Summary
Fiberoptic endoscopic evaluation of swallowing (FEES) is now a first choice method for studying swallowing disorders on account of the various advantages it offers: easy to use, very well tolerated, allows bedside examination and is economic. Nevertheless, this diagnostic procedure is not without risks, the most probable consequences of which include discomfort, gagging and/or vomiting, vasovagal syncope, epistaxis, mucosal perforation, adverse reactions to topical anaesthetics and laryngospasm. The risks involved with FEES stress the importance of informing the patient of these; this is an important aspect in medicine that necessarily and immediately implies receiving the patient’s so-called “informed consent”. Informed consent should be obtained not only by means of specific printed forms but also after the patient has had an interview with the physician who will be performing the procedure and who will offer information according to the personal clinical, psychological, cultural and linguistic situation of the patient and in keeping with the type of procedure proposed. In the case of FEES, as with other invasive or non-invasive diagnostic procedures, therefore, routine written and signed consent, together with a patient/physician interview should fulfil what is known as “complete information”. In this report, a specific form for informed consent to FEES procedures, is proposed.
Keywords: Deglutition disorders, Diagnosis, Fiberoptic endoscopic evaluation, Informed consent
Riassunto
La valutazione endoscopica a fibre ottiche della deglutizione (fiberoptic endoscopic evaluation of swallowing - FEES) rappresenta attualmente una metodica di primo impiego nello studio dei disturbi della deglutizione, alla luce dei vantaggi insiti nella metodica stessa e rappresentati da: facilità di esecuzione, elevata tollerabilità, possibilità di bedside examination e costi contenuti. Questa procedura diagnostica però non è priva di rischi; tra le complicanze vanno ricordate fastidio, vomito, sincope vasovagale, epistassi, lesione della mucosa, effetti collaterali degli anestetici locali e laringospasmo. I rischi connessi all’esecuzione della FEES inducono ad affrontare l’importante aspetto dell’informazione del paziente, che rappresenta uno dei cardini della prestazione professionale e che immediatamente e necessariamente, si ripercuote sull’acquisizione del cosiddetto “consenso informato”. L’acquisizione del consenso dovrebbe avvenire non solo attraverso la presentazione di moduli prestampati, ma anche attraverso un colloquio diretto con il medico che esegue l’esame, al fine di giungere ad una informazione personalizzata adeguata alla situazione clinica, psicologica, culturale e linguistica del paziente, e proporzionata alla tipologia della prestazione diagnostica proposta. Anche per la FEES quindi, così come per altre metodiche diagnostiche più o meno invasive, la prassi di un consenso scritto prestampato integrato da un colloquio medico/paziente, può soddisfare quella che oggi viene definita “completezza dell’informazione”. In questo lavoro, proponiamo un modello di dichiarazione di consenso informato, specifico per l’esecuzione della FEES.
Introduction
Dysphagia, a disorder with multifactorial aetiopathogenic features, presents several problems regarding both the definition of the nature of the condition and the classification of specific deficits in the structures and in the various stages of swallowing 1.
In fact, swallowing is a very complex physiological action that is rapid from the beginning to the end and, for this reason, morphological studies on the structures involved and functional evaluation of the action itself present technical problems that are not at all easy to solve 2.
According to the American Speech-Language-Hearing Association (ASHA) 3, a clinical-instrumental evaluation of swallowing should reveal: organic and functional alterations in the structures involved, the degree of efficacy of swallowing in its various stages, adequate protection of the lower airways and co-ordination between breathing and swallowing, and, furthermore, should detect and possibly quantify any penetration of the bolus in the tracheal-bronchial passage.
The diagnostic tools used for studying dysphagia should also be able to assess the various oro-pharyngo-oesophageal movements that take place during swallowing in relationship to the type of bolus administered, as well as evaluate the validity and efficacy of the relative compensation postures and manoeuvres 3.
The instrumental method currently considered the “gold standard” for studying swallowing is videofluoroscopy, which permits real time investigation of all stages during swallowing 4 5. Furthermore, for a clinical definition of dysphagia, other tools may be used: videoendoscopy 6–9, scintigraphy 10, ultrasound, for studying the oral stage 11 12 and pH-manometry, for investigating functional alterations in the oesophagus 13–15.
