Abstract
A MESSAGE FROM ASCO'S PRESIDENT
Nearly 40 years ago, President Richard Nixon signed the National Cancer Act, mobilizing the country's resources to make the “conquest of cancer a national crusade.” That declaration led to a major investment in cancer research that has significantly improved cancer prevention, treatment, and survival. As a result, two thirds of people diagnosed with cancer today will live at least 5 years after diagnosis, compared with just half in the 1970s. In addition, there are now more than 12 million cancer survivors in the United States—up from 3 million in 1971.
Scientifically, we have never been in a better position to advance cancer treatment. Basic scientific research, fueled in recent years by the tools of molecular biology, has generated unprecedented knowledge of cancer development. We now understand many of the cellular pathways that can lead to cancer. We have learned how to develop drugs that block those pathways; increasingly, we know how to personalize therapy to the unique genetics of the tumor and the patient.
Yet in 2008, 1.4 million people in the United States will still be diagnosed with cancer, and more than half a million will die as a result of the disease. Some cancers remain stubbornly resistant to treatment, whereas others cannot be detected until they are in their advanced, less curable stages. Biologically, the cancer cell is notoriously wily; each time we throw an obstacle in its path, it finds an alternate route that must then be blocked.
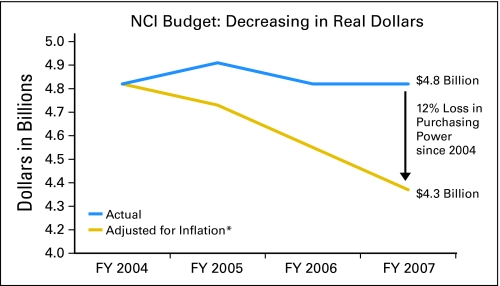
To translate our growing basic science knowledge into better treatments for patients, a new national commitment to cancer research is urgently needed. However, funding for cancer research has stagnated. The budgets of the National Institutes of Health and the National Cancer Institute have failed to keep pace with inflation, declining up to 13% in real terms since 2004. Tighter budgets reduce incentives to support high-risk research that could have the largest payoffs. The most significant clinical research is conducted increasingly overseas. In addition, talented young physicians in the United States, seeing less opportunity in the field of oncology, are choosing other specialties instead.
Although greater investment in research is critical, the need for new therapies is only part of the challenge. Far too many people in the United States lack access to the treatments that already exist, leading to unnecessary suffering and death. Uninsured cancer patients are significantly more likely to die than those with insurance, racial disparities in cancer incidence and mortality remain stark, and even insured patients struggle to keep up with the rapidly rising cost of cancer therapies.
As this annual American Society of Clinical Oncology report of the major cancer research advances during the last year demonstrates, we are making important progress against cancer. But sound public policies are essential to accelerate that progress. In 2009, we have an opportunity to reinvest in cancer research, and to support policies that will help ensure that every individual in the United States receives potentially life-saving cancer prevention, early detection, and treatment.
Sincerely, Richard L. Schilsky, MD President American Society of Clinical Oncology
EXECUTIVE SUMMARY
Each year, the American Society of Clinical Oncology (ASCO) independently reviews advances in clinical cancer research, and identifies those that will have the greatest impact on patient care. This report, Clinical Cancer Advances 2008: Major Research Advances in Cancer Treatment, Screening, and Prevention, highlights 31 of the most significant advances during last year, including 12 that the editors consider to be major advances.
Although these and many other research advances are making a real difference in patient care, cancer continues to take a tremendous toll—more than 500,000 people in the United States will die as a result of cancer this year. In this report, ASCO recommends two strategies for translating our growing basic science knowledge into new treatments for patients: increasing investment in cancer research and expanding patient participation in clinical trials.
Summary of Findings
Following is a summary of the 12 major clinical cancer research advances during the last year, grouped into six key areas:
Hard-to-treat cancers.
Some cancers remain highly resistant to treatment, or are diagnosed late in the course of disease, when treatment is less effective. Advances against hard-to-treat cancers during the last year include:
Cetuximab for lung cancer: Lung cancer is the largest cancer killer in the United States, taking the lives of more than 160,000 people every year. In 2008, a large, randomized study found that adding the targeted therapy cetuximab (Erbitux; ImClone Systems Inc, New York, NY) to initial chemotherapy increased overall survival by up to 21% in patients with advanced non–small-cell lung cancer (NSCLC) that expressed the epidermal growth factor receptor (EGFR).
Gemcitabine for pancreatic cancer: Pancreatic cancer is notoriously difficult to treat, and just 5% of patients survive 5 years or more. A large, randomized study of patients with early-stage pancreatic cancer that had been surgically removed found that 6 months of treatment with the chemotherapy drug gemcitabine (Gemzar; Eli Lilly & Co, Indianapolis, IN) after surgery doubled disease-free survival and increased overall survival.
New drug approvals.
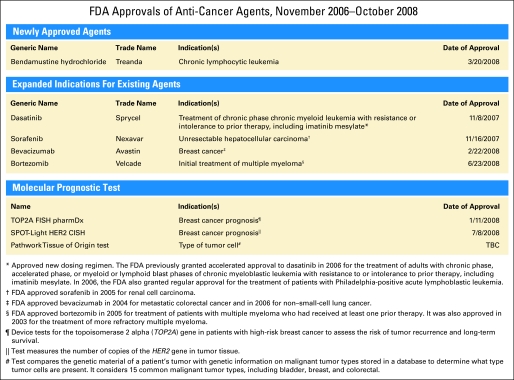
Identifying and expanding treatment options for people with cancer is critical to improving patient outcomes. This year, the US Food and Drug Administration (FDA) approved new cancer treatments for chronic lymphocytic leukemia (CLL) and metastatic breast cancer that are likely to have significant impact on patient care.
Bendamustine for CLL: Although CLL is incurable, it can be managed for long periods of time. A large, international study adds another approach to the treatment arsenal for the disease, finding that the anticancer drug bendamustine (Treanda; Cephalon Inc, Frazer, PA) eliminated CLL in 30% of patients, compared with only 2% of patients who received the standard chlorambucil. The data led to the approval if bendamustine for CLL by the FDA in March 2008.
Bevacizumab for metastatic breast cancer: The monoclonal antibody bevacizumab (Avastin; Genentech, South San Francisco, CA) has been an important treatment for patients with advanced colorectal cancer and NSCLC. In February 2008, the FDA approved the drug—in combination with the chemotherapy drug paclitaxel (Taxol; Bristol-Myers Squibb, Princeton, NJ)—for women with previously untreated metastatic breast cancer that does not express the human epidermal growth factor receptor 2 (HER-2) protein. This approval was based on a 2007 trial that found this treatment combination doubled disease-free survival and improved response rates (more women experienced tumor shrinkage), compared with paclitaxel alone. A second, similar trial released in 2008 confirmed that treatment with bevacizumab and a similar chemotherapy agent significantly improves outcomes for women with metastatic breast cancer.
Reducing cancer recurrence.
Many cancers are initially treated successfully but then recur years later. Cancer recurrence remains a major cause of death, and finding ways to reduce the risk of recurrence is a top research priority. Advances in reducing recurrence during the last year include:
Long-term hormonal therapy for breast cancer: Several new studies suggest that women who have finished the standard 5 years of hormonal therapy with tamoxifen after initial breast cancer treatment may further reduce their risk of recurrence by taking additional years of hormonal therapy, either with an aromatase inhibitor such as letrozole (Femara; Novartis Pharmaceuticals Corp, East Hanover, NJ) or possibly with additional years of tamoxifen.
Zoledronic acid for breast cancer: A large study found that administering the bone-strengthening drug zoledronic acid (Zometa; Novartis Pharmaceuticals Corp, East Hanover, NJ) to premenopausal women undergoing ovarian suppression and additional hormonal therapy with tamoxifen or an aromatase inhibitor reduced the risk of recurrence of early-stage breast cancer by 36% compared with hormonal therapy alone (tamoxifen or anastrozole [Arimidex; AstraZeneca, Wilmington, DE] plus goserelin [Zoladex; AstraZeneca, Wilmington, DE]).
Interferon for melanoma: Melanoma is the deadliest form of skin cancer. A large randomized European study showed that 1 year of pegylated interferon treatment reduced the risk of recurrence of stage III melanoma that had been surgically removed by 18% compared with patients who did not receive treatment.
Personalized medicine.
The growing field of personalized cancer medicine seeks to target cancer therapies based on the unique genetic characteristics of the tumor, and/or the patient. The most significant advance during the last year was in colon cancer treatment:
KRAS status and colon cancer treatment: A multinational team of investigators found that in patients with newly diagnosed advanced colorectal cancer, adding the monoclonal antibody cetuximab to chemotherapy was beneficial only when tumors contained the normal (wild type) form of the gene KRAS, and not when the gene had a mutation. These findings will help guide treatment for each patient, increasing efficacy while eliminating unnecessary adverse effects in those who will not benefit from the treatment.
Risk factors.
Identifying cancer risk factors is critical to prevention and early diagnosis. Advances during the last year that could reduce cancer risk or increase early detection include:
Ovarian cancer and birth control pills: A large analysis of data from 45 prior epidemiologic studies reported that women who have taken oral contraceptives lowered their risk of ovarian cancer by 20% for every 5 years they took the pill, providing a potentially important and readily available way for women at elevated risk of ovarian cancer to reduce their risk.
