Abstract
Fifty years ago, Canadian and US life expectancies were roughly equal. Now, however, Canadians are, on average, healthier than Americans. To discover the reasons behind this trend, the authors compared Canada and the United States on a range of determinants of health based on data from 1950 to the present. Their analysis yielded three conclusions: (1) greater economic well-being and spending on healthcare did not yield better health outcomes; (2) public provision and income redistribution trump economic success where population health is concerned; and (3) the gradual development of public provision represents the build-up of social infrastructure that has long-lasting effects on health status. The authors contend that in the context of thinking about population health, the historical, dynamic approach casts a clearer light on trends than does the cross-sectional approach.
Abstract
Il y a cinquante ans, l'espérance de vie au Canada et aux États-Unis était sensiblement la même. Aujourd'hui, toutefois, les Canadiens sont en moyenne plus sains que les Américains. Afin de connaître les raisons de cette tendance, les auteurs ont comparé les deux pays en fonction d'un éventail de déterminants de la santé, à partir de données recueillies de 1950 à nos jours. L'analyse permet de dégager trois conclusions : (1) un bien-être économique accru et des dépenses plus élevées dans les services de santé ne donnent pas de meilleurs résultats pour la santé; (2) en matière de santé de la population, la prestation de services publics et la redistribution du revenu ont plus de poids que la prospérité économique; (3) le développement graduel des services publics se traduit par l'accroissement d'une infrastructure sociale qui a des effets à long terme sur l'état de santé. Les auteurs affirment que, dans le contexte de la santé des populations, une approche historique dynamique permet de mieux comprendre ces tendances qu'une approche transversale.
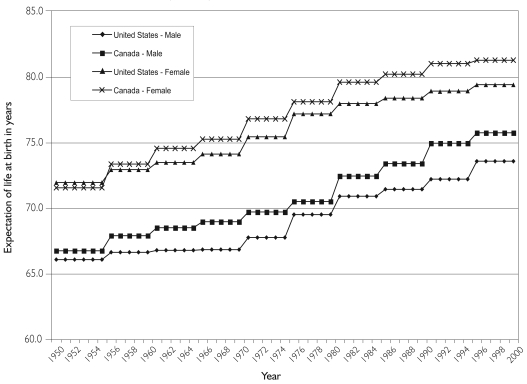
Canadians are, on average, healthier than Americans. This is widely known, at least among students of such matters. Less widely known is that this situation was not always so. Fifty years ago, life expectancies were more or less equal on both sides of the border, as were infant mortalities. The gap shown in Figure 1 has emerged over the last half century. Why did this happen?
FIGURE 1.
Male and female life expectancy in Canada vs. the United States
To answer this question, we need to start with the work of Thomas McKeown (1979). McKeown studied mortality and its putative determinants, as they gradually unfolded over decades, in 19th- and 20th-century England and Wales. This long view demonstrated conclusively that the factors that led to large declines in mortality from the major infectious diseases of antiquity were to be found outside the medical care system per se, since the force of mortality from these diseases declined in the decades prior to the advent of effective healthcare interventions.
McKeown's work redirected our attention towards such factors as economic growth, rising living standards and improved nutrition. This shift has been foundational for the field of population health and a prime motivator of the search for determinants of health embedded in those aspects of society that are not specifically designed to support health or fight disease. Often neglected, however, is McKeown's view of time.
Population health has rarely returned to the type of evidence McKeown used: tracing health trends that emerge slowly over decades and trying to account for them according to gradually evolving factors deeply embedded in society. Instead, we have tended to focus on cross-sectional and short-term follow-up studies. These have been very useful in many respects. They have demonstrated that, in all wealthy countries, there is a gradual, non-threshold decline in health status from the richest to the poorest groups and from the most to the least educated groups in society. This phenomenon is known as the socio-economic gradient in health.
Short-term follow-up studies have also shown which countries in Central and Eastern Europe did, or did not, experience a profound health crisis immediately following the collapse of the Soviet system in the late 1980s and early 1990s. But short-term studies have not given us satisfactory answers to the question of why some wealthy societies are healthier than others. This is a critical question for population health and health policy alike.
The long-term Canada–United States comparison clearly demonstrates that slow-moving processes can cumulate over time to have big effects. Figure 1 compares American and Canadian life expectancy, in five-year averages, from 1950 to 2000, showing the gap gradually widening in favour of Canada until, by the end of the 20th century, it reached approximately two years. One crucial detail is that during the late 1970s, the gap narrowed considerably. But starting around 1980, it re-opened and has not closed again. Although differences in infant mortality contributed to the gap, it is driven, primarily, by differences in adult mortality. A two-year life expectancy gap may not sound large, but during ages 25 to 64, it translates into annual mortality rates that are 30% to 50% higher in the United States.
