The case
You have a 76-year-old patient with heart failure that was diagnosed 2 months ago. She has a history of hypertension, which is being treated with amlodipine. On her initial visit 2 months previously, you prescribed furosemide 40 mg once daily. She responded favourably with a decrease in some symptoms. The patient has returned for follow-up. She denies chest pain but continues to experience mild dyspnea on climbing more than 1 flight of stairs. Her blood pressure is 130/80 mm Hg, her heart rate is 79 beats/min and regular, and her jugular venous pressure is 5 cm above the sternal angle. She has a fourth heart sound, mild rales at the base of both lungs and mild edema in both ankles. Her hemoglobin, glucose and creatinine levels are normal. An electrocardiogram shows sinus rhythm with left ventricular hypertrophy; a cardiac perfusion scan is normal. A 2-dimensional echocardiogram shows a normal left ventricular ejection fraction, a thickened left ventricle and impaired left ventricular relaxation. How would you proceed with management of this patient?
Heart failure is defined by the Canadian Cardiovascular Society as “a complex syndrome in which abnormal heart function results in, or increases the subsequent risk of, clinical symptoms and signs of low cardiac output and/or pulmonary or systemic congestion.”1 Traditionally, heart failure has been associated with systolic pump dysfunction — that is, the failure of the left ventricle to eject blood into the aorta.2 Recently though, diastolic dysfunction has been recognized increasingly as a cause of much of the burden of heart failure.3 Diastolic dysfunction has been described as inadequate filling of the left ventricle during diastole owing to impaired left ventricular relaxation.2,4 When heart failure ensues in this setting and the ejection fraction remains normal or near normal, it is termed diastolic heart failure.5,6
Both the term “diastolic heart failure” and the method used to diagnose the condition are subject to ambiguity and debate in the literature.5,7 Often, the phrase “heart failure with preserved systolic function” is used interchangeably with “diastolic heart failure.”1 This reflects a presumption that patients with heart failure and preserved ejection fraction have diastolic dysfunction even in the absence of evidence from an objective assessment of left ventricular function.8 The question of whether diastolic abnormalities must be proven before making a diagnosis of diastolic heart failure is debatable. What the best modality of cardiac imaging is to accomplish this is also debatable.5 Diseases related to pericardial or valvular defects and systemic conditions (e.g., renal failure and anemia) that can lead to heart failure in the presence of a normal ejection fraction can also fall under the umbrella of “heart failure with preserved systolic function.”6 Finally, the definitions of both “diastolic heart failure” and “heart failure with preserved ejection fraction” require a normal or near normal ejection fraction.2,4 Near normal, however, can include ejection fractions ranging from 35% to 55% depending on the source.2,8
Various groups have proposed criteria for the diagnosis of diastolic heart failure.5,9–11 All acknowledge that the condition cannot be distinguished from systolic heart failure on the basis of symptoms, physical examination, chest radiography or electrocardiography.3 They also all agree that signs and symptoms compatible with heart failure must be present and that a normal ejection fraction must be demonstrated.
Practical recommendations for diagnosis have been made by both the Canadian Cardiovascular Society1 and the American College of Cardiology in a joint effort with the American Heart Association.9 According to these groups, a diagnosis of diastolic heart failure should be considered when there are signs and symptoms of heart failure (e.g., fatigue, pulmonary congestion and dependent edema) and when there is objective evidence of a normal or near normal ejection fraction, either with or without demonstrated diastolic abnormalities, and without valvular defects.1,9 Patients should also be free of pericardial disease or a systemic condition (e.g., anemia or renal failure) that could explain their heart failure. This is the definition of diastolic heart failure that we have adopted for our review.
The challenge of defining the epidemiology of diastolic heart failure
Not only do the definition and diagnostic criteria of diastolic heart failure vary in the literature, but large, prospective epidemiologic studies have not differentiated between systolic and diastolic heart failure.12 Identifying high-quality, uniform studies of diastolic heart failure on which to base precise conclusions regarding prevalence, risk factors and prognosis is therefore difficult.8 To deal with this deficiency, reviews of primary studies most often report mean estimates with wide ranges and include a call for further studies.13
How common is diastolic heart failure?
