Abstract
The mean costs of providing healthcare increase with age, but within every age/sex cohort there is substantial variation. Moreover, this variation does not disappear over the users' lifetime. This study applies Markov modelling to administrative data to examine the variability of healthcare costs currently covered under the Canada Health Act across a population and over the lifespan. Policy initiatives that ignore individual variability across the lifespan yield inequitable results. For example, age-specific policies that exempt seniors from costs charged to the rest of the population will transfer healthcare resources to healthy low-cost seniors from younger individuals with higher needs.
Abstract
Le coût moyen de prestations de services de santé accroît avec l'âge, mais au sein de toute cohorte âge/sexe il existe des variations substantielles. Or, ces variations ne s'estompent pas au cours de la vie des utilisateurs. La présente étude applique le modèle de Markov aux données administratives pour étudier la variabilité des coûts de services de santé présentement couverts par la Loi canadienne sur la santé pour une population donnée au cours de la vie de l'utilisateur. Les initiatives politiques qui ne tiennent pas compte des variabilités individuelles au cours de la vie mènent à des résultats inéquitables. Par exemple, les politiques fondées sur l'âge qui accordent aux aînés une exemption de coûts par rapport au reste de la population conduiront à un transfert des ressources en faveur d'aînés sains et peu coûteux au détriment de jeunes personnes dont les besoins sont importants.
Throughout the developed world, aging populations have been identified as a threat to the sustainability of healthcare. Many have argued that researchers must refine their estimates of age-related costs in order to facilitate the social and public policy changes necessary before private finances and government budgets are overwhelmed by demographic changes (Alemayehu and Warner 2004; Knickman and Snell 2002). Most research has estimated age and sex-standardized utilization and costs, benchmarks that are clearly necessary for general planning and projection purposes. In order to ensure that resources are in place to serve an aging population, we must know how much it costs, on average, to provide healthcare to men and women as they age. Less attention has been paid to the variability of individual costs over time, which is the focus of this paper.
Knowing something about individual variability of costs over a lifetime, and the variation of costs among members of particular age–sex cohorts, will allow us to estimate the distributional impact of proposed policy changes. For example, if costs are strongly related to age and vary little within particular age cohorts, then age-specific policies that exempt seniors from some healthcare costs that younger Canadians pay out of pocket or through third-party insurers are reasonable. If, on the other hand, costs vary dramatically within particular age–sex cohorts, such policies will subsidize many low-cost seniors at the expense of younger people with greater needs. This paper uses Markov modelling to estimate the level of individual variability, both at any point in time and over a lifetime.
Although opinions vary about the extent of the challenge, mean healthcare costs clearly increase with age (Hogan and Hogan 2002; Barer et al. 2004; Hogan and Lise 2004). This correlation seems to imply a relatively predictable lifetime pattern of costs; a typical individual might anticipate many years of increasingly costly disability before dying an expensive death at an advanced age. However, in any one year, healthcare expenditures are not normally distributed but are highly skewed within all age–sex categories (Monheit 2003; Forget et al. 2002, 2005). If individual variations largely even out over a lifetime, most individuals would experience some years in which their costs exceeded the mean for others of their age and sex and other years in which their own costs are lower than expected. Alternatively, most individuals might remain low-cost users of the healthcare system, even at very advanced ages. The policy implications clearly depend on the distribution of expenditures, both in any single year and over a lifetime.
Studies in the United States have highlighted the age-dependent nature of healthcare costs. While the precise figures depend on which costs are included in the calculation, one study found that mean per capita costs climb slowly through adulthood, then more rapidly after age 50 (Meerding et al. 1998). Within the US Medicare population, those over 85 cost three times as much as those between 65 and 74, and twice as much as those between 75 and 84 (Fuchs 1999). Nearly half of lifetime expenditure is incurred during the senior years, and for those who survive to age 85, more than one-third of their lifetime expenditures will accrue in their remaining years (Alemayehu and Warner 2004). However, these findings are partly a reflection of how care is organized and delivered; nursing home costs are a significant portion of the larger healthcare consumption of the oldest (Liang et al. 1996; Alemayehu and Warner 2004). Similar trends have been documented elsewhere in the OECD (Maguire 1987; Reinhardt et al. 2002).
Costs incurred in the period before death account for a disproportionate share of healthcare resources (Roos et al. 1987; Scitovsky 1988). However, people who die at older ages cost significantly more in the last six months of life than do those dying at younger ages (Roos et al. 1987). Mean costs for women tend to exceed those of men at any age (Mustard et al. 1998; Forget et al. 2005; Alemayehu and Warner 2004). Nearly all age-specific gender differences can be explained by sex-specific conditions, such as costs associated with childbirth (Mustard et al. 1998).