Between the early 1970s and the late 1990s, the socio-economic gradient in health status remained stable in Canada. Over the 25-year period from 1971 to 1996, each income quintile experienced roughly equal gains in life expectancy (Wilkins et al. 2002). In the United States, by contrast, the highest income quintiles gained life expectancy at a significantly faster pace than the lowest quintile (Singh and Siahpush 2002). By the end of the 20th century, the poorest 20% of Canadians enjoyed the same life expectancy as Americans of average income (Singh and Siahpush 2002; Wilkins et al. 2002). Something big happened here, albeit gradually, and it deserves recognition and explanation.
In order to understand these emerging differences, we compared Canada and the United States on a range of determinants of health for which routine data have been collected for all or most of the period between 1950 and the present (Siddiqi and Hertzman 2007). This analysis, briefly summarized here, led us to three key conclusions:
1. Greater economic well-being and spending on healthcare did not yield better health outcomes
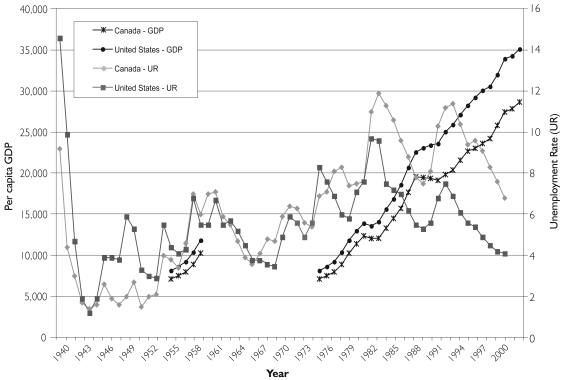
As in McKeown's work, our most definitive conclusions are the negative ones: identifying what did not matter. From 1975 to 1988, purchasing power parity (PPP)-adjusted gross domestic product (GDP) per capita grew in both Canada and the United States, tracking closely through business cycles (Figure 2). Throughout this period, the United States remained approximately 10% higher than Canada. From 1988 to 1993, however, there was a brief break in this pattern. Income essentially stagnated in Canada while continuing to grow in the United States. After 1994, parallel growth resumed, but the ground lost during the five-year period of stagnation in Canada was not made up. PPP-adjusted GDP per capita remained approximately 20% lower than in the United States.
FIGURE 2.
Per capita gross domestic product and unemployment rates, 1940–2002
Unemployment rates in the two countries show a similar parallelism. From the end of the Second World War until 1982, unemployment rates in Canada and the United States overlapped from business cycle to business cycle, such that no systematic trend can be detected. But from 1982 until 2000, unemployment rates were consistently 2% to 4% higher in Canada than in the United States.
During the 1960s, Canada spent approximately 0.5% of GDP more on healthcare than the United States did. Healthcare spending in the two countries then converged, however, in the 1970–1973 period, at approximately 7% of GDP. After that, spending rates diverged dramatically. From 1973 to 1993, spending on healthcare in Canada rose to 10% of GDP and stayed between 9% and 10% until 2002. In the United States, spending on healthcare rose to 13.5% by 1993, and further to 14% by 2002.
Canada's universal, single-payer medicare plans (for hospitals' and physicians' services) were fully in place by 1971, and the spending gap began to emerge at exactly that point. (The US medicare plan, established in 1965, is universal only for seniors.) Thus, the 30-year period subsequent to 1971 has been characterized by universal access to care “on equal terms and conditions” in Canada, but by much more rapidly growing spending (though unequal access) in the United States. As of the end of this follow-up period, Canada was spending 4% of GDP less than the United States on healthcare. (By 2006, the difference was over 6%.)
The conclusion is clear: the country with lower rates of economic growth, higher unemployment and less spending on healthcare far outstripped its neighbour in mortality reduction.
2. Public provision and income redistribution trump economic success where population health is concerned
In 1980, public social expenditures consumed approximately 13% of GDP in both Canada and the United States. By 1990, a large gap had opened, such that Canada was spending more than 4% of GDP more than the United States (>18% and <14%, respectively). These rates were largely unchanged by 1998. In the 1970s, the Gini coefficient of income inequality, post-tax and post-transfer, was approximately two points lower (i.e., the income distribution was more egalitarian) in Canada than in the United States. Canadian Gini coefficients were in the high 20s in Canada and in the low 30s in the United States. From then until the late 1990s, the Gini stayed in the same range in Canada but increased in the United States. By the late 1980s, there was a five-point gap, and by the late 1990s this had grown to approximately seven points. In other words, over this time and by this measure, the distribution of income became increasingly unequal in the United States but not in Canada. The United States has long been a more unequal society than Canada, but the difference has become much more marked since 1980.
