Abstract
Aims
Clinical outcomes of patients with chronic heart failure (CHF) have improved, but evidence-based treatment appears to be imbalanced depending on patients' and physicians' gender. We aimed to determine the interactions of gender with medical treatment of CHF.
Methods and results
Consecutive patients with CHF (n = 1857) were evaluated regarding co-morbidities, New York Heart Association classification, current medical treatment, and dosage of angiotensin-converting enzyme-inhibitors (ACE-Is) and beta-blockers. Gender of patients and treating physicians was recorded. Baseline characteristics of patients and physicians were comparable for males and females. Female patients were less frequently treated with ACE-Is, angiotensin-receptor blockers, or beta-blockers. Achieved doses were lower in female compared with male patients. Guideline-recommended drug use and achieved target doses tended to be higher in patients treated by female physicians. There was no different treatment for male or female patients by female physicians, whereas male physicians used significantly less medication and lower doses in female patients. In multivariable analysis, female gender of physicians was an independent predictor of use of beta-blockers.
Conclusion
Treatment of CHF is influenced by patients', but also physicians' gender with regard to evidenced-based drugs and their dosage. Physicians should be aware of this problem in order to avoid gender-related treatment imbalances.
Keywords: Gender, Chronic heart failure, ACE inhibitor, Angiotensin antagonist
Introduction
Chronic heart failure (CHF) imposes an increasing burden to healthcare systems, with a rising prevalence, especially in the ageing populations of Western industrialized countries.1 Clinical outcomes of patients with CHF have improved in recent years, but use of evidence-based treatments appears to be imbalanced according to the gender of the patient. In female patients, a decreased use of coronary angiograms and implantation of cardiac devices such as implantable cardioverter defibrillators or biventricular pacemakers has been reported.2–4 Gender-related differences in medical treatment of CHF could influence survival of male compared with female patients.5 The gender of the treating physician, as well as the interaction of patients' and physicians' gender, could be important factors in optimal medical treatment. Perception and interpretation of clinical symptoms, and also ambitions of skill enhancement and knowledge about latest guidelines, might be different in male and female physicians. In addition, time available for education is likely to be different according to gender-related responsibilities such as supporting family, for example. Thus, we hypothesize that physicians' gender plays an important role in guideline adherence of drug treatment for CHF.
Methods
Study population
Consecutive patients (n = 1857) with CHF were evaluated between March and November 2006 in centres in eastern Germany; all patients were included in an observational cross-sectional trial evaluating drug treatment of CHF. Baseline data, which included co-morbidities, New York Heart Association (NYHA) classification, current medical treatment, and vital parameters, were documented by 829 physicians (65.3% general practitioners, 27.6% internists, 7.1% cardiologists). Data were analysed with regard to evidence-based drug treatments to improve survival, such as ACE-inhibitors (ACE-Is), angiotensin-receptor blockers (ARBs), and beta-blockers. Dosages of ACE-I and beta-blockers were calculated as a percentage of the guideline-recommended doses for the treatment of CHF.6 Physicians' gender, age, and some professional details were also documented. The investigation conforms with the principles outlined in the Declaration of Helsinki and national medical law.7
Statistical analysis
All data are expressed as mean ± SD. Statistical significance was assumed at a P-level <0.05. Inter-group differences were assessed with the two-sided Pearson χ2 test for categorical and the Student's t-test for continuous variables with SPSS 15.0®. A multivariable linear analysis was performed to determine the association between patients' and physicians' gender (independent variables) and use of ACE-I and beta-blockers as the dependent variable. Possible confounders included in the model were hypertension, coronary heart disease, NYHA classification, current use of either ACE-I/ARB or beta-blockers, and specialization of physicians as categorical and age of patients, time since medical board examination, and left ventricular ejection fraction as continuous variables. Renal insufficiency was added as a confounder in the analysis with ACE-I/ARB as the dependent variable; current chronic obstructive pulmonary disease was added as a confounder in the analysis with beta-blockers as the dependent variable. The interaction of patients' and physicians' gender was applied to the statistical model to account for any possible influences. Patients with missing values were not included in the statistical analysis.