The increasing size of the elderly population in North America is causing the number of people affected by the disease to increase dramatically. This increase has given rise to a perception that heart failure is a growing epidemic despite its stable incidence.13,14 Diastolic heart failure is common and is responsible for a large proportion of society's health care costs.15 A recent review of primary epidemiologic studies of its prevalence across various communities suggests that diastolic heart failure accounts for 54% of all cases of heart failure on average, with a range of 40%–74%.13,16–20 This wide range likely reflects not only the unique characteristics of the communities investigated, but also the lack of a consistent definition of diastolic heart failure and the variability of the cutoff point for what is considered a normal or near normal ejection fraction.21,22
The factors most often found to be associated with the development of diastolic heart failure include increasing age, female sex, hypertension and atrial fibrillation.3,18,23–25 Although there is some discrepancy regarding the risk posed by coronary artery disease, its prevalence among patients with diastolic heart failure is generally lower than it is among patients with systolic heart failure and higher than it is among healthy controls.13 A recent investigation of 2802 admissions because of heart failure to 103 Ontario hospitals compared patients with diastolic heart failure (ejection fraction > 50%) and systolic heart failure (ejection fraction < 40%).3 The study found significant differences between the 2 groups. Patients with diastolic heart failure were older (75 years v. 72 years), more often female (66% v. 37%) and more likely to have a history of hypertension (55% v. 49%) and atrial fibrillation (32% v. 24%). However, they were less likely to have coronary artery disease (36% v. 49%) and cardiac risk factors including diabetes, hyperlipidemia and a history of smoking. Another analysis involving 4596 patients in hospital confirmed those findings and identified further significant associations with diastolic heart failure, including higher body mass index and obesity, and lower hemoglobin level on admission as compared with patients who had systolic heart failure.25 Reports of patients in the community with diastolic heart failure have made similar observations.16,23
What is the prognosis of patients with diastolic heart failure?
Whether diastolic heart failure leads to a similar or better outcome than systolic heart failure is still unknown. Earlier data from the 1980s and 1990s suggested that diastolic heart failure carries a better prognosis than systolic heart failure.16 Participants in the Framingham Heart Study, for example, were followed for 6 years: those with diastolic heart failure were found to have an annual mortality of 9%, as compared with 18% among those with systolic heart failure.16 More recent literature, however, suggests that mortality for the 2 conditions may be similar.13,26 In a study involving Ontario residents admitted to hospital, mortality at 1 year was 22% among those with diastolic heart failure and 25% among those with systolic heart failure — a nonsignificant difference.3 Similarly, in the community study of Minnesota residents with heart failure, the 1-year mortality was 29% among those with diastolic heart failure.23 The reason for the difference between older and more recent studies is unclear. It may be due to differences in the diagnostic criteria used and the clinical characteristics of the patients included.26 The morbidity of diastolic heart failure is high, paralleling that of systolic heart failure in terms of required outpatient visits and a 1-year hospital readmission rate that approaches 50%.5,17
Why is it important to differentiate diastolic and systolic heart failure?
Distinguishing diastolic and systolic heart failure in patients is important because the strategies for their management may differ. A vast and sound body of evidence exists to guide clinicians in managing systolic heart failure. However, treatment of diastolic heart failure may not be easily extrapolated from these data and has yet to be firmly accepted.
How should patients with diastolic heart failure be managed?
Because fewer large clinical trials have addressed the management of diastolic heart failure compared with those addressing systolic heart failure, most guidelines on the topic have admittedly made their recommendations in the absence of evidence.1,9 Many reviews have resorted to a physiologic understanding of diastolic dysfunction to draw conclusions.27 The few articles that do review the literature on treatment of diastolic heart failure, although evidence-based, used nonsystematic methodology for study selection or did not consider nonpharmacologic strategies.28,29 With the increasing focus on diastolic heart failure as an important problem, more studies are emerging. We conducted a systematic review of the literature on the effective drug therapies and nonpharmacologic therapies available for diastolic heart failure in the outpatient setting (details of the literature search appear in Box 1). We also propose recommendations for clinicians that are practical and evidence-based.