Human papilloma virus and oral cancer: A major review found that the incidence of oral cancers related to human papilloma virus (HPV) increased by 0.8% per year between 1973 and 2004 in the United States. By contrast, the incidence of HPV-unrelated cancers was stable through 1982 and declined significantly from 1983 to 2004. The authors attributed the increase to possible changes in sexual behaviors, including oral sex. The study suggests a potential role for the HPV vaccine (approved for cervical cancer prevention) in reducing the risk of oral cancers.
Access to care.
Ensuring that cancer patients and survivors have access to high-quality cancer care is critical to increasing survival rates and ensuring long-term health. Research during the last year provides insight into the health care needs of cancer patients and survivors:
Looming shortage of oncologists: A study examining trends in the use of oncology services between 1998 and 2003 in the United States projected a major shortage of oncologists by 2020. Although the total number of cancer patients in the United States was projected to increase 55% by 2020 as the population grows and ages, the supply of oncologists is expected to increase at a significantly slower rate. Based on these data, ASCO estimates that the United States will face a shortage of up to 4,000 oncologists by 2020.
Long-term health needs of childhood cancer survivors: A report from the large, ongoing Childhood Cancer Survivor Study showed that survivors of childhood cancers are five to 10 times more likely than their healthy siblings to develop heart disease 30 years after diagnosis. This finding emphasizes the need to educate patients, their families, and health care providers about the need to monitor for delayed cardiovascular side effects of cancer treatments.
SUMMARY OF RECOMMENDATIONS
To accelerate the pace of progress against cancer, ASCO makes the following recommendations for 2009.
Increase federal funding for clinical cancer research: The United States is in the midst of the longest sustained period of flat funding for cancer research in our history—budgets for the National Institutes of Health (NIH) and the National Cancer Institute (NCI) have been flat for 5 years (Fig 1). As a result, fewer research projects are funded, fewer patients can participate in clinical trials, and young researchers will find it much more difficult to receive funding. ASCO and others in the cancer community are calling for an increase in annual NIH funding of at least $2 billion to keep pace with inflation, fund studies of cancers' molecular mechanisms, and accelerate progress against hard-to-treat cancers.
Remove barriers to participation in clinical trials: Clinical trials are the engine that drives cancer research, yet only 5% of patients participate. With so few patients involved, research is slow and many people with cancer miss out on opportunities to access potentially effective new treatments before they are widely available. To encourage and increase patient participation in cancer clinical trials, ASCO recommends nationwide public and private insurance coverage of clinical trials, full reimbursement to oncology practices for the cost of participating in clinical trials, and measures to increase diversity in clinical trials.
Fig 1.
National Cancer Institute (NCI) budget.
ABOUT THIS REPORT
ASCO—the leading medical society representing more than 25,000 oncologists and other professionals worldwide who care for people with cancer—has developed this report to demonstrate the important progress being made in clinical cancer research and to highlight emerging trends in the field. The report is also intended to fill a gap in cancer literature. It is the only published report to highlight the major advances in clinical cancer research and care each year, and it is written for everyone with an interest in cancer care: the general public, cancer patients and organizations, policymakers, oncologists, and other medical professionals.
This report, now it its fourth year, was developed under the guidance of a 21-person editorial board made up of leading oncologists and other cancer specialists, including specialty editors for each of the disease-specific and issue-specific sections. The editors reviewed research published in peer-reviewed scientific journals and the early results of research presented at major scientific meetings during a 1-year period (October 2007 to September 2008). Only studies that significantly altered the way a cancer is understood or had an important impact on patient care were included. Research in each section is divided into “major advances” and “notable advances,” depending on the impact of the advance on patient care and survival.
Although important research is underway in all cancer types, advances that met the above criteria were not demonstrated in all types of cancer during the last year. Studies included in this year's report are grouped as follows:
Blood and lymphatic cancers
Breast cancer
CNS tumors
GI cancers
Genitourinary cancers
Gynecologic cancers
Head and neck cancers
Lung cancer
Pediatric cancers
Sarcoma
Skin cancer
Cancer prevention
Access to care
Quality of life
The research considered for this report covers the full range of clinical cancer issues:
Epidemiology (populations at greatest or increasing risk)
Prevention
Screening/early detection
Treatment with traditional therapies (surgery, chemotherapy and radiation therapy) as well as newer, more targeted therapies (monoclonal antibodies, kinase inhibitors, angiogenesis inhibitors, and epidermal growth factor receptor inhibitors)
Personalized cancer medicine (targeting treatment based on genetic traits of the tumor or the patient)
Access to high-quality care
Survivorship.
CANCER RESEARCH ADVANCES
Cancers of the blood and lymphatic system.
Cancers of the blood and lymphatic system (also called hematologic cancers) include leukemias, lymphomas, multiple myeloma, and myelodysplastic syndromes. Important advances were made in the treatment of chronic leukemia and Hodgkin's lymphoma in the last year.
Major Advance
Bendamustine is effective against CLL.
CLL is diagnosed in more than 15,000 people each year, primarily in adults age 50 and older. There is no cure, though chemotherapy (with chlorambucil, cyclophosphamide, or fludarabine) is often used to slow the progression of the disease.
Bendamustine has been used in Europe for some 30 years. It was believed to have the same properties of similar drugs called alkylating agents, but researchers have recently learned more about its modes of action and its potential use for treating a variety of hematologic cancers.1
An international phase III study found that bendamustine eliminated cancer completely in 30% of patients with CLL, compared with only 2% of patients who received chlorambucil, which is often used to treat symptomatic CLL. Bendamustine also increased progression-free survival by more than 1 year (21.7 v 9.3 months). The data supported the use of bendamustine as first-line treatment for CLL and led to the approval of bendamustine for CLL by the FDA in March 2008.
Notable Advance
SGN-35 is active in patients with relapsed/refractory Hodgkin's lymphoma.
A phase I study found that the investigational agent SGN-35 induced partial remission in nine of 28 patients and an additional 11 patients had stable disease. Of 13 patients who received 1.2 m/kg, or more, there were seven partial remissions. SGN-35 was generally well tolerated, with fatigue, diarrhea, and cough as the most common adverse effects.
SGN-35 is an engineered antibody attached to a chemotherapy drug called monomethyl auristatin E. The antibody component binds to a protein called CD30 on Hodgkin's lymphoma cells, and the monomethyl auristatin E disrupts cell growth and division, and prompts cancer cells to self-destruct. Approximately 5% of people with Hodgkin's lymphoma experience a relapse or stop responding to treatment. If confirmed in additional studies, these findings suggest that SGN-35 may play a role in the treatment of this cancer, offering an approach that is more targeted than conventional chemotherapy and radiation therapy, and potentially associated with fewer adverse effects.2
BREAST CANCER
During the last several decades, improvements in early detection and the development of more effective treatments have led to significant declines in breast cancer deaths, improving the outlook for women living with the disease. Increasingly, breast cancer is being treated as a family of diseases, each with its own molecular features and corresponding behaviors, rather than as a single disease. Today the molecular characteristics of each woman's tumor cells are routinely taken into account when doctors consider treatment options.
During the last year, the FDA approved an angiogenesis inhibitor and a new cytoxic agent. Both were shown to slow the growth of metastatic disease. Preliminary data regarding an association between vitamin D levels in the body and breast cancer outcome were also reported.
Major Advances
Hormonal therapy after 5 years of tamoxifen reduces risk of recurrence and metastasis.
A major study provided evidence that hormonal therapy after 5 years of standard tamoxifen reduces the risk of breast cancer recurrence and metastases among all age groups. Previously, this multicenter phase III clinical trial—called the MA.17 study, led by the National Cancer Institute of Canada Clinical Trials Group—reported that the aromatase inhibitor letrozole cuts the risk of breast cancer recurrence by 63% among postmenopausal women with early-stage disease who completed 5 years of tamoxifen therapy.1 A 2008 analysis of the same patient group found that the reduced risk of breast cancer recurrence persisted among all age groups, including women older than age 70.2 years.
Two other studies suggested that continuing tamoxifen beyond the initial 5-year treatment period may reduce the risk of recurrence, though this finding needs to be confirmed before longer-duration tamoxifen can be recommended routinely. The international randomized Adjuvant Tamoxifen, Longer Against Shorter (ATLAS) study found that women who took tamoxifen for 10 years had a 13% reduction in their risk of recurrence compared with those who took the drug for 5 years. The aTTom (Adjuvant Tamoxifen—To Offer More?) study reported a 6% reduction in risk with 10 years of tamoxifen. The authors of both studies state that the follow-up time (4.2 years) may have been too short to see a significant result, and that longer follow-up is necessary to accurately assess the value of 10-year tamoxifen treatment.3,4
Although tamoxifen has been an important and effective part of breast cancer treatment among women with estrogen receptor–positive breast cancer who take the drug, more than half of all recurrences and two thirds of breast cancer deaths occur after 5 years of tamoxifen therapy. Together, the new studies suggest that additional hormonal therapy after standard tamoxifen treatment may further reduce the risk of cancer recurrence; this approach is becoming part of the standard of care. It remains unknown if any therapy is beneficial after a 5-year course of an aromatase inhibitor in postmenopausal women.
Adding zoledronic acid to hormonal therapy reduces the risk of recurrence in premenopausal women with early-stage breast cancer.
A study found that administering zoledronic acid, a drug used to treat bone metastases and recently approved to treat osteoporosis, to premenopausal women undergoing ovarian suppression and hormonal therapy significantly reduces the risk of recurrence of early-stage breast cancer. In this study, zoledronic acid with hormonal therapy reduced the risk of breast cancer recurrence by 36% compared with hormonal therapy alone (tamoxifen or anastrozole plus goserelin).