Taxes generally take more from those with higher incomes, and transfer payments provide more support for those with lower incomes, thus mitigating the inequality of incomes received from employment alone. In the early 1980s, the net impact of the Canadian tax and transfer programs (that is, their effectiveness in income redistribution) was to reduce the Gini by approximately 24%. During the 1980s and early 1990s, the redistributive work of these programs rose to a 31% reduction in Gini, then fell to slightly under 30% by the late 1990s. In the United States the redistributive work of taxes and transfers remained between 22.5% and 24.5% from the late 1980s to the late 1990s. Thus, the relative redistributive work of the Canadian programs rose compared to the US programs from the late 1980s to the late 1990s. “Market” incomes, before payment of taxes and receipt of transfers, were becoming increasingly unequal in both countries over this period, but Canadian fiscal and other public policies significantly mitigated the impact of this trend. American policies did not.
The relative differences between the countries were particularly marked in their success at poverty reduction (Zuberi 2001). In 1974–1975, taxes and transfers reduced the poverty rate by approximately 11% in both countries. By 1994, poverty reduction had risen to 24% in Canada, but only to 13% in the United States.
In contrast to economic growth and health expenditure, these time trends of changing public expenditure and income redistribution correspond to the changes in relative health status and the relative steepness of the socio-economic gradient in Canada and the United States. The period during which Canadian life expectancy increasingly surpassed the United States was a time when Canada's levels of public spending on social programs and the redistributive impact of its fiscal system and social protection policies worked much more powerfully than those in the United States to maintain a more equitable distribution of income in the face of contrary market forces. The effects go well beyond money income: equity of access to education, as well as, of course, healthcare (not shown here) surpassed those in the United States.
3. The gradual development of public provision represents the build-up of social infrastructure that has long-lasting effects on health status
Public provision and income redistribution do not fall from the sky, but are products of a society's evolving institutional landscape. A powerful example of potential health benefits comes from the fact that, despite periods of relatively high unemployment, Canadian health status continued to improve. Where the labour market intersects with social protection, Canada differed from the United States during this period. In particular, Canada scored higher on indexes of unemployment protection, labour relations and corporate governance (Estevez-Abe et al. 2001).
Unemployment protection represents the extent to which wages and benefits accrue to individuals, even in times of unemployment. The higher the unemployment protection score, the greater the wages and benefits afforded to unemployed workers. This index depends upon a set of social policies that are designed to stabilize the labour market and reduce risk (as does the scale on labour relations). Unemployment protection, in particular, is mandated through policies that transfer financial risk to corporations, governments and insurance companies. Such policies are meant to help maintain and sustain the middle class by reducing the burden of risk on individuals in the labour market who are less able to bear it. As Zuberi (2006) has shown, Canadian unemployment protection policies have also benefited highly vulnerable members of the labour force, such as immigrant workers, in ways that US policies have not.
Corporate governance refers to the extent to which the state has a role in determining and enforcing the rights and responsibilities of corporations. Higher scores on this index suggest greater government input. Compared with the United States, Canada features lower incomes for chief executive officers and other upper management and higher tax rates (and fewer loopholes) for large corporations. These features of the institutional landscape are reasonable places to look for an explanation of the observation that Canadians have experienced health gains even during periods of high unemployment.
Although this is only one example, there is reason to believe that comparisons of public policies in a number of other areas with implications for health – such as immigrant-welcoming policies, access to education, regional equalization and the organization of urban space, to name a few – show a similar advantage for Canada.
Understanding the origin and development of institutions with health-supporting or health-threatening capacity poses a timescale challenge of its own. How far back in time should we go? Would telling a full, complete story of institutional evolution and public provision in the United States have to start at least as far back as the Depression-era New Deal? Would it have to take account of the post-war GI bills and the Great Society programs prior to the Reagan-era rollbacks, when American health status started its current relative decline? In Canada, the history might stem from a more muted response to the Great Depression; but a gradual phasing in of national hospital and unemployment insurance, old age pensions, physician coverage, federal–provincial social assistance transfers, increasing secondary and tertiary education subsidies, increasingly progressive labour legislation after the Second World War, and the gradual embrace of a series of policies and programs that have turned Canada into the world's most multicultural society. From the standpoint of health, these represent a relatively successful evolutionary trajectory in Canada and a relatively unsuccessful one in the United States. Relative mortality measures provide a hard-edged way of keeping score.
