Summary
Cervicofacial actinomycosis is the most common clinical form of actinomycosis. This bacterial infection is rare. Diagnosis is difficult, often it is definitive only after surgical excision of the cervicofacial mass. Personal experience is reported concerning two cases of cervicoactinomycosis. Diagnosis, in both cases, has been based on histological findings, not on clinical symptoms. A review of the literature shows that mainly males are affected by this condition and, in fact, both patients described here are males. Symptoms of acute infection were absent. Both patients denied any history of oromaxillofacial trauma or recent dental extraction or oral manipulations. Imaging techniques – ultrasonography and computerized tomography – were not effective in making the diagnosis, in either of these patients. Furthermore, fine needle aspiration cytology did not provide a definitive diagnosis. Both patients underwent surgical excision of the mass. Penicillin was the drug of choice in post-operative long-term treatment (one month). In one of the two men, intravenous steroids were administered. As in several reports in the literature, the definitive diagnosis was histological and not clinical.
Keywords: Head and neck, Bacterial infection, Actinomycosis
Riassunto
La actinomicosi cervicofacciale è la più comune forma clinica della actinomicosi, infezione batterica rara. La diagnosi è difficile e spesso definitiva solo dopo la exeresi chirurgica della massa cervicofacciale. La nostra esperienza consta di due casi che abbiamo trattato circa due anni fa. In entrambi i casi la diagnosi si è basata sui dati istologici e non su quelli clinici. Come si può trovare anche in letteratura i nostri pazienti erano uomini e non avevano sintomi di flogosi acuta in atto. I nostri pazienti non hanno riferito recenti traumi a carico del distretto maxillo facciale né estrazioni dentarie né altri trattamenti al cavo orale. Le indagini diagnostiche per immagini che avevano effettuato (ecografia e tomografia computerizzata) non hanno dato informazioni adeguate a porre la diagnosi; neanche l’ago aspirato ecoguidato con ago sottile ha portato ad una diagnosi certa. Sono stati entrambi sottoposti ad intervento chirurgico e ad una terapia antibiotica postchirurgica prolungata per un mese con penicillina per via orale. Come in molti riferimenti bibliografici anche nei nostri casi la diagnosi è stata istologica.
Introduction
Actinomycosis was first described as a clinical entity over 100 years ago 1: in fact, the first case of actinomycosis, in man, was described by Von Langebeck, in 1845, and it was attributed to a fungus. Israel and Ponfick, in 1891, defined the anaerobic nature of actinomyces and isolated it in man. In the 1960’s, Waksman showed that actinomyces was a Gram positive bacteria. Actinomycosis is a suppurative and granulomatous chronic infectious disease, rarely diagnosed in the human 2–9.
Actinomyces are non acid fast, anaerobic or microaerophilic filamentous branched bacteria, living as commensal organisms in the human oral cavity and respiratory and digestive tracts, becoming invasive when, through a mucosal lesion, they gain access to the subcutaneous tissue 10.
Of the five actinomyces species causing actinomycosis infection in man, Actinomyces Israeli is the most frequently isolated; it takes the name from J. Israeli 11.
In 1938, Cope classified actinomycosis infection into three distinct clinical forms: cervicofacial, pulmonary or pulmothoracic, abdominal-pelvic 3–5 10–12.
It may involve the female genital organs, in the event an intra-uterine device is in use 11.
The first of these manifestations is the most frequent (50%), although uncommon 1–4 10–15.
Case reports
Two cases are described of cervicofacial actinomycosis, diagnosed and treated on february 2005.
Patient no. 1: A.L., a 39-year-old man, a bricklayer, smoker and drinker, in good health, with a 3 months’ history of a firm mass in the right cervical region. He did not present fever but, sometimes, moderate pain in the right side of the neck.
The ENT examination was requested by his family doctor. Routine blood tests were normal. Serological tests, such as microbiological tests, were negative for tuberculosis.