Zoledronic acid is already used to treat multiple myeloma, and lung and prostate cancer. The drug has also been used to reduce or delay the onset of bone complications (such as fractures) in women with breast cancer that has spread to the bones. This study suggests that zoledronic acid can reduce metastases in women with early-stage breast cancer and that fewer women will develop recurrences; a similar finding was noted several years earlier in clinical trials with another bisphosphonate drug called clodronate. If confirmed by other research, the results of this new study could expand the indication for the use of zoledronic acid in breast cancer treatment.5
FDA approves bevacizumab for metastatic breast cancer.
In February 2008, the FDA approved the use of bevacizumab in combination with paclitaxel for treating women with previously untreated metastatic breast cancer who are not candidates for trastuzumab (Herceptin; Genentech Inc, South San Francisco, CA) because their cancers do not express the human epidermal growth factor receptor 2 protein. The approval was based on the results of a phase III Eastern Cooperative Oncology Group clinical trial reported in 2007, which found that progression-free survival among women who received paclitaxel plus bevacizumab was twice as long (11.8 months) as that among women who received paclitaxel alone (5.9 months). More women in the bevacizumab group (36.9%) showed response to treatment (eg, tumor shrinkage) than in the paclitaxel group (21.2%).6
Similar findings were reported by the Avastin Plus Docetaxel Chemotherapy (AVADO) study in 2008, which found that adding bevacizumab to treatment with docetaxel (Taxotere [Sanofi-aventis, Bridgewater, NJ],which is chemically similar to paclitaxel) improved progression-free survival and increased the response rate from 44.4% to up to 63.1%.7 Bevacizumab, which works by inhibiting the development of blood vessels tumors need to grow and spread, is also approved for the treatment of advanced colorectal cancer and advanced NSCLC.
Notable Advances
FDA approves ixabepilone for refractory metastatic breast cancer.
Effective treatment options for patients with metastatic breast cancer that is resistant to anthracyclines and taxanes are limited. In October 2007, the FDA approved the drug ixabepilone (Ixempra; Bristol-Myers Squibb, Princeton, NJ) for the treatment of advanced breast cancer in patients whose tumors are unresponsive to other types of chemotherapy. The approval was based on an international phase III randomized clinical trial, reported in 2007, which found that adding ixabepilone to capecitabine (Xeloda; Roche Laboratories Inc, Nutley, NJ) treatment in women with metastatic breast cancer that persisted despite prior therapy with anthracyclines and/or taxanes reduced progression of the cancer by 25% (5.8 months with ixabepilone v 4.2 months). Ixabepilone also more than doubled the response rate (from 14% with capecitabine alone to 35% for capecitabine plus ixabepilone). The most common moderate to severe adverse effects seen in the ixabepilone group were sensory nerve problems, fatigue, and low WBC counts.
This study was the first to demonstrate superior progression-free survival and response rates after the addition of a second agent to capecitabine in patients with metastatic breast cancer that is resistant to anthracyclines and taxanes.10
Vitamin D deficiency is linked to worse breast cancer outcome.
Canadian researchers found for the first time that women with vitamin D deficiency at the time of breast cancer diagnosis were more likely to experience metastasis of their cancer and more likely to die, compared with women with adequate vitamin D levels. Only 24% of the patients in the study had adequate levels of vitamin D when they were diagnosed with cancer. Women deficient in vitamin D (less than 50 nmol/L) were also more likely to have high-grade (more aggressive) cancers. After 10 years, 83% of women with adequate levels (more than 72 nmol/L) remained free of metastases and 85% were still alive, compared with 69% and 74%, respectively, of women with vitamin D deficiency.
There is no Recommended Dietary Allowance for vitamin D in the United States, and high doses can be toxic. This study is of great interest, but it was retrospective in nature, highly preliminary, and in need of confirmation.
CNS CANCERS
Tumors of the CNS (the brain and spinal cord) are a unique clinical challenge in the field of oncology, especially when the tumor has returned or persisted despite treatment. Although clinical trials during the last 25 years have evaluated a variety of drugs and treatment delivery systems, the prognosis for people with brain tumors has remained largely unchanged. Recent studies have produced promising data on the use of bevacizumab against gliomas—the most aggressive and difficult-to-treat form of brain cancer.
Notable Advance
Bevacizumab plus irinotecan increases progression-free survival for glioblastoma.
Several studies in the last year demonstrated that administering bevacizumab to patients with glioblastoma can increase progression-free survival. A phase II study showed that bevacizumab plus irinotecan (Camptosar; Pfizer Inc, New York, NY) increased 6-month progression-free survival from 35.1% with bevacizumab alone to 50.2% with the two drugs together in patients with glioblastoma that had returned or persisted despite therapy. More patients in the group that received both drugs responded to treatment (32.9%) than among those who received bevacizumab alone (20%). The incidence of moderate to severe adverse effects was higher in the patients who received both drugs (67.1%) than in those who received bevacizumab alone (47.6%).
Bevacizumab targets a protein in cancer cells called vascular endothelial growth factor, which is found in large amounts in high-grade gliomas and which plays a role in the growth of the blood vessels supplying nutrients to tumors. Although bevacizumab is approved for treating breast, lung, and colorectal cancers, it is increasingly used to treat patients with recurrent/refractory gliomas; these data will help guide clinicians regarding its optimal use for this purpose.11
GI CANCERS
GI cancers include those of the esophagus, stomach, liver, pancreas, biliary tract, colon, rectum, and anus. The ability to treat these cancers effectively varies significantly. For example, although many colorectal cancers can be diagnosed in their early, more curable stages using colonoscopy, no such screening tests exist for less common cancers of the digestive tract—such as those of the pancreas—which are often diagnosed when they are advanced and more difficult to treat.
Notable studies published in the last year explored new ways to use existing anticancer drugs for pancreatic cancer as well as novel methods for predicting which patients with colorectal cancer are most likely to respond to specific drug regimens.
Major Advances
KRAS status predicts whether patients with newly diagnosed metastatic colorectal cancer respond to cetuximab.
A multinational team of investigators found that patients with newly diagnosed metastatic colorectal cancer have an added benefit when the monoclonal antibody cetuximab is added to chemotherapy only when their tumors contain the normal form (wild type) of the gene KRAS, and not when the gene has a mutation. Investigators found that among patients with normal KRAS, 59.3% experienced tumor shrinkage when treated with chemotherapy and cetuximab, compared with 43.2% who responded to chemotherapy alone. Among patients with mutated KRAS in their tumors, however, there was no difference in response rates between those who received chemotherapy alone and those who received chemotherapy and cetuximab.
Cetuximab is a targeted therapy that blocks the EGFR in tumors. KRAS mutations, which are found in 30% to 45% of all colorectal tumors, have previously been shown to predict whether patients will benefit from EGFR-inhibiting drugs in the second-line or later setting.
These findings represent an important contribution to the field of personalized medicine, in which molecular and genetic tests are employed to help determine the optimal treatment for each patient and to avoid overtreatment with drugs that have potentially toxic adverse effects but little benefit.12
Gemcitabine extends survival in operable pancreatic cancer.
Pancreatic cancer remains very difficult to treat, and even a few months increased survival represent a major advance for people with the disease. Two studies during the last year examined novel ways to administer gemcitabine—a drug widely used to treat pancreatic cancer—to maximize its effectiveness.
A phase III study of patients with pancreatic cancer that had been surgically removed found that 6 months of treatment with gemcitabine after surgery doubled disease-free survival (13.4 months in those who received gemcitabine v 6.9 months in those who did not receive chemotherapy) and extended overall survival (22.8 v 20.2 months, respectively).13
In related research, an Eastern Cooperative Oncology Group study showed that patients with locally inoperable pancreatic cancer who underwent radiation therapy plus gemcitabine lived almost 2 months longer (11 months) compared with patients who received gemcitabine alone (9.2 months).14
Notable Advances
Patients with colon cancer with inability to repair genes less likely to respond to fluorouracil-based chemotherapy.
In a pooled reanalysis of randomized chemotherapy trials, patients with colon cancer who had an inability to correct certain genetic alterations, called deficient mismatch repair, did not benefit from fluorouracil-based chemotherapy (as determined by disease-free and overall survival) compared with patients with proficient mismatch repair, who were more likely to benefit. These confirmatory results suggest that mismatch repair status should be considered when choosing therapy for patients with colon cancer. The assessment of mismatch repair could become another test to predict how well patients might respond to chemotherapy.15
GENITOURINARY CANCERS
Cancers of the genitourinary system include those of the kidneys, bladder, and prostate, as well as less common cancers such as those of the urethra and ureters. Prostate cancer is the most common cancer diagnosed in the United States, with more than 186,000 cases annually. During the last year, several early-phase studies generated promising data regarding the use of new drugs to treat advanced prostate cancers that have become resistant to hormonal therapies, so-called hormone-refractory prostate cancer.
Notable Advance
Advanced prostate cancers respond to new agents in early studies.
Four percent of men diagnosed with prostate cancer in the United States each year are found to have metastatic disease at diagnosis, and their 5-year survival rate is far lower than for men with early-stage disease: 31.9% versus nearly 100%. Prostate cancers are initially dependent on the male hormone testosterone for growth. Hormonal therapies that lower the level of testosterone are among the most effective treatments for prostate cancers that have metastasized. However, the effectiveness of hormonal treatments is not permanent, and over time many prostate cancers progress despite hormones. Two clinical trials demonstrated encouraging results regarding new treatments for hormone-refractory prostate cancer; the findings need to be confirmed in larger, later-stage studies before the drugs can be incorporated into clinical practice.