Pharmacologic therapy
Angiotensin-converting-enzyme (ACE) inhibitors
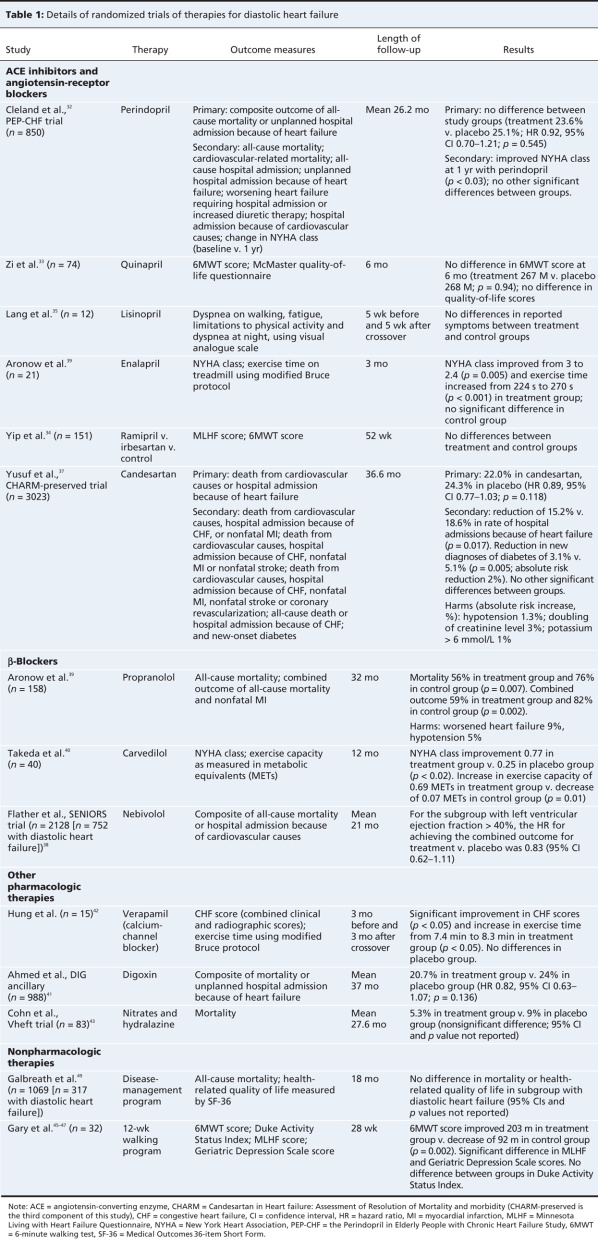
We found 5 randomized controlled trials examining the role of ACE inhibitors in diastolic heart failure ((Table 1)Appendices 2 and 3, available online at www.cmaj.ca/cgi/content/full/180/5/520/DC1). Of these, the trial that was largest and of the highest quality studied perindopril use for chronic heart failure in 850 elderly people. It found no difference in the composite outcome of all-cause mortality or unplanned hospital admission because of heart failure between the treatment and placebo groups after 2.1 years.32 Notably, a high percentage of participants either stopped the study treatment (40% in the perindopril group and 36% in the placebo group) or used open-label ACE inhibitors (35% in the perindopril group and 37% in the placebo group), which reduced the likelihood that a detectable difference would be found.
Table 1
Three smaller randomized trials (n = 151, 74 and 12) that examined the effects of ramipril, quinapril or lisinopril on diastolic heart failure showed no significant difference between treatment groups and control groups in exercise capacity, quality of life or symptoms.33–35
One small study involving 21 elderly patients with diastolic heart failure and prior myocardial infarction compared enalapril plus furosemide with furosemide alone for 3 months. Patients given enalapril had an improved exercise time of 46 seconds on average on the modified Bruce protocol test (p < 0.001); and their New York Heart Association functional classifications improved from 3 to 2.4 on average (p = 0.005).36
Angiotensin-receptor blockers
We found 2 randomized trials evaluating angiotensin-receptor blockers. The higher quality of the 2 was also the largest of the 14 studies we included in our review. The CHARM-Preserved Trial, the third component trial of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity, enrolled 3023 patients.37 For the primary composite outcome of cardiovascular-related mortality or hospital admissions because of heart failure, there was no difference between the candesartan group and the placebo group (hazard ratio [HR] 0.89, 95% CI 0.77–1.03). As a predefined outcome, the rate of hospital admissions because of heart failure decreased significantly (absolute risk reduction 3.3%; p = 0.017). Notably, however, adverse events requiring permanent discontinuation significantly increased in the candesartan group. The adverse events included hypotension (absolute risk increase 1.3%), an increase in creatinine level (absolute risk increase 2.4%) and hyperkalemia (absolute risk increase 0.9%). A smaller randomized trial (n = 151) comparing the addition of irbesartan to standard therapy with the use of standard therapy alone found no benefit in quality of life, scores on a 6-minute walking test or rate of hospital admission.34
β-Blockers
We found 3 randomized trials evaluating the role of β- blockers in diastolic heart failure. The largest study enrolled patients who were at least 70 years old, had a clinical history of chronic heart failure and had either been admitted to hospital because of heart failure during the 12 months before enrolment or had a documented ejection fraction of 35% or less during the 6 months before enrolment.38 In the subgroup of patients with an ejection fraction of greater than 40%, there was no difference at 21 months in the nonprespecified outcome of combined all-cause mortality and hospital admission because of cardiovascular causes between those given nebivolol and those given placebo.