Analysis of the variability of healthcare costs reveals that most expenditure is incurred by a very small proportion of the population (Forget et al. 2002, 2005; Deber et al. 2004; Monheit 2003). This significant variation exists even in age-specific expenditures. Manitoba data for hospital and physician expenditures show that, for example, 90% of men aged 20 to 24 and 70% of women aged 65 to 74 spend less than the mean per capita expenditure for their age–sex group (Forget et al. 2002; Deber et al. 2004). Not all of the high-cost users are elderly, nor are most of the elderly high-cost users. This study examines the distribution of lifetime healthcare costs across a population, taking into account the significant variability of costs in all age–sex cohorts.
Analyzing health costs over a lifetime
Most investigations of healthcare costs over a lifetime are based on cross-sectional studies of age-specific expenditures (Waldo et al. 1989; Mustard et al. 1998; Forget et al. 2005). These studies do not reflect the lifetime costs of particular individuals as they age; instead, they compare various birth cohorts at a point in time. Such studies cannot capture the implications for lifetime costs of systematic differences in life expectancies, morbidity patterns, socio-economic status and service use across a population. In particular, while they can examine the variation in healthcare costs for a particular age–sex cohort, they cannot build an individual's health history into the model and show how present costs depend not only on age and sex, but also on past utilization. Longitudinal studies, by contrast, follow a particular cohort as its members age, thus building history into the model (Lubitz and Riley 1993; Lubitz et al. 1995; Spillman and Lubitz 2000). But these studies attribute all changes over time to aging and are unable to control for changes in medical technology, relative prices and disease incidence.
Other approaches may be able to blend the advantages of both cross-sectional and longitudinal studies. A period life table model takes the experience of a “typical” individual for each year and then simulates costs (Alemayehu and Warner 2004). This approach has the advantage of holding everything but the age of an individual constant as a pattern of lifetime costs is constructed, but does not readily incorporate variation within age–sex groups. The present study uses a variation of the life table model. It employs a Markov model, which simulates expenditure patterns across a population as that population ages. As in the period life table model, costs, medical technology and disease incidence are held constant while the model examines the distribution of lifetime costs across a population.
Method
We developed a Markov model of healthcare expenditures in which the probabilities of moving between various cost states (and death) depended on age, sex and past utilization. We constructed 10 different transition matrices for males and 10 for females: <1 year of age, 1–4 years of age, 5–14, 15–19, 20–24, 25–34, 35–44, 45–54, 65–74 and ≥75. We used per capita healthcare expenditures and the morbidity and mortality experience of a population, differentiated by age and sex, for two years (2002–2003) to generate profiles of healthcare expenditures from birth to death. This procedure estimates the effects of aging on individual costs, holding constant the state of medical technology, disease incidence and relative healthcare prices as our cohort ages.
Per capita healthcare expenditure
Manitoba was chosen as the study site because the Manitoba Population Health Research Data Repository captures standardized data based on almost every physician and hospital contact in the province. This information (including patient identification numbers, physician claims, diagnoses, costs and hospitalization and institutionalization data) is maintained and controlled by the provincial department of health. All records deposited in the repository have been processed by Manitoba Health and Healthy Living to remove patient identifiers such as name and address, while preserving the capacity to link records together to form individual histories of healthcare use. The database includes direct information on physician billings, excluding some patient visits outside the province, salaries for trainees and some physicians' paid salaries for specific services (Roos et al. 1993).
The costs of inpatient hospital care and day surgery procedures have been estimated by applying the Manitoba average cost per weighted case to each discharge. This method takes into account the typical resource use associated with particular types of cases. Because Canadian hospitals receive block funding from the province, no direct hospital price data are associated with individual patients. Total cost of care for an inpatient or day surgery patient includes all physician services received during the hospital stay. Some costs, such as those associated with blood products and emergency wards, are omitted from the study because we cannot track these costs to individual patients. Other costs, such as those associated with capital expenditure and public health, are omitted because these costs are not patient specific. We capture and allocate to individual patients approximately 64% of the total amount that the province claims to spend on hospital funding. Some small percentage of costs omitted will have been spent to provide care for non-Manitoba residents, but the great bulk of the omitted costs are associated with capital costs and trainee salaries, particularly in the teaching hospitals.
This study looks only at physician visits and hospital stays, the core services fully insured and publicly provided under the Canada Health Act. Hospital and physician costs together accounted for 43.4% of total health expenditure and 57.7% of public expenditure in Canada in 2003 (CIHI 2005). In 2005, the comparable figures were 42.7% and 57.3%.
The database also includes data on all pharmaceutical use outside institutions, as well as information on care in the home and nursing home settings. We have chosen to omit these costs from the present study because while most provinces, including Manitoba, cover some or all of these costs for some or all patients, specific insurance arrangements vary among provinces and have changed significantly over time. While the Canada Health Act makes the provinces responsible for physician and hospital care, no such requirement exists for other services. This analysis focuses on publicly funded healthcare costs that are mandated by the Canada Health Act. Results can therefore be generalized to all provinces.
