Summary
Isolated congenital malformations of semicircular canals are rare abnormalities. Most inner ear abnormalities occur in syndromes and are associated with hearing loss. Unilateral or bilateral single aplasia of one semicircular canal does not usually result in vertigo, but these become clinically important if there are clinical complaints of vertigo. Computed tomography imaging and high resolution magnetic resonance imaging may reveal inner ear abnormalities. The case is presented here of a 46-year-old male with a 10-year history of recurrent positional vertigo with strong onset when changing position to the left side. Magnetic resonance imaging of the inner ear showed a bilateral posterior semicircular canal aplasia as well as an enlarged vestibule on both sides. Dix-Hallpike positional manoeuvre revealed a positional nystagmus in the left head-hanging position of short duration and latency of a few seconds. When rising, vertigo occurred, but no nystagmus was visible. The fast phase of the nystagmus was mainly vertical down-beating with a slight torsional component to the uppermost ear. Although benign paroxysmal vertigo of the anterior canal was suspected, physical therapy was not effective using a modified liberatory manoeuvre. Brandt-Daroff therapy was effective permanently.
Keywords: Vertigo, Semicircular canal, Bilateral aplasia, Diagnosis, Brandt-Daroff therapy
Riassunto
Le malformazioni congenite isolate dei canali semicircolari sono rare. La maggior parte delle malformazioni dell’orecchio interno si ritrovano infatti associate in quadri sindromici caratterizzati da ipoacusia. L’aplasia mono- o bilaterale di un canale semicircolare può rimanere misconosciuta, e rendersi manifesta solo in caso di comparsa di sintomatologia vertiginosa. La tomografia computerizzata e la risonanza magnetica ad alta risoluzione permettono la diagnosi delle malformazioni dell’orecchio interno. Presentiamo il caso di un uomo di 46 anni con una storia di dieci anni di vertigini posizionali ricorrenti associate all’assunzione della posizione sul fianco sinistro. La risonanza magnetica dell’orecchio interno ha evidenziato un’aplasia bilaterale del canale semicircolare posteriore ed un allargamento del vestibolo da entrambi i lati. La manovra di Dix-Hallpike ha messo in evidenza un nistagmo posizionale con la testa ruotata verso sinistra di breve durata e con una latenza di qualche secondo. Al termine della manovra, si è osservata l’insorgenza di sintomatologia vertiginosa in assenza di nistagmo. La fase rapida del nistagmo risultava principalmente verticale diretta verso il basso e con una lieve componente torsionale. Nel sospetto clinico di una vertigine parossistica posizionale del canale anteriore, il paziente è stato sottoposto a manovra liberatoria modificata senza risoluzione della sintomatologia. Al contrario la manovra di Brandt-Daroff è risultata efficace in modo definitivo.
Introduction
Malformations of the semicircular canals are the most common congenital abnormalities of the inner ear. Depending on induction time during embryological development, they may involve simultaneous several structures such as the cochlea, vestibule, vestibular aqueduct or semicircular canals (SCC). Anterior semicircular canal (ASCC) and posterior semicircular canal (PSCC) dysplasia are commonly associated with a dysplastic lateral semicircular canal and severe hearing loss 1. The horizontal semicircular canal (HSCC) is the last single structure to be formed during embryogenesis of the inner ear. Malformation can be found as an isolated anomaly. Absence of three semicircular canals has been reported in Goldenhaar syndrome and CHARGE association 2 3. Congenital isolated abnormalities may not become clinically significant if not associated with hearing loss or acute aquired vertigo symptoms. Computed tomography (CT) and high resolution magnetic resonance imaging (HR-MRI) can identify peripheral vestibular lesions especially anomalies such as deformities of the bony labyrinth 4. T2 weighted turbo-spin-echo-sequences may show pathological changes of the membranous labyrinth 5. Detection of inner ear abnormalities is important in the diagnosis of vertigo symptoms. Furthermore, CT and MRI imaging are necessary for pre-operative planning of temporal bone surgery especially in preparation for cochlear implant surgery. However, there are still several vestibular diseases that cannot be visualized, such as vestibular neuritis, Menière`s disease and benign paroxysmal positional vertigo (BPPV). BPPV of one PSCC is the most common. Involvement of the HSCC is rare. ASCC BPPV has been described, but opinions are controversial 6 7. Besides the typical forms, there are some idiopathic forms of paroxysmal positional vertigo that cannot be classified (atypical BPPV).
A case of bilateral posterior canal aplasia and enlarged vestibule on both sides, associated with an atypical positional nystagmus is described.
Case report
A 46-year-old male presented with a history of vertigo episodes for 10 years. Until the onset of vertigo no symptoms were present. There was no trauma and no history of inner ear diseases in the past. Clinical examination, including otomicroscopy, showed no pathological findings. Pure tone audiogram showed a bilateral symmetrical sensorineural hearing loss (high tone reduction) with a linear increase of hearing loss above 3,000 Hz.