Two other studies of lesser quality and smaller size (n = 158, n = 40) did find significant improvements in clinically important outcomes with β-blockers compared with standard therapy.39,40 The first study showed an absolute risk reduction of 20% in mortality with propranolol over a mean follow-up of 32 months. The second showed significant improvements in New York Heart Association functional classifications over 12 months of follow-up in the carvedilol group, from 2.37 to 1.56 on average, compared with a nonsignificant improvement, from 2.29 to 2.11 on average, in the group receiving standard therapy.
Other drugs
We found 1 randomized trial evaluating digoxin, the Digitalis Investigation Group ancillary trial.41 This high-quality study enrolled 988 ambulatory patients with chronic heart failure, an ejection fraction greater than 45% and normal sinus rhythm at baseline. The study found no added benefit with digoxin compared with placebo. The combined primary outcomes of hospital admission or death because of heart failure were experienced by 21% in the digoxin group and 24% in the placebo arm (HR 0.82, 95% CI 0.63–1.07).
We found a single trial of calcium-channel blockers that compared verapamil with placebo in 15 patients. At 3 months, verapamil was associated with a significant improvement in a nonstandard symptom score and a significant improvement of 54 seconds in exercise time using the modified Bruce protocol.42
We found a single trial of nitrates plus hydralazine compared with placebo in 83 patients. The study treatment was associated with a nonsignificant relative risk reduction of 41% in all-cause mortality.43 This trial was of lower quality and included only men with evidence of cardiac enlargement.
Overall, we found 4 large, high-quality studies of pharmacotherapy, but none showed any benefit in mortality or cardiovascular-related death.32,37,38,44 In terms of symptom management, angiotensin-receptor blockers have been tested the most rigorously in the largest of all of the trials we identified (CHARM-Preserved trial).37 These agents appeared to reduce the rate of hospital admissions because of heart failure. This finding was balanced, however, by an increase in adverse events such as hypotension, worsening renal function and hyperkalemia. As suggested by the Digitalis Investigation Group ancillary trial, digoxin is unlikely to be effective in managing patients with diastolic heart failure.41 The evidence for or against β-blockers, calcium-channel blockers and nitrates plus hydralazine is simply lacking, because existing trials are few and poor in quality. Similarly, the value of ACE inhibitors has yet to be investigated adequately. Although the large trial of perindopril for chronic heart failure in elderly people showed a lack of benefit, the high use of open-label ACE inhibitors may have minimized any difference in outcome between the treatment and placebo groups and diluted measurement of the drug's true value.32
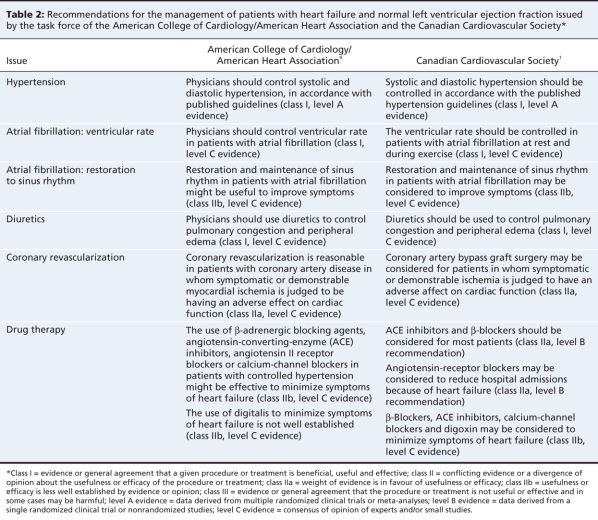
Given the lack of therapies shown to be effective in randomized trials, where should the clinician managing patients with diastolic heart failure seek advice? Clinical practice guidelines that incorporate expert opinion are likely to provide the most helpful suggestions. The Canadian Cardiovascular Society and the joint task force of the American College of Cardiology and American Heart Association make similar recommendations (Table 2).1,9 They stress the importance of treating causes of diastolic dysfunction such as hypertension and ischemia, managing comorbidities such as atrial fibrillation, and prescribing furosemide to control pulmonary and peripheral edema. These are all reasonable recommendations based on the current understanding of the pathophysiology of diastolic dysfunction.