When performing dynamic studies on swallowing with fluoroscopy, water-soluble boluses of different consistency may be administered; therefore, any penetration into the airways is not a true risk for complications such as bronchial-pulmonary infection 16.
Fiberoptic endoscopic evaluation of swallowing (FEES) is well tolerated and is easy to perform, it is, nevertheless, an endoscopic examination that can result in easily controlled complications such as discomfort, gagging, vomiting, vaso-vagal syncope, anterior or posterior epistaxis or even dramatic, though rare, complications such as laryngospasm 6.
Due to the risk of laryngospasm and inhalation of the bolus, during a FEES procedure, the importance of ‘informed consent’ should not be underestimated. Herewith, the model used, in our Unit, for the declaration of informed consent to the FEES procedure, is proposed.
Fiberoptic endoscopic evaluation of swallowing
FEES has been proposed, in recent years, as a useful supplementary tool for studying swallowing 7 17 . In spite of the fact that this method supplies limited information compared to videofluoroscopy, because it only investigates the pharyngeal stage with a moment of “white-out” in the swallow, it is now employed as a routine procedure 6. In fact, FEES is now a first choice method of investigation in Europe due to the important advantages it offers: easy to use, well tolerated, possibility of bedside examination and less costly 6. Moreover, the relative literature shows that the results obtained with videofluoroscopy and videoendoscopy correlate well in the detection of pathological aspects such as aspiration of the bolus into the airways and the presence of bolus residue in the pharynx and pharyngeal-laryngeal area 7–9.
The advantages and disadvantages of FEES are outlined in Table I.
Table I. Advantages and disadvantages of FEES.
| Advantages | Disadvantages |
| Only slightly invasive | Investigates only pharyngeal stage |
| Easy to perform | Swallowing white-out |
| Possible bedside examination | No quantification of bolus inhaled |
| Can be repeated | |
| Economic | |
| Investigates motor component | |
| Investigates sensory component | |
| Good estimate of stagnation | |
| Penetration of bolus into airways can be seen |
Static and dynamic evaluation of the structures involved during swallowing
Videoendoscopic evaluation of swallowing is performed with a fiberoptic rhinopharyngoscope for studying the physiology and physiopathology of certain stages of swallowing, particularly the pharyngeal stage. This examination offers detailed information of swallowing and of the relative functions of the upper airways and upper digestive tract. Endoscopic assessment of swallowing can also be achieved by testing laryngeal sensitivity; this is accomplished by directly stimulating the various pharyngeal-laryngeal areas with the tip of the rhinopharyngolaryngoscope. This evaluation can be completed by the rhythmic administration of air in a sequence of pressures, to elicit laryngeal adduction and consequently establish the sensitivity threshold (FEESST).
During the FEES examination, compensatory positions may be kept to improve swallowing efficacy and therapeutic manoeuvres can be performed that can help establish the appropriate rehabilitation approach for managing feeding and swallowing techniques. Hence, FEES offers the possibility to study the physiology of swallowing, the evaluation of the presence, degree and type of dysphagia, and is also a good method for establishing the best means of feeding (by mouth, by mouth with dietary restrictions, by tube), for indicating and following appropriate rehabilitation programmes, for advising diets and for planning any other diagnostic investigation 18.
Specific competence is required for performing a FEES examination: in particular, the otorhinolaryngologist and/or phoniatric specialist involved must be familiar with the physiology and physiopathology of swallowing, the principle disorders that cause dysphagia, as well as the manoeuvres, exercises and techniques used in rehabilitation. In addition, the specialist performing FEES must not only be able to manage a subject with swallowing disorders but should also be well trained in the use of flexible endoscopy – especially FEES – in dysphagic patients 19.
Videoendoscopy permits a static and dynamic evaluation of the structures in the upper airways and upper digestive tract. As far as concerns the static investigation, three main positions are recommended for the tip of the endoscope 1 2 20: naso-pharyngeal, upper position and lower position. In the upper position (with the endoscope next to the velum palati), it is possible to detect stagnation of secretion in the glossoepiglottic valleculae, the pyriform recesses, the interarytenoid area and the laryngeal vestibule.
The lower position (the endoscope is placed at the laryngeal aditus) is the most appropriate with which to study laryngeal sphincter function, which can be tested by simply inviting the patient to cough, swallow saliva and carry out a Valsalva manoeuvre 7.
