Abstract
Home-based health services remain one of the fastest-growing sectors in the Canadian healthcare system. While there have been studies addressing the characteristics of home care users and the determinants of utilization, the costs associated with the use of home care services, particularly private costs, have been largely neglected. To gain a comprehensive appreciation of the financing context in which ambulatory and home-based care is delivered and received, it is imperative to assess costs incurred by clients and their family/friends. Accordingly, this study examined the magnitude and determinants of the share of private costs incurred by Ontarians who received in-home publicly financed services and by their unpaid caregivers. The private share of costs was found to be 75%. Determinants of the private share included participants’ gender, martial status, functioning in activities of daily living and the type and length of service received. These findings suggest that recipients of home-based health services in Ontario may bear an economic burden when care is shifted into the home setting.
Abstract
Les services de santé à domicile demeurent un des secteurs du système de soins de santé canadien qui connaît la croissance la plus rapide. Tandis que des études ont été effectuées sur les caractéristiques des prestataires de soins à domicile et les déterminants de l’utilisation, les coûts associés à l’utilisation des services de soins à domicile – en particulier les coûts privés – ont été en grande partie négligés. Afin de mieux apprécier le contexte de financement dans lequel les soins ambulatoires et les soins à domicile sont fournis et reçus, il est absolument essentiel d’évaluer les coûts défrayés par les clients et leurs aidants naturels (parents et amis). Par conséquent, cette étude a examiné l’ampleur et les déterminants de la proportion des coûts privés engagés par les Ontariens qui ont reçu des soins à domicile financés par l’État et par leurs aidants naturels non rémunérés. On a constaté que la part privée des coûts s’élevait à 75 %. Parmi les déterminants de la part privée, citons le sexe des clients, leur état civil, leur degré de participation aux activités de la vie quotidienne, ainsi que le type et la durée des services reçus. Ces résultats suggèrent que les personnes qui reçoivent des soins de santé à domicile en Ontario pourraient avoir à assumer un fardeau financier lors-que ces soins sont transférés à domicile.
Introduction
Over the past 30 years, home-based care has been one of the fastest-growing sectors in Canadian healthcare (Coyte and McKeever 2001). It is estimated that more than 500,000 Ontarians receive home-based services annually (Government of Ontario 2006). The Ontario government continues to increase funding to the home care sector. In 2004, C$1.3 billion was allocated to home-based healthcare, and this level of expenditure is expected to expand to C$1.7 billion by 2007/2008. It is projected that as a result of this funding increase, the population receiving in-home care will increase by almost 20% over four years (from 2004–2008) (Government of Ontario 2004).
The provision of home-based health services is provincially regulated in Canada; a unique medley of public and private services is found in each province and territory (MacAdam 2000). Prior to January 1, 2007, 42 Community Care Access Centres (CCACs) operated to facilitate public access to government-funded home and community care services throughout Ontario (Ministry of Health and Long-Term Care 2005b). Although these facilities have since been amalgamated into 14 organizations, CCACs continue to provide access to a range of services such as nursing and personal support, homemaking, meal deliveries and transportation, with the intent of providing comprehensive healthcare. However, because public sector services may not meet the needs and preferences of clients, some individuals also pay out of pocket for ambulatory and home-based services or rely on family members for the provision of care. The extent to which this privately financed component of care supports the delivery of home-based care remains unknown. Consequently, the first objective of this study was to quantify the magnitude of the share of total home care costs that are financed privately.
Canadian research addressing home-based care has focused primarily on the patterns (Alcock et al. 1998; Coyte and Young 1999; Forbes and Janzen 2004; Hall and Coyte 2001; Mitchell et al. 2004; Peterson et al. 2005; Wilkins and Park 1998) and determinants (Forbes and Janzen 2004; Forbes et al. 2003; Hall and Coyte 2001; Hawranik 1998; Hawranik and Strain 2001; Morgan et al. 2002; Penning 1995) of utilization. The home-based care population has been described as predominantly female and elderly (i.e., aged 65 or older) (Alcock et al. 1998; Coyte and Young 1999; Mitchell et al. 2004; Wilkins and Park 1998), with care recipients having two or more chronic conditions (Wilkins and Park 1998), being single (Mitchell et al. 2004) and living with others (Alcock et al. 1998; Wilkins and Park 1998). The determinants of home-based care have been identified as age (Forbes et al. 2003; Hall and Coyte 2001; Hawranik 1998; Hawranik and Strain 2001; Wilkins and Park 1998), gender (Forbes et al. 2003), health status (Forbes et al. 2003; Hall and Coyte 2001; Hawranik and Strain 2001; Wilkins and Park 1998), activities of daily living functioning (Hall and Coyte 2001; Hawranik 1998; Hawranik and Strain 2001; Penning 1995; Wilkins and Park 1998), cohabitation status (Forbes et al. 2003; Hawranik 1998; Hawranik and Strain 2001; Penning 1995; Wilkins and Park 1998), income (Forbes et al. 2003; Wilkins and Park 1998) and geographic location of residence (rurality) (Forbes and Janzen 2004; Penning 1995). Several Canadian studies have assessed the determinants of utilization of specific home-based services, such as nursing (Forbes et al. 2003; Hawranik 1998; Hawranik and Strain 2001; Penning 1995), personal-support care (Forbes and Janzen 2004; Hawranik 1998; Hawranik and Strain 2001; Penning 1995), homemaking (Forbes et al. 2003; Hawranik 1998; Hawranik and Strain 2001) and meal deliveries (Hawranik and Strain 2001); however, most have focused on elderly clients and those with cognitive impairment (Hawranik 1998; Hawranik and Strain 2001; Penning 1995). Although historically, the majority of home-based care clients have been older individuals at risk for admission to long-term care facilities, home-based care is increasingly provided to short-term, acute care clients. Given that these two client types typically access home-based care for different reasons, their needs are often quite different. As such, the extent to which previous studies’ findings apply to non-cognitively impaired clients and younger, short-term clients is unknown (Chappell et al. 2004; Di Matteo and Di Matteo 2001; Hawranik 1998; Hawranik and Strain 2001; Mitchell et al. 2004; Morgan et al. 2002; Penning 1995; Peterson et al. 2005). Hence, the second objective of this study was to determine the extent to which short-term and long-term clients differ with respect to their use of privately financed home-based services.