A phase I study found that abiraterone acetate reduced prostate-specific antigen (PSA) levels by up to 90% in men with hormone-refractory prostate cancer. Declines in PSA levels of 30%, 50%, and 90% or more were observed in 66%, 57%, and 29% of patients, respectively, and lasted from a few months to nearly 2 years. Some patients also had an improvement in their symptoms. Abiraterone works by inhibiting an enzyme called CYP17, which plays an important role in the production of hormones such as testosterone.16
Another study showed that custirsen (OGX-011), a drug classified as an antisense oligonucleotide, plus the combination of docetaxel and prednisone (drugs conventionally used to treat advanced prostate cancer) was more effective than the combination of custirsen, mitoxantrone, and prednisone in reducing PSA levels and pain responses in men with hormone-refractory prostate cancer. Custirsen works by increasing the sensitivity of prostate cancer cells to chemotherapy drugs such as docetaxel.17 Forty percent of men in the custirsen/docetaxel group experienced a PSA reduction of 50% or more, versus 27% of those in the custirsen/mitoxantrone group; pain relief was observed in 67% of men in the docetaxel group and 50% of men in the mitoxantrone group.
GYNECOLOGIC CANCERS
Gynecologic cancers include cancers of the cervix, uterus, ovaries, fallopian tubes, vulva, and vagina. This last year, a definitive analysis was published linking oral contraceptive use to a reduction in the risk of ovarian cancer, which is difficult to treat because it is usually diagnosed at an advanced stage.
Major Advance
Oral contraceptives reduce ovarian cancer risk.
An analysis of data from 45 prior epidemiologic studies reported that women who have taken oral contraceptives lowered their risk of ovarian cancer by 20% for every 5 years they took the pill. This reduction in risk persisted for more than 30 years after oral contraceptive use had ceased, but lessened over time: the proportional risk reductions for each 5 years of use were 29% for use that had ceased less than 10 years previously, 19% for use that had ceased 10 to 19 years before, and 15% for use that had ceased 20 to 29 years earlier.
Although the reduction in ovarian cancer risk associated with oral contraceptive use has been recognized for some time (and is due to the suppression of ovulation resulting from taking the pill), this is the largest and most definitive study on this topic, assessing data on more than 110,000 women. The researchers estimated that oral contraceptives have prevented approximately 200,000 ovarian cancers and 100,000 deaths from the disease worldwide, and that during the next several decades, the number of ovarian cancers prevented could increase to at least 30,000 each year. Researchers are discussing whether this approach could have a role for reducing ovarian cancer risk in women who are at elevated risk due to a family history of the disease.18
HEAD AND NECK CANCERS
The phrase head and neck cancer generally refers to tumors that arise in or around the throat, larynx, nose, sinuses, and mouth. Although tobacco consumption and alcohol abuse are the primary causes of these tumors, studies during the last year linked HPV to some of these cancers, particularly in the oropharynx, which includes the base of the tongue and tonsils.
Other research published in the last year reported on the promise of novel targeted agents for treating thyroid cancers that require chemotherapy as part of their management.
Major Advance
Increase in incidence of HPV-related head and neck oral cancers.
The incidence of head and neck cancers related to HPV increased by 0.8% per year between 1973 and 2004 in the United States. These HPV-related carcinomas were diagnosed at a slightly younger age (mean age, 61.0 years) than HPV-unrelated cancers (mean age, 63.8 years). In contrast, the incidence of cancers arising from HPV-unrelated primary sites was stable through 1982 and declined significantly from 1983 to 2004. Of note, the authors also found that patients with HPV-related cancers had better survival rates than those whose cancers were not associated with HPV when treated with radiotherapy.19
The authors attributed the increase to possible changes in sexual behaviors, which increase the risk of HPV transmission to the mouth and throat, such as oral sex. Because of the association between HPV and these head and neck cancers, there is increasing discussion regarding the potential role of the HPV vaccine (currently approved for preventing cervical cancer) as a preventive intervention.
Notable Advance
Targeted therapies slow growth of advanced thyroid cancer.
Several studies in the last year demonstrated the effectiveness of targeted agents for the treatment of advanced thyroid cancer. One phase II study showed that sorafenib (Nexavar; Bayer Healthcare Pharmaceuticals, Leverkusen, Germany), a drug approved for treating renal cell carcinoma and liver cancer, induced partial responses in 23% of patients with metastatic and refractory thyroid cancer. An additional 53% had stabilization of their disease. Overall, the median progression-free survival was 79 weeks.20
Another phase II study demonstrated that the investigational drug axitinib induced responses in 30% of patients with advanced, incurable thyroid cancer and resulted in a median progression-free survival of 18.1 months.21 A third study showed that 14% of patients with progressive, radioiodine-resistant thyroid cancer responded to the experimental drug motesanib, with an estimated progression-free survival of 40 weeks.22
Thyroid cancer is successfully treated in most cases with a combination of surgery, thyroid-stimulating hormone suppression through the administration of supplemental thyroid hormone, and in selected cases the addition of radioiodine. Doxorubicin (Adriamycin; Johnson & Johnson, New Brunswick, NJ) is the only chemotherapy drug approved by the FDA for use in thyroid cancer that is refractory to standard treatments, but it has disappointing efficacy and is associated with potentially significant adverse effects.
Sorafenib, axitinib, and motesanib are all taken orally and share the ability to inhibit angiogenesis, or the growth of blood vessels that feed tumors. Although larger clinical trials are required to explore the potential for these agents to improve overall survival among patients with refractory thyroid cancer, these studies signal an approaching paradigm shift in the way advanced thyroid cancer is treated.23
LUNG CANCER
A number of advances in lung cancer treatment have been made in recent years. Targeted agents are available for many patients, and studies are demonstrating the value of new uses for conventional chemotherapy drugs after surgery to improve overall survival. Researchers are also learning that specific characteristics of an individual's tumor may help predict prognosis and response to treatment.
In the last year, studies supported the role of the targeted drug cetuximab in lung cancer treatment and evaluated new ways of monitoring treatment response by analyzing the genetics of tumor cells in the bloodstream.
Major Advance
First-line treatment with cetuximab extends survival in NSCLC.
Cetuximab is approved for treating advanced colorectal and head and neck cancers. A phase III study (called Cisplatin/Vinorelbine ± Cetuximab as First-Line Treatment of Advanced Non–Small-Cell Lung Cancer [FLEX]) found that adding cetuximab to initial chemotherapy with cisplatin and vinorelbine (Navelbine; GlaxoSmithKline, Brentford, Middlesex, United Kingdom)—anticancer drugs conventionally used to treat patients with NSCLC—extended overall survival by up to 21% in patients with advanced NSCLC that expressed epidermal growth factor receptor (EGFR). Cetuximab works by targeting EGFR.
This study adds to the body of evidence showing that EGFR plays a strong role in the progression of some lung cancers and that treatments targeting EGFR can improve survival. It also validates the continued exploration of the molecular biology of lung cancer, including studies identifying new therapeutic targets.24
Notable Advance
Noninvasive method for genotyping tumor cells in blood.
Drugs such as erlotinib (Tarceva; Genentech Inc, South San Francisco, CA) and gefitinib (Iressa; AstraZeneca, Wilmington, DE) target the EGFR protein, but some patients develop resistance to these drugs, as evidenced by the emergence of EGFR mutations in tumor cells. In a new study, researchers captured circulating tumor cells in the blood of patients with NSCLC, to show that an increase in the number of tumor cells with EGFR mutations was associated with tumor progression (and the emergence of new EGFR mutations in some cases). A reduction in the number of tumor cells detected was associated with tumor shrinkage.
Molecular characterization of circulating tumor cells may potentially provide a noninvasive strategy for monitoring the genetic profile of tumor cells during treatment, enabling doctors to better tailor therapy. The noninvasive approach is especially important because not all patients with lung cancer have operable disease, and therefore many of them do not have tumor tissue available for genetic analysis.25
PEDIATRIC CANCERS
As a result of progress made in collaborative multicenter clinical trials, children diagnosed with cancer today have a better chance than ever before of surviving their disease—and in many cases, their survival is significantly better than that of adults. However, researchers are also learning more about the long-term adverse effects of therapy, and are using that knowledge to refine current approaches to treating childhood cancers, and to monitoring the health of adult survivors who were treated many years ago.
In the last year, studies generated more data on the long-term effects of cancer treatment, such as increased risk of heart disease and leukemia, and ways to predict leukemia treatment outcome. Other research identified a genetic marker for neuroblastoma predisposition in children with a family history of this rare cancer.
Major Advances
Childhood cancer survivors face increased risk of heart disease.
A report from the Childhood Cancer Survivor Study showed that survivors of childhood cancers are five to 10 times more likely than their healthy siblings to develop heart disease 30 years after diagnosis (though the rate was low overall): 2% had atherosclerosis (hardening of the arteries), 4% developed congestive heart failure, 1% experienced a myocardial infarction (heart attack), 3% developed pericardial disease, and 4% had valvular heart disease.
The Childhood Cancer Survivor Study follows the largest cohort of childhood cancer survivors in the world and has generated the greatest amount of data related to the long-term adverse effects of cancer treatment. These new findings emphasize the need to educate patients, their families, and other health care providers about the risk of delayed cardiovascular adverse effects of cancer treatments, so that patients can be closely monitored after their treatments end for many years.26
Notable Advances
Gene that increases risk of neuroblastoma is identified.