Results
Baseline characteristics of patients are shown in Table 1. There was no gender-related difference in specialization of physicians (63.2% male vs. 68.0% female general practitioners, n.s.; 29.0% male vs. 25.7% female internists, n.s.; 7.8% male vs. 6.2% female cardiologists, n.s.). Duration since medical board examination was comparable for both genders (male 23.9 ± 9.1 years and female 23.5 ± 8.8 years, n.s.).
Table 1.
Baseline characteristics
| Total | Male patient | Female patient | P | Patients treated by male physician | Patients treated by female physician | P | |
|---|---|---|---|---|---|---|---|
| Number | 1857 (100%) | 52.6% | 47.4% | 63.3% | 36.7% | ||
| Age | 68.1 ± 10.6 | 66.5 ± 9.8 | 69.9 ± 11.1 | 0.001 | 68.0 ± 10.4 | 68.7 ± 10.6 | n.s. |
| LVEF (%) | 48.8 ± 12.6 | 48.5 ± 11.9 | 49.2 ± 13.4 | n.s. | 47.7 ± 12.1 | 50.3 ± 13.0 | 0.013 |
| RRsys (mmHg) | 150.8 ± 18.2 | 150.9 ± 18.9 | 150.8 ± 17.2 | n.s. | 150.5 ± 18.3 | 151.2 ± 18.1 | n.s. |
| RRdias (mmHg) | 88.0 ± 10.6 | 88.0 ± 10.5 | 87.9 ± 10.7 | n.s. | 88.1 ± 10.7 | 87.4 ± 10.6 | n.s. |
| Heart rate (b.p.m.) | 77.9 ± 10.9 | 78.3 ± 11.2 | 77.5 ± 10.4 | n.s. | 77.9 ± 11.0 | 77.9 ± 10.7 | n.s. |
| Hypertension (%) | 83.2 | 82.1 | 84.4 | n.s. | 80.7 | 86.6 | 0.001 |
| CAD (%) | 45.5 | 49.4 | 41.1 | 0.001 | 44.1 | 48.9 | n.s. |
| TIA/stroke (%) | 7.0 | 7.3 | 6.7 | n.s. | 6.2 | 7.9 | n.s. |
| Diabetes (%) | 33.1 | 33.1 | 33.1 | n.s. | 32.5 | 34.2 | n.s. |
| HLP (%) | 58.3 | 60.1 | 56.4 | n.s. | 56.8 | 60.6 | n.s. |
| NYHA (%) | |||||||
| I | 7.1 | 5.5 | 8.8 | 6.4 | 7.8 | ||
| II | 72.4 | 73.7 | 71.1 | 72.8 | 70.5 | ||
| III | 19.6 | 19.8 | 19.4 | n.s. | 19.8 | 20.9 | n.s. |
| IV | 0.9 | 1.0 | 0.7 | 1.0 | 0.8 | ||
Baseline characteristics of female and male patients as well as patients treated by a female or male physician. LVEF, left ventricular ejection fraction; CAD, coronary artery disease; HLP, hyperlipoproteinaemia.
Treatment with an ACE-I or ARB was present in 80.4% of the patients (72.5% ACE-I, 4.3% ARB, 3.6% ACE-I + ARB), whereas treatment with beta-blockers was documented in 69.9% of the patients. Usage of ACE-Is or ARBs was significantly higher in male compared with female patients (P = 0.021), and recommended dosages also tended to be higher in male patients (P = 0.058). There was no difference in use or dosage in patients treated by a male or female physician (n.s.). Male patients tended to receive more beta-blockers (P = 0.075) with significantly higher doses (P = 0.021), compared with female patients. There was no difference in dosing between the genders of treating physicians. Use of beta-blockers tended to be higher in patients treated by a female physician (P = 0.054).