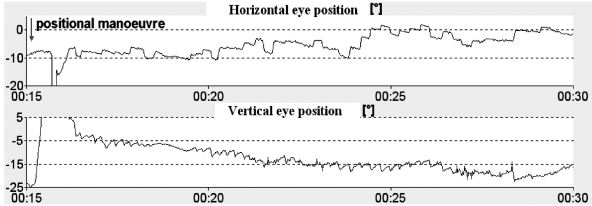
There was no spontaneous nystagmus using Frenzel glasses. Since the patient reported dizziness when lying on his left side, vertigo and nystagmus were provoked using the Dix-Hallpike manoeuvre. Vertigo occurred after a latency of 3 seconds with head rotation, of approximately 45 degrees, to the left. A predominantly down-beating nystagmus with a slight torsional nystagmus component and a quick phase toward the uppermost ear was observed using Frenzel glasses and two dimensional video-oculography (Fig. 1). The duration of nystagmus and vertigo was approximately 20 seconds and showed a crescendo-decrescendo pattern. Repetition resulted in decreasing of symptoms.
Fig. 1.
Ageotropic (counterclockwise) positioning nystagmus when Dix-Hallpike test was performed. Nystagmus was vertical with the vertical component beating downwards.
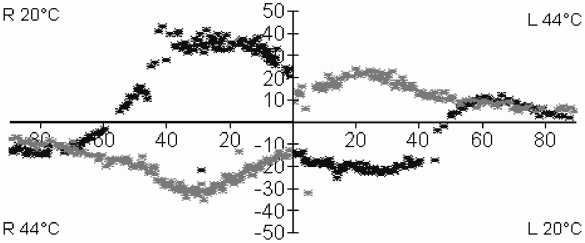
In a sitting position, there was no positional nystagmus, but vertigo, that was reproducible on several days. Testing BPPV of the HSCC and in other positions of the head, no vertigo or nystagmus was observed. Caloric irrigation using water at 44 degrees (50 ml in 30 s) showed less excitation of the HSCC in comparison to the right side (Fig. 2) but was within the normal range. Testing the thermal stimulus with water at 20 °C when the patient was turned from the prone position in the face-down position after 40 s showed a change in direction of induced nystagmus. In conclusion, utriculus function was assessed as normal. Otolithic function (sacculus), also tested using vestibular evoked myogenic potentials (VEMP), off vertical axis rotation (OVAR) and eccentric rotation, static lateral tilting, showed no pathological findings. On account of the unusual nystagmus constellation and the fact that the liberatory manoeuvre for ASCC BPPV of the right side did not improve complaints, CT and MRI imaging were performed. Inner ear structures showed aplasia of both PSCC. No central nervous diseases were revealed at CT or MRI of the head. Brandt-Daroff exercises were performed successfully (Figs. 3, 4, 5a-d).
Fig. 2.
Result of thermal irrigation using 44 and 20 degrees of water. Patient was turned after 40 seconds from pronation (Hallpike) in supination (“anti” Hallpike) position.
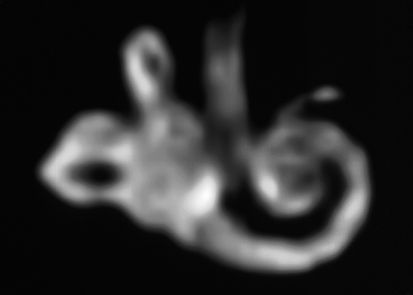
Fig. 3.
MRI, Maximum intensity pixel (MIP) projection shows aplasia of the right PSCC and an enlarged vestibule (right side).
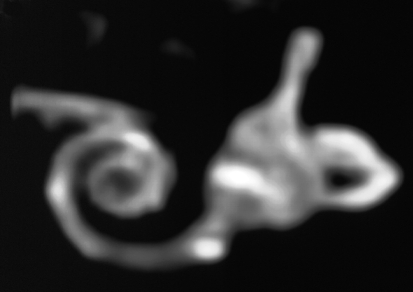
Fig. 4.
MRI, Maximum intensity pixel (MIP) projection shows aplasia of the left PSCC and an enlarged vestibule (left side).
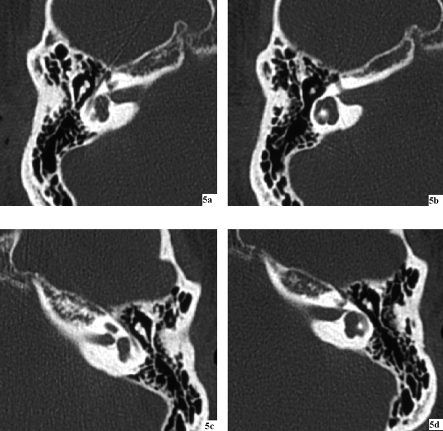
Fig. 5a-d.