The rhino-pharyngo-laryngeal region, explored by flexible fiberoptic examination, was normal. Thorax and teeth, studied by standard radiology, were normal.
A.L. reported a cutaneous sinus, discharging pus, in the same site as the cervical mass, one month before, that closed spontaneously.
The patient had previously been treated with Rokitamycinum tablets (800 mg/day). This treatment was interrupted immediately on account of an allergy and replaced with Levofloxacinum tablets (500 mg/day) for 10 days without success. The patient underwent ultrasonography (US) which revealed an oval hypoechogeneous dyshomogeneous mass, approximately 3.5 x 1.5 cm in size in the right side of the neck. Also associated were submandibular lymphadenopathies, (max 1.6 cm in size) on the other side of the neck.
A computerized tomography (CT) scan (Fig. 1) of the neck confirmed a right cervical mass without particular characteristics useful for diagnosis. It helped only in defining the extension of the disease.
Fig. 1.
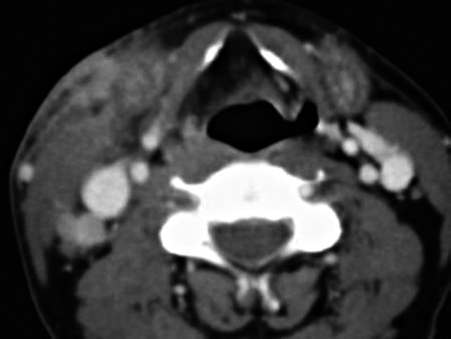
CT before surgical management. Beside the right submandibular gland, a well-defined area with infiltration of the adjacent fat tissue can be seen. There is also a lymph node with moderate enhancement (~ 2.5 cm in size). Multiple smaller lymph nodes are present in both internal jugular chains.
Fine needle aspiration cytology (FNAC) was not effective for diagnosis: the specimen was not useful as it did not contain pathological tissue, but only red cells and granulocytes.
Within one week, the mass increased rapidly in size and the neck skin became erythematous, hot and red, without injury. A.L. was, therefore, admitted to our ENT Department and operated on for a selective right neck dissection; he then received treatment with intravenous (iv) Piperacillinum + Tazobactanum 2 g + 0.250 g x 3/day and Betamethasone iv 4 mg/2 ml/day for 6 days, then with oral Amoxicillinum + Acidum Clavulanicum 875 mg + 125 mg tablets x 3/day for one month.
Actinomycotic colonies were detected in the surgically resected tissue (Fig. 2).
Fig. 2.
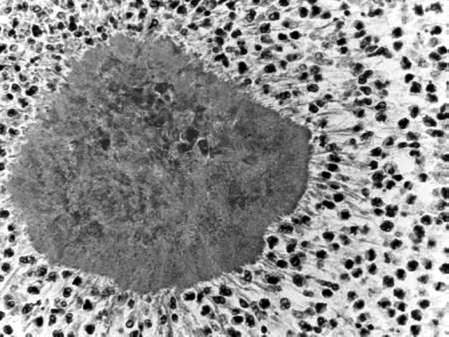
Microscopic findings of colonies of Actinomyces: characteristic micro-organisms with a filamentous appearance.
Therefore the definitive diagnosis was lymphadenitis due to Actinomyces.
Six months after surgical treatment, CT demonstrated the absence of relapse (Fig. 3); after two years the patient remains free of disease.
Fig. 3.

Post-operative CT (after 6 months). The mass involving the fat tissue on the right side of the neck is no longer visible. In the right submandibular region and in the cervical spaces, multiple small lymph nodes, < 1 cm in size, are present.
Patient no. 2: A.B., a 58-year-old man, allergic to Metamizolum Natricum, smoker, with high blood pressure, with recurrent headache, with a 12 months’ history of parotid gland swelling.