Finally, while studies to date provide insight into the demographic and clinical characteristics of the home care environment, the majority neglect the financing environment. Of the studies that have addressed costs (Alcock et al. 1998; Chappell et al. 2004; Di Matteo and Di Matteo 2001; Guerriere, Tullis et al. 2006), very few have focused on privately financed care (Browne et al. 1990; Guerriere, Tullis et al. 2006), only one has considered the determinants of public costs (Alcock et al. 1998) and none has explored the determinants of privately financed care. To gain a comprehensive appreciation of the financing context in which ambulatory and home-based care is delivered and received, it is imperative to assess costs incurred by clients and their family and friends. Accordingly, the final objective of this study was to identify the determinants of the share of private costs. Specifically, the influence of nine determinants was considered: age, gender, marital status, number of chronic conditions, activities of daily living (ADL) functioning, rurality, education, income and type of services (e.g., nursing, personal support, etc.) and length of service (e.g., short-term vs. continuing care).
Methodology
Participant recruitment
Six Community Care Access Centres (CCACs), representing six distinct geographical regions across the province of Ontario, were used to recruit study participants. At each CCAC, a member of the administrative staff identified potential participants who met eligibility criteria. Individuals were eligible if they (1) were scheduled to receive or had been receiving publicly financed nursing and/or personal-support services, (2) were fluent in English (or had an available caregiver who was fluent in English) and (3) were at least 18 years of age. Individuals receiving palliative care were not eligible to participate. In addition, two groups of participants were recruited: those expected to receive short-term nursing and/or personal-support services (i.e., <90 days) (short-term clients); and those who were receiving nursing and/or personal-support services on a continuing basis (i.e., >90 days with no more than a one-week break in servicing within the 90-day period) (continuing care clients). Participants were purposefully sampled by group membership because they were expected to differ in terms of their demographic and clinical characteristics, health services utilization rates and total expenditures. Specifically, we anticipated short-term clients to be younger with acute conditions and continuing care clients to be older with chronic conditions. If the duration of care extended beyond 90 days for short-term participants, an intention-to-treat approach was used in that they continued to be classified as short-term participants.
Over the telephone, CCAC employees asked potential participants for their permission to be telephoned by the research assistant to discuss the study. CCAC recruiters contacted potential participants sequentially based on eligibility criteria; recruitment ceased once a sufficient number of participants were enrolled by the research assistant to satisfy sample sizes for each client group from each CCAC. To be enrolled, participants were required to provide verbal consent for participation and to complete a written consent form, which was mailed to them with a postage-paid envelope. Caregivers participated as proxy respondents when clients were cognitively or physically incapable of participating, when they were not fluent in English, or both.
Data collection
Interviews were conducted between 2003 and 2005. Each participant was contacted four times over four consecutive weeks for 15-minute telephone interviews. A four-week timeframe was selected in order to capture a period in which services were provided at the greatest intensity for clients who had an in-hospital referral, and to capture the variability in resource use for all participants (Coyte and Young 1999).
Four distinct data collection tools were used during interviews. The Ambulatory and Home Care Record (AHCR) was used during all interviews to measure health services utilization and clients’ and caregivers’ costs (Guerriere, Ungar et al. 2006). This instrument has been evaluated with a population of cystic fibrosis care recipients and has been shown to assess private and public healthcare costs, including home-based care costs, accurately. The psychometric properties of the AHCR have recently been published and show good to excellent agreement between participants’ reports and administrative data (kappa ranging from 0.41 to 1.00) (Guerriere, Ungar et al. 2006). Using the AHCR, participants were asked to recall their resource use over the previous week. Publicly financed resources include ambulatory and home-based consultations with healthcare providers, laboratory and diagnostic tests, medications covered by government-sponsored drug programs, and equipment and supplies provided by the CCACs. Private expenditures consisted of out-of-pocket costs, time costs and third-party insurance. “Out-of-pocket costs” refers to the amount of money clients and their families pay for medications, supplies, household help, healthcare professional appointments and travel expenses. “Time costs” refers to the monetary value assigned to the time dedicated to receiving and providing care by clients and their families/friends. Here, time costs were calculated for care provided over and above that which caregivers normally provide; this distinction is explicitly made within the AHCR. “Third-party insurance” refers to any costs claimed through a private insurance company.