CT-scans show an enlarged vestibule on both sides.
Discussion
Inner ear development is a complex process involving growth of labyrinth structures in three dimensions. The embryological origin of the inner ear is the so-called ear vesicle. This divides into a ventral part, composed of sacculus and ductus cochlearis and a dorsal component, the utriculus. Development of the inner ear begins after 6 weeks. Three SCC arise at the same time from three flattened protuberances of the utriculus 8. Further SCC development is a process of growth and fusion of the protuberances.
Single malformation of the posterior semicircular canal has been described in several diseases. Higashi et al., in 1992, found in 26% of all cases, aplasia of the PSCC, as a characteristic symptom in Waardenburg syndrome 9. Irie et al., in 1990, reported on two cases of unilateral aplasia of PSCC in Waardenburg syndrome. They also described an association with enlarged vestibules 10. Furthermore, abnormalities of the SCC can be found in CHARGE association 11 and trisomie 18 12. Among the SCC, HSCC malformations are the most frequent 13. PSCC aplasia seems to be comparatively rare. Probably, the SCC malformation is the result of an abnormal fusion during embryological development. Kiernan et al., in 2002, described a model for canal truncation in mutants. They demonstrated that SCC development is encoded in the proximal portion of chromosome 4 near the centromere 14.
To our knowledge, bilateral loss of PSCC has, until now, not been described in the present literature. Isolated uni- or bi-lateral SCC malformations may be clinically undetectable because of the complete compensation. Therefore, CT and MRI are indispensable diagnostic tools in some selected cases 15 16. Sennaroglu et al. recently presented a new classification for cochleo-vestibular malformations. Bilateral aplasia of the posterior SCC can be reassigned to the vestibular subgroup of this classification system with single semicircular malformations 17.
Since vertigo and nystagmus occurred strictly, in this case, at the left head hanging position and in the plane of the right anterior SCC during Dix-Hallpike manoeuvre, BPPV was a possible differential diagnosis in the absence of both PSCC. From the geometric orientation of the SCC, taking up the Dix-Hallpike position, either the right anterior and the left posterior SCC or the left anterior and the right posterior SCC are situated approximately in the same direction. Downbeat nystagmus, during Hallpike manoeuvre, with a slight counter-clockwise torsional component, in the present case, gave rise to the assumption of anterior canal (AC) BPPV as a differential diagnosis. The presence of anterior canal BPPV is rare. Some Authors doubt its existence. The anterior canal is normally the highest part of the inner ear. The otoconial debris in BPPV would naturally tend to fall into the posterior canal and, therefore, the PSCC BPPV is the most common variant of BPPV. In rare cases, the horizontal canal may be involved in BPPV.
Bertholon et al. described 50 cases with down beating nystagmus and assumed that some patients with idiopathic paroxysmal down beat nystagmus have paroxysmal positional vertigo with lithiasis of the anterior canal 18. The torsional component may be weak on account of the predominantly saggital orientation of the anterior canal and, clinically, may not be readily detected.
Rapoport and Sadeh 19 also observed patients with an atypical paroxysmal positioning vertigo. They showed apogeotropic nystagmus when the Dix-Hallpike test was performed. Nystagmus was torsional and vertical with the vertical component beating downwards. The torsional component was beating away from the lowermost ear. The Authors assumed ASCC BPPV in these cases. The absence of central nervous system signs and symptoms as well as normal imaging suggested that this predominantly vertical nystagmus may be another variant of BPPV.
Typical forms of paroxysmal positional vertigo are the variants of BPPV (PSCC and HSCC BPPV) and the central paroxysmal positional vertigo (CPPV) 20 21. The duration of CPPV is usually longer than BPPV 20 and the direction of nystagmus does not correspond with the plane of the SCC. On account of the absence of nystagmus in the sitting position during Hallpike positioning and the fact that the liberatory manoeuvre for the right anterior SCC were not successful, in this case, other forms of paroxysmal positional vertigo seem to be likely. Some atypical forms, without any central nervous involvement, may, therefore, derive from peripheral vestibular origin but the mechanism is still not completely understood.
In summary, congenital bilateral aplasia of the semicircular canals may be clinically silent if there is no additional vertigo. Patients with atypical BPPV should be submittted to CT and MRI imaging.
