Abstract
Objective To compare anxiety symptoms and disorders in children and adolescents with recurrent abdominal pain (RAP), anxiety disorders, and healthy control children. Methods Twenty-one children with RAP (nine males, mean age = 11.05) were compared to 21 children with anxiety disorders (11 males, mean age = 12.29), and 21 children without pain or anxiety (nine males, mean age = 11.57) using diagnostic interviews and continuous measures of anxiety and other internalizing symptoms. Results Sixty-seven percent of children with RAP met criteria for an anxiety disorder. Children with RAP were higher than well children but not significantly different from children with anxiety on total internalizing and anxiety symptoms. Conclusions RAP and anxiety are closely related. Further understanding between these disorders is essential to understanding the development and progression of RAP, and to inform the prevention and treatment of the disorder.
Keywords: adolescents, anxiety, children, recurrent pain
Recurrent abdominal pain (RAP) is the most common recurrent pain complaint of childhood (McGrath, 1990). The pain must occur at least once a month for at least 3 months, in order to meet traditional criteria (Apley, 1975); however, many researchers note that Apley's (1975) criteria are too general and include too many subtypes of abdominal pain, including those with an organic cause, to be a useful classification (Rasquin-Weber et al., 1999). For the purposes of this article, we will continue to use the term “RAP” to denote abdominal pain that is without organic cause (i.e., functional), is usually periumbilical and does not relate to any specific physical activity. Epidemiological studies suggest that RAP affects 8–25% of school-age children ages 9- to 12-years old (Apley, 1975; Devanarayana, de Silva, & de Silva, 2008; Huguet & Miro, 2007; Konijnenberg, de Graeff-Meeder, van der Hoeven, Klimpen, Buitelaar, & Uiterwaal, 2006), and is more prevalent among girls (Apley, 1975; Colletti, 1998). RAP accounts for 2–4% of pediatric office visits (Starfield, Katz, & Gabriel, 1984), and many children with RAP go through potentially risky and possibly unnecessary hospitalizations, tests and procedures, thus placing a heavy burden on the medical community (Walker, Garber, Van Slyke, & Greene, 1995). Medical evaluations reveal organic disease in fewer than 5% of children evaluated in primary care settings (Stickler & Murphy, 1979). Nonetheless, nearly one-third to one-half of children with RAP continue to complain of abdominal pain and related symptoms after they reach adulthood (Walker et al., 1995).
RAP is defined as “functional” because, in most cases, no organic cause can be found to explain the child's pain. RAP is therefore best conceptualized using a biopsychosocial approach that examines factors other than disease as potential mechanisms through which the condition emerged or is exacerbated (Gatchel, Peng, Peters, Fuchs, & Turk, 2007). One psychological variable that may contribute significantly to RAP in children is anxiety.
A recent meta-analysis shows that internalizing symptoms, as measured by parent- and self-report, are approximately six times more likely to occur in children with RAP than matched healthy controls (Dufton & Compas, 2007). Campo et al. (2004) conducted an empirical study that showed parent reports of psychological symptoms as measured by the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2002) were significantly higher for children with RAP than for a matched healthy control. In addition, four studies completed structured diagnostic interviews with this population and found the prevalence of anxiety disorders in children with RAP to be between 42% and 85% (Campo et al., 2004; Dorn et al., 2003; Garber, Zeman & Walker, 1993; Liakopoulou-Kairis et al., 2002).
The association between recurrent pain and anxiety in children is important for several reasons. First, there is evidence of an association between physical and psychological problems in children and adolescents. Egger, Costello, Erkanli, and Angold (1999) found that stomachaches, headaches, and musculoskeletal pains were strongly associated with anxiety, depression, and behavioral disorders in children age 9- to 16-years old. Second, physical symptoms are often part of the criteria for a psychological disorder. For example, “repeated complaints of physical symptoms (such as headaches, stomachaches, nausea, or vomiting) when separation from major attachment figures occurs or is anticipated” is part of the definition of separation anxiety disorder as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV, American Psychiatric Association, 1994). Third, pain symptoms may exacerbate or contribute to psychological symptoms, and vice versa. For example, a child with recurrent nausea induced by her stomachaches may become anxious in situations in which she may be far from a restroom, and as a result she may refuse to leave home to attend school or other social functions. Her avoidance of social situations may, in turn, increase her anxiety when she anticipates or is forced to engage in activities outside the home, which may also then exacerbate her gastrointestinal symptoms.
