Abstract
Canada's apparent capacity to reform its health system is inversely proportionate to the volume of high-quality reports that document its need to do so. One of the principal causes of this inertia is our unusual preoccupation with the financial sustainability of the public system, despite compelling evidence that this is a fundamental misdiagnosis. The case made here is that we need to declare a moratorium on the sustainability debate, become more adept at learning which features of international systems we can and cannot easily import, and recognize that what ails our system originates in design rather than the laws of nature.
Abstract
La capacité apparente du Canada de réformer son système de santé est inversement proportionnelle au volume de rapports très valables qui rendent compte du besoin de cette réforme. Une des causes principales de cette inertie est notre étrange souci de la durabilité financière du système public, malgré les preuves convaincantes que ce souci constitue une erreur d'analyse fondamentale. Cet article préconise le besoin de déclarer un moratoire sur le débat sur la durabilité, d'apprendre à mieux distinguer quels éléments des systèmes internationaux nous pouvons ou ne pouvons pas facilement importer et de reconnaître que les maux de notre système tiennent à la conception de ce dernier plutôt qu'aux lois de la nature.
Never ascribe to malice that which is adequately explained by incompetence.
Napoleon Bonaparte
Napoleon was not renowned for his generous impulses, but this is surely one of them. Incompetence is a condition; malice is a motive. The presence of the former is hardly proof of the absence of the latter (indeed, the two often make a nice combo). Canada's healthcare system is, like everybody else's, large, complex, expensive and imperfect. We get many things right, we get some things wrong, and we aim to preserve what is right and remedy what is wrong. Yet our reforms seem timid and ineffective, and suffer enormous energy loss on the path from conception to outcome (e.g., physician payment systems; primary healthcare renewal; nurse practitioners; electronic health records; interprofessional education; patient safety and quality improvement, among others).
The connection between intention and action seems stronger and more immediate elsewhere. Other countries aren't Nirvana, but their errors are braver – sins of commission rather than omission. The United Kingdom exhausts its system with perpetual change; we exhaust ours with endless talk and death by a thousand demonstration projects. Wherein lies the difference? Are we incompetent, maliciously hostile to large-scale improvement, gridlocked by federalism and vested interests, or too easily contented with what we have? We look to pockets of excellence for inspiration, but history and interest accommodation set policy. We accept great performance but never insist on it. If the status quo isn't good enough, we add money.
A perpetual question in Canada is what we can learn from other countries. Here we make two kinds of errors. Sometimes we claim we can learn nothing from other countries' experiences because they are so context-specific, culturally rooted, historically conditioned and structurally unique. Some are, but some aren't, and we need to know the difference. And sometimes we claim we can cherry-pick one feature – say, co-payments for physician visits in France – with no understanding of how it is connected to a broad and intricate policy regime. We obsess about the pathway to change while losing sight of the destination. Denmark hasn't built a nursing home bed in over a decade, and Kaiser Permanente patients use fewer than half as many hospital bed-days per capita as Canadian patients. Am I the only one who thinks it's odd that Canadians spend endless hours debating whether and how to organize a wait list and no time setting clear targets that match the best of elsewhere? What accounts for our innovation learning disability?
Canada's Strange Obsession with Sustainability
There are 30 countries in the Organisation for Economic Co-operation and Development. By my reckoning 19 of them are, broadly speaking, Canada's economic peers, with a GDP per capita no more than 20% lower or higher than ours.1 Here are some basic facts about their economies and healthcare spending (all data from OECD Principal Economic Indicators 2007 and OECD Health Data 2007).
Canada's real per capita GDP grew by 16.6% between 2000 and 2006, about two percentage points more than the 20-country average, and four percentage points more than the G7 countries.2
In 2005 all spent between 7.5% and 11.6% of their GDP on healthcare. Canada, at 9.8%, ranked sixth of 20.
The government-financed share of total health spending ranged from 59% (Switzerland) to 87% (UK). Canada, at 70%, was next to last, and five countries exceeded 80%.