Static evaluation of the morphology and function of the upper airways and upper digestive tract is followed by a dynamic evaluation of swallowing, administering a bolus to the patient. The presence of abundant secretion in the laryngeal vestibule or a non-protective cough can be contraindications to an examination with a bolus.
With patients at high risk of inhaling a bolus, it is advisable to administer a small bolus of water coloured with methylene blue (blue-dyed food), so that it is easier to see any liquid penetrating the lower airways 17. If the test is positive, without triggering protective reflexes, such as coughing, it is better not to continue the dynamic evaluation with boluses of other consistencies. On the other hand, if it is negative, or positive but with an efficacious protective reflex, it is advisable to continue the dynamic test by administering substances of a consistency well tolerated by the patient and with a colour contrasting that of the mucosa (e.g.: milk, yoghurt, jam, jelly, bread, biscuits, etc.).
As far as concerns the use of food dyed with methylene blue, it should not be forgotten that an overdose of this substance can cause serious side-effects (hyper-bilirubinaemia, Heinz body haemolytic anaemia, desquamation of the skin) 21. No consensus guidelines exist regarding the volume of dye to be added to the food; this differs greatly from one clinician to another and the amount of dye added is typically ‘eyeballed’ to the desired shade of blue 22 23.
Some Authors suggest starting the dynamic evaluation with solid food, gradually reducing the consistency of the bolus, since there is less probability of inhaling food of greater consistency 24. Furthermore, liquids administered during the final stage of the evaluation would help to remove any residue of the bolus in the glossoepiglottic valleculae, at the base of the tongue, or in the pyriform recesses, thus decreasing the risk of post-swallowing inhalation 24.
Once the food has been administered, the patient must chew it or disintegrate it in his/her mouth and only swallow it when asked to do so; in this manner, if there is a premature drop of the bolus, it is easily seen. This is frequently associated with penetration of remains of the food in the laryngeal vestibule and in the lower airways (pre-swallowing inhalation). The oro-pharyngeal stage is not visible endoscopically when the swallowing reflex starts, because the endoscope will be in contact with the base of the tongue, with the epiglottis and the bolus itself (swallowing white-out).
During this stage, penetration or inhalation of the food may occur due to incompetence of the glottis (intra-swallowing inhalation). Inhalation should be suspected if there are indirect signs such as coughing or the remains of a bolus in the laryngeal vestibule. If intra-swallowing inhalation is suspected, it is advisable to invite the patient to cough several times because, in certain cases, this may expel the remains of the bolus from the lower airways even a few minutes after the food has passed. At the end of each swallow, it is important to see if and where remains of the bolus are; if these are abundant, they might penetrate the larynx and cause later inhalation (post-swallowing inhalation), possibly when the patient turns his head or when he is speaking.
Therefore, inhalation of the bolus can occur as a consequence of an alteration in any of the swallowing stages, especially if it is associated with reduced efficacy of the cough reflex; this condition is not always suspected when evaluating the case history and, if it presents without symptoms or associated with an inefficient cough, it can only be demonstrated with instrumental investigation (FEES, videofluoroscopy, oro-pharyngo-oesophageal scintigraphy).
Inhalation of a bolus during a FEES procedure is doubly important because not only it is a fundamental element requiring investigation but is also a complication to be feared. Dynamic endoscopic examination with boluses of different consistency not only reveals eventual inhalation but also reveals the efficacy of the various postures and manoeuvres that facilitate swallowing and which are either spontaneous in the patient or acquired after specific rehabilitation therapy.
Nevertheless, it must not be forgotten that inhalation of a bolus is a risk factor for infectious bronchial pneumonia which, in debilitated patients, may considerably compromise their general health conditions and require emergency treatment.
In performing the FEES and FEESST examination, it is necessary to pass the endoscope through the nasal cavity, nasopharynx, and pharynx. On doing this, it is possible, on rare occasions, to encounter adverse effects which may include: discomfort, gagging and/or vomiting, anterior epistaxis, posterior epistaxis, laceration of the mucosa, allergic reactions/hypersensitivity to topical anaesthesia or nasal spray, adverse effect of methylene blue, vasovagal response and laryngospasm 6 10 18 25 26.