Table 2
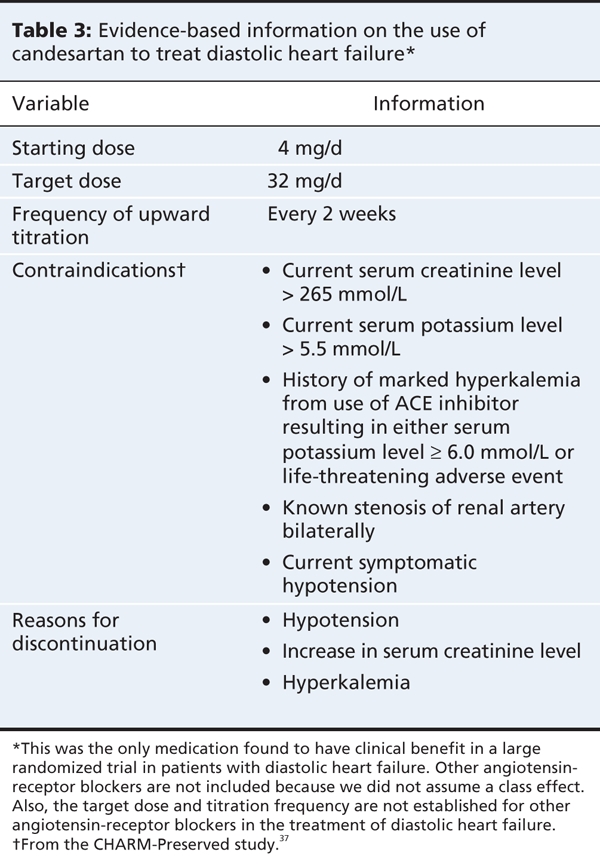
In terms of specific pharmacotherapies, the task force of the American College of Cardiology and American Heart Association suggests that ACE inhibitors, angiotensin-receptor blockers, β-blockers and calcium channel blockers may be effective for the control of symptoms (class IIb, level C recommendation). Based on our review, the use of angiotensin-receptor blockers has the most convincing evidence to support it. Clinicians should probably consider them in patients with no contraindications, while carefully monitoring for hypotension, worsening renal function and hyperkalemia. Table 3 shows the evidence-based drug information, including starting doses and contraindications, for candesartan, the only angiotensin-receptor blocker found to have clinical benefit in a large randomized trial of diastolic heart failure. These guidelines also recommend against using digoxin, which is in keeping with our findings. Any opinions on the use of β-blockers, calcium-channel blockers and ACE inhibitors are asserted in the absence of good trial data. But again, treatment with these agents seems reasonable based on knowledge of the pathophysiology of diastolic heart failure.
Table 3
Nonpharmacologic therapy
We found 1 randomized trial, described in 3 articles,45–47 that studied the effects of a 12-week exercise program in 32 older women (mean age 68 years) with diastolic heart failure. The trial found that exercise was associated with an average improvement of 295 feet in the 6-minute walk test (range 135–455 feet).
We found 1 randomized trial, described in 2 articles,48,49 of a disease-management program for patients with diastolic and systolic heart failure. The intervention consisted of a proprietary disease-management protocol in which disease managers contacted patients (first weekly, then monthly) and made recommendations in accord with the guidelines for heart failure of the American College of Cardiology and American Heart Association.9 Patient education was also provided. The trial found that the intervention had no effect on mortality or quality of life in the predefined subgroup of 317 patients with diastolic dysfunction.