Between 1970 and 2003, the average rate of real per capita spending increase in healthcare was 4%. Canada's rate was 3% – the sixth lowest of the 20 countries. On top of this, our governments are in excellent fiscal shape, with a long run of big federal surpluses, balanced budgets the norm among provinces, and all achieved while cutting taxes. Among the G7 countries our fiscal performance has been spectacular: our debt-to-GDP ratio has declined by two-thirds in a decade and continues downward, while others' are flat or rising.
In summary, governments have left a larger share of healthcare spending to the private sector than all but one of our peers; our cumulative rate of spending increases has been unexceptional; our fiscal houses are in order; and our economy is humming. It's hard to imagine a less daunting sustainability situation. Yet sustainability appears to be a uniquely Canadian preoccupation. How do I know? Google, of course.
In an earlier draft of this paper I included the results of a number of Google searches, such as “sustainable healthcare” AND “Canada OR Canadian.” The numbers are unstable within very short time periods, and sometimes the results make no sense: “New Zealand” AND “sustainable healthcare” yields 884 hits, but the same search WITHOUT “Canada OR Canadian” yields 885, and the same search WITHOUT “Canadian OR Canada” yields 853. (This erratic behaviour is somewhat disconcerting from the genius search engine of all time and a company with market capitalization of $158 billion.)
So the exact numbers are not worth reproducing here, but there is a pattern. In a search for “country name” + “sustainable healthcare,” Canada has slightly more hits than the United Kingdom, twice as many as Australia and 2.5 times as many as Sweden. But excluding references to Canada from searches for other countries reduces the UK total by half, and Australia's and Sweden's by 95%. Conversely, excluding references to the UK from the Canadian search reduces our hits by a quarter; to Australia, by 30%; and to Sweden, by 17%.
The overall picture starts to get pretty clear. Canada appears to drive a good deal of the worldwide talk on sustainability even though not a single objective economic indicator points to a Canadian problem. Needless to say, objective reality is not always the arbiter of conviction.
The sustainability crisis mantra is traceable to three sources of inspiration. One is ideology: those who want to privatize the system need to persuade the public and politicians that even if we think public healthcare is a good idea that serves us well, what we could afford then we can barely afford now, and certainly cannot afford in the future. Let's all pay our respects at the funeral and move on. A second is adherence to the contention that an aging population will bankrupt the system. And the third is concern about the growing proportion of provincial government spending consumed by healthcare. The first two have been refuted so well by so many that if you still believe either or both, your beliefs rely on other than fact and logic, and fact and logic are all that I have to offer, so I'll spend my words elsewhere.
The third claim is or has been factual, and merits examination. Governments have spent increasing proportions of their budgets on healthcare over the past decade. Bear with me here; how this occurs requires some parsing.3 Following is a list of possible explanations for the increasing percentage of spending going to healthcare, and what has actually occurred.
Governments can decide to increase the rate of healthcare spending faster than the rate of spending on other programs and services. Over the past decade they have, and the percentage of the budget spent on healthcare has risen.
Governments can slow the rate of increase, or outright reduce total spending in order to reduce or eliminate deficits, pay down debt, accumulate surpluses and/or build up a rainy-day fund (notably, the Alberta Heritage Fund). This reduction can occur even while revenues are stable or increasing. If at the same time healthcare spending increases at the same rate or higher than before, its share of total spending will rise even if it is not taking a larger share of total revenues. This, too, was the case when provinces decided to get their fiscal houses in order. It is not generally the case now because provincial budgets are balanced or in surplus.
Governments can limit the rate of growth in total revenues by cutting taxes. They have done so dramatically. One result has been that the growth rate in healthcare spending has sometimes exceeded the growth rate in total government revenues.