Discomfort has been reported as the most frequent adverse effect, but the use of topical anaesthesia may reduce the occurrence, however possibly affecting the swallowing mechanisms 27. Some adverse effects, such as changes in heart rate, epistaxis, laryngospasm, and vasovagal response, may present health risks to the patient; however, studies have shown that these events are infrequent 28. A study on 500 consecutive FEESST assessments in patients with various underlying diagnoses, including stroke and chronic neurological disease, revealed that minor epistaxis with spontaneous cessation of bleeding occurred in 0.6% of the cohort and there was no incidence of laryngospasm or vasovagal responses 29. Similar results were found in 305 outpatients examined in an office setting: airway compromise 0% and epistaxis 1.1% 27. Of the 6000 FEES examinations, Langmore et al. reported 2 incidents of laryngospasm (0.03%), 4 vasovagal episodes (0.06%) and 20 cases of epistaxis (0.3%) 30.
The possible complications arising from FEES are outlined in Table II.
Table II. Complications with FEES.
| Complications |
| Discomfort |
| Gagging and/or vomiting |
| Anterior epistaxis |
| Posterior epistaxis |
| Laceration of mucosa |
| Vasovagal episodes |
| Adverse reactions to topical anaesthetic |
| Adverse effect of methylene blue |
| Laryngospasms |
The overall risk involved in FEES and FEESST is minimal, but it is recommended that clinicians be well trained in the signs and symptoms of adverse reactions and be ready to take appropriate action if these occur 18 31.
Informed consent
Due to the risk of laryngospasm and inhalation of the bolus (as well as other complications), during the FEES procedure, it is necessary to consider the importance of obtaining “informed consent” from the patient; this is a very important aspect in medicine that unavoidably and immediately implies receiving the patient’s consent.
In particular, the problem of “informed consent” for physicians, which is more difficult than it appears and has become one of the main factors that can spoil the relationship between physician and patient, can, in theory, be solved by using a specifically prepared form for the patient to sign: this should contain all the information concerning the reasons for proposing the diagnostic examination or treatment to the patient and, above all, it should provide details of the risks that the patient might encounter 32. However, the professional requirement of reaching a balance between adequately informing the patient of the diagnostic programme he/she will be submitted to and the ethical and moral duty to not worry him/her in an excessive and dangerous way, makes the question of “informed consent” extremely difficult and intricate under the particular circumstances, due to the difference (cultural and psychological) between one patient and another and because of the complexity of their conditions (neurological, surgical, etc.) 32.
Information is, therefore, an indispensable and integrative part of medical assistance, one which patients have a right to. Granting consent implies that the patient becomes aware and that he/she exercises a right to be informed, two conditions that are constitutionally guaranteed and represented by his/her own will 33.
The opinion and conviction currently held is that informed consent is necessary from an operative point of view; but can the patient reach a sufficient degree of awareness, in a short time, that will allow him/her to make the best impartial decision?
This implies that if consent is to be considered valid, it should not only be freely and explicitly manifested, but also expressed by someone who has been adequately informed.
In order to fulfil this requirement – i.e., that consent should be “informed consent” – the characteristics of “correct information” must be respected; this must be specific for each individual, comprehensible, true, objective, complete and not imposed 32 34–36.
It must be stressed that besides the use of printed forms, consent should also include information adequately suited to the patient’s personal health, psychological, cultural and linguistic conditions, as well as being proportionate to the type of examination or treatment proposed 34. Hence, written information must be considered an “integration” and not a “substitute” for a physician/patient interview and it is strongly recommended that this informed consent be acquired personally by the specialist who will be performing the examination or treatment. In effect, an expert physician with a proficient “bedside manner” should be able to interpret what the individual patient needs to know and relate with him/her by offering the type of information accordingly 32.
In our opinion, information is adequately fulfilled when it is offered taking into consideration the disease and the relative clinical conditions of the patient with that disease, and when the information takes into account the general and specific risks related to the disease and the examination or treatment proposed. In this way, together with a printed form providing details of all the possible complications that might occur during the examination or treatment (stressing not only the difference between those most frequently encountered and the less serious types, but also the complications that are less frequent, or even rare, but are more serious), consent should also be “oral” and based on “correct information”.