Temperament and responses to stress may also play an important role in the development and maintenance of the illness, as well as account for the possible link between RAP and anxiety. For example, a behaviorally inhibited temperament in infancy is predictive of anxiety disorders in childhood (Biederman et al., 1993; Hirshfeld et al., 1992), and children with RAP have been found to display many temperamental features found in behaviorally inhibited children (Campo et al., 2004). Further, differences in temperament have been associated with differences in biobehavioral reactivity to stress (Boyce, Barr, & Zeltzer, 1992). For example, behavioral inhibition has been associated with a number of psychophysiological correlates, such as a high and stable resting heart rate (Kagan, Reznick, & Snidman, 1988). Because of the strong association between behavioral inhibition and anxiety disorders, many of these psychophysiological responses to stress are also found in anxious children, adolescents, and adults (Grillon, Ameli, Merikangas, Woods, & Davis, 1993; Thayer, Friedman, & Borkovec, 1996). It is possible that children with RAP may also display these same psychophysiological correlates that may contribute to their abdominal pain.
Finally, the association between RAP and anxiety disorders and symptoms needs to be examined while controlling for somatic symptoms and features of anxiety that may artificially inflate this association. If recurrent bouts of abdominal pain are one of the criteria for an anxiety disorder, the apparent association between RAP and anxiety may be a result of this overlap in symptoms.
To date, only one study has specifically compared children with RAP and children with an anxiety disorder. Dorn et al. (2003) compared children meeting criteria for RAP (n = 14) with children meeting criteria for an anxiety disorder (n = 14) and matched healthy controls (n = 14) using a structured diagnostic interview as well as several questionnaires. Dorn et al. found that 64% of the children with RAP met criteria for an anxiety disorder and that the RAP and anxious participants had comparable scores on psychological measures. This study builds upon Dorn et al.'s results by assessing the level of anxiety symptoms and diagnoses in a population of children with RAP, children with anxiety and a healthy comparison group. This current builds upon Dorn et al.'s results by including a larger sample size (and increased statistical power), obtaining parents’ and adolescents’ reports of internalizing symptoms (e.g., somatic complaints, anxiety, and depression), and using different and more specific measures of anxiety symptoms.
We hypothesize that children with RAP will present with significantly more symptoms of anxiety than well children, though less than the children with an anxiety disorder. In addition, we expect the overall levels of somatic complaints to be higher in the RAP group than in both the anxiety and well groups given that this is a population with recurrent functional pain. Finally, structured diagnostic interview data will be examined in order to determine the point-prevalence rate of anxiety disorders in children with RAP. We hypothesize that children with RAP will have significantly more anxiety disorder diagnoses than well children.
Methods
Participants
Participants included 63 children and adolescents (21 children per group; 29 males, 34 females) ages 8- to 16-years old (mean age 11.64 years) and one parent per child. The mean occupational status, based on the Hollingshead Occupational scores that range from 10 to 90 (Hollingshead, 1975) was 43.22 (SE = 10.46), equivalent to that of administrators, lesser professionals, and proprietors of medium-sized businesses. The sample identified as 71% white, 19% African American, 3% Asian, 6% other, and 2% Hispanic, which is representative of the area of Tennessee from which the sample was drawn. Parent participants included 58 mothers and 5 fathers (mean age 40.56). Of the 87 children and parents approached to participate in the study, 13 were ineligible after the phone screen for the following reasons: the child met criteria for attention-deficit hyperactivity disorder (ADHD) (n = 2), the child was too old to participate (n = 1), or the child no longer met criteria for RAP or anxiety (n = 10). Eleven eligible families were no longer interested in participating after completing the phone screen due to time constraints, difficulty finding transportation to the study center, or difficulty finding childcare for siblings.
Children were recruited to represent three groups: children with RAP, children with anxiety, and well children. The groups were matched on gender and age. A phone screen was used to determine eligibility of participants and to determine into which group the child would fall (see below).
Children with RAP were recruited from a tertiary care gastrointestinal clinic at a major Southern academic medical center. Participants were considered eligible for the “RAP group,” if they were diagnosed with functional abdominal pain by a medical doctor and if their pain qualified them to fall into any one of the following ROME-II categories: functional dyspepsia, irritable bowel syndrome, functional abdominal pain, abdominal migraine, or aerophagia (Rasquin-Weber et al., 1999). Further, the abdominal pain must also have occurred at least three times in the past 3 months and was severe enough to impair functioning or interrupt activities, thus also meeting Apley's (1975) criteria. In our sample, the abdominal pain diagnoses included irritable bowel syndrome (n = 5), functional dyspepsia (n = 1), and functional abdominal pain (n = 18). All of the children in the RAP group (100%) were experiencing abdominal pain with functional disability at least one time per week.