References
- 1.Lemmerling M, Kollias Spyros S. Radiology of the petrous bone. Roma: Springer; 2004. [Google Scholar]
- 2.Murofushi T, Ouvrier RA, Parker GD, Graham RI, da Silva M, Halmagyi GM. Vestibular abnormalities in CHARGE association. Ann Otol Rhinol Laryngol 1997;106:129-34. [DOI] [PubMed] [Google Scholar]
- 3.Lemmerling MM, Vanzieleghem BD, Mortier GR, Dhooge IJ, Kunnen MF. Unilateral semicircular canal aplasia in Goldenhar’s syndrome. Am J Neuroradiol 2000;21:1334-6. [PMC free article] [PubMed] [Google Scholar]
- 4.Jäger L, Strupp M, Brandt T, Reiser M. Bildgebung von Labyrinth und Nervus vestibularis. Nervenarzt 1997;68:443-58. [DOI] [PubMed] [Google Scholar]
- 5.Krombach GA, Schmitz-Rode T, Tacke J, Düwel P, Di Martino E, Engelke JC, et al. Magnetic resonance tomography imaging of the inner ear of patients with sensorineural hearing loss or vertigo. Laryngorhinootologie 2001;80:177-81. [DOI] [PubMed] [Google Scholar]
- 6.Von Brevern M, Lempert T. Benigner paroxysmaler Lagerungsschwindel. HNO 2002;50:671-81. [DOI] [PubMed] [Google Scholar]
- 7.Vannuchi P, Giannoni B, Pagnini P. Treatment of horizontal semicircular canal benign paroxysmal positional vertigo. J Vestib Res 1997;7:1-6. [PubMed] [Google Scholar]
- 8.Langman J. Medizinische Embryologie. Sixth Edn. Stuttgart, New York: Thieme; 1977. [Google Scholar]
- 9.Higashi K, Matsuki C, Sarashina N. Aplasia of posterior semicircular canal in Waardenburg syndrome type II. J Otolaryngol 1992;21:262-4. [PubMed] [Google Scholar]
- 10.Irie K, Ogata H, Mitsudome A. CT findings of the temporal bones in Waardenburg’s syndrome. No To Hattatsu 1990;22:241-6. [PubMed] [Google Scholar]
- 11.Wiener-Vacher SR, Amanou L, Denise P, Narcy P, Manach Y. Vestibular function in children with the CHARGE association. Arch Otolaryngol Head Neck Surg 1999;125:342-7. [DOI] [PubMed] [Google Scholar]
- 12.Wright CG, Brown OE, Meyerhoff WL, Rutledge JC. Inner ear anomalies in two cases of trisomy 18. Am J Otolaryngol 1985;6:392-404. [DOI] [PubMed] [Google Scholar]
- 13.Johnson J, Lalwani AK. Sensorineural and conductive hearing loss associated with lateral semicircular canal malformation. Laryngoscope 2000;110:1673-9. [DOI] [PubMed] [Google Scholar]
- 14.Kiernan AE, Erven A, Voegeling S, Peters J, Nolan P, Hunter J, et al. ENU mutagenesis reveals a highly mutable locus on mouse Chromosome 4 that affects ear morphogenesis. Mamm Genome 2002;13:142-8. [DOI] [PubMed] [Google Scholar]
- 15.Wright CG, Brown OE, Meyerhoff WL, Rutledge JC. Auditory and temporal bone abnormalities in CHARGE association. Ann Otol Rhinol Laryngol 1986;1:480-6. [DOI] [PubMed] [Google Scholar]
- 16.Madden C, Halsted MJ, Hopkin RJ, Choo DI, Benton C, Greinwald JH Jr. Temporal bone abnormalities associated with hearing loss in Waardenburg syndrome. Laryngoscope 2003;113:2035-41. [DOI] [PubMed] [Google Scholar]
- 17.Sennaroglu L, Saatci I. A new classification for cochleovestibular malformations. Laryngoscope 2002;112:2230-41. [DOI] [PubMed] [Google Scholar]
- 18.Bertholon P, Bronstein AM, Davies RA, Rudge P, Thilo KV. Positional down beating nystagmus in 50 patients: cerebellar disorders and possible anterior semicircular canalithiasis. J Neurol Neurosurg Psychiatry 2002;72:366-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rapoport A, Sadeh M. Posterior semicircular canal type benign paroxysmal positioning vertigo with ageotropic paroxysmal positioning vertigo nystagmus. Audiol Neurol 2001;6:50-3. [DOI] [PubMed] [Google Scholar]
- 20.Brandt T, Strupp M, Dieterich M. Vertigo. Leitsymptom Schwindel (Gebundene Auscabe). Heidelberg: Steinkopff Verlag; 2004. [Google Scholar]
- 21.Büttner U, Brandt T, Helmchen C. Diagnostic criteria for central vs. peripheral positioning nystagmus and vertigo. Acta Otolaryngol 1999;119:1-5. [DOI] [PubMed] [Google Scholar]