A proposal for informed consent for FEES
The physician has an ethical responsibility to obtain the patient’s consent prior to any treatment or procedure, as outlined in the ASHA Code of Ethics 37. Legislation and regulations governing the conditions under which informed consent is required, vary from one country to another. In our opinion, informed consent for FEES procedures is fundamental since this endoscopic examination should not be considered a mere diagnostic investigation implying implicit consent (not written, therefore), but rather a diagnostic procedure during which complications may occur, some more frequent and with limited medical consequences (anterior epistaxis), and others that may be uncommon or even rare but which become medical or surgical emergencies (inhalation of the bolus with acute obstruction of the airways, spasm of the glottis).
Hence, also in the case of examinations using FEES, the routine step of obtaining written consent, on a printed form, together with an interview between physician and patient can fulfil what is known, today, as “complete information” 32 38.
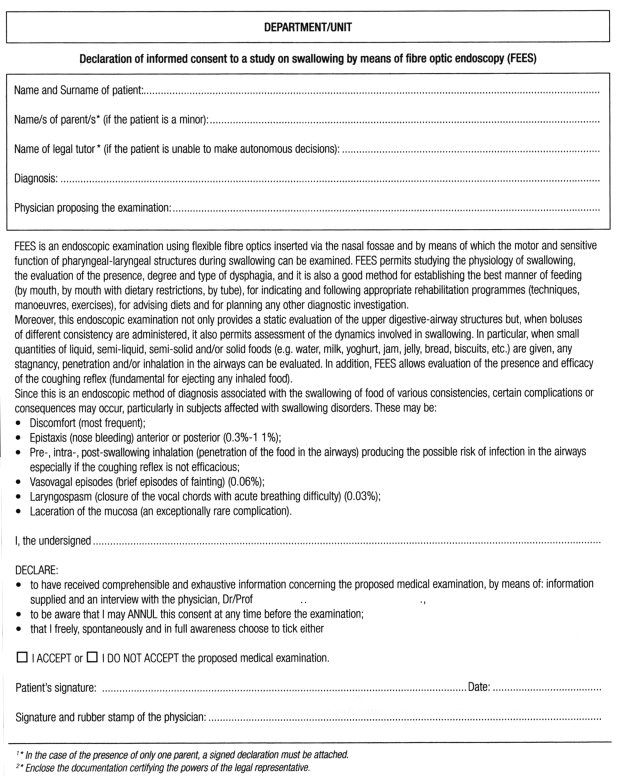
In this report, a form is proposed for declaring informed consent, specifically for FEES procedures, in our Unit (Fig. 1).
Fig. 1.
Specific form for informed consent to FEES procedures.
The first part concerns the patient’s identification, names of the parents (required when the patient is a minor) and of the legal tutor (required when the patient lacks, either partly or completely, power of decision). If only one of the parents is present, a signed declaration, in this respect, is to be attached whereas, in the case of a patient who is not self-sufficient, documentation certifying the legal tutor’s powers must be attached.
In this section, a space for details of the patient’s health has also been included (to be filled in by the physician), where a brief description of the patient’s clinical situation will be included under the heading “Diagnosis” (e.g. dysphagia in a patient with amyotrophic lateral sclerosis (ALS), dysphagia in a patient with ischaemic encephalopathy, post-surgical swallowing disorder, etc.), plus details concerning the physician who proposes the examination (general practitioner, specialist in otorhinolaryngology, phoniatrics, neurology, neurosurgery, etc.).
In the second part of the form, a brief description is given of the diagnostic procedure (FEES), of its usefulness and the various complications that may be encountered, indicating also their frequency.
In the third and last section (to be filled in by the patient), the patient expresses his/her will to consent to the procedure; here, the patient declares having received a comprehensible and exhaustive description of the proposed medical procedure by means not only of printed information, but also an interview with the physician (this part will include details of the physician who has informed the patient), of being aware that he/she can withdraw consent, at any time prior to the start of the procedure, and that he/she freely, spontaneously and in full awareness accepts/does not accept to be submitted to the proposed medical procedure.
The patient’s signature, with the date, will be placed at the end of the declaration of consent to the FEES procedure, together with the signature (with date of signature) and rubber stamp of the physician receiving the consent and who has, in the interview, informed the patient.
