, then it beats again to the initial direction when the head is returned in axis with the body and increases when the head is bent 30° backwards. Changing the LSC bending angle, the otoliths change their direction and velocity, settling along the canal.
A diagnostic meaning can be assigned to the PSN, since it beats in the same direction as the Ny evoked, when the patient is briskly brought from the seated position to the supine position: SSPN. Therefore, in geotropic forms, the PSN beats to the healthy ear, whereas in apogeotropic forms, it beats to the affected ear. Passing from the seated to the supine position usually increases the intensity of the PSN, as this manoeuvre bends the LSC from 30° to 90° with respect to the horizontal plane, provoking greater movement of the otoliths causing a wider deflection of the cupula. When the patient is in the supine position with the head flexed 30°, the LSC is placed on a vertical plane (Fig. 1); due to both gravity and the brisk deceleration in the passage from the seated to the supine position, otoliths are pushed downwards: if they are in the posterior arm of the LSC (geotropic LSC-BPPV), they float towards the utricle, whereas if they are near the cupola (apogeotropic BPPV), they float towards the ampulla (Fig. 1).
Only 12 out of 293 patients did not show either the PSN or the SSPN. In all of these patients, diagnosis was made some months later and, moreover, the HYT was initially ineffective in eliciting any Ny. In patients with a delayed diagnosis, the HYN may not be evoked the first time the head is turned to the left or right side. Sometimes, only a few jerks of non-paroxysmal Ny can be evoked after rotating the head 180° to each side. A typical LSC-BPPV paroxysmal Ny was evoked after repeating the HYT 3-10 times and at the same time both PSN and SSPN appeared.
In these patients, the otoliths were initially spread inside the LSC. In fact, the movement of otoliths is effective in deflecting the cupula only if they are gathered in such a way as to act as a piston 10. The repeated head rotations make them move, causing them to gather, due to the forces of superficial adhesion.
Conclusions
The differential diagnosis between a spontaneous nystagmus and a PSN is easy to achieve with the Head Pitch Test (HPT) in the sitting position: with the head bent 30° forward the PSN disappears (neutral position), it reverses direction with the head bent 60° forward, it becomes visible again bringing the head in axis with the body and increases in intensity extending the head about 30° backwards.
This study proves the effectiveness of PSN in determining the affected ear in LSC-BPPV.
The resolution of the LSC-BPPV in patients with a symmetrical HYN, confirms the efficacy of both these clinical signs, the PSN and the SSPN, in order to identify the affected ear in LSC-BPPV.
References
- 1.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec 1989;51:161-70. [DOI] [PubMed] [Google Scholar]
- 2.Nuti D, Vannucchi P, Pagnini P. Benign paroxysmal positional vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vestib Res 1996;6:173-84. [PubMed] [Google Scholar]
- 3.Pagnini P, Vannucchi P, Nuti D. Le nystagmus apogéotrope dans la vertige paroxystique positionnel bénin du canal sémi-circulaire horizontal: une canalolithiase. Revue d’ONO 1994;31:17-9. [Google Scholar]
- 4.Ewald R. Physiologische Untersuchungen über das Endorgan des Nervus Octavus. Weisbaden: Bergmann; 1892. [Google Scholar]
- 5.Nuti D, Vannucchi P, Pagnini P. Lateral canal BPPV: Which is the affected side? Audiological Medicine 2005;3:16-20. [Google Scholar]
- 6.Asprella-Libonati G. Diagnostic and treatment strategy of the lateral semicircular canal canalolithiasis. Acta Otorhinolaryngologica Italica 2005;25:277-83. [PMC free article] [PubMed] [Google Scholar]
- 7.Asprella-Libonati G, Gagliardi G, Cifarelli D, Larotonda G. “Step by step” treatment of lateral semicircular canal canalolithiasis under videonystagmoscopic examination. Acta Otorhinolaryngologica Italica 2003;23:10-5. [PubMed] [Google Scholar]
- 8.Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope 1996;106:476-78. [DOI] [PubMed] [Google Scholar]
- 9.Vannucchi P, Asprella-Libonati G, Gufoni M. The physical treatment of lateral semicircular canal canalolithiasis. Audiological Medicine 2005;3:52-6. [Google Scholar]
- 10.Epley JM. Positional vertigo related to semicircular canalolithiasis. Otolaryngol Head Neck Surg 1995;112:154-61. [DOI] [PubMed] [Google Scholar]