None of these phenomena, either individually or in tandem, is cause for alarm. On top of this, healthcare spending rate changes are variable and controllable by governments. If healthcare spending is rising faster than some think it should, remember that governments formally have determined that this is good public policy – it is they who draw up the budget and decide on its component parts. Furthermore, since 2000 Ottawa has committed itself to huge and mostly unconditional additional cash transfers to the provinces for healthcare, with built-in escalator clauses, a situation that, among other things, sends signals to the sellers of labour and goods to increase their prices. (The rate of inflation in healthcare tends to be somewhat higher than the overall inflation rate.) Repeated polls suggest that the public in general supports higher healthcare spending, and governments occasionally do what the people want.
The key point is this: a proportion or percentage derives from a numerator (healthcare spending) and a denominator (the total pool of funds available to spend). Governments have deliberately determined the size of both; the deception is to claim that the changing proportion is an inexplicable act of nature, a fiscal crop circle drawn by aliens. If healthcare is eating others' lunch (as some, but not all, would concede), it does so by design, and government has a number of levers at its disposal to get some of it back if that's what's desired.
That said, there is nothing intrinsically unsustainable about gradually increasing the proportion of provincial budgets spent on healthcare. Relative expenditures change all the time. The important question is whether the redistribution produces good value for money. The percentage of household spending on computers and vacation properties has skyrocketed in the past generation, yet no one terms this a crisis. In a federal system like Canada's, the chances of at least one of 14 governments declaring a healthcare spending crisis at any given time are about the same as picking the winner if you bet on every horse in the race.
But let's put away the calculator and make the groundless concession that yes, healthcare has a sustainability crisis, we're spending too much, we're getting poor value for money (true) and we have to fix it. What can we learn from other countries? What measures hold some promise of improvement, and which are dead losers? Briefly, here's a buyer's guide to international healthcare innovation.
Is for-profit healthcare cheaper or better?
No. It is certainly more expensive (Devereaux et al. 2004), and in some cases – notably, dialysis in the US – it is of lower quality (Devereaux et al. 2002). In long-term care, for-profit institutions provide less direct and supportive care per resident (McGregor et al. 2006). Then-Senator Michael Kirby remained agnostic on the subject, but as a member of the board of directors of the for-profit nursing home chain Extendicare Ltd. and holder of over a million dollars' worth of company stock and options prior to releasing his report, his objectivity might reasonably be doubted.4
Are PPPs (public–private partnerships) cheaper?
No. They are more expensive. The government can borrow money more cheaply than private firms. Private firms expect, and almost always receive, a built-in, guaranteed profit, lucrative lease-back terms and so on. Pollock and colleagues (2002) have done the math in the UK. The verdict: the private partner makes off with huge returns, the public sector overpays and the risk stays with all of us.
Do user fees solve any problems?
No. They deter poor and sick people from seeking care, and have little effect on others. Where they are modest they raise little cash; where they are substantial – as for drugs – prices do not fall, utilization does not become more rational, but many people forgo effective treatment. Healthcare spending is highly concentrated – a mere 2% of people can account for over 40% of health spending in any given year. Nickeling and diming – or even looneying and tooneying them – will accomplish nothing.
Is it better to have too few or too many healthcare workers?
For the workers, too few is better financially, but not necessarily for their overall well-being; for the public, a modest oversupply is better both financially and in terms of access. Europe has much higher physician-to-population ratios than Canada and, in some countries, significant physician unemployment (Rechl et al. 2006). It's just basic economics that if Canada tightly controls its workforce supply and guarantees every graduate a job, wages will rise and labour of all types will substantially control the agenda.
How many healthcare workers is enough?
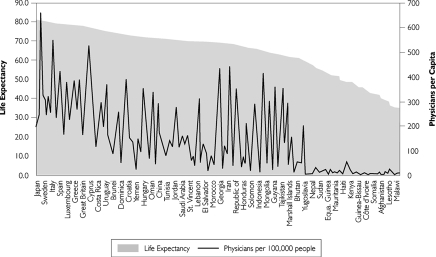
No one knows. Canada is in constant turmoil about the doctor shortage. Many Canadians do not have a regular family physician. Curiously, the same physician-to-population ratio that was seen as a surplus 20 years ago became a serious and growing shortage by about 1995. It is still not clear why; per capita use of physicians' services has continued to grow throughout this time. But how does the physician-to-population ratio affect overall population health status? If you can figure out the connection from Figure 1 below, they'll name a statistical test after you. And remember that it's not all about doctors. Three dozen randomized, controlled trials have shown that nurse practitioners can deliver huge swaths of primary care as effectively as physicians (Horrocks et al. 2002), yet we continue to deploy them gingerly. At its August 2007 meeting, the Canadian Medical Association yet again attempted to turn back the clock on the sensible delegation of limited prescribing authority to pharmacists.