Overall with respect to nonpharmacologic therapy, we conclude that, based on a single small study, exercise programs may be helpful in reducing symptoms in patients with diastolic heart failure, especially older women.
The case revisited
It is reasonable for the clinician to make sure the patient's hypertension continues to be well controlled, aiming for a blood pressure of less than 140/90 mm Hg. Furosemide should be used to control pulmonary congestion and peripheral edema. A cardiac rehabilitation program that encourages physical activity may improve her exercise tolerance. Patient education is recommended for all patients with heart failure and should be provided.1 The clinician may find the educational modules from the Heart Failure Society of America50 to be useful. Finally, the clinician could consider adding or switching to an angiotensin-receptor blocker to reduce symptoms, while monitoring for possible adverse effects including hypotension, worsening renal function and hyperkalemia (Table 3).
Gaps in knowledge
Our systematic review of the most recent literature has confirmed that there is still a paucity of effective therapies for diastolic heart failure. As well, many of the studies included both patients with systolic heart failure and patients with diastolic heart failure. Moreover, there is still disagreement over the definition of diastolic heart failure.
Our review has several limitations. First, because the definition and diagnostic criteria of diastolic heart failure are still debated, the condition may be labelled differently by various study authors. Our search strategy could have thus failed to identify applicable trials. To safeguard against this possibility, we also scrutinized the reference lists of review articles for high-quality randomized controlled trials or meta-analyses that may not have been included in our search results. Second, the inclusion criteria used by the trials we found were heterogeneous. Different cut-off values, ranging from 40% to 50%, were used to define left ventricular ejection fraction. In 5 of the 14 studies, patients without diastolic dysfunction documented by echocardiography were excluded. Two trials evaluating ACE inhibitors and β-blockers included only patients with a history of myocardial infarction, which raises concern that these medications may have benefited patients for reasons other than treatment of their diastolic heart failure. Despite the heterogeneity of the studies, we are reassured by the fact that their results were predominately homogeneous in finding limited effectiveness in existing therapies.
Clinical implications
Clinicians who have patients with diastolic heart failure should understand that treatment of the disease cannot be based solely on evidence from randomized trials. Despite large trials of angiotensin-receptor blockers, ACE inhibitors, β-blockers and digoxin, none has shown a reduction in mortality. It would therefore be reasonable for clinicians to treat diastolic heart failure with angiotensin-receptor blockers, based on evidence showing a reduction in the rate of hospital admissions because of heart failure as a secondary outcome. Clinicians should be mindful, however, of the potential for hypotension, increased creatinine levels and hyperkalemia when using angiotensin-receptor blockers.
Key points.
Diastolic heart failure is increasingly recognized as an important clinical syndrome, but the criteria for diagnosis are subject to debate.
Large, high-quality randomized trials of angiotensin-converting-enzyme inhibitors, β-blockers, angiotensin-receptor blockers and digoxin do not show any improvement in survival rates.
Use of angiotensin-receptor blockers reduces the rate of hospital admissions due to heart failure but is associated with an increased risk of hypotension, renal failure and hyperkalemia.
In the absence of evidence-based interventions for diastolic heart failure, clinicians should focus on treating comorbidities, such as hypertension, atrial fibrillation and coronary artery disease.
Supplementary Material
Acknowledgments
We acknowledge the help of our librarian, Jessie McGowan, for advising us on our search strategy and for executing the search.
Footnotes
This article has been peer reviewed.
Contributors: Katina Tzanetos, Derek Leong and Robert Wu conceived the study. All of the authors participated in the systematic review of the literature. Derek Leong and Robert Wu abstracted and summarized the results. Katina Tzanetos drafted the article. All of the authors revised it critically for important intellectual content and approved the final version submitted for publication.
Competing interests: None declared.