By studying the genetics of neuroblastoma in 18 families, researchers found a hereditary neuroblastoma predisposition gene located on chromosome 2p24-23. Familial neuroblastoma is aggressive and usually lethal during childhood. The authors speculated that inactivation of this gene may also influence the development of nonfamilial human neuroblastomas.
These findings might be useful for predicting neuroblastoma risk in children from families that have a history of the disease. In addition, mutations in the same gene have been associated with a much more common cancer called anaplastic large-cell lymphoma; the development of targeted therapies for anaplastic large-cell lymphoma might therefore potentially benefit patients with neuroblastoma.27
Childhood exposure to some anticancer agents increases leukemia risk.
A Children's Oncology Group study found that children treated with platinum compounds and etoposide for their primary cancer have a three-fold to six-fold higher risk of developing therapy-related myelodysplasia (a precancerous disorder of the bone marrow) and acute myeloid leukemia, after adjusting for known exposure to alkylating agents and anthracyclines (drugs commonly used to treat cancer which are already known to potentially cause leukemia).
Given that platinum and etoposide are widely used in the treatment of pediatric cancers, the association between exposure to these agents and the development of acute myeloid leukemia justifies continued follow-up of these children after completion of therapy. In addition, these findings provide a strong rationale for identifying alternative treatment approaches to reduce the risk of therapy-related leukemia.28
Minimal residual disease is useful for predicting leukemia outcome.
Minimal residual disease (MRD)—the amount of cancer remaining in the body after treatment—is a measurement used to monitor response to treatment and predict a patient's outcome. It is usually measured 1 to 3 months into therapy in children being treated for acute lymphoblastic leukemia (ALL). A study assessing MRD later in the course of treatment found that relatively few patients with ALL have MRD 5 to 6 months into therapy (4.8% of patients), but that those who do have a poor prognosis (43% were free of relapse at 5 years, compared with 83% of those without late MRD). The finding indicates that MRD after initial therapy in ALL is an important biomarker that may be used as a substitute end point in the design of clinical trials to expedite the discovery of more effective treatments for childhood ALL.29
SARCOMA
Sarcomas are rare tumors that can occur in any site of the human body, although about half occur in the limbs. There are more than 50 different types of soft tissue sarcomas, which arise in tissues such as fat, muscles, nerves, tendons, and blood and lymph vessels. Approximately 15% of soft tissue sarcomas occur in the abdominal region, and many of those tumors are known as GI stromal tumors (GISTs). Ewing sarcoma is a rare soft tissue sarcoma that mainly affects children, whereas osteosarcomas originate in the bones.
Because these tumors vary greatly in their tissue of origin, treatments also vary. Advances in molecular biology are benefiting patients with sarcoma by identifying new therapeutic targets. During the last year, studies reported promising findings regarding targeted therapies for soft tissue sarcomas, including Ewing sarcoma and GISTs.
Notable Advances
Anti–insulin-like growth factor 1 receptor antibody shows promise for treating sarcoma.
A phase I study showed that about a third of patients with sarcoma either experienced tumor shrinkage or disease stabilization after receiving the anti–insulin-like growth factor 1 receptor (anti–IGF-1R) antibody CP-751,871—especially those with Ewing sarcoma. Given that sarcomas depend on IGF signaling more than normal cells, anti-IGF antibodies have the potential to be active against these cancers.30
Sorafenib slows growth of refractory GIST.
This phase II study showed that sorafenib controlled disease growth in 71% of patients with GIST that had become resistant to imatinib (Gleevec; Novartis Pharmaceuticals, East Hanover, NJ) and sunitinib (Sutent; Pfizer Inc, New York, NY). Median progression-free survival was 5.3 months and median survival was 13.0 months. These preliminary data suggest that sorafenib could be another treatment alternative for patients with GIST who have become resistant to imatinib or sunitinib—the two targeted therapies currently approved for treating this disease. More studies are necessary to validate the potential role of sorafenib in the treatment of GIST.31
SKIN CANCER
Basal cell and squamous cell carcinomas remain the most common skin cancers in the United States, are usually treated successfully, and can often be prevented by ensuring adequate sun protection. Melanoma, however, remains a far more deadly form of skin cancer. Although treatable when detected early, melanoma that has spread can be life threatening.
Studies published in the last year described new approaches for slowing the progression of advanced melanoma and reducing recurrence. Other research explored the use of dermoscopy for analyzing skin lesions.
Major Advance
Pegylated interferon reduces risk of melanoma recurrence.
A phase III randomized study by the European Organisation for Research and Treatment of Cancer showed that 1 year of pegylated interferon treatment reduced the risk of recurrence of stage III melanoma that had been surgically removed by 18% compared with patients who underwent observation. The 4-year rate of recurrence-free survival was 45.6% for patients who receive pegylated interferon alfa-2b versus 38.9% for the observation group. Overall survival did not differ between the two groups. The most common adverse effects associated with pegylated interferon were fatigue, liver toxicity, and depression.
Interferon has been used for years as part of standard therapy to reduce the risk of melanoma recurrence and to slow the progression of metastatic disease, but it is not a cure. Pegylated interferon is a form of interferon that enables it to remain in the patient's body longer, reducing the number of injections needed from three times a week to only once a week. The results of this study suggest that pegylated interferon may have a role in the treatment of patients with resected (surgically removed) stage III melanoma.32
Notable Advances
Sorafenib improves progression-free survival in advanced melanoma.
A randomized phase II study showed that sorafenib plus dacarbazine (a chemotherapy drug that is the standard of care for advanced melanoma) increased progression-free survival by 34% in patients with advanced melanoma compared with dacarbazine alone. Median progression-free survival in patients who received sorafenib plus dacarbazine arm was 21.1 weeks, compared with 11.7 weeks in patients who received dacarbazine plus placebo.
If confirmed in a phase III clinical trial, sorafenib could potentially become part of the treatment regimen for patients with melanoma. The drug targets components of a signaling pathway that includes the Raf kinase enzyme; this pathway is activated in most advanced melanomas.33
Study Shows Value of Dermoscopy for Analyzing Skin Lesions
A meta-analysis conducted in Australia reported that dermoscopy is more accurate than naked-eye examination for the diagnosis of cutaneous melanoma in skin lesions that are suggestive of disease when performed in the clinical setting. Dermoscopy is a noninvasive technique that enables the clinician to perform direct microscopic examination of diagnostic features, invisible to the naked eye, in pigmented skin lesions in a clinical office setting. The technique may enhance the ability of clinicians to stratify patients who need more extensive evaluation (such as a biopsy) from those who do not.34
CANCER PREVENTION
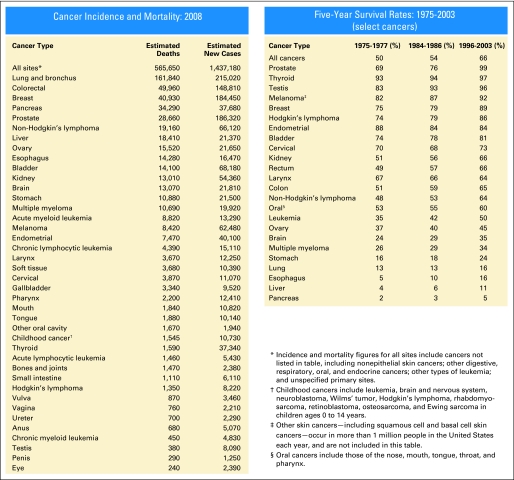
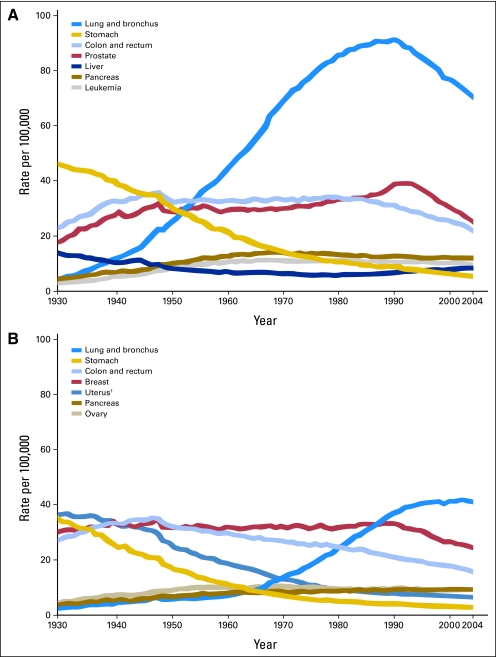
Advances in molecular biology and in our understanding of the mechanisms underlying cancer development are allowing health care professionals to develop new ways to reduce cancer risk (Figs 2, 3, and 4). Two studies published in the last year shed light on the use of a common prostate drug to reduce the risk of prostate cancer.
Fig 2.
Cancer statistics: cancer incidence, mortality, and survival rates; 5-year survival rates, 1975 to 2003. Incidence and mortality figures for all sites include cancers not listed in table, including nonepithelial skin cancers; other digestive, respiratory, oral, and endocrine cancers; other types of leukemia; and unspecified primary sites. Source: Cancer Facts and Figures 2008. Atlanta, GA, American Cancer Society, 2008.
Fig 3.