While we have chosen to omit long-term residential care from this analysis of public healthcare spending for the purposes of policy analysis, this decision does have significant implications for the costs simulated by the model. A significant portion of seniors (75+) reside in personal care homes, particularly during the last year of life. Once in a personal care home, however, these people tend to use fewer hospital resources than they otherwise might. Therefore, high users may show a transition into the medium-user group when they enter a personal care home because long-term facility costs are not counted in the analysis. A significant portion of full lifetime healthcare costs is, therefore, omitted from our model, which focuses only on those publicly funded costs mandated by the Canada Health Act. Some caution, therefore, should be used in interpreting these results. We omitted these costs because they are not currently mandated by the Canada Health Act, and we wanted to use our results to examine the distributional impact of proposed policies. Policy analysis requires that one starts from the status quo. In other words, our analysis is conducted from the perspective of the public payer mandated to provide the services covered by the Canada Health Act. To examine the full social cost of an aging population, we would have to include not only residential care, but all age-dependent social policies that might affect use of medical services and hospitals.
To calculate annual per capita costs, we summed physician and hospital costs for each individual for each of 2002 and 2003. We next ranked each individual by per capita costs for each year, from lowest to highest, and arranged these into deciles. Costs were divided into three categories on the basis of natural breaks in the distribution of expenditures. We defined as low costs the lowest-spending 70% of the population, moderate costs the next 20% and high costs the remaining 10% of the population. The mean annual per capita costs for each of these categories were $96, $600 and $6,635, respectively, all measured in 2002 dollars. Distinguishing between low, moderate and high costs in this way is also useful for policy simulation, in which “catastrophic” costs are often associated with the costliest 10% of the population (cf. Forget et al. 2002).
To calculate predicted lifetime costs, we defined the cost categories on the basis of the experience of the entire population. This means that the per capita costs assigned to low, moderate and high users do not vary by age and sex in our model. Instead, the probabilities that individuals will incur low, moderate or high costs (or die) will change with age and sex to reflect the actual experience of the population. In order to determine whether patterns of population costs are stable over time, we then examined the distribution of annual per capita costs between 1997 and 2003. The same pattern of a high-cost 10%, a moderate-cost 20% and a low-cost 70% persisted. When the distributions were compared in constant dollars, mean per capita costs for each of the three categories did not differ significantly by year.
Transition probabilities
We constructed 10 different transition matrices for males and 10 for females based on the probability by age and sex that an individual in each cost category would stay in the same category in the next year, move to one of the other two cost categories or die. The categories were based on previous analyses of per capita expenditure by age group: <1 year of age, 1–4, 5–14, 15–19, 20–24, 25–34, 35–44, 45–54, 65–74 and ≥75. Age categories beyond 75 were not further subdivided because the relatively small number of surviving men might introduce instability into the estimates.
Each live birth in Manitoba in 2002 was assigned to low-, moderate- or high-cost categories in the first instance, based on costs for infants less than one year of age in Manitoba in 2002. Moderate costs were incurred by 74.45% of females and 68.75% of males, while 21.99% of females and 28.41% of males incurred high costs. Only 3.56% of female infants and 2.84% of male infants fell into the low-cost category. We then calculated the probability that a low-cost female infant in 2002 would move to a low-, moderate- or high-cost category in 2003 or die before the year was complete, and repeated the process for moderate- and high-cost females, and low-, moderate- and high-cost male infants.
Table 1 illustrates the transition probabilities for male and female infants less than one year of age in 2002. Those infants who incurred moderate costs in 2002 were the least likely to die during the year and the most likely to transition to a low-cost category in 2003. This finding is as one might expect, since most infants have a number of routine contacts with the healthcare system during their first year. Moderate-cost infants received the medical services that normal infants are expected to receive during their first year of life. Those infants who incurred high costs in 2002 were more likely to incur moderate or high costs in subsequent years. Again, this finding is as expected, because the high-cost infants include those with birth anomalies and those born too early or too small.
TABLE 1.
Transition probabilities for male and female infants (<1 year) in 2002–2003
| 2002 category | 2003 category | |||
|---|---|---|---|---|
| Low | Moderate | High | Dead | |
| MALES | ||||
| Low | 0.6599 | 0.2183 | 0.1015 | 0.0203 |
| Moderate | 0.6980 | 0.2418 | 0.0596 | 0.0006 |
| High | 0.5341 | 0.3121 | 0.1310 | 0.0228 |
| FEMALES | ||||
| Low | 0.7087 | 0.1739 | 0.1087 | 0.0087 |
| Moderate | 0.7470 | 0.2068 | 0.0453 | 0.0008 |
| High | 0.5862 | 0.2885 | 0.1056 | 0.0197 |
Infants may incur low costs during their birth year for two different reasons. If an infant dies during the year, total costs incurred during that year may be quite low, depending on when the death occurred. In this case, the low cost is a statistical anomaly resulting from the way we gather costs. But an infant may also incur low healthcare costs during her first year of life because she does not receive the routine healthcare she ought to receive. Such infants would include children whose family circumstances put them at increased risk for injury or illness, with subsequent higher healthcare costs. Our data show that the low-cost infants who survived the year were more likely than their counterparts who incurred moderate costs to be in a high-cost category during their second year of life. Female low-cost infants were even more likely than high-cost infants to incur high costs during their second year.