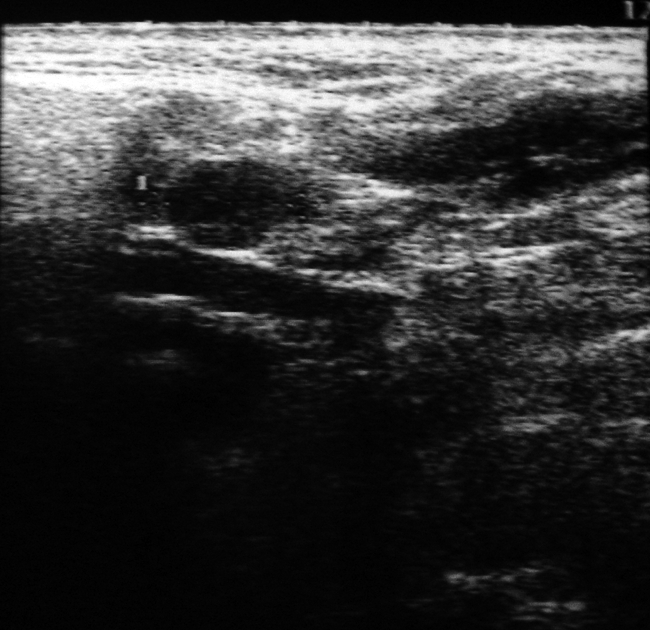
No fever or pain were present and the facial nerve was not involved. Panendoscopy was normal. The patient had not been treated with any drug. Routine blood tests were normal. Microbiological tests for tuberculosis were negative. A.B. was submitted to US which revealed an oval hypoecogeneous mass (~ 4 cm in size) in correspondence to the right parotid gland, as well as cervical and submandibular lymphadenopathies, on the same side (Fig. 4).
Fig. 4.

Ultrasonography features before surgical treatment. In the right cervical parotid space, a voluminous, dyshomogeneous and hyperechogeneous oval mass, about 4 cm in size, is visible.
FNAC revealed only necrosis and colliquate material. Surgical treatment was proposed as it was necessary to achieve a definitive and clear diagnosis.
A partial parotidectomy was performed.
One hour before the surgical excision, A.B. underwent short-term iv treatment with Amoxicillinum + Acidum Clavulanicum 2000 mg + 200 mg.
Four days after surgical treatment, fever and a sinus discharging yellow pus, related to the surgical wound, appeared.
Therefore, administration was commenced of Amoxicillinum + Acidum Clavulanicum 2000 mg + 200 mg iv x 2/day for 5 days, then oral Amoxicillinum + Acidum Clavulanicum 875 mg + 125 mg tablets x 3/day for one month.
The histological examination revealed a granulomatous reaction with sulphur granules (Fig. 5).
Fig. 5.
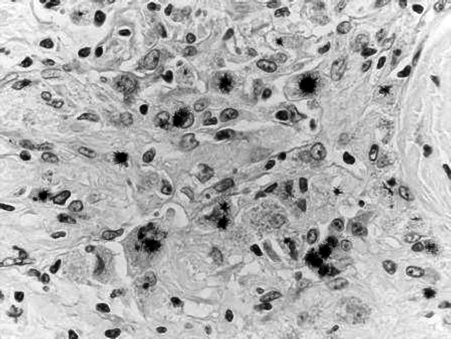
Macrophagic epithelioid cells: a central zone of necrosis and sulphur granules.
The definitive diagnosis was actinomycosis of the parotid gland.
Six months after surgical treatment, the patient refused to undergo magnetic resonance imaging (MRI) on account of claustrophobia and therefore US was performed which demonstrated the absence of relapse (Fig. 6); after two years the patient is still free of disease.
Fig. 6.
US post-operative treatment. Final result after management: there is no evidence of the pre-existing mass in the right parotid space.
Discussion
Cervicofacial actinomycosis is the most common form of this rare disease 1–4 13–15.
In cervicofacial actinomycosis, the sites most commonly involved include the submandibular space 3 6 7 10 11 16 17, cheek 3, parotid gland 2 3 8 16 18–20, teeth 3, tongue 3, nasal cavity, gingival and oral space, hypopharynx, medial aspect of ary-epiglottic fold 3, parapharyngeal space, hyoid area and the cartilage area of the thyroid 16, the frontal region 21, lymph nodes of the neck 6.