FIGURE 1.
Life expectancy vs. physicians per capita
Univ. of California Atlas of Global Inequality, http://ucatlas.ucsc.edu/spend.php
Left to their own devices, most healthcare professions want to maintain exclusive scope of practice over certain territory and move onto others' turf when it suits them. There has also been a marked trend towards increasing entry-to-practice credentials (e.g., to a baccalaureate degree for nursing, an added year of residency for family doctors, a master's degree for physiotherapy). Both the inflexibility of the workplace and the creation of barriers to entry into health professions contribute to shortages and inefficiencies. Thus far the policy response has been to increase enrollments. Before doing so, we should have figured out how to allow healthcare workers to use all their knowledge and skills, acquire new capacities efficiently and replace a mainly credential-based framework to ensure safety and quality with a competency-based approach.
What's the key to controlling costs?
European countries with much older populations than Canada's appear to have better access, shorter wait times, as much or more high-end technology and similar or lower costs. How do they do it? They pay doctors less. They use more home care and less long-term residential care. They have more egalitarian societies and more extensive social programs. The government covers a larger share of health costs, particularly drugs.
That's all fine, but we're not Europe. What can we do?
Identify and shrink variations in costs. In Canada, three- and fourfold variations in intervention rates among identical populations are far from rare. South of the border, seniors in Miami use twice as much healthcare as seniors in Minneapolis, with poorer outcomes. We're terrified by underuse and oddly unconcerned about overuse. Pay attention to both and we'll save money.
What about information technology?
We're proven laggards. Denmark has a universal electronic health record accessible to patients on the Web. Its physicians estimate they save an hour a day previously spent chasing down test results and other information. The dramatic ascent of the Veterans Affairs health system in the United States from “worst to first” went hand in hand with major investment in and use of health information technology. We're haltingly building ground-up systems that may not be able to talk to one another, with different data definitions. In the move to alternative payment plans for physicians (a fine idea), we've actually lost data (a potential disaster). In the usual Canadian way, we don't invest enough, and we don't have a solid policy framework to ensure that the systems are useful for clinical care, management, governance, resource allocation and evaluation.
What's the biggest lesson we can learn from other countries?
They think, they plan and they act, often decisively. Somehow, the risks of innovation and policy experimentation seem lower. They are less afraid to set meaningful targets and shoot at them. In Canada, the 2003 Health Accord promised that 50% of Canadians would have access to an undefined primary healthcare system on a 24/7/365 basis by 2011. England today offers you a physician's appointment within 48 hours, 99% of the time. We set vague and distant wait time targets and oil the squeaky wheels; England foresees that within two years the maximum wait time from first walking into a GP's office to completion of whatever procedure is necessary will be four months. I'm no fan of much of what New Zealand does, but it had the guts to set needs-based, measurable thresholds for surgical interventions, and it has bargained brilliantly to secure very low drug prices. You can raise or lower the bars in Figure 2 in accordance with your own perceptions of the healthcare world, but it is incontestable that many countries have lapped us in the race to reform.
FIGURE 2.