Transition probabilities vary by age and sex, and are based on the costs incurred by an individual in the previous year. This approach builds “memory” into the model, in that young men incurring high costs in 2002 were much more likely to return to a low- or moderate-cost category in 2003 than were elderly women who incurred high costs in 2002 (81% versus 53%) (Table 2). And yet, young men who incurred high costs in 2002 were still much more likely to incur high costs in 2003 than were men of the same age having low costs in 2002 (18% versus 2.5%). Even though we have used only one-year transitions, the model recognizes the persistence in healthcare expenditure and reflects the way that past use of the healthcare system is mediated by age and sex. It builds in the higher probability that high-cost individuals will remain higher cost in subsequent years, but recognizes that this situation is particularly true for older people than for younger. Linear interpolation was used to smooth the transition probabilities among age categories, so there is no threshold effect as individuals age.
TABLE 2.
Transition probabilities for young males (20–24) and elderly females (65–74) in 2002–2003
| 2002 category | 2003 category | |||
|---|---|---|---|---|
| Low | Moderate | High | Dead | |
| MALES (20–24) | ||||
| Low | 0.9229 | 0.0511 | 0.0253 | 0.0007 |
| Moderate | 0.6483 | 0.2619 | 0.0890 | 0.0009 |
| High | 0.6463 | 0.1673 | 0.1792 | 0.0071 |
| FEMALES (65–74) | ||||
| Low | 0.6512 | 0.2494 | 0.0937 | 0.0057 |
| Moderate | 0.2314 | 0.5602 | 0.2056 | 0.0027 |
| High | 0.1685 | 0.3660 | 0.4012 | 0.0643 |
Many attempts to model lifetime costs have been criticized for not distinguishing between survivors and decedents. Without this distinction, estimates of lifetime costs tend to be biased upwards because mean age-dependent costs for the elderly are inflated by the high costs incurred by those at the end of life. Our modelling strategy recognizes that individuals in any cost category and at any age may die. The transition probabilities are based on the experiences of an actual population in particular years, adjusting for the increased probability of death with age and for individuals incurring high costs.
The stability of the matrices was tested by calculating single-year transition matrices for men and women for 1997–1998, 1998–1999, 1999–2000 and 2002–2003. Individual transition probabilities for particular age–sex cost categories varied slightly; for example, the probability that low-cost 20- to 24-year-old males would remain low cost the following year did vary at the third decimal point. However, using constant dollars, the distribution of predicted lifetime costs did not vary significantly over the period. From this finding we concluded that the transition probabilities were relatively stable, at least over the short run. Over longer periods of time, probabilities will change to reflect changes in medical technology, as well as the morbidity and mortality experience of the population. Having transition probabilities for only a few years, we did not attempt a second-order Markov model, which would have required assumptions about the distribution from which the annual transition probabilities were drawn.
Simulation
We constructed a Markov model based on age-dependent probabilities for males and for females. As noted above, per capita costs assigned to low, moderate and high users do not vary by age and sex in our model, but the probabilities that individuals will be in each category (including death, an absorbing state) change with age and sex to reflect the actual experience of the population. We used TreeAge Pro Software to simulate the model. Figure 1 represents the costing tree for males, which is identical to that for females except that the initial distribution of the birth cohort varies to reflect the higher proportion of male infants who are high cost.
FIGURE 1.
A costing tree for males
Figure 1 represents a Markov model, which is based on the concept of a decision tree. A cohort enters the model at the left. At each node, the model assigns an individual to a particular branch based on the age- and sex-dependent transition probabilities calculated from the data. When an individual “dies,” the model calculates lifetime costs and life-years. As long as an individual survives, the model reassigns him to a particular branch, with the probability of entering a high-cost category rising with age and dependent on past utilization.
Figure 1 represents a Markov model. We can simulate costs by running a cohort through this model, and allowing the model to assign actual outcomes based on the transition probabilities drawn from our data.
For example, the first member of the cohort enters the model from the left. Based on our data, the model will assign this individual to the moderate-cost category in his first year with a probability of 0.6875, to a high-cost category with a probability of 0.2841 and to a low-cost category with a probability of 0.0284. For each of these possibilities, the infant may survive his first year or he may die before his first birthday. His fate will be chosen by the model based on the transition probabilities we have calculated from the data. If he dies, the model calculates his total lifetime cost and his total number of years of life. If he survives his first year, the model will assign him to a cost category in his second year based on transition probabilities. Again, he may die or he may survive. If he dies, the model calculates his lifetime cost and his total years of life. If he survives, the model will assign him to a cost category in his third year of life. As the individual exits the right-hand side of the model alive, he is sent back to repeat the costing cycle for another year. As he ages, the transition probabilities adjust to increase his probability of being assigned to a high-cost category. For each individual in the cohort, the model will create a unique synthetic life based on the transition probabilities calculated from the actual data. Each individual in our cohort is a fiction created by the model, but together they represent the distribution of costs and outcomes that our data contain.