Cancer mortality trends: cancer death rate graphs for (A) men and (B) women. Source: Cancer Facts and Figures 2008. Atlanta, GA; American Cancer Society, 2008.
Fig 4.
US Food and Drug Administration (FDA) approvals of anticancer agents: October 2007 to September 2008. CP, chronic phase; FISH, fluorescent in situ hybridization; CISH, chromagen in situ hybridization; TBC, taxane-based chemotherapy.
Notable Research
Link between finasteride and high-grade prostate cancer explained.
Finasteride is a drug commonly used to treat benign enlargement of the prostate, and has shown promise for preventing prostate cancer. It works by inhibiting an enzyme, 5-alpha reductase, which converts testosterone into dihydrotestosterone hormones that can fuel prostate cancer growth. Previous results of the Prostate Cancer Prevention Trial (PCPT)—a prospective randomized clinical trial that compared finasteride with a placebo—showed that 5 mg of daily finasteride reduced the overall risk of prostate cancer over a 7-year period from 24.4% to 18.4% (a relative risk reduction of 24.8%) in men who underwent regular screenings for prostate cancer. But the study also showed that more men in the finasteride group (6.4%) developed potentially aggressive (high grade) cancers compared with those in the placebo group (5.1%). This caused many health care professionals to view the results of the PCPT with caution until the data could be further explained.
In an analysis reported in the last year, investigators examined tumor size and other features of the high-grade cancers to see if they could explain the findings of the PCPT. They found that finasteride reduced prostate volume compared versus treatment with placebo. This effect could increase the likelihood that physicians could detect high-grade prostate cancers by needle biopsy. In other words, PSA seemed to become a more sensitive screening test in men who took finasteride.
Moreover, among men with high-grade tumors, those who were taking finasteride had less extensive cancers than those in the placebo group. This finding provides further reassurance that finasteride does not cause a true increase in the risk of aggressive prostate cancer. The authors noted that no single mechanism is likely to explain the increase in high-grade prostate cancers observed among men who took finasteride in the PCPT.35
An additional study using a statistical model for prostate cancer detection in the PCPT confirmed these findings by showing that prostate volume was 25% lower in the finasteride group than in the placebo group, and that the likelihood of detecting high-grade prostate cancer decreased as prostate volume increased.36
ACCESS TO CARE
Access to health care in general and cancer care in particular is a major concern for patients and health care providers. A 2008 study on the oncology workforce predicted that as the current population ages, there will be severe shortages in the number of oncologists available to meet the needs of people living with cancer.
Cost of care is also a pressing issue for patients, and the price of novel targeted therapies has received special attention, as costs for some drugs exceed tens of thousands of dollars per year for therapies that in some cases may extend life by only a few months. A study in the last year analyzed increases in the cost of initial cancer treatments. Another study examined how changes in insurance may affect patients' choice of cancer screening tests.
Major Research
Shortage of oncologists forecasted by 2020.
A new study examined trends in the use of oncology services between 1998 and 2003 in the United States and projected future trends. The total number of cancer patients in the United States was projected to increase 55%, from 11.8 million in 2005 to 18.2 million in 2020. The total number of oncology visits was projected to increase from 38 million in 2005 to 57 million in 2020.
The authors concluded that utilization of oncologists' services will increase significantly between 2005 and 2020, driven primarily by an increase in the number of cancer survivors and by the aging of the population. They noted that the United States may face an acute shortage of medical oncologists if efforts are not taken to meet this growing need.37 A separate analysis by ASCO based on the raw data from this study estimated that the United States will face a shortage of 2,550 to 4,080 oncologists by 2020.
Notable Research
Cancer screening choices may change with health insurance changes.
Health plans with high deductibles could lead patients to avoid preventive care, such as cancer screening. A study conducted in Massachusetts showed that people who changed from a health maintenance organization to a high-deductible health insurance plan (which fully covered mammography, Papanicolaou tests, and fecal occult blood testing, but not colonoscopy, flexible sigmoidoscopy, or double-contrast barium enema) were just as likely to seek cancer screening tests, but were likely to change which tests they received. For example, they were likely to choose fecal occult blood testing instead of colonoscopy (a positive stool blood test would signal the need for a colonoscopy). These results indicate that patients remain likely to continue seeking some type of cancer screening as long as the tests are covered by their insurance providers.38
Costs of initial cancer treatment increase.
A study found a significant increase in the cost of initial cancer treatment from 1991 to 2002 among elderly patients with breast, colon, prostate, and lung cancers. For patients diagnosed in 2002, Medicare paid an average of $39,891 for initial care for each lung cancer patient, $41,134 for each colorectal cancer patient, and $20,964 for each breast cancer patient, corresponding to inflation-adjusted increases from 1991 of $7,139, $5,345, and $4,189, respectively. By contrast, the mean Medicare payment for initial care for prostate cancer declined by $196 during this period, to $18,261 in 2002.
The researchers noted that the increase in initial cancer treatment costs reflects more patients receiving surgery and adjuvant therapy as well as increasing prices for these treatments. They added that these trends are likely to continue in the near future, but that more efficient and targeted use of costly therapies could diminish the economic impact of this trend.39
QUALITY OF LIFE
The quality of life of people with cancer has become increasingly important as more people live longer with the disease, and research in this area is increasing. During the last year, one study analyzed acupuncture as a way to minimize adverse effects after cancer surgery.
Notable Research
Acupuncture eases pain and dry mouth after head and neck surgery.
A study found that acupuncture was more effective than usual care for easing pain, dysfunction, and dry mouth in patients who had surgery for head and neck cancers 3 or more months earlier. These adverse effects are common among patients being treated for head and neck cancers, and the usual course of care includes physical therapy, anti-inflammatory drugs, and analgesic drugs. In this study, more patients who had acupuncture (39%) responded to treatment (demonstrating relief of pain, dysfunction, and dry mouth) than patients who received usual care (7%).40
RECOMMENDATIONS
As this report demonstrates, significant progress is being made against cancer. New treatments are improving patient survival and reducing cancer recurrence, even for some of the most difficult-to-treat cancers. We know more about cancer risk factors, which may help prevent cancer and increase early diagnosis. Treatments are increasingly targeted to a tumor's specific molecular characteristics. In addition, we have more insight than ever into the long-term health care needs of cancer survivors.
These advances are possible because of the nation's investment in clinical research, which depends on robust federal funding and patient participation in clinical trials. However, federal funding has stalled, and just 5% of cancer patients participate in clinical trials.
To accelerate the pace of cancer research, ASCO makes two primary recommendations for the coming year: increase funding for clinical research, and remove barriers to patient participation in cancer clinical trials.
Increase Federal Funding for Clinical Research
The United States is in the midst of the longest sustained period of flat funding for cancer research in the country's history. Budgets for the NIH and the NCI have been flat for 5 years. Adjusted for biomedical inflation, the NIH budget has declined 13% since 2003, and the NCI budget has declined 12% since 2004—a decrease of $500 million in real dollars. As a result, fewer research projects are funded, fewer patients can participate in clinical trials, and young physicians considering a career in cancer research will find it much more difficult to receive research funding.
To accelerate the pace of discovery, ASCO and others in the cancer community are calling for an increase in NIH funding of at least $2 billion to reverse the effects of flat funding, keep pace with medical research inflation, and maintain the nation's world-class research infrastructure. Over the longer term, greater increases in funding will be needed to take full advantage of the many basic science discoveries waiting to be translated into new cancer treatments for patients.
Remove Barriers to Participation in Cancer Clinical Trials
Patient participation in cancer clinical trials is essential to the search for new treatments. For patients themselves, it is an opportunity to access new approaches before they are widely available, receive high-quality care, and help future generations of patients.
To encourage and increase patient participation in cancer clinical trials, ASCO recommends the following strategies:
Provide coverage for patients participating in clinical trials. Although participation in clinical trials can represent a reasonable option, Medicare and private insurers may deny coverage for some or all routine patient care costs associated with clinical trials, arguing that such care is experimental and thus not a covered benefit. Without assurance of coverage, however, patients, fearing significant out-of-pocket costs, may choose not to participate in clinical trials.
For more than a decade, ASCO and others in the patient advocacy community have sought to reform health plans' clinical trials policies. Such efforts have resulted in reforms in Medicare payment policy and in legislation to ensure clinical trials coverage in more than 20 states. These federal, state, and private-sector initiatives reflect widespread recognition that clinical trials coverage is a critical element of quality cancer care. However, Medicare policy is inconsistently applied and many states still do not require private insurance coverage of clinical trials, leaving a significant number of cancer patients beyond the reach of these reforms.
ASCO supports laws and guidelines that require public and private insurers in every state to cover participation in cancer clinical trials that: (1) provide treatment with a therapeutic intent, 2 are conducted under a written protocol, and 3 have undergone scientific review by a group of independent and qualified experts.
Bring clinical trials to patients in the community setting. The vast majority of people with cancer—nearly 80%—receive cancer care in an oncologist's office close to their home, rather than at large academic cancer centers or hospitals. To increase patient participation in clinical trials, the involvement of community oncology practices is therefore critical.
Currently, NCI's clinical trial per-case reimbursement rate covers only one third of the cost of patient participation in a clinical trial, so some community practices (as well as academic centers and hospitals) may struggle to find ways to cover the remaining costs. ASCO is calling for funding in the NCI budget to reimburse for the full cost of participating in NCI-sponsored cancer clinical trials.
Ensure that clinical trials include ethnically diverse participants and the elderly. Minority patients, the elderly, and society as a whole benefit when clinical trials include diverse populations. Research indicates that greater participation from minority and other under-represented populations in clinical trials would help guide doctors on how to treat diseases that disproportionately affect these populations.