Children with anxiety disorders (“Anxiety group”) were recruited through an outpatient community mental health center and through e-mail advertisements and flyers both in the university medical center and sent to the larger community surrounding the study site. “Anxiety group” participants were considered eligible if they were currently in or had received past mental health treatment for an anxiety disorder and if they continued to meet criteria for an anxiety disorder.
Finally, healthy control children (“well group”) were recruited through e-mail advertisements and flyers distributed throughout the community. All well participants were screened for possible anxiety and abdominal pain symptoms over the phone. If the child had received treatment for anxiety or had seen physician for recurrent abdominal pain, they child was considered ineligible for the well group and was rescreened for the RAP or anxiety groups. None of well group participants originally screened for the study switched groups after screening.
For all three groups, exclusionary criteria included a known chronic health condition, physical handicap, mental retardation, and ADHD. ADHD was an exclusionary criterion due to other parts of the study protocol that involved a computer-based attention task part of a larger study.
Power calculations were used in order to determine whether we had a sufficient number of participants per group to detect a significant effect in this sample. Power calculations were based on effect sizes from the only published study that has compared children with RAP, children with anxiety, and well children (Dorn et al., 2003). Effect sizes in the Dorn et al. study ranged from medium to large. Power estimates for the proposed study were therefore based on estimates of medium effects with a power of.85 and an α-coefficient of.05. Based on these anticipated effect sizes, 20 participants will be required for each group (children with RAP, children with anxiety, and healthy controls) to detect differences of this magnitude or larger. As mentioned previously, we included 21 children per group, enough to detect medium to large effects in comparisons between groups.
Procedure
The study site's Internal Review Board approved the study protocol. Upon arrival at the research lab, parents and children were presented with the study protocol and asked to sign consent and assent forms. A diagnostic interview (see below) was administered to the parent about their participating child. Parents were also administered a brief semi-structured interview about their child's abdominal pain symptoms and use of psychological services and were asked about their child's past and current psychological treatment for anxiety (see below). Both parent and child participants completed questionnaire data on the day of the laboratory visit. Child participants were administered the child version of the diagnostic interview by telephone within one week following their study appointment. Previous research conducting diagnostic interviews face-to-face and over the phone has shown little difference between the two methods in diagnosing anxiety disorders (Rohde, Lewinsohn & Seeley, 1997).
Measures
Anxiety and Depression Symptoms and Somatic Problems
The CBCL and Youth Self Report (YSR; Achenbach & Rescorla, 2002) were used to assess parent reports and self-reports of the participants’ levels of symptoms of anxiety and depression and somatic complaints. The CBCL is a 120-item checklist of problem behaviors and competencies that parents rate as not true (0), somewhat or sometimes true (1), or very true or often true (2) of their child in the past 6 months. The CBCL assesses internalizing (anxiety/depression, somatic complaints), and externalizing (aggression, delinquency) emotional and behavioral problems, as well as social and academic competence. Data are reported as normalized T-scores based on separate norms for age and sex. Raw scores were used in the analyses to allow for maximum variance. Reliability and validity of the CBCL and YSR are well-established. Only children aged 11 and above were administered the YSR (Achembach & Rescorla, 2002), which resulted in a reduced sample size for analyses. Of the 21 children per group, 12 children with RAP, 15 children with anxiety, and 10 healthy control children completed the YSR.
An additional specific measure of anxiety (Multidimensional Anxiety Scale for Children, MASC; March & Albano, 1996) was administered to participating parents and children. The MASC consists of 39 items distributed across four scales (Physical Symptoms, Harm Avoidance, Social Anxiety, and Separation/Panic) and an Anxiety Disorder Index. Data are reported as normalized T-scores based on separate norms for age and sex; raw scores were used in analyses. Reliability and validity of the MASC are well-established.