Two methods of Monte Carlo simulation were used. First, a cohort estimation technique permitted both calculation of mean lifetime costs for men and women and estimation of the proportion of lifetime costs incurred in high-, moderate- or low-cost years. It also allowed calculation of both life expectancy and the number of high-, moderate- and low-cost years a typical male or female can expect. Individuals in a birth cohort were assigned to an initial cost category based on population probabilities; the experience of the entire birth cohort was modelled until all died. Second, microsimulation trials were used to estimate the model. We allowed 100,000 men and 100,000 women to move through the model from birth to death and calculated the distribution of lifetime costs across the population.
Results
Lifetime costs for a typical individual
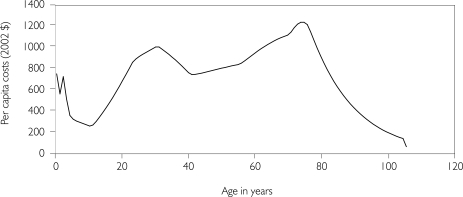
Women incur a mean cost of $89,741 over a lifetime in hospital and physician costs, 40% more than the $64,091 incurred by men (Figures 2 and 3). Consistent with other studies, mean per capita costs decline through childhood. Not surprisingly, women show higher per capita costs than do men during peak childbearing years. The typical female can expect to live almost six years longer than the typical male. Although a similar proportion of lifetime costs occur in high-cost years for men and women, the typical woman can expect more high-cost years. She will incur 81.6% of her lifetime costs in her 11 high-cost years, while he will incur 80.5% of his lifetime costs in his 7.8 high-cost years. The typical female will incur 20 moderate-cost years compared to 12 for the typical male. Only 47 of her years will be low cost, compared to his 52.6. The life expectancies generated by this model – 78 for women and 72.4 for men – are consistent with Canadian mean life expectancies at birth for the 1980–1982 cohort (Statistics Canada 2005). Life expectancies in Canada, and in Manitoba, have increased since then.
FIGURE 2.
Mean annual per capita costs by age (females, 2002–2003)
FIGURE 3.
Mean annual per capita costs by age (males, 2002–2003)
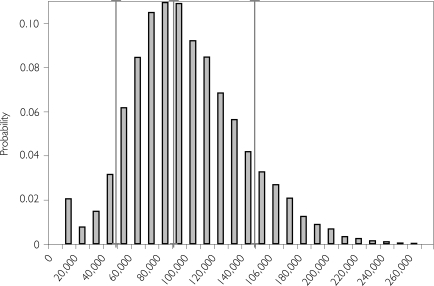
Distribution of lifetime costs across a population
In order to calculate the distribution of lifetime costs, we estimated the Markov models using Monte Carlo microsimulation trials (Figures 4 and 5). As might be expected, lifetime costs are somewhat less skewed than are per capita costs in any single year. However, the distribution is far from normal; costs are not tightly grouped around the mean. For women, mean lifetime costs are $89,722, with a standard deviation of $38,776. Median costs for women were $86,125. Ten per cent of women incur lifetime costs of less than $43,843. For men, the mean is $64,052 with a standard deviation of $35,331. Median costs for men were $59,819, while 10% of men incurred lifetime costs of less than $22,450.
FIGURE 4.
The distribution of lifetime costs (females, 2002–2003)
Each vertical bar in Figure 5 represents the probability that a female will incur lifetime costs of the magnitude on the horizontal axis, measured in 2002 dollars. The three vertical lines represent the 10th, 50th and 90th percentiles. About 10% of women have a lifetime cost of less than $43,843 and 50% have a lifetime cost of less than $86,125.
FIGURE 5.
The distribution of lifetime costs (males, 2002–2003)
Each vertical bar in Figure 4 represents the probability that a male will incur lifetime costs of the magnitude on the horizontal axis, measured 2002 dollars. The three vertical lines represent the 10th, 50th and 90th percentiles. About 10% of men have a lifetime cost of less than $22,450 and 50% have a lifetime cost of less than $59,819.
Based on the Monte Carlo trials, the typical woman can expect 11 high-cost years, but the standard deviation is 5.33. Fully 10% can expect more than 18 high-cost years; 2.5% can expect more than 23. A typical man can expect 7.8 high-cost years, with a standard deviation of 4.9 years. Ten per cent of men can expect more than 14 high-cost years, and 2.5% can expect more than 19 high-cost years.