Studies show that racial minorities and the elderly often are reluctant to or are not provided the opportunity to participate in clinical trials, limiting knowledge about how cancer affects different races, ethnicities, and ages, and limiting our understanding of the most effective treatment options for these groups. Potential reasons for low participation in clinical trials include lack of awareness, low health literacy, cost of care, lack of health insurance, language differences, and mistrust of the medical establishment.
ASCO is developing strategies to make clinical trials more accessible, such as translating information for patients that do not speak English as a primary language. In addition, ASCO's Clinical Trials Participation Awards program is recognizing and documenting the approach of practices that are successfully engaging under-represented populations in clinical trials.
Expanding access to clinical trials—and to care—for minority patients is enhanced by the presence of physicians from minority backgrounds. For this reason, ASCO is partnering with Susan G. Komen for the Cure on its Diversity in Oncology Initiative, with the goal of diversifying the oncology work force.
ASCO joins the cancer community in calling for increased diversity in clinical trials and support for minority medical students who want to study oncology. For more information about ASCO's policy positions related to cancer research funding and clinical trials, visit www.asco.org/ASCO/Research+Policy.
Footnotes
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Barnett Kramer, Journal of the National Cancer Institute (C); Derek Raghavan, Bristol-Myers Squibb Co (C); Howard Sandler, Medscape (U), ITA Partners (C), Mitos (C) Consultant or Advisory Role: Beth Karlan, Genzyme (C), Amgen Inc (C), Tigris (C); George Demetri, Alnylam (C), Idera (C), Zymogenetics (C), ZioPharm (C), Daiichi-Sankyo (C), Amgen Inc (C), Bayer Pharmaceuticals (C), Merck-Serono (C), Pfizer Inc (C), Ariad (C), Plexxikon (C), Novartis, Genentech, Johnson & Johnson, Infinity (C); Mark Kris, GlaxoSmithKline (C), Merck & Co (C), Eli Lilly & Co (C), MGI Pharma (C), Pfizer Inc (C), Bayer Pharmaceuticals (C), Bristol-Myers Squibb Co (C), Boehringer Ingelheim (C), Novartis (C); Maurie Markman, Eli Lilly & Co (C), Genentech (C), Telek (C), GlaxoSmithKline (C), Cellgene (C), CTI (C), Ortho Biotech (C); Robert Mayer, Celgene (C); David Pfister, Sanofi-aventis (C); Derek Raghavan, YM Biosciences (U), Revolution Health Care Website (C), GlaxoSmithKline (C), Isis Pharmaceuticals (C), Schering-Plough (C); Gregory Reaman, Enzon Pharmaceuticals (C); Howard Sandler, Sanofi-aventis (C), TAP (C), General Electric (C), Genentech (C), Calypso (C); Richard L. Schilsky, Roswell Park Cancer Institute (C), Ontario Institute of Cancer Research (C), University of California at San Francisco (C), University of Texas Southwestern Medical Center-Simmons Cancer Center (C), University of North Carolina-Chapel Hill GI SPORE (C), Novartis (U), Dana Farber Cancer Institute (C), AdventRx Pharmaceuticals (C), Fred Hutchinson Cancer Research Center (C), National University of Singapore (C), M. D. Anderson Cancer Center (C) Stock Ownership: George Demetri, Coley Pharmaceutical Group; Howard Sandler, Amgen Inc, Genentech, Dendreon, Cytogen Honoraria: Julie Gralow, Roche, Novartis, Genentech; Eric Winer, Amgen Inc, Genomic Health; Beth Karlan, GlaxoSmithKline, Genentech, Eli Lilly & Co; George Demetri, PharmaMar, Pfizer, Novartis; Patricia Ganz, Novartis, Roche, Ortho Biotech, Amgen Inc, Pfizer; Maurie Markman, Telek, Ortho Biotech, Eli Lilly & Co, Genentech, CTI, Bristol-Myers Squibb Co, Merck & Co; Howard Sandler, Sanofi-aventis, AstraZeneca, Amgen Inc; Linda Vahdat, Bristol-Myers Squibb Co Research Funding: Julie Gralow, Bristol-Myers Squibb Co, Sanofi aventis, Genentech, Bayer, Amgen Inc, Novartis, Roche; Eric Winer, Aventis, Genomic Health, Genentech, Pfizer, AstraZeneca, Aventis; Beth Karlan, Genentech, Unither Pharmaceuticals; Patrick Loehrer, Eli Lilly & Co, Novartis, AstraZeneca, Imclone; George Demetri, Bristol-Myers Squibb Co, Johnson & Johnson, Genentech, Daiichi–Sankyo, Amgen Inc, Novartis, Pfizer, Infinity, PharmaMar, Ariad; Patricia Ganz, Amgen Inc; Derek Raghavan, Eli Lilly & Co; Howard Sandler, Sanofi-aventis Expert Testimony: George Demetri, Novartis (U), Ariad (U), Infinity (U), Johnson & Johnson (U), PharmaMar (U), Pfizer (U); Mark Kris, AstraZeneca (C) Other Remuneration: Mark Kris, Sanofi-aventis
AUTHOR CONTRIBUTIONS
Conception and design: Eric Winer, Julie Gralow, Lisa Diller, Beth Karlan, Patrick Loehrer, Lori Pierce
Collection and assembly of data: Eric Winer, Julie Gralow, Lisa Diller, Beth Karlan, Patrick Loehrer, Lori Pierce, George Demetri, Patricia Ganz, Barnett Kramer, Mark Kris, Robert Mayer, David Pfister, Derek Raghavan, Scott Ramsey, Gregory Reaman, Howard Sandler, Raymond Sawaya, Lynn Schuchter, John Sweetenham, Linda Vahdat
Data analysis and interpretation: Eric Winer, Julie Gralow, Lisa Diller, Beth Karlan, Patrick Loehrer, Lori Pierce, George Demetri, Patricia Ganz, Barnett Kramer, Mark Kris, Robert Mayer, David Pfister, Derek Raghavan, Scott Ramsey, Gregory Reaman, Howard Sandler, Raymond Sawaya, Lynn Schuchter, John Sweetenham, Linda Vahdat
Manuscript writing: Eric Winer, Julie Gralow, Lisa Diller, Beth Karlan, Patrick Loehrer, Lori Pierce, George Demetri, Patricia Ganz, Barnett Kramer, Mark Kris, Robert Mayer, David Pfister, Derek Raghavan, Scott Ramsey, Gregory Reaman, Howard Sandler, Raymond Sawaya, Lynn Schuchter, John Sweetenham, Linda Vahdat
Final approval of manuscript: Eric Winer, Julie Gralow, Lisa Diller, Beth Karlan, Patrick Loehrer, Lori Pierce, George Demetri, Patricia Ganz, Barnett Kramer, Mark Kris, Maurie Markman, Robert Mayer, David Pfister, Derek Raghavan, Scott Ramsey, Gregory Reaman, Howard Sandler, Raymond Sawaya, Lynn Schuchter, John Sweetenham, Linda Vahdat
REFERENCES
- 1.Rummel MJ, Atta J, Welslau M, et al. Bendamustine and rituximab (BR) are effective in the treatment of relapsed or refractory indolent and mantle-cell lymphomas: Long-term follow-up of a phase II study. J Clin Oncol. 2007;25(suppl):18S. abstr 8034. [Google Scholar]
- 2.Younes A, Forero-Torres A, Bartlett NL, et al. Objective responses in a phase I dose-escalation study of SGN-35, a novel antibody-drug conjugate (ADC) targeting CD30, in patients with relapsed or refractory Hodgkin lymphoma. J Clin Oncol. 2008;26(suppl):460s. abstr 8526. [Google Scholar]
- 3.Goss PE, Ingle JN, Pater JL, et al. Late extended adjuvant treatment with letrozole improves outcome in women with early-stage breast cancer completing 5 years of tamoxifen. J Clin Oncol. 2008;26:1948–1955. doi: 10.1200/JCO.2007.11.6798. [DOI] [PubMed] [Google Scholar]
- 4.Muss HB, Tu D, Ingle JN, et al. Efficacy, toxicity and quality of life in older women with early-stage breast cancer treated with letrozole or placebo after 5 years of tamoxifen: NCIC CTG Intergroup Trial MA.17. J Clin Oncol. 2008;26:1956–1964. doi: 10.1200/JCO.2007.12.6334. [DOI] [PubMed] [Google Scholar]
- 5.Peto R, Davies C. ATLAS (Adjuvant Tamoxifen, Longer Against Shorter): International randomized trial of 10 versus 5 years of adjuvant tamoxifen among 11,500 women preliminary results. the 30th Annual San Antonio Breast Cancer Symposium; December 13–16, 2007; San Antonio, TX. Presented at. [Google Scholar]
- 6.Gray RG, Rea DW, Handley K, et al. ATTom (adjuvant Tamoxifen—To offer more?): Randomized trial of 10 versus 5 years of adjuvant tamoxifen among 6,934 women with estrogen receptor-positive (ER+) or ER untested breast cancer—Preliminary results. J Clin Oncol. 2008;26(suppl):10s. abstr 513. [Google Scholar]
- 7.Gnant M, Mlineritsch B, Schippinger W, et al. Adjuvant ovarian suppression combined with tamoxifen or anastrozole, alone or in combination with zoledronic acid, in premenopausal women with hormone-responsive, stage I and II breast cancer: First efficacy results from ABCSG-12. J Clin Oncol. 2008;26(suppl):6s. abstr LBA4. [Google Scholar]
- 8.Reference deleted [Google Scholar]
- 9.Reference deleted [Google Scholar]