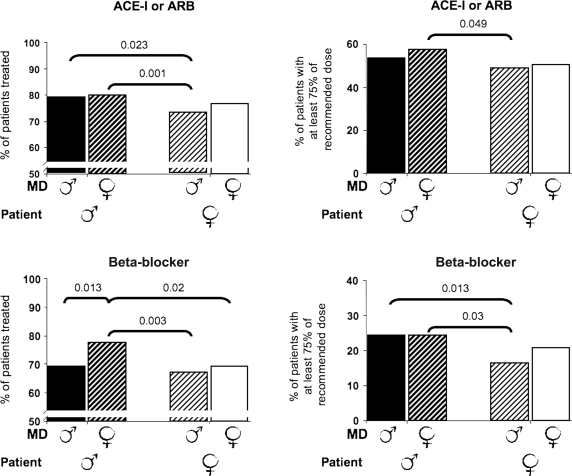
Treatment and dosing of ACE-Is/ARBs and beta-blockers related to patients' and physicians' gender are presented in Figure 1. The use of ACE-Is or ARBs was significantly lower in female patients treated by a male physician compared with male patients treated by either a female or male physician. Dosage of ACE-Is or ARBs was highest in male patients treated by a female physician and was significantly different from the reverse gender combination (female patients–male physician). Beta-blocker use was highest in male patients treated by a female physician, compared with other possible combinations. Dosage of beta-blockers was comparable in male patients irrespective of physicians' gender, whereas female patients treated by a male physician received lowest doses.
Figure 1.
Gender-specific treatment of chronic heart failure. Left, differences in use of angiotensin-converting enzyme-inhibitors (ACE-Is)/angiotensin-receptor blockers (upper left panel) or beta-blockers (lower left panel) according to the gender of patient and physician. Right: percentage of patients receiving at least 75% of recommended dose of ACE-Is (upper right panel) or beta-blockers (lower right panel) according to the gender of patient and physician. MD, medical doctor.
Multivariable linear analysis adjusted for gender of patients and physicians, age of patients, time since medical board examination, physicians specialization, ejection fraction, NYHA classification, hypertension, coronary heart disease, renal insufficiency, chronic obstructive pulmonary disease as well as the interaction of patients' and physicians' gender, and either current use of ACE-I/ARBs or beta-blockers revealed physicians' gender as well as the interaction of physicians' and patients' gender as an independent predictor in patients with CHF for receiving a beta-blocker (Table 2). Use of ACE-Is or ARBs was not dependent on physicians' gender in multivariable analysis (95% confidence interval −0.174 to 0.225, P = 0.802).
Table 2.
Independent risk factors for drug treatment of chronic heart failure
| Estimate | 95% CI | P | |
|---|---|---|---|
| Ejection fraction | 0.006 | 0.003–0.009 | <0.001 |
| Use of ACE-I | 0.124 | 0.034 to −0.214 | 0.007 |
| Physicians' gender | −0.310 | −0.521 to −0.100 | 0.004 |
| Patients' gender | −0.220 | −0.426–0.013 | 0.037 |
| Interaction: patients' and physicians' gender | 0.166 | 0.645–1.538 | 0.016 |
| COPD | 0.132 | 0.024–0.240 | 0.017 |
| Age (patient) | 0.001 | −0.004–0.003 | 0.931 |
| Speciality | 0.003 | −0.042–0.048 | 0.894 |
| Duration since medical board examination | 0.002 | −0.002–0.005 | 0.394 |
| Hypertension | 0.033 | −0.058–0.124 | 0.477 |
| Coronary heart disease | −0.048 | −0.119–024 | 0.195 |
| NYHA classification | 0.015 | −0.024–0.054 | 0.446 |
Multivariable regression analysis was performed to determine association of patients' and physicians' gender (independent variables) and use of ACE-I and beta-blockers as the dependent variable. Possible confounders were included in the model: hypertension, coronary heart disease, NYHA classification, current use of either ACE-I/ARB or beta-blockers, renal insufficiency, current chronic obstructive pulmonary diseases as well as the interaction of patients' and physicians' gender and specialization of physicians as categorical and age of patient, time since medical board examination and left ventricular ejection fraction as continuous variables. COPD, chronic obstructive pulmonary disease. Prescription of beta-blockers.