Diagnostic Interview
Supplement #1 (Affective Disorders) and Supplement #3 (Anxiety Disorders) of Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children, present and lifetime version (K-SADS-PL) were administered to child participants and their participating parent separately (Kaufman, 1997). The K-SADS-PL is a widely used semi-structured, DSM-based psychiatric diagnostic interview with established psychometric properties (Orvaschel & Puig-Antich, 1987). Because child and mother reports do not always agree (Comer & Kendall, 2004; Safford, Kendall, Flanner-Schroeder, Webb & Sommer, 2005), and because parent and child interviews may provide complementary data (since children may report symptoms of which the parents are unaware, or parents may report symptoms which the child may not wish to admit), we followed the “or” rule, and considered a disorder positive if diagnostic criteria were unequivocally met in either the parent or child interview. This a priori procedure for combining information from direct and indirect interviews has been used in previous studies using the K-SADS interview (Biederman, 2001). All interviewers were trained graduate and undergraduate research assistants who underwent several weeks of training, wherein they were taught structured interview skills, reviewed diagnostic criteria for relevant DSM-IV disorders, observed simulated interviews, and role-played interviews. Once interviews were completed, diagnoses were made by supervision with a Master's or PhD-level psychologist. Based on a randomly selected subsample (28%), inter-rater reliability was excellent with κ of.93 and 98% agreement. Further, should a child or parent have endorsed symptoms of suicidal ideation, a standard protocol was in place in order to determine the individual's risk and refer for psychological services if necessary. None of the participants endorsed symptoms of suicidal ideation or intent to harm oneself. Parent- and child-ratings of symptoms were combined to formulate a final diagnosis where if one or both of the participants positively endorsed the symptom, it counted towards diagnosis. Summary scores were thus used to determine whether the child met criteria for a diagnosis.
Recurrent Abdominal Pain Symptoms and Use of Psychological Services
Each parent was administered a brief semi-structured interview developed for this study regarding their child's current level and past history of abdominal pain symptoms including diagnoses from their medical provider, functional impairment due to abdominal pain, anxiety, and use of psychological services. Responses were used to verify the child's current diagnosis of functional RAP, and in order to detail past and current treatment of mental health issues and overall levels of parent-rated anxiety.
Results
Statistical Analyses
Correlations were conducted between all demographic variables and dependent variables. None of these correlations was significant (e.g., age did not correlate with any diagnoses or symptom counts from the questionnaires). Analysis of variance (ANOVA) with a Bonferonni correction to correct for family-wise error rate was applied to each set of inter-related analyses (adjusted p <.02), in order to determine whether the three groups (RAP, Anxious, and Well) differed on the various subscales of the CBCL, YSR, and parent and child versions of the MASC. If significant, independent t-tests were used to conduct paired comparisons between two groups at a time on each variable. Cohen's d effect size calculations (1988) were performed for all significant between-group differences. Effect sizes <0.2 indicate a negligible effect, those between 0.2 and 0.5 indicate a small effect, those between 0.5 and 0.8 indicate a medium effect, and those >0.8 are considered large effects. Chi-squared analyses were used to compare groups on total number of participants currently qualifying for an anxiety disorder diagnosis.
Recurrent Abdominal Pain Symptoms
All children with RAP reported having had three or more stomachaches in the last 3 months with associated functional impairment (interference with school, activities, and/or eating). Therefore, each child in the RAP group met Apley's (1975) criteria for RAP as well as Rome II criteria for functional abdominal pain (n = 16; 76%) or Irritable Bowel Syndrome (n = 5, 25%). Twenty-nine percent of children with anxiety (n = 6) reported having three or more stomachaches in the past 3 months with subsequent functional impairment. No well children reported stomachaches in the previous 3 months. A cross-tabs chi-squared test was used to determine whether this item was endorsed significantly different by children in the anxiety group compared to children in the RAP and well groups. Children with anxiety endorsed this item significantly less often than children in the RAP group [χ2(1) = 3.82, p <.001] and significantly more often than children in the well group [χ2(1) = 8.57, p <.01].
Anxiety/Internalizing Symptoms
Use of Psychological Services
Thirty-eight percent of children with RAP (n = 8) received in the past or currently received psychological services for anxiety, compared with 100% of children with anxiety (n = 21) and 0% of the well children.
YSR/CBCL Subscale Comparisons
Means and SDs of YSR (n = 37) and CBCL (n = 63) data are presented in Table I. Children with RAP reported significantly more somatic complaints on the YSR than both well children, t(20) = 3.41, p <.005, d = 1.4, and anxious children, t(20) = 3.32, p <.005, d = 1.0.
Table I.