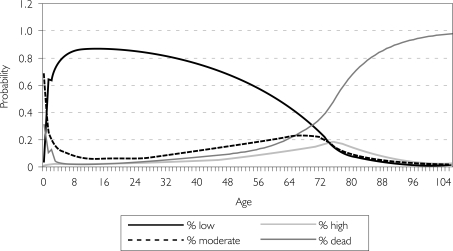
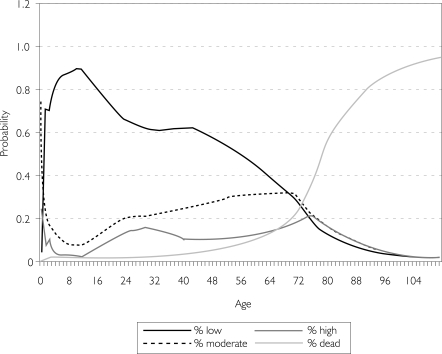
The probability of incurring high costs by age and sex
Our analysis uses transition probabilities and focuses on the distribution of age- and sex-dependent costs. Although we cannot determine when, in any individual's life, high-cost periods will occur, the pattern of probabilities that govern individual costs can be examined. Because the probability of falling into a particular cost category in any year depends on an individual's previous healthcare costs as well as age and sex, Monte Carlo estimation allows recovery of the pattern of lifetime probabilities from simulation. The probabilities of incurring low, moderate and high costs by age and sex are shown in Figures 6 and 7.
FIGURE 6.
Probability of incurring low, moderate and high costs by age (males, 2002–2003)
FIGURE 7.
Probability of incurring low, moderate and high costs by age (females, 2002–2003)
At any age, men are more likely to be low-cost healthcare consumers than to be moderate- or high-cost users. Although mean per capita healthcare costs clearly increase with age and the typical male will incur 7.8 high-cost years in his lifetime, an individual male at any age has a greater probability of incurring low costs than of incurring higher costs. Indeed, by the time the probability of incurring high costs exceeds those of incurring low costs (at age 76), a male is more likely to be dead than still alive and incurring any costs.
The story differs for women. Women, like men, have a greater probability of being low-cost users than high-cost users all their lives. In part because of childbirth, they are more likely to be moderate-cost users throughout much of their adulthood than are men; by age 71, the probability of being a moderate-cost user exceeds that of being a low-cost user. However, as was the case for men, at the age when the probability of incurring high costs exceeds that of incurring low costs, women are more likely to be dead than still alive incurring costs. While the typical female will incur 11 high-cost years in her lifetime, and while mean per capita costs for women increase with age, an individual woman younger than 71 still has a greater probability of incurring low costs than she has of incurring higher costs in any given year.
Beyond the age of 75, both male and female survivors are about equally likely to incur high, moderate or low costs.
Discussion
Healthcare costs will be affected as a larger cohort moves through the age spectrum, followed by a smaller cohort. This pattern implies that mean per capita healthcare costs are relevant for social planners. A greater number of individuals facing a greater probability of incurring high healthcare costs will indeed cost more in the aggregate; this factor must be taken into account when healthcare budgets are determined. Efforts to improve the efficiency of healthcare delivery make sense on grounds of both efficiency and distribution.
The relationship between individual aging and anticipated healthcare costs, however, is not a simple one. Each individual faces a greater probability of incurring higher healthcare costs as he or she ages, but the greatest likelihood is that, even in advanced age, most individuals will incur relatively low costs. However, this finding results in part from our decision not to include pharmaceuticals and costs for personal care homes, which are not mandated by the Canada Health Act. These costs are covered for some people, at least in part, in all provinces, but the Act does not require them to be covered, and different provinces have adopted different schemes. Effectively, our results show that publicly funded services are not likely to be unsustainable because of demographic changes; rather, unsustainability stems from the fact that large portions of age-related spending fall outside the Canada Health Act. Those areas – pharmaceuticals and personal care homes – are where we will see the greatest pressure for public–private partnerships and for creative financing options in coming years.
Age-specific social policies
The path-dependence of probabilities, as shown in Figures 6 and 7, implies that older individuals who move into high-cost categories are more likely to stay there than are younger individuals. Nevertheless, for any individual, the relationship between healthcare costs and aging is far from clear and predictable. This fact presents a number of implications for social policy. The simplest, and least satisfactory, set of policies designed to deal with an aging population confounds individual aging and population aging by designing a set of age-specific health benefits. Age-specific policies, such as exempting individuals over age 65 from some healthcare costs that others bear out of pocket or through third-party insurance, are likely to subsidize many low-cost seniors at the expense of younger individuals with higher costs. For example, most Canadian provinces have chosen in the past few years to cease paying for such services as eye examinations for those between the ages of 18 and 64 while retaining coverage for those over age 65. Healthcare benefits based only on age, as in the case of US Medicare, similarly fail to take into account the wide variety of individual experience within any age–sex group. A policy based on age alone, rather than individual healthcare costs, will lead to a substantial transfer to healthy seniors from the younger individuals falling into the high-needs category.
However, relying upon private insurance to cover some of the costs currently paid under the Canada Health Act for younger people, while retaining public coverage for seniors, would not appear to be a satisfactory answer. High-risk individuals face notorious difficulty in accessing private health insurance at reasonable costs. Risk-adjustment software that predicts healthcare expenditures for every individual in a defined population on the basis of past utilization is available and is commonly used by private health insurance companies to set premiums. As we have seen, healthcare costs tend to persist over time for all individuals, and this persistence increases with age. Those individuals likely to be most in need of healthcare insurance are, therefore, the least likely to be able to access private insurance at reasonable premiums, the most likely to exceed lifetime limits and the most likely to be disadvantaged by the widespread uninsurability of existing conditions. Limiting public coverage for certain services under the Canada Health Act on the basis of age will not lead to equitable outcomes.