Correspondence to: Dr. Robert Wu, Toronto General Hospital, Rm. 14EN-222, 200 Elizabeth St., Toronto ON M5G 2C4; robert.wu@uhn.on.ca
REFERENCES
- 1.Arnold JM, Liu P, Demers C, et al. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol 2006;22:23-45. [DOI] [PMC free article] [PubMed]
- 2.Gaasch WH, Zile MR. Left ventricular diastolic dysfunction and diastolic heart failure. Annu Rev Med 2004;55:373-94. [DOI] [PubMed]
- 3.Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 2006;355:260-9. [DOI] [PubMed]
- 4.Zile MR, Baicu CF, Bonnema DD. Diastolic heart failure: definitions and terminology. Prog Cardiovasc Dis 2005;47:307-13. [DOI] [PubMed]
- 5.Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure. Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 2002;105:1387-93. [DOI] [PubMed]
- 6.Wu EB, Yu CM. Management of diastolic heart failure — a practical review of pathophysiology and treatment trial data. Int J Clin Pract 2005;59:1239-46. [DOI] [PubMed]
- 7.Banerjee P, Banerjee T, Khand A, et al. Diastolic heart failure: Neglected or misdiagnosed? J Am Coll Cardiol 2002;39:138-41. [DOI] [PubMed]
- 8.Thomas MD, Fox KF, Coats AJ, et al. The epidemiological enigma of heart failure with preserved systolic function. Eur J Heart Fail 2004;6:125-36. [DOI] [PubMed]
- 9.Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 2005;112:e154-235. [DOI] [PubMed]
- 10.How to diagnose diastolic heart failure. European Study Group on Diastolic Heart Failure. Eur Heart J 1998;19:990-1003. [DOI] [PubMed]
- 11.Vasan RS, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation 2000;101:2118-21. [DOI] [PubMed]
- 12.Ho KK, Pinsky JL, Kannel WB, et al. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 1993;22(Suppl A):6A-13A. [DOI] [PubMed]
- 13.Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis 2005;47:320-32. [DOI] [PubMed]
- 14.Braunwald E. Shattuck lecture — cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med 1997;337:1360-9. [DOI] [PubMed]
- 15.Liao L, Jollis JG, Anstrom KJ, et al. Costs for heart failure with normal vs reduced ejection fraction. Arch Intern Med 2006;166:112-8. [DOI] [PubMed]
- 16.Vasan RS, Larson MG, Benjamin EJ, et al. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 1999;33:1948-55. [DOI] [PubMed]
- 17.Redfield MM, Jacobsen SJ, Burnett JC Jr, et al. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003;289:194-202. [DOI] [PubMed]
- 18.Kitzman DW, Gardin JM, Gottdiener JS, et al.; Cardiovascular Health Study Research Group. Importance of heart failure with preserved systolic function in patients > or = 65 years of age. Cardiovascular Health Study. Am J Cardiol 2001;87:413-9. [DOI] [PubMed]
- 19.Devereux RB, Roman MJ, Liu JE, et al. Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the Strong Heart Study. Am J Cardiol 2000;86:1090-6. [DOI] [PubMed]
- 20.Kupari M, Lindroos M, Iivanainen AM, et al. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med 1997;241:387-94. [DOI] [PubMed]
- 21.Sanderson JE. Heart failure with a normal ejection fraction. Heart 2007;93:155-8. [DOI] [PMC free article] [PubMed]
- 22.Shammas RL, Khan NU, Nekkanti R, et al. Diastolic heart failure and left ventricular diastolic dysfunction: What we know, and what we don't know! Int J Cardiol 2007;115:284-92. [DOI] [PubMed]
- 23.Chen HH, Lainchbury JG, Senni M, et al. Diastolic heart failure in the community: clinical profile, natural history, therapy, and impact of proposed diagnostic criteria. J Card Fail 2002;8:279-87. [DOI] [PubMed]
- 24.Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol 1995;26:1565-74. [DOI] [PubMed]
- 25.Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006;355:251-9. [DOI] [PubMed]
- 26.Senni M, Redfield MM. Heart failure with preserved systolic function. A different natural history? [review]. J Am Coll Cardiol 2001;38:1277-82. [DOI] [PubMed]
- 27.Little WC, Brucks S. Therapy for diastolic heart failure. Prog Cardiovasc Dis 2005;47:380-8. [DOI] [PubMed]
- 28.Hogg K, McMurray J. The treatment of heart failure with preserved ejection fraction (“diastolic heart failure”). Heart Fail Rev 2006;11:141-6. [DOI] [PubMed]