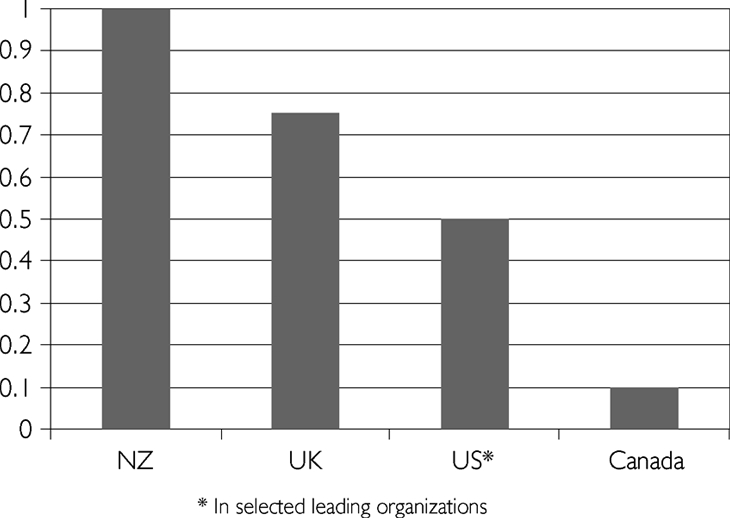
Completely invalid inferred estimate of action-to-talk ratio in four countries
Which brings us back to sustainability. If we're going to get better at change, we need to declare a moratorium on the sustainability argument for at least five years. It is a monumental distraction that takes up too much deliberative time. Let's move on to more worthy preoccupations, such as quality improvement, aligning incentives with goals, making excellence mandatory and reducing health (and healthcare) disparities. Canada talks like other countries; now it's time to act like them. Only our refusal to embrace large-scale change that serves the public rather than private interests is unsustainable.
To illustrate, Greece is in, Hungary out (too poor); Luxembourg is out (too rich); the United States is out because its healthcare structure and data are real but absurd, and hence of no interest here.
Calculated using 2000 prices and exchange rates.
This version is highly truncated. For a much fuller explanation, see R.G. Evans, “Economic Myths and Political Realities: The Inequality Agenda and the Sustainability of Medicare,” UBC Centre for Health Services and Policy Research, July 2007. <http://www.chspr.ubc.ca/node/791>.
Many, including newspaper editorialists, have doubted it – see http://www.healthcoalition.ca/kirby.html.
References
- Devereaux P.J., Heels-Ansdell D., Lacchetti C., et al. Payments for Care at Private for-Profit and Private Not-for-Profit Hospitals: A Systematic Review and Meta-analysis. Canadian Medical Association Journal. 2004 Jun 8;170(12):1817–24. doi: 10.1503/cmaj.1040722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devereaux P.J., Schünemann H.J., Ravindran N., et al. Comparison of Mortality between Private for-Profit and Private Not-for-Profit Hemodialysis Centers: A Systematic Review and Meta-analysis. Journal of the American Medical Association. 2002;288(19):2449–57. doi: 10.1001/jama.288.19.2449. [DOI] [PubMed] [Google Scholar]
- Horrocks S., Anderson E., Salisbury C. Systematic Review of Whether Nurse Practitioners Working in Primary Care Can Provide Equivalent Care to Doctors. British Medical Journal. 2002;324(7341):819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor M.J., Tate R.B., McGrail K.M., Ronald L.A., Broemeling A-M., Cohen M. Care Outcomes in Long-Term Care Facilities in British Columbia, Canada: Does Ownership Matter? Medical Care. 2006;44:929–35. doi: 10.1097/01.mlr.0000223477.98594.97. [DOI] [PubMed] [Google Scholar]
- OECD Health Data. 2007 Jul; Retrieved September 22, 2007. < http://www.oecd.org/dataoecd/46/33/38979719.pdf>.
- OECD Principal Economic Indicators. Data from OECD Annual National Accounts database. 2007 Jul; Retrieved September 22, 2007. < http://www.oecd.org/dataoecd/48/4/37867909.pdf>.
- Pollock A., Shaoul J., Vickers J. Private Finance and ‘Value for Money’ in NHS Hospitals: A Policy in Search of a Rationale? British Medical Journal. 2002;324:1205–9. doi: 10.1136/bmj.324.7347.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rechl B., Dubois C-A., McKee M., editors. The Health Care Workforce in Europe: Learning from Experience. Copenhagen: WHO European Observatory on Health Systems and Policies; 2006. [Google Scholar]