CBCL and YSR Means, SDs
| RAP | Anxious | Well | F-Scores | Cohen's d: RAP vs. Anx | Cohen's d: RAP vs. Well | Cohen's d: Anx vs. Well | |
|---|---|---|---|---|---|---|---|
| YSR | (n = 12) | (n = 15) | (n = 10) | ||||
| Anxious/depressed | 56.8 (6.0)a | 56.8 (6.4)a | 52.4 (2.3)b | F (2, 34) = 2.2, p =.13 | 0 | 1.06 | 1.01 |
| Somatic complaints | 61.8 (5.6)a | 56.0 (6.0)b | 54.6 (4.9)b | F (2, 34) = 7.3, p <.002 | 1.0 | 1.37 | 0.26 |
| Total internalizing | 59.6 (5.4)a | 54.9 (7.6)b | 49.9 (9.6)c | F (2, 34) = 4.2, p <.05* | 0.72 | 1.94 | 0.58 |
| DSM affective problems | 57.0 (5.7)a | 54.5 (5.4)a | 54.1 (5.3)a | NS | 0.45 | 0.53 | 0.07 |
| DSM anxiety problems | 55.3 (6.4)a | 58.0 (7.0)a | 52.9 (4.1)a | NS | 0.40 | 0.46 | 0.92 |
| DSM somatic problems | 61.9 (5.4)a | 56.7 (6.3)b | 55.7 (4.3)b | F (2,34) = 5.21, p <.01 | 0.89 | 1.28 | 0.19 |
| CBCL | (n = 21) | (n = 21) | (n = 21) | ||||
| Anxious/depressed | 56.5 (5.3)a | 63.8 (9.5)b | 53.6 (4.9)c | F (2, 60) = 12.1, p <.001 | 0.98 | 0.57 | 1.42 |
| Somatic complaints | 63.3 (8.5)a | 60.1 (10.2)a | 53.4 (4.2)b | F (2, 60) = 7.5, p <.001 | 0.34 | 1.56 | 0.93 |
| Total internalizing | 59.6 (6.3)a | 61.1 (10.5)a | 48.2 (10.3)b | F (2, 60) = 4.4, p <.05* | 0.18 | 1.37 | 1.24 |
| DSM affective problems | 57.0 (6.1)a | 59.7 (9.1)a | 53.6 (5.1)b | F (2, 60) = 4.5, p <.05* | 0.36 | 0.61 | 0.86 |
| DSM anxiety problems | 56.6 (5.5)a | 62.4 (9.4)b | 53.2 (4.8)c | F (2, 60) = 8.4, p <.001 | 0.78 | 0.66 | 1.30 |
| DSM somatic problems | 63.5 (9.0)a | 60.4 (10.9)a | 53.3 (4.2)b | F (2, 60) = 7.1, p <.002 | 0.31 | 1.55 | 0.94 |
Data are presented as normalized T-scores. Those columns with differing superscripts are significantly different.
*After Bonferonni correction, this difference is no longer considered significant.
Similar results were found on the CBCL; parents of children with RAP rated their child as having significantly more somatic complaints, t(40) = 4.69, p <.001, d = 1.56, and total internalizing symptoms than well children, t(40) = 4.03, p <.001, d = 1.37. Children with RAP and anxious children did not differ on the CBCL somatic complaints and total internalizing symptoms scales. Children with anxiety disorders displayed significantly higher scores on the anxiety/depression subscale of the CBCL when compared to children with RAP, t(40) = 2.95, p <.005, d = 1.01, but not on the total internalizing subscale.
The three groups were also compared on DSM-IV-based subscales of the CBCL and YSR. On the YSR, children with RAP reported significantly more symptoms on DSM Somatic Problems than both well and anxious children t(20) = 2.99, p <.005, d = 1.28; t(20) = 2.73, p <.01, d =.89. Children with RAP did not endorse more symptoms than well children on the DSM Affective and Anxiety Problems subscales.
Children with RAP were rated by their parents significantly higher than well children on Anxiety Problems, t(40) = 2.31, p <.05, d =.66, and Somatic Problems, t(40) = 4.5, p <.001, d = 1.55. Children with anxiety were rated significantly higher than well children on the CBCL DSM Anxiety Problems subscale, t(2,60) = 3.56, p <.001, d = 1.30. However, children with anxiety and children with RAP did not differ on DSM Affective and Somatic Problems subscales of the CBCL, though anxious children were rated significantly higher than well children on these two subscales, t(40) = 2.67, p <.01, d =.86; t(40) = 3.56, p <.001, d =.94, respectively.