There is a slight male prevalence in young adults 11 12.
The well-known predisposition of male patients to acquire the disease varies with age and appears to be especially pronounced in patients aged 20-60 years, the highest incidence, in female patients, being found between 11-40 years and in male patients, aged 21-50 years 9.
There is no racial predisposition or geographic factors 11.
Most cases of cervical actinomycosis are odontogenic in origin and occur predominantly in immunocompetent individuals 5.
Actinomyces are usually of low pathogenicity and cause disease only in the setting of previous tissue injury 5: for example, as a complication of a maxillo facial trauma (a ski-pole injury of the face 21), after surgical procedures and/or dental manipulations 13, in patients presenting poor oral hygiene or caries 3 6 11, after recent dental treatment which usually involves extraction of a mandibular molar 2 8 10 11.
Actinomyces are bacteria that cannot penetrate healthy tissue and mucosal break-down is a prerequisite for infection 3 11.
Actinomycosis is an endogenous infection, there is no person to person transmission 11.
Malnutrition, radiation therapy, alcoholic, debilitating states, such as diabetes, malignancy and immuno-suppression, are considered predisposing factors.
The common initial signs and symptoms of infection such as fever, sudden onset of cervicofacial pain, swelling, erythema, oedema and suppuration may be absent 2 8.
Some Authors have described unusual cases of cervicofacial actinomycosis presenting as acute upper airway obstruction and demanding emergency tracheostomy 16 19.
Another patient had extensive cervical, posterior mediastinal and abdominal lymphadenopathy 6.
The infection most commonly presents as a chronic mass 6 10 16, as a suppurative or indurative mass 8 21 with discharging sinuses 5 10 13 20, as intra-oral lesions 13, combined with a parotid gland cystoadenolymphoma 19, as a chronic, often floating mass frequently located at the border of the mandible 6 10, with or without cervical lymphadenopathy 6.
According to some Authors, actinomycosis rarely involves the regional lymph nodes 3 10 11 or it develops late 3.
The macroscopic presence of the classic sulphur granules in tissue specimens or drainage may be of some help for diagnosis but Nocardiosis may also present with sulphur granules 3 7 10 15.
According to some Authors, the characteristic sulphur granules, in the specimens, are present in only 35-55% of cases. In these cases, the diagnosis is definitive 5 10 11 13 15 16.
The infection develops silently in a subacute form, as a solid mass, slowly increasing in size without pain 11 with erosion of skull bones 20 and infiltration of the ramus of the mandible 8 19.
Actinomycosis can present in a variety of forms and may mimic other infections such as tuberculosis, other chronic granulomatous lesions, fungal infection or even malignancy, both clinically as well as radiologically 1–8.
Imaging techniques such as CT and MRI usually yield non-specific findings, contributing only to define radiological features of the mass and its involvement in adjacent soft tissues 2 3 10 11 16.
These techniques provide only quantitative information (limits and borders of the lesions, homogeneity and density of the content, localization, invasion of surrounding organs etc.) 11.
Diagnosis may be difficult because of a general lack of familiarity with the disease and a low success rate in culturing the organism as a result of its fastidious nature 10–17.
Isolation of the organism and its identification take from 2 to 3 weeks (it grows slowly).
Cultures should be placed immediately in anaerobic conditions and incubated for approximately 48 hours 3 11.
FNAC is the method of choice in the diagnosis of cervical actinomycosis. It is an easy, safe, rapid and highly effective method 2 12 23.
It has become more and more important, since not only does it allow morphologic identification, but it is an effective means of collecting material for microbiologic identification 5 7 9 10 11 13 21–23.
Actinomycoses are usually sensitive to several antibiotics: penicillin G, chloramphenicol, tetracycline, erythromycin, clindamycin, imipenem, streptomycin, third-generation cephalosporins 1–16.