During the first interview, a demographic data form was used to collect information on participants’ characteristics. In addition, a portion of the Canadian Community Health Survey’s (CCHS) Chronic Conditions module was used to assess participants’ health by identifying the number of chronic conditions experienced (Statistics Canada 2003). Finally, participants’ level of ADL functioning was determined through the Older American’s Resources and Services’ Activities of Daily Living Scale (ADLS). The ADLS consists of 15 items assessing the level of functioning for individuals who live at home. It provides a total score ranging from 2 (excellent functioning) to 6 (complete impairment). Testing of its psychometric properties indicates good inter-rater reliability (intraclass correlation coefficient ranged from 0.662 to 0.865) and content validity [Spearman’s r=.89; p=0.001]) (Fillenbaum 1988; Fillenbaum and Smyer 1981).
Data analysis
Total public expenditure was calculated for each participant. Costs for physician, laboratory and diagnostic services were determined using the Ontario Health Insurance Plan database. Rates determined by home care agencies were used to determine costs associated with consultations by healthcare professionals (other than physicians) and laboratory services. Nursing and homemaking visits were valued at $62.30 and $32.04 per hour, respectively. Prescription medication costs were derived using prices in the Ontario Drug Benefit Formulary (as of July 2005) (Ministry of Health and Long-Term Care 2005a).
Private expenditures over the four-week period were calculated as an aggregation of out-of-pocket costs, unpaid time costs and costs claimed through third-party insurance. The cost of travel by car was calculated using the cost per kilometre ($0.43/km) as reported by the Canadian Automobile Association (2006) and was treated as an out-of-pocket expense. A total out-of-pocket cost was calculated for each participant by summing the amounts reported and then subtracting any reimbursements received from drug plans or insurance. Time costs were determined by assigning a monetary value to each unit of time, using the human capital approach (Rice and MacKenzie 1989; Torgerston et al. 1994). The human capital approach applies current average earnings by age and gender to lost time. To value time lost from work, age- and sex-based earnings estimates from the 2001 Census were used. These earnings were adjusted for 15% nominal earnings growth to 2004 (Statistics Canada n.d.), then multiplied by 1.20 to account for employer-paid benefits (Chan et al. 1996) and then further multiplied by 52/46 to account for vacation days and holidays (Guerriere, Tullis et al. 2006). Time lost from work or leisure was valued using the estimated earnings of a homemaker from the 2001 Census; this amount was adjusted for benefits, vacation days and holidays. Finally, third-party insurance costs were calculated by summing the amounts reimbursed to participants.
Total health expenditure was computed as the sum of public and private expenditures. The private share is defined as the proportion of the total health expenditures that were financed by the private sector, calculated by dividing private expenditures, comprising out-of-pocket, third-party and time costs, by total expenditures.
Univariate analyses were conducted with the private share and each of the nine determinants considered: age, gender, marital status, number of chronic conditions, activities of daily living (ADL) functioning, rurality, education, income and type of services (e.g., nursing, personal support, etc.) and length of service (e.g., short-term vs. continuing care). The results of these analyses are found in Table 1.
TABLE 1.
Results of univariate analyses with the private share
| Variable | Correlation (r) | P-value |
|---|---|---|
| Age | 0.154 | 0.004 |
| Gender | 0.049 | 0.267 |
| Marital status | 0.081 | 0.066 |
| Education level | 0.122 | 0.105 |
| Income | 0.099 | 0.287 |
| ADL level | 0.454 | <.0001 |
| Number of chronic conditions | 0.195 | <0.001 |
| Rurality | 0.047 | 0.284 |
| Service group membership | 0.254 | <0.0001 |
A backward, stepwise multiple linear regression analysis was then used to assess which determinants and interactions were associated with variations in the private share. As is standard in health services research with a sample size similar to ours, a p-value of 0.05 was used to identify significant determinants. For service group membership, participants were stratified into five subgroups: continuing personal support, continuing nursing, continuing nursing and personal support, short-term nursing, and short-term nursing and personal support. Since the home-based care population has been characterized as predominantly female (Alcock et al. 1998; Coyte and Young 1999; Mitchell et al. 2004; Wilkins and Park 1998), interactions between each of the determinants and gender were included. Furthermore, because income has been found to be a determinant of utilization (Forbes et al. 2003; Wilkins and Park 1998), interactions between income and service group membership, as well as education and service group membership, were also included. Finally, the interaction term for ADL level and number of chronic conditions was included as an additional indicator of need.
The residuals from the backward regression analysis were not random and thus were in violation of the classic assumptions underlying regression analyses, specifically the assumption of homoskedasticity. Therefore, a regression analysis using robust standard errors was conducted (Moller et al. 2005). Results from the regression analysis with robust standard errors are reported herein. Finally, regressions were done to determine which category of private expenditures, public expenditures or both was associated with the observed variation in the private share (see Results).