Healthcare savings accounts
The large number of healthy low-cost seniors, however, should not lead to complacency about other proposals. In recent years, one proposal that gained a lot of attention in Canada before fading from the policy scene was the suggestion that universal health insurance for physician and hospital services should be replaced by healthcare savings accounts, in which each individual's allowance or entitlement would be paid by the government to the individual, based on some proportion of mean age and sex-dependent healthcare costs (Forget et al. 2002; Deber et al. 2004). The individual would then be responsible for paying all physician and hospital costs from that allowance or, should healthcare costs exceed the allowance, out of pocket. Allowing individuals to save surpluses in low-cost years to pay for catastrophic costs in high-cost years was imagined to make the system sustainable. Figures 4 and 5 emphasize the significant variation in lifetime healthcare costs around the age- and sex-dependent mean.
If costs were tightly distributed about the mean, then determining the optimal annual allocation to a healthcare savings account would be relatively simple; this allocation could pay costs over a lifetime if surpluses were retained to pay for excess costs in high-cost years. But lifetime costs vary tremendously, suggesting a significant cohort of individuals who incur high costs over much of their lives. Their catastrophic costs will continue to be a policy issue that health savings accounts cannot address. Dealing with catastrophic costs through other mechanisms (such as government-provided health insurance for the costliest 10% of individuals in any particular year), coupled with a program of healthcare savings accounts for non-catastrophic costs, would do little to contain government expenditure in the aggregate. The vast bulk of healthcare costs are incurred by those few individuals incurring catastrophic costs.
Healthcare savings accounts in the United States have attempted to handle this problem by allowing individuals to pay the premiums for catastrophic health insurance from these sorts of accounts. To the extent that individuals with a history of high-cost episodes remain insurable at reasonable cost, the purchase of catastrophic insurance will reduce the threat to persistently high-cost individuals. However, co-payments and annual (and lifetime) limits, the difficulty of insuring against costs incurred through existing conditions, and risk-based premiums lessen the protection that catastrophic insurance provides to high-cost individuals.
Cautions for policy makers
Mean healthcare costs are clearly age dependent; an aging population will imply increasing aggregate costs. Policy responses to this inevitability, however, often confound mean age-dependent costs for a population with the actual risk faced by a particular individual. The “typical” individual clearly faces a lifetime of gradually and then rapidly increasing costs as he or she ages. Any particular individual, however, is not “typical”; up to 75 years of age, each individual has a significantly greater probability of incurring low healthcare costs than moderate or high healthcare costs.
This study shows that per capita healthcare costs for individuals of a particular age and sex vary, not only at a point in time but over a lifetime as well. Policy initiatives based on population means that ignore the reality of individual variation, both at any point in time and over a lifetime, can only increase inequity and inefficiency.
Acknowledgements
We are grateful for financial support from the Canadian Institutes for Health Research (MOP-127833). The results and conclusions are those of the authors; we are indebted to Health Information Services, Manitoba Health and Healthy Living, for providing data (MB Health No. 2002/2005 – 18). No official endorsement by Manitoba Health and Healthy Living is intended or implied.
Contributor Information
Evelyn L. Forget, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB.
Leslie L. Roos, Department of Community Health Sciences, University of Manitoba; Manitoba Centre for Health Policy, Winnipeg, MB.
Raisa B. Deber, Department of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Randy Walld, Manitoba Centre for Health Policy, Winnipeg, MB.
References
- Alemayehu B., Warner K.E. The Lifetime Distribution of Health Care Costs. Health Services Research. 2004;39(3):627–42. doi: 10.1111/j.1475-6773.2004.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barer M.L., Evans R.G., McGrail K.M., Green B., Hertzman C., Sheps S.B. Beneath the Calm Surface: The Changing Face of Physician-Service Use in British Columbia, 1985/86 versus 1996/97. Canadian Medical Association Journal. 2004;170(5):803–7. doi: 10.1503/cmaj.1020460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler J.R.G. Policy Change and Private Health Insurance: Did the Cheapest Policy Do the Trick? Australian Health Review. 2002;25(6):33–41. doi: 10.1071/ah020033. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI) Table C.3.1: Public Sector Health Expenditure, by Use of Funds, Canada, 1975–2005 – Current Dollars. 2005 Retrieved June 17, 2008. < http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=media_07dec2005_e#tables>.
- Chaoulli v. Quebec (Attorney General) 2005. 1 SCR 791, 2005 SCC 35.
- Deber R.B., Forget E.L., Roos L.L. Medical Savings Accounts in a Universal System: Wishful Thinking Meets Evidence. Health Policy. 2004;70(1):49–66. doi: 10.1016/j.healthpol.2004.01.010. [DOI] [PubMed] [Google Scholar]
- Diehr P., Derleth A., Newman A., Cai L. Is the Number of Sick Persons in a Cohort Constant over Time? 2005 Discussion Paper No. 264. Retrieved June 17, 2008. < http://www.bepress.com/cgi/viewcontent.cgi?article=1097&context=uwbiostat>.