Penicillin is the drug of choice for prolonged treatment, usually administered for 2 to 12 months 5 7 13 15 16 18 21 22 24.
Tetracycline and erythromycin are employed in patients allergic to penicillin 10 11, or after intravenous penicillin, for oral use 8 17.
In the acute phase of treatment, penicillin can be replaced by third-generation cephalosporins which are also effective if co-infection with other bacteria, not responding to penicillin, causes persistence of symptoms due to Actinomyces 2 10 13.
A steroid (for example, methylprednisolone) is effective in eliminating the residual inflammatory granulomatous reaction 2 11.
Surgical treatment is often indicated for curettage of bone, resection of necrotic tissue, excision of sinus tracts, drainage of soft tissue abscesses 5 8 15 19 22.
Surgery plays an important role both in the diagnosis and treatment of actinomycosis 10 20.
Surgery is necessary if CT and US cannot exclude a neoplasm 3 8 16 19.
When the cervico-facial infection is circumscribed, of small size and not associated with draining fistulas, a medical approach is preferred to a surgical procedure 11.
Conclusions
Diagnosis of actinomycosis is not always easy. When it is not an occupational disease (for example, in agriculturists, butchers, breeders) diagnosis is difficult, both radiologically (with the help of US and CT) as well as by means of FNAC.
Actinomycosis is an aspecific granulomatous chronic infection, therefore results of routine blood tests are usually normal, sometimes leukocyte values are high.
Both of our patients denied any history of recent dental extraction or oral manipulations; our cases of actinomycosis were not odontogenic in origin.
FNAC is the method of choice for diagnosis of actinomycosis but, in our two cases, it was not effective.
The definitive diagnosis was possible only after surgical excision of the mass in both cases (a selective neck dissection in the first patient, a partial parotidectomy in the second), therefore, antibiotic treatment of choice has been administered only in the second time.
Both patients underwent treatment with oral penicillin, for one month.
Today, both patients are free of disease.
A correct diagnosis before the surgical approach would have been an excellent result.
The medical approach to actinomycosis, when possible, should be preferred to surgical excision of the mass.
References
- 1.Nagler R, Paled M, Laufer D. Cervicofacial actinomycosis: a diagnostic challenge. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:652-6. [DOI] [PubMed] [Google Scholar]
- 2.Biasotto M, Cadenaro M, Di Learda R. Actinomyces parotid infection after mandibular third molar extraction. Minerva Stomatol 2003;52:531-4. [PubMed] [Google Scholar]
- 3.Park JK, Lee HK, Ha HK, Choi HY, Choi CG. Cervicofacial actinomycosis: CT and MR imaging findings in seven patients. AJNR Am J Neuroradiol 2003;24:331-5. [PMC free article] [PubMed] [Google Scholar]
- 4.Bennhoff DF. Actinomycosis: diagnostic and therapeutic considerations and a review of 32 cases. Laryngoscope 1984;94:1198-217. [DOI] [PubMed] [Google Scholar]
- 5.Oostman O, Smego RA. Cervicofacial actinomycosis: diagnosis and management. Curr Infect Dis Rep 2005;7:170-4. [DOI] [PubMed] [Google Scholar]
- 6.Amnirikachi M, Krishnan B, Finch CJ, Shahab I. Actinomyces and actinobacillus actinomycetemcomitans-Actinomyces-associated lymphadenopathy mimicking lymphoma. Arch Pathol Lab Med 2000;124:1502-5. [DOI] [PubMed] [Google Scholar]