Results
Clients and caregivers: characteristics
Between 2003 and 2005, 869 individuals were identified as eligible for study participation. Seventy per cent of those eligible and approached (n=612) agreed to participate, and of those, 84% (514) completed the study. Proxy respondents who completed the study (n=102) consisted of clients’ spouses (52%), children (33%), parents (7%) and other relatives (8%). Among those who did not complete the study, 80 (82%) withdrew and 18 (18%) no longer met eligibility criteria at the time of their first interview. Reasons for withdrawal included a change of decision about participating (34%), health deterioration (15%), lack of time (8%) and death (3%). A further 40% could not be contacted for interviews. Other than being older than continuing care clients who completed the study (p<0.05), the withdrawals were not statistically different from participants in terms of demographic characteristics and service group membership.
Short-term (n=243) and continuing care (271) clients were distributed across service categories as follows: continuing care personal support (88), continuing care nursing (96), continuing care nursing and personal support (87), short-term personal support (0), short-term nursing (228) and short-term nursing and personal support (15). As indicated in Table 2, short-term and continuing care clients differed with respect to their demographic characteristics. Specifically, short-term clients were more likely to be younger, married and employed men with higher incomes and levels of education, but fewer limitations in ADLs than continuing care clients. These findings support our initial hypothesis that two distinct client groups exist within the home care population.
TABLE 2.
Participant characteristics
| Short-Term (n=243) | Continuing Care (n=271) | |
|---|---|---|
| Age (mean) | 60 | 70 |
| Female | 54.0% | 63.0% |
| Marital status* | ||
| Married | 69.0% | 43.9% |
| Never married | 9.5% | 13.3% |
| Divorced or widowed | 21.5% | 42.8% |
| Education level+ | ||
| Less than high school | 11.3% | 18.1% |
| Some or all high school | 45.4% | 48.3% |
| Some or all college | 20.8% | 18.1% |
| Some or all university or postgraduate education | 22.5% | 15.5% |
| Employment status | ||
| Employed | 33.3% | 6.3% |
| Retired/not working due to disability | 56.8% | 88.2% |
| Never employed outside of home | 9.9% | 5.5% |
| Income groupΦ | ||
| ≤ $25,000 | 26.8% | 59.8% |
| $25,001- $45,000 | 27.9% | 25.3% |
| $45,001 – $65,000 | 15.7% | 9.8% |
| ≥ $65 001 | 29.6% | 5.1% |
| ADL levelβ | ||
| Excellent | 16.2% | 5.7% |
| Mild impairment | 35.4% | 22.6% |
| Moderate impairment | 21.7% | 23.0% |
| Severe impairment | 16.3% | 17.0% |
| Total impairment | 10.4% | 31.7% |
n = 242 for Short-term clients
n = 240 for Short-term clients, n = 265 for Continuing care clients
n = 179 for Short-term clients, n = 194 for Continuing care clients
n = 240 for Short-term clients, n = 265 for Continuing care clients
There were regional differences in the study participants. Across the six geographic regions in Ontario, short-term clients differed with respect to education (p<0.05) and rurality (p<0.0001). Regional differences among continuing care clients included age (p<0.05), education (p<0.05) and rurality (p<0.0001). A higher proportion of married continuing care clients was also identified in one geographic region (p<0.05).
Clients received care from a spouse or significant other (235), child (212), friend or neighbour (103), sibling (40), parent (36), other relative (e.g., grandchild, niece/nephew, cousin, aunt, etc.) (34) and other (e.g., landlady, pastor) (5). The mean number of caregivers per client was 1.63; 62% were female (415), and their mean age was 53 years (range, 6–88). The youngest reported caregiver, aged 6, assisted his mother with household chores.
Expenditures
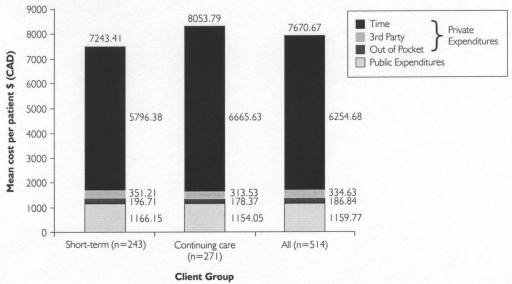
Among short-term clients, 222 (91%) reported out-of-pocket costs, 243 (100%) reported time costs and 70 (29%) reported having claimed costs from a private insurance provider. Of continuing care clients, 259 (96%) reported out-of-pocket costs, 271 (100%) reported time costs and 55 (20%) reported private third-party costs. The mean out-of-pocket costs, time costs, third-party costs, public costs and total costs incurred by short-term and continuing care clients were compared (see Figure 1). Only time costs were found to be statistically significantly different (p=0.02), with continuing care clients reporting greater time costs. The proportion of time costs attributed to care recipients and caregivers was 5% and 95%, respectively.
FIGURE 1.
Mean costs per patient by client group
Determinants
The mean private share for all clients was 75%. Four variables were the primary determinants of variations in the private share: gender, service group membership, ADL level and marital status. The effect of these determinants is described in detail below and presented in Table 3. No interaction terms accounted for statistically significant variations in the private share.