MASC Subscale Comparisons
Means and SDs of parent- and child-reports on the MASC are presented in Table II. On the MASC, parents of children with RAP rated their children as significantly higher than well children on the following scales: Somatic/Autonomic, t(40) = 3.18, p <.01, d = 1.0, Separation/Panic Scale, t(40) = 3.49, p <.001, d = 1.15, and Anxiety Disorder Index, t(40) = 2.65, p <.01, d =.83. Children with RAP rated themselves as significantly higher than well children only on the Separation/Panic subscale, t(40) = 3.50, p <.001, d = 1.13. When compared to children with anxiety disorders, children with RAP did not rate themselves differently on any of the self-reported indices. However, parents of anxious children rated their child significantly higher than parents of children with RAP on the Tense/Restless Scale, t(40) = 2.99, p <.01, d =.96. Parents of anxious children rated their child significantly higher than parents of well children on the Humiliation/Rejection, t(40) = 2.98, p <.01, d = 1.0, Performing in Public, t(40) = 3.13, p <.01, d =.79, Social Anxiety, t(40) = 3.57, p <.001, d = 1.1, Separation/Panic subscales, t(40) = 4.85, p <.001, d = 1.64, and Anxiety Disorder Index, t(40) = 4.85, p <.001, d = 1.5.
Table II.
MASC Means, SDs
| RAP | Anxious | Well | F-Scores | Cohen's d: RAP vs. Anx | Cohen's d: RAP vs. Well | Cohen's d: Anx vs. Well | |
|---|---|---|---|---|---|---|---|
| Child report | |||||||
| Physical Symptoms Scale | 49.1(7.2) | 48.1(7.5) | 47.5(8.8) | NS | 0.14 | 0.20 | 0.07 |
| Tense/restless | 49.6(9.2) | 49.2(8.8) | 49.3(8.3) | NS | 0.04 | 0.03 | 0.01 |
| Somatic autonomic | 48.5(6.2) | 47.2(7.2) | 45.8(8.6) | NS | 0.19 | 0.36 | 0.18 |
| Harm Avoidance Scale | 50.1(9.8) | 51.7(9.6) | 51.5(10.5) | NS | −0.16 | −0.14 | 0.02 |
| Perfectionism | 49.4(7.8) | 49.7(7.6) | 48.7(10.9) | NS | −0.04 | 0.07 | 0.11 |
| Anxious coping | 50.7(10.8) | 52.8(10.6) | 53.4(9.5) | NS | −0.20 | −0.27 | 0.06 |
| Social Anxiety Scale | 54.6(12.1) | 50.2(8.4) | 54.5(12.1) | NS | 0.43 | 0.01 | −0.42 |
| Humiliation/rejection | 54.4(14.1) | 49.3(8.8) | 53.6(12.5) | NS | 0.45 | 0.06 | −0.40 |
| Performing in public | 53.6(10.7) | 51.5(8.4) | 54.6(10.6) | NS | 0.22 | −0.09 | 0.32 |
| Separation/Panic Scale | 56.6(8.6)a | 53.8(9.2)a | 47.3(7.8)b | F(2,60) = 5.5, p <.01 | 0.31 | 1.13 | 0.76 |
| Anxiety Disorder Index | 53.0(9.8) | 50.0(8.1) | 49.9(9.6) | NS | 0.34 | 0.32 | 0.01 |
| Parent report | |||||||
| Physical Symptoms Scale | 42.4(5.2)a | 45.0(6.5)b | 40.4(4.4)a | F(2,60) = 2.7, p <.10 | −0.44 | 0.42 | 0.84 |
| Tense/restless | 39.5(4.7)a | 44.8(6.3)b | 41.7(5.8)a | F(2,60) = 4.3, p <.05* | −0.96 | −0.42 | 0.51 |
| Somatic autonomic | 46.8(7.3)a | 46.0(7.7)a | 41.0(4.4)b | F(2,60) = 4.6, p <.05* | 0.11 | 0.99 | 0.83 |
| Harm Avoidance Scale | 49.4(7.1) | 51.2(8.3) | 45.8(10.1) | NS | −0.23 | 0.42 | 0.59 |
| Perfectionism | 53.4(7.7)a | 53.9(9.7)a | 48.0(9.4)b | NS | −0.05 | 0.60 | 0.59 |
| Anxious coping | 46.6(8.1) | 48.8(10.6) | 45.4(9.7) | NS | −0.24 | 0.13 | 0.33 |
| Social Anxiety Scale | 52.5(8.7)a | 59.9(11.3)b | 47.8(11.5)a | F(2,60) = 5.8, p <.01 | −0.74 | 0.49 | 1.06 |
| Humiliation/rejection | 54.7(9.2)a | 61.7(11.6)b | 49.4(12.8)a | F(2,60) = 5.3, p <.01 | −0.67 | 0.48 | 1.01 |
| Performing in public | 49.3(9.4)a | 55.0(13.4)b | 46.2(9.0)a | F(2,60) = 3.2, p <.05* | −0.50 | 0.34 | 0.79 |
| Separation/Panic Scale | 55.9(10.7)a | 59.5(13.5)a | 44.8(8.7)b | F(2,60) = 7.7, p <.001 | −0.30 | 1.14 | 1.32 |
| Anxiety Disorder Index | 46.8(8.4)a | 53.0(8.1)b | 40.1(7.6)c | F(2,60) = 11.5, p <.001 | −0.75 | 0.84 | 1.64 |
Data are presented as normalized T-scores. Those columns with differing superscripts are significantly different.