- 7.Kolebacz B, Stryjewska-Makuch G, Grzegorzek T. Cervicofacial actinomycosis – case reports. Otolaryngol Pol 2004;58:1019-22. [PubMed] [Google Scholar]
- 8.Lang-Roth R, Schippers C, Eckel HE. Cervical actinomycosis. A rare differential diagnosis of parotid tumor. HNO 1998;46:354-8. [DOI] [PubMed] [Google Scholar]
- 9.Pulverer G, Schutt-Gerowitt H, Schaal KP. Human cervicofacial actinomycosis: microbiological data for 1997 cases. Clin Infect Dis 2003;37:490-7. [DOI] [PubMed] [Google Scholar]
- 10.Volante M, Contucci AM, Fantoni M, Ricci R, Galli J. Cervicofacial actinomycosis: still a difficult differential diagnosis. Acta Otorhinolaryngol Ital 2005;25:116-9. [PMC free article] [PubMed] [Google Scholar]
- 11.Bubbico L, Caratozzolo M, Nardi F, Ruoppolo G, Greco A, Venditti M. Actinomycosis of submandibular gland: an unusual presentation Acta Otorhinolaryngol Ital 2004;24:37-9. [PubMed] [Google Scholar]
- 12.Das DK. Actinomycosis in fine needle aspiration cytology. Cytopathology 1994;5:243-50. [DOI] [PubMed] [Google Scholar]
- 13.Aguirrebengoa L, Romana M, Lopez L, Martin J, Montejo M, Gonzales De Zarate P. Oral and cervicofacial actinomycosis. Presentation of five cases. Enferm Infecc Microbiol Clin 2002;20:53-6. [DOI] [PubMed] [Google Scholar]
- 14.Albertos JM, Junguera LM, Palacios JJ, Gonzales M, Perez MJ, Gener M. Cervicofacial actinomycosis. An Otorrinolaringol Ibero Am 1997;24:255-68. [PubMed] [Google Scholar]
- 15.Balatsouras DG, Kaberos AK, Eliopoulos PN, Kandiloros D, Economou CN. Cervicofacial actinomycosis presenting as an acute upper respiratory tract obstruction. J Laryngol Otol 1994;108:801-3. [DOI] [PubMed] [Google Scholar]
- 16.Moriwaki K, Sakata Y, Kato T, Uno A, Nagai M, Sawada T. Report of two cases of actinomycosis of the neck, one acute and one chronic. Nippon Jibiinkoka Gakkai Kaiho 2000;103:1238-41. [DOI] [PubMed] [Google Scholar]
- 17.Khan AR, Arif S. Actinomycosis in neck glands. J Ayub Med Coll Abbottabad 2004;16:84-5. [PubMed] [Google Scholar]
- 18.Hensher R, Bowerman J. Actinomycosis of the parotid gland. Br J Oral Maxillofac Surg 1985;23:128-34. [DOI] [PubMed] [Google Scholar]
- 19.Barabas J, Suba Z, Szabo G, Nemeth Z, Bogdan S, Huszar T. False diagnosis caused by Warthin tumor of the parotid gland combined with actinomycosis. J Craniofacial Surg 2003;14:46-50. [DOI] [PubMed] [Google Scholar]
- 20.Varghese BT, Sebastian P, Ramachandran K, Pandey M. Actinomycosis of the parotid masquerading as malignant neoplasm. BMC Cancer 2004;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ermis I, Topalan M, Aydin A, Erer M. Actinomycosis of the frontal and parotid regions. Ann Plast Surg 2001;46:55-8. [DOI] [PubMed] [Google Scholar]
- 22.Vesely BT, Hyza P, Koncena J, Kuklinek I, Kozak J, Ranno R, et al. Unusual case of resistant actinomycosis following facial trauma. Acta Chir Plast 2005;47:119-23. [PubMed] [Google Scholar]
- 23.Custal-Teixidor M, Trull-Gimbernat JM, Garijo-Lopez G, Valldosera-Rosello M. Fine-needle aspiration cytology in the diagnosis of cervicofacial actinomycosis: report of 15 cases. Med Oral Patol Oral Cir Bucal 2004;9:464-7;467-70. [PubMed] [Google Scholar]
- 24.Sudhakar SS, Ross JJ. Short-term treatment of actinomycosis: two cases and a review. Clin Infect Dis 2004;38:444-7. [DOI] [PubMed] [Google Scholar]