Conclusions
FEES allows the clinician to identify the physiology of swallowing, to determine the safest and least restrictive level of oral intake, to include appropriate compensatory techniques, and to establish a dysphagia rehabilitation programme. On account of the risks involved with FEES, it is necessary to be aware of the importance of informing the patient of these possibilities; this is an important aspect in medicine that un-avoidably implies receiving the patient’s so-called “informed consent”. In the case of FEES, therefore, as with other invasive or non-invasive diagnostic procedures, a routine written and signed consent together with a patient/physician interview should fulfil what is known as “complete information”. In this report, a form is proposed for the declaration of informed consent, specifically drawn up for FEES procedures.
References
- 1.Tesei F, Caliceti G, Brusoni S, Gavelli GP, Mattioli S, Rinaldi Ceroni A. Lo studio endoscopico e per “imaging” della deglutizione. In: Piemonte M. Fisiopatologia della deglutizione. XIV Giornate Italiane di Otoneurologia. Manifestazione Ufficiale dell’AOOI: Senigallia, 18 aprile 1997. p. 87-107. [Google Scholar]
- 2.Schindler O, Ruoppolo G, Schindler A. Deglutologia. Torino: Omega Edizioni; 2001. [Google Scholar]
- 3.American Speech Language Hearing Association. Special interest division 13. Atlanta, GA. Swallowing and swallowing disorders. 1998. [Google Scholar]
- 4.Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin North Am 1988;21:613-22. [PubMed] [Google Scholar]
- 5.Logemann JA. Dysphagia: evaluation and treatment. Folia Phoniatr Logop 1995;47:140-64. [DOI] [PubMed] [Google Scholar]
- 6.Aviv JE, Kaplan ST, Thomson E, Spitzner J, Diamond B, Close LG. The safety of flexible endoscopic evaluation of swallowing with sensory testing (FEESST): an analysis of 500 consecutive evaluations. Dysphagia 2000;15:39-44. [DOI] [PubMed] [Google Scholar]
- 7.Bastian RW. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg 1991;104:339-50. [DOI] [PubMed] [Google Scholar]
- 8.Langmore SE, Schatz K, Olsen N. Endoscopic and video-fluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 1991;100:678-81. [DOI] [PubMed] [Google Scholar]
- 9.Kidder TM, Langmore SE, Martin BJW. Indications and techniques of endoscopy in evaluation of cervical dysphagia: comparison with radiographic techniques. Dysphagia 1994;9:256-61. [DOI] [PubMed] [Google Scholar]
- 10.Fattori B, Grosso M, Bongioanni P, Nacci A, Cristofani R, AlSharif A, et al. Assessment of swallowing by oro-pharyngo-esophageal scintigraphy in patients with amyotrophic lateral sclerosis. Dysphagia 2006;21:280-6. [DOI] [PubMed] [Google Scholar]
- 11.Fanucci A, Cerro P, Ietto F, Brancaleone C, Berardi F. Physiology of oral swallowing studied by ultrasonography. Dentomaxillofac Rad 1994;23:221-5. [DOI] [PubMed] [Google Scholar]
- 12.Watkin KL. Ultrasound and swallowing. Folia Phoniatr Logop 1999;51:183-98. [DOI] [PubMed] [Google Scholar]
- 13.Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, et al. Timing of videofluoroscopic, manometric events and bolus transit during the oral and the pharyngeal phases of swallowing. Dysphagia 1989;4:8-15. [DOI] [PubMed] [Google Scholar]
- 14.Castell JA, Castell DO. Modern solid state computerized manometry of the pharyngoesophageal segment. Dysphagia 1993;8:270-5. [DOI] [PubMed] [Google Scholar]
- 15.Périé S, Laccoureye L, Flahault A, Hazebroucq V, Chaussade S, St Guily JL. Role of videoendoscopy in assessment of pharyngeal function in oropharyngeal dysphagia: comparison with video-fluoroscopy and manometry. Laryngoscope 1998;108:1712-6. [DOI] [PubMed] [Google Scholar]
- 16.Morcos SK. Effects of radiographic contrast media on the lung. Review article. Br J Radiol 2003;76:290-5. [DOI] [PubMed] [Google Scholar]