TABLE 3.
Determinants of the private share
| Determinant | Est. beta | Std. error* | 95% confidence interval* | P-value* |
|---|---|---|---|---|
| Female | –0.036 | 0.017 | –0.003 to –0.069 | 0.037 |
|
Service group Continuing care PSW (ref. group) Short-term nursing Continuing care both Continuing care nursing Short-term both |
- 0 –0.065 –0.067 –0.092 –0.101 |
- - 0.015 0.021 0.024 0.015 |
- - –0.036 to –0.094 –0.026 to –0.108 –0.045 to –0.139 –0.072 to –0.130 |
< 0.001 - < 0.001 0.002 < 0.001 < 0.001 |
|
ADL level Excellent (reference group) Mild impairment Moderate impairment Severe impairment Total impairment |
- 0 0.140 0.180 0.245 0.267 |
- - 0.040 0.040 0.041 0.040 |
- - 0.062 to 0.218 0.102 to 0.258 0.165 to 0.325 0.189 to 0.345 |
< 0.001 - < 0.001 < 0.001 < 0.001 < 0.001 |
|
Marital status Never married (reference group) Divorced or widowed Married |
- 0 0.047 0.075 |
- - 0.030 0.028 |
- - –0.012 to 0.106 0.020 to 0.130 |
< 0.01 - 0.119 0.007 |
The robust estimate of the standard error is reported.
Males reported a higher private share than females. Males’ higher share was the result of having higher private expenditures than females and not the result of having lower public expenditures; the magnitude of public expenditures was not significantly different for males and females. Specifically, the higher private expenditures for males were associated with higher overall time costs (p=0.002). Males spent more time caring for themselves (p<0.001) and received more caregiver assistance (p=0.02) than females. In contrast, female clients reported more home help (p=0.05), suggesting that males and females received assistance for different activities.
Continuing care clients who received personal support had a higher private share than all other service groups (Table 4). The private share for those who received nursing care or nursing and personal support care on a short-term or continuing care basis did not differ significantly from each other. The higher private share for continuing care clients who received personal-support care was attributable to lower public expenditures (p<0.005) compared to all other service groups. Specifically, lower public home-based healthcare costs (p<0.004) were found to be responsible for the lower public expenditures of continuing care clients who received personal support compared to the other client groups. Participants did not differ by client group in terms of medication and supply costs. Ambulatory services costs were lower for continuing care clients who received personal support compared to short-term clients who received both nursing and personal support (p=0.02).
TABLE 4.
Magnitude of participants’ private share, by determinant
| Determinant (n) | Private share (%) |
|---|---|
| Gender | |
| Female (303) | 75 |
| Male (211) | 77 |
| Service group | |
| Continuing care nursing (96) | 70 |
| Short-term nursing (228) | 73 |
| Short-term both (15) | 78 |
| Continuing care both (87) | 80 |
| Continuing care personal support (88) | 84 |
| ADL level | |
| Excellent (54) | 55 |
| Mild impairment (145) | 71 |
| Moderate impairment (113) | 76 |
| Severe impairment (84) | 83 |
| Total impairment (109) | 85 |
| Marital status | |
| Unmarried (59) | 69 |
| Divorced or widowed (168) | 75 |
| Married (286) | 77 |
| Overall mean | 75 |
With each incremental rise in ADL limitation, the private share increased. Clients with an ADL level of 2 (excellent functioning), 3 (mild impairment), 4 (moderate impairment), 5 (severe impairment) and 6 (complete impairment) had a mean private share of 55%, 71%, 76%, 83% and 85%, respectively. This incremental increase in the private share is attributable to higher private expenditures (p<0.05). These larger shares were due to greater time costs (p<0.05). Public expenditure did not differ significantly by ADL level.
Married clients had a higher private share (77%) than those who were unmarried (69%) (p=0.007). This higher share was attributable to higher private expenditures by married clients than by unmarried clients (p=0.02). Total expenditure and public expenditures did not differ according to marital status. Furthermore, married clients reported greater time costs (p=0.03) due to greater caregiver and home-help costs (p<0.001). Private expenditures were not higher due to clients’ time costs, or medications and supplies costs. Being divorced or widowed was not found to be a determinant of private share; the private share of divorced or widowed clients (75%) did not differ significantly from that of those who were married or unmarried. Similarly, the private expenditures of divorced or widowed clients did not differ from those of married or unmarried clients.
Discussion
Although the Ontario government has made investing in home-based services a healthcare priority, such investment is varied within Canada. A national program for home-based health services does not presently exist (MacAdam 2000). Moreover, home-based health services are not covered under the principles of the Canada Health Act (1984). Consequently, each province and territory has its own definition, standards and mechanisms for the organization and delivery of home-based care. It is unknown whether current levels of investment across the country (and among regions within provinces) reflect local needs. This uncertainty has raised concerns regarding eligibility, cost, quality and accessibility of home-based health services in Canada.