Discussion
The outcome of patients with CHF has improved over the last two decades in parallel with the increased use of evidenced-based medical treatment with ACE-Is, ARBs, and beta-blockers.8–11 The results of the present study demonstrate good medical treatment of patients with CHF, compared with previous registries in heart failure populations.12,13 About 80% of the patients received an ACE-I or ARB, and 2–5% a combination thereof. Almost 70% of the patients were treated with a beta-blocker, which is higher than in some previous studies, but comparable with the most recent heart failure trials.14–16 Although adherence to guidelines is an important predictor of outcome in CHF, the actual dosages of ACE-Is or beta-blockers used has a major impact on mortality and morbidity of patients.13,17 Relatively high doses, as derived from clinical trials of ACE-Is/ARBs and beta-blockers, are recommended.18 The results of the present study demonstrate underutilization of evidence-based drug treatment, with only half of the patients being treated with sufficient doses of an ACE-I and only every fourth patient being treated with the recommended dose of a beta-blocker.
Male patients with CHF are more likely to receive evidence-based drug treatment than females. This result was significant for prescription of ACE-Is and dosage of beta-blockers. This finding is in line with the results of previous studies, e.g. in patients with myocardial infarction, showing different drug treatments according to patients' gender.3 In female patients, symptoms of coronary heart disease were significantly more often misinterpreted than in male patients. One reason for this could be a physician-related shift of symptoms from organic to psychogenic origin, especially when symptoms are dependent on psychologically stressful situations.19 Interestingly, underutilization of cardiovascular drugs in female patients with CHF is not suggested to influence clinical outcome, which might be explained by a generally lower risk of fatal or non-fatal outcome in women.20,21
Similar to patients' gender, physicians' gender was also shown to influence drug treatment in patients with heart failure. The present study demonstrated for the first time that drug treatment is more complete when female physicians are taking care of the patients. Female physicians did not treat male or female patients differently with regard to the use and the dosage of ACE-Is or ARBs. Use of beta-blockers was more frequent in male than in female patients, but dosage was not different. In contrast, male physicians favoured male patients for both prescription and dosage. A female patient was likely to receive the worst medical treatment from a male physician, whereas male patients were best treated by a female physician. In multivariable analysis adjusted for co-morbidities, but also possible physician's confounders such as time since medical board examination, female gender of physicians was an independent predictor of use of beta-blockers.
Previous studies have shown that female physicians emphasize patients' needs and opinion and encourage questions and cooperation from their patients more effectively than male physicians.22 Female physicians are more likely to talk about psychosocial issues and probably conduct a more detailed analysis of the patients' condition, which could potentially improve drug treatment, although interestingly time spent with patients is comparable for male and female physicians.23,24 In addition, female physicians are more likely to work part-time due to family commitments; part-time workers have been shown to be more productive per time unit and to achieve better patient satisfaction.25 Thus, evaluation of clinical symptoms and consecutive adjustment of medical treatment might be superior in patients treated by a female physician due to the different social communication styles. In addition, female physicians have been reported to be more satisfied with their patient relationships.26
Strengths and limitations
There was no difference with regard to specialism or duration since medical board examination in univariate analysis between female and male physicians confounding the presented results. Moreover, baseline characteristics of patients were comparable between those treated by a female or male physician, particularly with respect to heart failure symptoms and co-morbidities. Thus, a selection bias of patients' distribution is not likely and could be excluded in the multivariable analysis. However, the number of patients with hypertension was higher in the group treated by female physicians. This might have had an influence on drug treatment in the univariate analysis. Hypertension was included in the multivariate model as a possible confounder, thus without effects on multivariate results.
Guideline-recommended treatment in this study was for chronic systolic heart failure. However, some of our patients may have had diastolic heart failure, especially in view of the high prevalence of hypertension. However, echocardiographic data on mitral flow and E/A or E/E' ratio were not available, thus the presence of diastolic heart failure could not be established. In addition, there is currently no consensus about the definition of preserved left ventricular function, which further frustrates the diagnosis of diastolic heart failure. In univariate analysis of the data presented, unknown diastolic heart failure might have influenced the medical treatment decisions of the physicians. However, this limitation is only likely to have played a minor role, because distribution of patients with diastolic heart failure is likely to be comparable within all of the subgroups analysed. Moreover, in the multivariate analysis, left ventricular ejection fraction was included as a confounding variable, thus it is suggested that the results are independent of diastolic heart failure.