- 29.Massie BM, Fabi MR. Clinical trials in diastolic heart failure. Prog Cardiovasc Dis 2005;47:389-95. [DOI] [PubMed]
- 30.Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the Survival and Ventricular Enlargement trial. The SAVE Investigators. N Engl J Med 1992;327:669-77. [DOI] [PubMed]
- 31.Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet 2001;357:1385-90. [DOI] [PubMed]
- 32.Cleland JG, Tendera M, Adamus J, et al. PEP-CHF I. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J 2006;27:2338-45. [DOI] [PubMed]
- 33.Zi M, Carmichael N, Lye M. The effect of quinapril on functional status of elderly patients with diastolic heart failure. Cardiovasc Drugs Ther 2003;17:133-9. [DOI] [PubMed]
- 34.Yip GW, Wang M, Wang T, et al. The Hong Kong diastolic heart failure study: a randomised controlled trial of diuretics, irbesartan and ramipril on quality of life, exercise capacity, left ventricular global and regional function in heart failure with a normal ejection fraction. Heart 2008;94:573-80. [DOI] [PubMed]
- 35.Lang CC, McAlpine HM, Kennedy N, et al. Effects of lisinopril on congestive heart failure in normotensive patients with diastolic dysfunction but intact systolic function. Eur J Clin Pharmacol 1995;49:15-9. [DOI] [PubMed]
- 36.Aronow WS, Kronzon I. Effect of enalapril on congestive heart failure treated with diuretics in elderly patients with prior myocardial infarction and normal left ventricular ejection fraction. Am J Cardiol 1993;71:602-4. [DOI] [PubMed]
- 37.Yusuf S, Pfeffer MA, Swedberg K, et al. CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 2003;362:777-81. [DOI] [PubMed]
- 38.Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J 2005;26:215-25. [DOI] [PubMed]
- 39.Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 1997;80:207-9. [DOI] [PubMed]
- 40.Takeda Y, Fukutomi T, Suzuki S, et al. Effects of carvedilol on plasma B-type natriuretic peptide concentration and symptoms in patients with heart failure and preserved ejection fraction. Am J Cardiol 2004;94:448-53. [DOI] [PubMed]
- 41.Ahmed A, Rich MW, Fleg JL, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation 2006;114:397-403. [DOI] [PMC free article] [PubMed]
- 42.Hung MJ, Cherng WJ, Kuo LT, et al. Effect of verapamil in elderly patients with left ventricular diastolic dysfunction as a cause of congestive heart failure. Int J Clin Pract 2002;56:57-62. [PubMed]
- 43.Cohn JN, Johnson G. Heart failure with normal ejection fraction. The V-HeFT Study. Veterans Administration Cooperative Study Group. Circulation 1990;81(Suppl):III48-53. [PubMed]
- 44.Ahmed A, Rich MW, Love TE, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J 2006;27:178-86. [DOI] [PMC free article] [PubMed]
- 45.Gary R. Exercise self-efficacy in older women with diastolic heart failure: results of a walking program and education intervention. J Gerontol Nurs 2006;32:31-9; quiz 40-1. [DOI] [PubMed]
- 46.Gary RA, Sueta CA, Dougherty M, et al. Home-based exercise improves functional performance and quality of life in women with diastolic heart failure. Heart Lung 2004;33:210-8. [DOI] [PubMed]
- 47.Gary R, Lee SY. Physical function and quality of life in older women with diastolic heart failure: effects of a progressive walking program on sleep patterns. Prog Cardiovasc Nurs 2007;22:72-80. [DOI] [PubMed]
- 48.Smith B, Forkner E, Zaslow B, et al. Disease management produces limited quality-of-life improvements in patients with congestive heart failure: evidence from a randomized trial in community-dwelling patients. Am J Manag Care 2005;11:701-13. [PubMed]
- 49.Galbreath AD. KRS. Long-term healthcare and cost outcomes of disease management in a large, randomized, community-based population with heart failure. Circulation 2004;110:3518-26. [DOI] [PubMed]
- 50.Heart Failure Society of America. Educational modules on heart failure. Saint Paul (MN): The Society. Available: www.hfsa.org/hf_modules.asp (accessed 2009 Feb. 2).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.