This study examined the costs associated with providing and receiving home-based care in Ontario. By examining the share of private-to-total costs, it is the first study to evaluate who bears the economic burden when healthcare is shifted to the home setting. Moreover, by differentiating between short-term and continuing care clients, this study is the first to assess whether these two distinct home-based care recipient populations differ in terms of their use of resources. The magnitude of the private share of costs, that is, the share of private expenditure divided by overall expenditure, suggests that clients and their unpaid caregivers bear the greatest burden of cost when healthcare is delivered in the home. Specifically, 75% of healthcare costs were found to be financed by the private sector. Although both short-term and continuing care clients incurred similar overall costs, continuing care clients relied more heavily on informal, unpaid care.
Females were found to have a lower private share than males. Females had lower private expenditures because they spent less time caring for themselves and received less caregiver assistance than male clients. This finding is consistent with previous studies that found females to be less likely to receive care and more likely to provide care to others (Aykan 2003; Katz et al. 2000; Walter-Ginzburg et al. 2001). We conjecture that women may take on caregiver roles more often than men, as suggested by our survey of caregivers (62% were female), because they perceive activities related to caregiving to be their responsibility within the home. We also speculate that women are less likely to receive unpaid care because men may not assume the role of caregiver, women feel that they should be self-sufficient and care for themselves rather than rely on a family member, or a combination of these reasons. This finding suggests that female clients may not be receiving sufficient and satisfactory care in the home setting. Alternatively, it is possible that males receive care beyond their needs.
Married clients were found to have a higher private share than those who were unmarried. Further analysis revealed that married clients reported significantly more caregiver assistance and home help. This finding is consistent with previous findings that suggest living with at least one other person increases the likelihood of receiving assistance with instrumental ADLs (Chappell 1991). Further, this finding may suggest that a greater burden is placed on spouses when healthcare services are provided in the home. It may also reflect an inadequacy of home-based health services: spouses may be required to forgo other activities (work, leisure or both) to provide care, and unmarried clients may have unmet care needs that are not being appreciated. However, similar to the argument proposed for males, married individuals may receive more care than they need. Also of note, divorced or widowed clients may not have had a statistically different private share because they may have received more support than unmarried clients but less support than married clients; thus, they may have received an intermediate amount of care. Support may have been provided by children, as previous research has found children to be the most important source of care for elderly women (Aykan 2003).
Continuing care clients who received personal support had a higher private share than any other service group because of lower public home-based service expenditures. One explanation for this observation is that personal-support care is less costly than nursing care. However, these continuing, personal-support clients incurred similar private costs as other service groups. It is hypothesized that there may be a relationship between the length of time that services are provided and the amount of publicly financed service that is provided. The intensity of care provided may have an inverse relationship to the duration of service provision. Public home care agencies with limited resources may be unable to provide care with the same intensity to clients over time. In order to understand why continuing, personal-support clients appear to bear a greater cost burden, research is needed to examine the temporal relationship between the intensity and duration of home-based care.
As ADL limitations increased for clients, their private share also increased. The increasing private share was attributed to high private expenditures. Public expenditures did not differ significantly among clients, regardless of ADL limitations. It may be argued that public home-based health services are not providing adequate care to meet the needs of clients; clients with greater care needs are supplementing their public health services with privately financed care. This finding raises concerns regarding equity and accessibility of home-based health services. Furthermore, the priorities of public home-based care should be reviewed, as it appears that short-term clients or those who receive nursing services face a smaller private burden.
Although this study provides novel insights into the costs associated with home-based care, several limitations are noted. The study did not include individuals who rely solely on privately financed home-based services or who receive services other than nursing and personal support; study participants were recruited based on their receipt of publicly financed home-based nursing or personal-support care. In addition, as a consequence of our partnership with CCACs, we were unable to monitor directly how each CCAC employee identified eligible participants. As a result, our study sample may be subject to selection bias. Nonetheless, we believe that given the financial and logistic burden of recruiting across Ontario from six distinct geographic locations, the risk of selection bias was a minimal trade-off for a diverse sample of Ontarians. Moreover, we recognize that because of our sampling strategy, our results for short-term and continuing care clients may not be generalizable to all clients in their respective populations.
The valuation of time may also be considered a limitation in two respects. While some may disagree with the methodology used to assign a monetary value to time, we have used methods that are consistent with those highlighted in the literature. Furthermore, in this study, these methods were applied across all study subjects. Others may argue that it is unnecessary to assign monetary values to time because many individuals willingly provide care to family members in need and would not desire additional public services. While we recognize this fact, we argue that time costs are needed to quantify lost opportunity costs, not to estimate replacement costs for public services.
Conclusions
This study is one of the first to attempt to value simultaneously both the private and public costs associated with home-based care. Moreover, the study assessed costs for two client populations: short-term and continuing care clients. As such, it provides needed insight into the cost ramifications of shifting care into the home setting.
The private share of home-based care depends on the demographic and clinical characteristics of the clients. Given this finding, decision-makers who are responsible for the allocation of resources or planning for home-based services in Ontario must consider the characteristics of clients to determine who may be at risk for receiving inadequate care or for incurring the greatest burden (time and money) associated with caregiving by family members. In particular, policy makers and health system managers should use this study as evidence that the population of home care recipients is heterogeneous; thus, services must be tailored to address the specific needs of various populations. Consequently, the method by which services are distributed must be assessed to ensure that services are allocated according to physical, medical and psycho-social needs. Future allocation of resources must appreciate the important role that family members play in the overall delivery of home-based care, and this care may need to be recognized by providing financial support to caregivers.