This study was conducted in Germany, thus results cannot be transferred to other countries and other healthcare systems. Moreover, the trial was conducted within an observational survey of evidence-based treatment of heart failure. Thus, physicians taking part in the study may be more likely to treat their patients according to recent guidelines; hence results may overestimate the overall treatment of patients. This limitation also applies to patient selection, which was up to the treating physician. However, these confounders are not likely to have had a major influence on the results, in view of the high number of physicians taking part.
Conclusions
The intensity of guideline-recommended treatment of CHF is influenced by physicians' and patients' gender. Physicians should be aware of this problem in order to avoid bias in the treatment of these patients. Further studies are required to provide a detailed explanation of this phenomenon.
Conflict of interest: M.B. and M.B. received grants for clinical trials from AWD Pharma, Germany, not influencing analysis and interpretation of data. U.M. is an employee of AWD Pharma, Germany responsible for collecting the data. U.W. critically revised the manuscript not influencing data analysis or interpretation.
Funding
The study was conducted and supported by AWD Pharma, Germany. The sponsor had no role in data collection, analysis, interpretation, and writing of the manuscript.
References
- 1.Remme WJ, Swedberg K. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J. 2001;22:1527–1560. doi: 10.1053/euhj.2001.2783. [DOI] [PubMed] [Google Scholar]
- 2.Rathore SS, Chen J, Wang Y, Radford MJ, Vaccarino V, Krumholz HM. Sex differences in cardiac catheterization: the role of physician gender. JAMA. 2001;286:2849–2856. doi: 10.1001/jama.286.22.2849. [DOI] [PubMed] [Google Scholar]
- 3.Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Kimata T, Uemura K. Impact of gender on in-hospital mortality of patients with acute myocardial infarction undergoing percutaneous coronary intervention: an evaluation of the TAMIS-II data. Intern Med (Tokyo, Japan) 2007;46:363–366. doi: 10.2169/internalmedicine.46.6137. [DOI] [PubMed] [Google Scholar]
- 4.El-Chami MF, Hanna IR, Bush H, Langberg JJ. Impact of race and gender on cardiac device implantations. Heart Rhythm. 2007;4:1420–1426. doi: 10.1016/j.hrthm.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 5.Sheppard R, Behlouli H, Richard H, Pilote L. Effect of gender on treatment, resource utilization, and outcomes in congestive heart failure in Quebec, Canada. Am J Cardiol. 2005;95:955–959. doi: 10.1016/j.amjcard.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 6.Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich A, Hoes A, Jaarsma T, Korewicki J, Lévy S, Linde C, Lopez-Sendon JL, Nieminen MS, Piérard L, Remme WJ Task Force for the Diagnosis Treatment of Chronic Heart Failure of the European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26:1115–1140. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 7.Rickham PP. Human experimentation. Code of Ethics of the World Medical Association. Declaration of Helsinki. Br Med J. 1964;2:177. doi: 10.1136/bmj.2.5402.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heidenreich PA, Lee TT, Massie BM. Effect of beta-blockade on mortality in patients with heart failure: a meta-analysis of randomized clinical trials. J Am Coll Cardiol. 1997;30:27–34. doi: 10.1016/s0735-1097(97)00104-6. [DOI] [PubMed] [Google Scholar]
- 9.Pfeffer MA, Braunwald E, Moyé LA, Basta L, Brown EJ, Jr, Cuddy TE, Davis BR, Geltman EM, Goldman S, Flaker GC. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the Survival and Ventricular Enlargement Trial. The SAVE Investigators. N Engl J Med. 1992;327:669–677. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- 10.Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med. 1987;316:1429–1435. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 11.Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF) Lancet. 1999;353:2001–2007. [PubMed] [Google Scholar]