*After Bonferonni correction, this difference is no longer considered significant
Anxiety Disorders
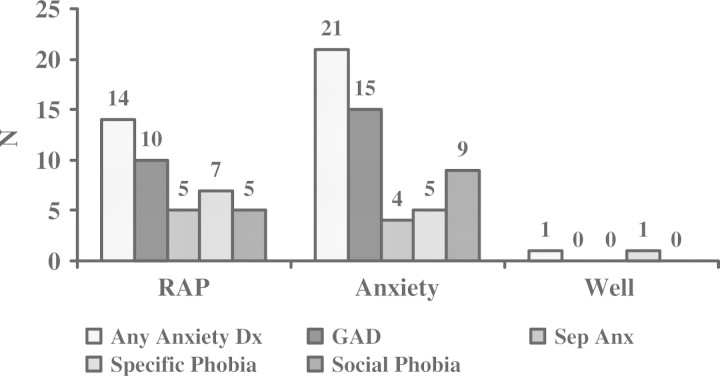
Figure 1 displays the anxiety disorder diagnoses in the RAP, Anxious and Well groups. Sixty-seven percent of children with RAP met criteria for an anxiety disorder, compared to 100% of children with anxiety disorders [χ2(1) = 8.40, p <.01] and 6% of well children [χ2(1) = 14.54, p <.001]. The most prevalent disorders in children with RAP were Generalized Anxiety Disorder (GAD, n = 10, 48%), Specific Phobia (n = 7, 33%), Social Phobia (n = 5, 24%), and Separation Anxiety Disorder (SAD, n = 5, 24%) (Fig. 1). Because GAD and SAD both include stomachaches as part of their criteria, the data were reanalyzed excluding those symptoms from the total number of symptoms qualifying the participant for the diagnosis. The percentage of children with RAP meeting criteria for these two disorders remained the same (48 and 24%, respectively). Further, six children in the RAP group (29%) and five children in the Anxious group (24%) met criteria for more than one anxiety disorder.
Figure 1.
Anxiety disorder diagnoses.
Discussion
This study examined the prevalence of anxiety symptoms and disorders in children with recurrent abdominal pain. Using self- and parent-report questionnaires and diagnostic interviews, children with RAP were compared to a group of children with anxiety disorders and a healthy control group. It was hypothesized that children with RAP would display significantly more anxiety and somatic symptoms and meet criteria for anxiety disorders more often than healthy controls.
Consistent with our hypotheses, questionnaire data showed that parents of children with RAP rated their child as significantly higher than well children on measures of anxiety, affective problems, and somatic symptoms. Also on parent measures, children with RAP were nearly indistinguishable from children with anxiety on measures of anxiety and somatic symptoms. Self-report data showed similar results where children with RAP rated themselves as significantly higher on somatic complaints and higher on symptoms of anxiety and other internalizing symptoms as compared to well children. Again, RAP and anxious children did not differ on self-report questionnaire data.
Previous research examining anxiety and other internalizing symptoms in children with RAP has often reported only overall levels of internalizing symptoms without distinguishing between anxiety, somatic, and depressive symptoms that contribute to total internalizing subscales, such as on the CBCL and YSR (De Los Reyes & Kazdin, 2005). This makes it difficult to determine whether increased levels of internalizing symptoms previously found in children with RAP relate to psychological symptoms or to physical symptoms that are also captured in total internalizing subscales. We found that the increases in internalizing symptoms previously found in children with RAP are not due to somatic symptoms alone, and that anxiety is also a significant psychological feature of this population.