- 17.Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia 1988;2:216-9. [DOI] [PubMed] [Google Scholar]
- 18.American Speech-Language-Hearing Association. Special interest division 13. Atlanta, GA. Role of the speech-language pathologist in the performance and interpretation of endoscopic evaluation of swallowing: Guidelines. 2004. [Google Scholar]
- 19.Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope 2003;113:1386-93. [DOI] [PubMed] [Google Scholar]
- 20.Bastian RW. Contemporary diagnosis of dysphagic patient. Otolaryngol Clin North Am 1998;31:489-506. [DOI] [PubMed] [Google Scholar]
- 21.Sills MR, Zinkham WH. Methylene blue-induced Heinz body haemolytic anaemia. Arch Paediatr Adolesc Med 1994;148:306-10. [DOI] [PubMed] [Google Scholar]
- 22.Leder SB, Acton LM, Lisitano HL, Murray JT. Fiberoptic endoscopic evaluation of swallowing (FEES) with and without blue-dyed food. Dysphagia 2005;20:157-62. [DOI] [PubMed] [Google Scholar]
- 23.Maloney JP, Ryan TA. Detection of aspiration in enterally fed patients: a requiem for bedside monitors of aspiration. J Parenter Enteral Nutr 2002;26(Suppl):S34-41. [DOI] [PubMed] [Google Scholar]
- 24.Spiegel JR, Selber JC, Creed J. A functional diagnosis of dysphagia using videoendoscopy. Ear Nose Throat J 1998;77:628-32. [PubMed] [Google Scholar]
- 25.Wu CH, Hsiao TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope 1997;107:396-401. [DOI] [PubMed] [Google Scholar]
- 26.Benjamin S. An endoscopic guide to hypopharynx. Washington, DC: Gastroenterology Treatment Updates by Medscape Education Collaborative 1999. [Google Scholar]
- 27.Cohen MA, Setzen M, Perlman PW, Ditkoff M, Mattucci KF, Guss J. The safety of flexible endoscopic evaluation of swallowing with sensory testing in an outpatient otolaryngology setting. Laryngoscope 2003;113:21-4. [DOI] [PubMed] [Google Scholar]
- 28.Langmore SE, McCulloch TM. Examination of the pharynx and larynx and endoscopic examination of pharyngeal swallowing. In: Perlman AL, Schulze-Delrieu K, editors. Deglutition and its disorders. San Diego: Singular Publishing Group, 1997. p. 201-26. [Google Scholar]
- 29.Aviv JE, Kaplan ST, Thomson JE, Spitzer J, Diamond B, Close LG. The safety of flexible endoscopic evaluation of swallowing with sensory testing (FEESST): an analysis of 500 consecutive evaluations. Dysphagia 2000;15:39-44. [DOI] [PubMed] [Google Scholar]
- 30.Langmore SE, Pelletier C, Nelson R. Results of FEES survey on safety of endoscopy for swallowing assessment. Presented at Fourth Annual Meeting of the Dysphagia Research Society, McLean, VA, October 28, 1995. [Google Scholar]
- 31.Watterson TL, McFarlane SC, Brophy JW. Some issues and ethics in oral and nasal videoendoscopy. Semin Speech Lang 1990;11:1-7. [Google Scholar]
- 32.Fiori A. Il consenso informato. In: Medicina legale della responsabilità medica. Milano: Giuffrè Ed; 1999. [Google Scholar]
- 33.Mallardi V. The origin of informed consent. Acta Otorhinolaryngol Ital 2005;25:312-27. [PubMed] [Google Scholar]
- 34.Progetto Risk Management. Proposta di linee di indirizzo per la gestione del consenso informato. Agenzia Regionale per i Servizi Sanitari Regione Piemonte. 12 aprile 2006.
- 35.Motta G, Motta S. La perizia medico-legale. Acta Otorhinolaryngol Ital 2004;23:239-49. [PubMed] [Google Scholar]
- 36.Motta G, Salerno G. Problemi etici nel consenso informato. In: Cenacchi V, editor. Il consenso informato in otorinolaringoiatria. Atti del Convegno sul “Consenso Informato in Otorinolaringoiatria”. Bologna: Ottobre 1996. Bologna: Ed CLUEB. 1998. [Google Scholar]
- 37.American Speech-Language-Hearing Association. Code of ethics (revised). ASHA 2003;23(Suppl):S13-S15. [Google Scholar]
- 38.Edwards SJ, Lilford RJ, Thornton J. Informed consent for clinical trials: in search of the “best” method. Soc Sci Med 1998;47:1825-40. [DOI] [PubMed] [Google Scholar]