Acknowledgments
The authors would like to acknowledge funding from CHSRF/CIHR (Grant # RC1-0875-06) and the Ontario Ministry of Health and Long-Term Care. Dr. Coyte is supported by funds from the Canadian Health Services Research Foundation, the Canadian Institutes of Health Research and the Ontario Ministry of Health and Long-Term Care for his Chair in Health Care Settings and Canadians.
Contributor Information
Vivian W. Leong, Department of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Denise N. Guerriere, Department of Health Policy, Management and Evaluation and Faculty of Nursing, University of Toronto, Toronto, ON.
Ruth Croxford, Clinical Epidemiology Unit, Sunnybrook Health Services Centre, Toronto, ON.
Peter C. Coyte, Department of Health Policy, Management and Evaluation and Faculty of Nursing, University of Toronto; Health Care, Technology and Place CIHR Strategic Training Program, Institute for Clinical Evaluative Sciences, Toronto, ON.
References
- Alcock D., Danbrook C., Walker D., Hunt C. Home Care Clients, Providers and Costs. Canadian Journal of Public Health. 1998;89(5):297–300. doi: 10.1007/BF03404478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aykan H. Effect of Childlessness on Nursing Home and Health Care Use. Journal of Aging & Social Policy. 2003;15(1):33–53. doi: 10.1300/J031v15n01_03. [DOI] [PubMed] [Google Scholar]
- Browne G.B., Arpin K., Corey P., Fitch M., Gafni A. Individual Correlates of Health-Service Utilization and the Cost of Poor Adjustment to Chronic Illness. Medical Care. 1990;28(1):43–58. doi: 10.1097/00005650-199001000-00006. [DOI] [PubMed] [Google Scholar]
- Canadian Automobile Association. CAA 2005 Edition Driving Costs. (June 2005.) 2006 Retrieved June 14, 2007. http://www.caa.ca/english/homepage/searchresults.asp .
- Chan B., Coyte P.C., Heick C. Economic Impact of Cardiovascular Disease in Canada. Canadian Journal of Cardiology. 1996;12(10):1000–6. [PubMed] [Google Scholar]
- Chappell N.L. Living Arrangements and Sources of Caregiving. Journal of Gerontology. 1991;46(1):S1–S8. doi: 10.1093/geronj/46.1.s1. [DOI] [PubMed] [Google Scholar]
- Chappell N.L., Dlitt B.H., Hollander M.J., Miller J.A., McWilliam C. Comparative Costs of Home Care and Residential Care. The Gerontologist. 2004;44(3):389–400. doi: 10.1093/geront/44.3.389. [DOI] [PubMed] [Google Scholar]
- Coyte P.C. , McKeever P. Home Care in Canada: Passing the Buck. Canadian Journal of Nursing Research. 2001;33(2):11–25. [PubMed] [Google Scholar]
- Coyte P.C., Young W. Regional Variations in the Use of Home Care Services in Ontario, 1993/95. Canadian Medical Association Journal. 1999;161(4):376–80. [PMC free article] [PubMed] [Google Scholar]
- Di Matteo L., Di Matteo R. Public Homecare Expenditures in Canada. Canadian Public Policy. 2001;27(3):313–33. [Google Scholar]
- Fillenbaum G. The OARS Assessment Methodology: Multidimensional Functional Assessment Questionnaire (2nd ed.) Durham, NC: Duke University Center for the Study of Aging and Human Development; 1988. [Google Scholar]
- Fillenbaum G., Smyer M. The Development, Validity and Reliability of the OARS Multidimensional Functional Assessment Questionnaire. Journal of Gerontology. 1981;36(4):428–34. doi: 10.1093/geronj/36.4.428. [DOI] [PubMed] [Google Scholar]
- Forbes D.A., Janzen B.L. Comparison of Rural and Urban Users and Non-Users of Home Care in Canada. Canadian Journal of Rural Medicine. 2004;9(4):227–35. [PubMed] [Google Scholar]
- Forbes D.A., Stewart N., Morgan D., Anderson M., Parent K., Janzen B. Individual Determinants of Home-Care Nursing and Housework Assistance. Canadian Journal of Nursing Research. 2003;35(4):14–36. [PubMed] [Google Scholar]
- Government of Ontario. Paper A: Ontario’s Finances (pp. 1–80) 2004 Retrieved June 14, 2007. http://www.fin.gov.on.ca/english/budget/ontariobudgets/2004/papera.html .
- Government of Ontario. Choosing Quality, Rewarding Excellence: Ontario’s Response to the Caplan Report on Home Care (pp. 1–37) 2006 Retrieved June 14, 2007. http://www.health.gov.on.ca/english/public/pub/ministry_reports/caplanresp06/caplanresp06.html .