- Forget E.L., Deber R.B., Roos L.L. Medical Savings Accounts: Will They Reduce Costs? Canadian Medical Association Journal. 2002;167(2):143–47. [PMC free article] [PubMed] [Google Scholar]
- Forget E.L., Deber R.B., Roos L.L., Walld R. Canadian Health Reform: A Gender Analysis. Feminist Economics. 2005;11(1):125–43. [Google Scholar]
- Fuchs V. Health Care for the Elderly: How Much? Who Will Pay for It? Health Affairs (Millwood) 1999;18(1):11–21. doi: 10.1377/hlthaff.18.1.11. [DOI] [PubMed] [Google Scholar]
- Hogan S., Hogan S. Commission on the Future of Health Care in Canada. Ottawa: Health Canada; 2002. How Will the Ageing of the Population Affect Health Care Needs and Costs in the Foreseeable Future? Discussion Paper No. 25. Retrieved June 17, 2008. < http://www.hc-sc.gc.ca/english/pdf/romanow/pdfs/25_Hogan_E.pdf>. [Google Scholar]
- Hogan S., Lise J. Life Expectancy, Health Expectancy and the Life Cycle. Horizons. 2004;6(2):17–20. [Google Scholar]
- Knickman J.R., Snell E.K. The 2030 Problem: Caring for Aging Baby Boomers. Health Services Research. 2002;37(4):849–84. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J., Liu X., Tu E., Whitelaw N. Probabilities and Lifetime Durations of Short-Stay Hospital and Nursing Home Use in the United States, 1985. Medical Care. 1996;34(10):1018–36. doi: 10.1097/00005650-199610000-00004. [DOI] [PubMed] [Google Scholar]
- Lubitz J., Beebe J., Baker C. Longevity and Medicare Expenditures. New England Journal of Medicine. 1995;332(15):999–1003. doi: 10.1056/NEJM199504133321506. [DOI] [PubMed] [Google Scholar]
- Lubitz J.D., Riley G.F. Trends in Medicare Payments in the Last Year of Life. New England Journal of Medicine. 1993;328(15):1092–96. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- Maguire M. Making Arrangements for Ageing Populations. OECD Observer. 1987;19(148):4–9. [PubMed] [Google Scholar]
- Meerding W.J., Bonneux L., Polder J.J., Koopmanschap M.A., van der Maas P.H. Demographic and Epidemiological Determinants of Healthcare Costs in Netherlands: Cost of Illness Study. British Medical Journal. 1998;317(7151):111–15. doi: 10.1136/bmj.317.7151.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monheit A.C. Persistence in Health Expenditures in the Short Run: Prevalence and Consequences. Medical Care. 2003;41(7):53–64. doi: 10.1097/01.MLR.0000076046.46152.EF. [DOI] [PubMed] [Google Scholar]
- Mustard C.A., Kaufert P., Kozyrskyj A., Mayer T. Sex Differences in the Use of Healthcare Services. New England Journal of Medicine. 1998;338(23):1678–83. doi: 10.1056/NEJM199806043382307. [DOI] [PubMed] [Google Scholar]
- Reinhardt U.E., Hussey P.S., Anderson G.F. Cross-National Comparisons of Health Systems Using OECD Data, 1999. Health Affairs (Millwood) 2002;2002(3):169–81. doi: 10.1377/hlthaff.21.3.169. [DOI] [PubMed] [Google Scholar]
- Roos L.L., Mustard C.A., Nicol J.P., McLerran D.F., Malenka D.J., Young T.K., Cohen M.M. Registries and Administrative Data: Organization and Accuracy. Medical Care. 1993;31(3):201–12. doi: 10.1097/00005650-199303000-00002. [DOI] [PubMed] [Google Scholar]
- Roos N.P., Montgomery P., Roos L.L. Healthcare Utilization in the Years Prior to Death. Milbank Quarterly. 1987;65(2):231–54. [PubMed] [Google Scholar]
- Scitovsky A.A. Medical Care in the Last Twelve Months of Life: The Relation between Age, Functional Status, and Medical Care Expenditures. Milbank Quarterly. 1988;66(4):640–60. [PubMed] [Google Scholar]
- Spillman B.C., Lubitz J. The Effect of Longevity on Spending for Acute and Long-term Care. New England Journal of Medicine. 2000;342(19):1409–15. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. Life Expectancy at Birth, by Sex, by Province. 2005 Retrieved June 17, 2008. < http://www40.statcan.ca/l01/cst01/health26.htm>.
- Waldo D.R., Sonnefeld S.T., McKusick D.R., Arnett R.H. Health Expenditures by Age Group, 1997 and 1987. Health Care Financial Review. 1989;10(4):111–20. [PMC free article] [PubMed] [Google Scholar]