- 12.Cleland JG, Cohen-Solal A, Aguilar JC, Dietz R, Eastaugh J, Follath F, Freemantle N, Gavazzi A, van Gilst WH, Hobbs FD, Korewicki J, Madeira HC, Preda I, Swedberg K, Widimsky J IMPROVEMENT of Heart Failure Programme Committees Investigators. Improvement programme in evaluation and management; Study Group on Diagnosis of the Working Group on Heart Failure of The European Society of Cardiology. Management of heart failure in primary care (the IMPROVEMENT of Heart Failure Programme): an international survey. Lancet. 2002;360:1631–1639. doi: 10.1016/s0140-6736(02)11601-1. [DOI] [PubMed] [Google Scholar]
- 13.Komajda M, Lapuerta P, Hermans N, Gonzalez-Juanatey JR, van Veldhuisen DJ, Erdmann E, Tavazzi L, Poole-Wilson P, Le Pen C. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. Eur Heart J. 2005;26:1653–1659. doi: 10.1093/eurheartj/ehi251. [DOI] [PubMed] [Google Scholar]
- 14.Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, Yusuf S, Pocock S CHARM Investigators Committees. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362:759–766. doi: 10.1016/s0140-6736(03)14282-1. [DOI] [PubMed] [Google Scholar]
- 15.Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–1675. doi: 10.1056/NEJMoa010713. [DOI] [PubMed] [Google Scholar]
- 16.Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JG, Cornel JH, Dunselman P, Fonseca C, Goudev A, Grande P, Gullestad L, Hjalmarson A, Hradec J, Jánosi A, Kamenský G, Komajda M, Korewicki J, Kuusi T, Mach F, Mareev V, McMurray JJ, Ranjith N, Schaufelberger M, Vanhaecke J, van Veldhuisen DJ, Waagstein F, Wedel H, Wikstrand J CORONA Group. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357:2248–2261. doi: 10.1056/NEJMoa0706201. [DOI] [PubMed] [Google Scholar]
- 17.Lenzen MJ, Boersma E, Reimer WJ, Balk AH, Komajda M, Swedberg K, Follath F, Jimenez-Navarro M, Simoons ML, Cleland JG. Under-utilization of evidence-based drug treatment in patients with heart failure is only partially explained by dissimilarity to patients enrolled in landmark trials: a report from the Euro Heart Survey on Heart Failure. Eur Heart J. 2005;26:2706–2713. doi: 10.1093/eurheartj/ehi499. [DOI] [PubMed] [Google Scholar]
- 18.Dobre D, van Veldhuisen DJ, Mordenti G, Vintila M, Haaijer-Ruskamp FM, Coats AJ, Poole-Wilson PA, Flather MD SENIORS Investigators. Tolerability and dose-related effects of nebivolol in elderly patients with heart failure: data from the Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure (SENIORS) trial. Am Heart J. 2007;154:109–115. doi: 10.1016/j.ahj.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 19.Chiaramonte GR, Friend R. Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychol. 2006;25:255–266. doi: 10.1037/0278-6133.25.3.255. [DOI] [PubMed] [Google Scholar]
- 20.Hudson M, Rahme E, Behlouli H, Sheppard R, Pilote L. Sex differences in the effectiveness of angiotensin receptor blockers and angiotensin converting enzyme inhibitors in patients with congestive heart failure—a population study. Eur J Heart Fail. 2007;9:602–609. doi: 10.1016/j.ejheart.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 21.O'Meara E, Clayton T, McEntegart MB, McMurray JJ, Piña IL, Granger CB, Ostergren J, Michelson EL, Solomon SD, Pocock S, Yusuf S, Swedberg K, Pfeffer MA CHARM Investigators. Sex differences in clinical characteristics and prognosis in a broad spectrum of patients with heart failure: results of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation. 2007;115:3111–3120. doi: 10.1161/CIRCULATIONAHA.106.673442. [DOI] [PubMed] [Google Scholar]
- 22.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 23.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995;33:1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Bertakis KD, Franks P, Azari R. Effects of physician gender on patient satisfaction. J Am Med Wom Assoc. 2003;58:69–75. [PubMed] [Google Scholar]
- 25.Parkerton PH, Wagner EH, Smith DG, Straley HL. Effect of part-time practice on patient outcomes. J Gen Intern Med. 2003;18:717–724. doi: 10.1046/j.1525-1497.2003.20401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians results from the physician work life study. The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15:372–380. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]