Conclusions
The comparative perspective and long-term view employed here have allowed us to detect the gradual divergence in health status between two societies whose fate is closely interconnected and to specify which features of institutions and policies may have the greatest returns to population health. The lesson is of public provision and redistribution trumping traditional economic growth and direct health spending in producing population health. Even when a long view is taken on wealth, spending on healthcare and actual health, associations are non-existent. Canadian health status increasingly surpassed that of the United States in a period in which US economic growth moved increasingly ahead of Canadian growth and US unemployment rates – for the first time since the Second World War – were consistently lower. Moreover, spending on healthcare in the United States increasingly surpassed that in Canada (and everywhere else in the world) during a time in which Canada had a national medicare scheme and the United States did not.
The approach we have taken focuses naturally on the introduction and evolution of institutional differences. In the context of thinking about population health, the historical, dynamic approach casts a clearer light on what has been going on than does the cross-sectional approach. The latter has been dominant in the literature so far, and has led to a number of ambiguities and unresolved controversies, such as, for example, the ongoing debate over absolute versus relative incomes.
Early cross-national research showed a consistent association between income inequality and health status (Wilkinson 1990, 1992). Soon, however, the results of these studies were contested, with charges of poor-quality data and lack of control for potential confounders such as transfer payments and social spending (Judge 1995). The characterization of transfers and social spending as “confounders” illustrates a core problem with an approach that reduces broad, long-term questions of society and health to isolated, current-time variables like income inequality. Instead, the perspective taken here would construe transfer payments and social spending as part of a gradually unfolding institutional landscape. Through a variety of mechanisms, this changing landscape, in turn, has the capacity to transform inequality, health and the relationship between the two.
The Canada–United States case study demonstrates what Roy Amara, former head of the Institute for the Future in California, once formulated as Amara's Law: people typically overestimate the short-run impact of innovations and underestimate their long-run impacts. Institutional and policy changes might take place with the stroke of a pen, but their impacts may unfold gradually over decades to influence population health. Moreover, a series of decisions taken over time may gradually unfold as an institutional/policy regime that would be unrecognizable from those of the past. At the same time, population health trends can change slowly over years and decades, resulting in large differences between societies that no one would have watched for or anticipated. Trends in human health, especially when based upon unambiguous endpoints like mortality, are brutally objective as measures of long-term societal success or failure. Those interested in health policy should be closely watching these big, slow-moving trends.
References
- Estevez-Abe M., Iversen T., Soskice D. Social Protection and the Formation of Skills: A Reinterpretation of the Welfare State. In: Hall P.A., Soskice D., editors. Varieties of Capitalism: The Institutional Foundations of Comparative Advantage. New York: Oxford University Press; 2001. [Google Scholar]
- Hertzman C. Health and Human Society. American Scientist. 2001;89:538–45. [Google Scholar]
- Judge K. Income Distribution and Life Expectancy: A Critical Appraisal. British Medical Journal. 1995;311:1282–85. doi: 10.1136/bmj.311.7015.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeown T. The Role of Medicine: Dream, Mirage or Nemesis? 2nd ed. Oxford, UK: Basil Blackwell; 1979. [Google Scholar]
- Siddiqi A., Hertzman C. Towards an Epidemiological Understanding of the Effects of Long-term Institutional Changes on Population Health: A Case Study of Canada versus the USA. Social Science & Medicine. 2007;64:589–603. doi: 10.1016/j.socscimed.2006.09.034. [DOI] [PubMed] [Google Scholar]
- Singh G.H., Siahpush M. Increasing Inequalities in All-Cause and Cardiovascular Mortality among US Adults Aged 25–64 Years by Area Socioeconomic Status, 1969–1998. International Journal of Epidemiology. 2002;31(3):600–13. doi: 10.1093/ije/31.3.600. [DOI] [PubMed] [Google Scholar]
- Wilkins R., Berthelot J.M., Ng E. Health Reports. Ottawa: Statistics Canada; 2002. Trends in Mortality by Neighbourhood Income in Urban Canada from 1971 to 1996. p. S13. Catalogue no. 82-003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R.G. Income Distribution and Mortality: A ‘Natural’ Experiment. Sociology of Health and Illness. 1990;12:391–412. [Google Scholar]
- Wilkinson R.G. Income Distribution and Life Expectancy. British Medical Journal. 1992;304:165–68. doi: 10.1136/bmj.304.6820.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuberi D. Transfers Matter Most. 2001. Luxembourg Income Study Working Paper #271.
- Zuberi D. Differences that Matter: Social Policy and the Working Poor in the United States and Canada. Ithaca, NY: Cornell University Press; 2006. [Google Scholar]