- Guerriere D.N., Tullis E., Ungar W.J., Tranmer J.E., Corey M., Gaskin L., Carpenter S., Coyte P.C. Economic Burden of Ambulatory and Home-Based Care for Adults with Cystic Fibrosis. Treatments in Respiratory Medicine. 2006;5(5):351–59. doi: 10.2165/00151829-200605050-00006. [DOI] [PubMed] [Google Scholar]
- Guerriere D.N., Ungar W.J., Corey M., Croxford R., Tranmer J.E., Tullis E., et al. Evaluation of the Ambulatory and Home Care Record: Agreement between Self-Reports and Administrative Data. International Journal of Technology Assessment in Health Care. 2006;22(2):203–10. doi: 10.1017/S0266462306051026. [DOI] [PubMed] [Google Scholar]
- Hall R., Coyte P.C. Determinants of Home Care Utilization: Who Uses Home Care in Ontario? Canadian Journal on Aging. 2001;20(2):176–92. [Google Scholar]
- Hawranik P. The Role of Cognitive Status in the Use of Inhome Services: Implications for Nursing Assessment. Canadian Journal of Nursing Research. 1998;30(2):45–65. [PubMed] [Google Scholar]
- Hawranik P.G., Strain L.A. Cognitive Impairment, Disruptive Behaviors, and Home Care Utilization. Western Journal of Nursing Research. 2001;23(2):148–62. doi: 10.1177/019394590102300204. [DOI] [PubMed] [Google Scholar]
- Katz S.J., Kabeto M., Langa K.M. Gender Disparities in the Receipt of Home Care for Elderly People with Disability in the United States. Journal of the American Medical Association. 2000;284(23):3022–27. doi: 10.1001/jama.284.23.3022. [DOI] [PubMed] [Google Scholar]
- MacAdam M. Home Care: It’s Time for a Canadian Model. Healthcare Papers. 2000;1(4):9–36. doi: 10.12927/hcpap.2000.17348. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Long-Term Care. Ontario Drug Benefit Formulary. 2005a Jul; Retrieved June 14, 2007. http://www.health.gov.on.ca/english/providers/program/drugs/odbf_eformulary.html .
- Ministry of Health and Long-Term Care. Seniors’ Care: Who Do I Contact for Information? 2005b Retrieved June 14, 2007. http://www.health.gov.on.ca/english/public/program/ltc/6_ccac.html .
- Mitchell L., Roos N.P., Shapiro E. Patterns in Home Care Use in Manitoba. Canadian Journal on Aging. 2004;24(suppl. 1):59–68. doi: 10.1353/cja.2005.0053. [DOI] [PubMed] [Google Scholar]
- Moller S.F., von Frese J., Bro R. Robust Methods for Multivariate Data Analysis. Journal of Chemometrics. 2005;19(10):549–63. [Google Scholar]
- Morgan D.G., Semchuk K.M., Stewart N.J., D’Arcy C. Rural Families Caring for a Relative with Dementia: Barriers to Use of Formal Services. Social Science & Medicine. 2002;55(7):1129–42. doi: 10.1016/s0277-9536(01)00255-6. [DOI] [PubMed] [Google Scholar]
- Penning M.J. Cognitive Impairment, Caregiver Burden, and the Utilization of Home Health Services. Journal of Aging and Health. 1995;7(2):233–53. doi: 10.1177/089826439500700204. [DOI] [PubMed] [Google Scholar]
- Peterson S., Shapiro E., Roos N.P. Regional Variation in Home Care Use in Manitoba. Canadian Journal on Aging. 2005;24(suppl. 1):69–80. doi: 10.1353/cja.2005.0054. [DOI] [PubMed] [Google Scholar]
- Rice D., MacKenzie E. Cost of Injury in the United States: A Report to Congress, 1989. San Francisco: Institute for Health and Aging, University of California; 1989. [Google Scholar]
- Statistics Canada. Table 2020407 (Income of Individuals, by Sex, Age Group and Income Source, 2002 Constant Dollars: Earnings). Canadian Socio-Economic Information Management System (CANSIM II) Retrieved June 14, 2007. http://cansim2.statcan.ca/cgi-win/cnsmcgi.exe?Lang=E&RootDir=CII/&ResultTemplate=CII/CII___&Array_Pick=1&ArrayId=2020407 .
- Statistics Canada. Canadian Community Health Survey – Mental Health and Well-being (CCHS) 2003 Aug 31; Retrieved June 14, 2007. http://www.statcan.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=5015&lang=en&db=IMDB&dbg=f&adm=8&dis=2 .
- Torgerston D., Donaldson C., Reid D. Private versus Social Opportunity Cost of Time: Valuing Time in the Demand for Health Care. Health Economics. 1994;3(3):149–55. doi: 10.1002/hec.4730030304. [DOI] [PubMed] [Google Scholar]
- Walter-Ginzburg A., Guralnik J.M., Blumstein T., Gindin J., Modan B. Assistance with Personal Care Activities among the Old-Old in Israel: A National Epidemiological Study. Journal of the American Geriatrics Society. 2001;49(9):1176–84. doi: 10.1046/j.1532-5415.2001.49234.x. [DOI] [PubMed] [Google Scholar]
- Wilkins K., Park E. Home Care in Canada. Health Reports. 1998;10(1):29–37. [PubMed] [Google Scholar]