- 10.Thomas ES, Gomez HL, Li RK, et al. Ixabepilone plus capecitabine for metastatic breast cancer progressing after anthracycline and taxane treatment. J Clin Oncol. 2007;25:5210–5217. doi: 10.1200/JCO.2007.12.6557. [DOI] [PubMed] [Google Scholar]
- 11.Cloughesy TF, Prados MF, Mikkelsen T, et al. A phase II, randomized, non-comparative clinical trial of the effect of bevacizumab (BV) alone or in combination with irinotecan (CPT) on 6-month progression free survival (PFS6) in recurrent, treatment-refractory glioblastoma (GBM) J Clin Oncol. 2008;26(suppl):91s. abstr 2010b. [Google Scholar]
- 12.Van Cutsem E, Lang I, D'haens G, et al. KRAS status and efficacy in the first-line treatment of patients with metastatic colorectal cancer (mCRC) treated with FOLFIRI with or without cetuximab: The CRYSTAL experience. J Clin Oncol. 2008;26(suppl):5s. abstr 2. [Google Scholar]
- 13.Neuhaus P, Riess H, Post S, et al. CONKO-001: Final results of the randomized, prospective, multicenter phase III trial of adjuvant chemotherapy with gemcitabine versus observation in patients with resected pancreatic cancer (PC) J Clin Oncol. 2008;26(suppl):214s. abstr LBA4504. [Google Scholar]
- 14.Loehrer PJ, Powell ME, Cardenes HR, et al. A randomized phase III study of gemcitabine in combination with radiation therapy versus gemcitabine alone in patients with localized, unresectable pancreatic cancer: E4201. J Clin Oncol. 2008;26(suppl):214s. doi: 10.1097/COC.0b013e3181e9c103. abstr 4506. [DOI] [PubMed] [Google Scholar]
- 15.Sargent DJ, Marsoni S, Thibodeau SN, et al. Confirmation of deficient mismatch repair (dMMR) as a predictive marker for lack of benefit from 5-FU based chemotherapy in stage II and III colon cancer (CC): A pooled molecular reanalysis of randomized chemotherapy trials. J Clin Oncol. 2008;26(suppl):180s. abstr 4008. [Google Scholar]
- 16.Attard G, Reid AHM, Yap TA, et al. Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, confirms that castration-resistant prostate cancer commonly remains hormone driven. J Clin Oncol. 2008;26:4563–4571. doi: 10.1200/JCO.2007.15.9749. [DOI] [PubMed] [Google Scholar]
- 17.Saad F, Hotte SJ, North SA, et al. A phase II randomized study of custirsen (OGX-011) combination therapy in patients with poor-risk hormone refractory prostate cancer (HRPC) who relapsed on or within six months of 1st-line docetaxel therapy. J Clin Oncol. 2008;26(suppl):250s. abstr 5002. [Google Scholar]
- 18.Beral V, Doll R, Hermon C, et al. Ovarian cancer and oral contraceptives: Collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet. 2008;371:303–314. doi: 10.1016/S0140-6736(08)60167-1. [DOI] [PubMed] [Google Scholar]
- 19.Chaturvedi AK, Engels EA, Anderson WF, et al. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612–619. doi: 10.1200/JCO.2007.14.1713. [DOI] [PubMed] [Google Scholar]
- 20.Gupta-Abramson V, Troxel AB, Nellore A, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol. 2008;26:4714–4719. doi: 10.1200/JCO.2008.16.3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen EE, Rosen LS, Vokes EE, et al. Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: Results from a phase II study. J Clin Oncol. 2008;26:4708–4713. doi: 10.1200/JCO.2007.15.9566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sherman SI, Wirth LJ, Droz JP, et al. Motesanib diphosphate in progressive differentiated thyroid cancer. N Engl J Med. 2008;359:31–42. doi: 10.1056/NEJMoa075853. [DOI] [PubMed] [Google Scholar]
- 23.Pfister DG, Fagin JA. Refractory thyroid cancer: A paradigm shift in treatment is not far off. J Clin Oncol. 2008;26:4701–4704. doi: 10.1200/JCO.2008.17.3682. [DOI] [PubMed] [Google Scholar]
- 24.Pirker R, Szczesna S, von Powel J, et al. FLEX: A randomized, multicenter, phase III study of cetuximab in combination with cisplatin/vinorelbine (CV) versus CV alone in the first-line treatment of patients with advanced non–small-cell lung cancer (NSCLC) J Clin Oncol. 2008;26(suppl):6s. abstr 3. [Google Scholar]
- 25.Maheswaran S, Sequist LV, Nagrath S, et al. Detection of mutations in EGFR in circulating lung-cancer cells. N Engl J Med. 2008;359:366–377. doi: 10.1056/NEJMoa0800668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mulrooney D, Yeazel M, Mitby P, et al. Cardiovascular disease in adult survivors of childhood and adolescent cancer: A report from the Childhood Cancer Survivor Study (CCSS) J Clin Oncol. 2008;26(suppl):504s. abstr 9509. [Google Scholar]
- 27.Mosse YP, Longo L, Laudenslager M, et al. Use of a genome-wide linkage screen to identify a hereditary neuroblastoma predisposition locus at chromosome 2p24-23. J Clin Oncol. 2008;26(suppl):541s. abstr 10010. [Google Scholar]
- 28.Shankar SM, Chen L, Zhou T, et al. Risk of therapy-related myelodysplasia and acute myeloid leukemia (t-MDS/AML) in children exposed to alkylating agents, anthracyclines, platinum compounds and epipodophyllotoxins: A report from Children's Oncology Group (COG) J Clin Oncol. 2008;26(suppl):540s. abstr 10005. [Google Scholar]
- 29.Children's Oncology Group. Borowitz MJ, Devidas M, et al. Prognostic significance of end consolidation minimal residual disease (MRD) in childhood acute lymphoblastic leukemia (ALL): A report from the Children's Oncology Group (COG) J Clin Oncol. 2008;26(suppl):539s. abstr 10000. [Google Scholar]
- 30.Olmos D, Okuno S, Schuetze SM, et al. Safety, pharmacokinetics and preliminary activity of the anti-IGF-IR antibody CP-751,871 in patients with sarcoma. J Clin Oncol. 2008;26(suppl):553s. doi: 10.1016/S1470-2045(09)70354-7. abstr 10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiebe L, Kasza KE, Maki RG, et al. Activity of sorafenib (SOR) in patients (pts) with imatinib (IM) and sunitinib (SU)-resistant (RES) gastrointestinal stromal tumors (GIST): A phase II trial of the University of Chicago Phase II Consortium. J Clin Oncol. 2008;26(suppl):553s. abstr 10502. [Google Scholar]
- 32.Eggermont AM, Suciu S, Santinami M, et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: Final results of EORTC 18991, a randomised phase III trial. Lancet. 2008;372:117–126. doi: 10.1016/S0140-6736(08)61033-8. [DOI] [PubMed] [Google Scholar]
- 33.McDermott DF, Sosman JA, Gonzalez R, et al. Double-blind randomized phase II study of the combination of sorafenib and dacarbazine in patients with advanced melanoma: A report from the 11715 Study Group. J Clin Oncol. 2008;26:2178–2185. doi: 10.1200/JCO.2007.14.8288. [DOI] [PubMed] [Google Scholar]
- 34.Vestergaard ME, Macaskill P, Holt PE, et al. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: A meta-analysis of studies performed in a clinical setting. Br J Dermatol. 2008;159:669–676. doi: 10.1111/j.1365-2133.2008.08713.x. [DOI] [PubMed] [Google Scholar]
- 35.Lucia MS, Epstein JI, Goodman PJ, et al. Finasteride and high-grade prostate cancer in the Prostate Cancer Prevention Trial. J Natl Cancer Inst. 2007;99:1375–1383. doi: 10.1093/jnci/djm117. [DOI] [PubMed] [Google Scholar]
- 36.Cohen YC, Liu KS, Heyden NL, et al. Detection bias due to the effect of finasteride on prostate volume: A modeling approach for analysis of the Prostate Cancer Prevention Trial. J Natl Cancer Inst. 2007;99:1366–1374. doi: 10.1093/jnci/djm130. [DOI] [PubMed] [Google Scholar]
- 37.Warren JL, Mariotto AB, Meekins A, et al. Current and future utilization of services from medical oncologists. J Clin Oncol. 2008;26:3242–3247. doi: 10.1200/JCO.2007.14.6357. [DOI] [PubMed] [Google Scholar]
- 38.Wharam JF, Galbraith AA, Kleinman KP, et al. Cancer screening before and after switching to a high-deductible health plan. Ann Intern Med. 2008;148:647–655. doi: 10.7326/0003-4819-148-9-200805060-00004. [DOI] [PubMed] [Google Scholar]
- 39.Warren JL, Yabroff KR, Meekins A, et al. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888–897. doi: 10.1093/jnci/djn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfister D, Vickers A, Deng G, et al. Acupuncture for pain and dysfunction after neck dissection: Preliminary results of a randomized controlled trial. J Clin Oncol. 2008;26(suppl):320s. doi: 10.1200/JCO.2009.26.9860. abstr 6016. [DOI] [PMC free article] [PubMed] [Google Scholar]