In addition to questionnaire data, this study used semi-structured diagnostic interviews in order to uncover whether children in the sample met criteria for an anxiety disorder. Diagnostic data from this study revealed that children with RAP were significantly more likely to have an anxiety disorder diagnosis than healthy controls. Sixty-seven percent of children with RAP met criteria for an anxiety disorder, with 48% meeting criteria for GAD. Specific Phobia, Social Phobia, and Separation Anxiety Disorder were also prevalent. When somatic symptoms associated with GAD and Separation Anxiety Disorder were controlled for, children with RAP continued to meet criteria for the diagnosis. The National Comorbidity Replication Study places the lifetime prevalence of any anxiety disorder in the general adult population at 18.1% (Kessler, Chiu, Demler, & Walters, 2005). In children, the true prevalence rates of anxiety disorders is less well-established, but have been reported to be at ∼8–10% (Costello et al., 2003; Fergusson, Horwood, & Lynskey, 1993; Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993). Therefore, the lifetime prevalence of anxiety disorders in our sample of children with RAP is substantially higher than would be expected in the general population. Anxiety appears to be a major concern in this population; children with RAP not only have higher than average symptoms of anxiety, but their levels of anxiety are severe enough to qualify for a diagnosis.
Our data reveal a strong relation between RAP and anxiety in children. Of note is that stomachaches with functional impairment also appear to be associated with anxiety disorders. Children with anxiety in our sample endorsed somatic symptoms as frequently as children with RAP. Nearly one-third of the children with anxiety also met Apley's (1975) criteria for RAP. In addition, 14% of children in the anxiety sample with frequent stomachaches had seen a health provider for their gastrointestinal distress.
Interestingly, data from the CBCL and MASC showed that the mean scores from our sample of children with anxiety and children with RAP did not fall into the clinically significant range. Achenbach and colleagues (2001) set the cut-point for the clinically significant range so as to optimize sensitivity and specificity in relation to referral for clinical services in general and not in reference to any particular disorder or disorders. Many children with anxiety disorders are not referred for treatment and therefore the clinical cut-point may yield a higher percentage of “false negatives;” that is, children who do not exceed the cut-off in relation to clinical referral but who meet DSM criteria for an anxiety disorder. This may thus be the case in our study. Further, although these mean scores were lower than expected, the reliability of our diagnoses based on the parent and child administrations of the K-SADS was excellent. Therefore, this pattern of findings suggests that the checklists may, at least in the present samples, under predict diagnoses of anxiety. This may be in part a reflection of the heterogeneity of anxiety symptoms included in the checklists relative to the more homogeneous sets of symptoms that are needed to meet criteria for specific anxiety disorders.
The strong association between RAP and anxiety symptoms and disorders has at least three possible implications. First, RAP and anxiety may be distinct but comorbid disorders. If they are distinct disorders, the present findings suggest that more children with RAP present with comorbid anxiety disorders than children with anxiety meet criteria for RAP; i.e., comorbidity may be unidirectional rather than bidirectional. If they are distinct disorders, future research is needed to determine if there is temporal precedence for either RAP or anxiety disorders. A second possibility is that RAP may be a subtype of an anxiety disorder. Given that most children with RAP in the current sample also met criteria for an anxiety disorder and children with RAP and children with anxiety disorders also presented with comparable levels of anxiety symptoms, it is possible that the presence of persistent and significant abdominal pain is a distinguishing feature of a distinct subtype of anxiety. This is consistent with the current finding that only a subgroup of children who presented with an anxiety disorder also met criteria for RAP. And third, it is important to note the RAP is characterized by a single symptom—abdominal pain. Therefore, RAP may be a salient and significant symptom of broader anxiety syndromes or disorders. The strong association between abdominal pain and other symptoms of anxiety may reflect the centrality of abdominal pain as a key symptom of anxiety.
Two promising factors have been identified in both children with RAP and children with anxiety that may help explain the link between the two: temperament and stress response and recovery. Behavioral inhibition to the unfamiliar, or the temperamental tendency to become physiologically aroused and behaviorally restrained in the face of novelty, has been found to be associated with increased risk for childhood anxiety disorders (Biederman et al., 1993; Hirshfeld et al., 1992; Kagan, 2003). Children with RAP have been found to display many temperamental features found in behaviorally inhibited children (Campo et al., 2004). Further, differences in temperament have been associated with more general differences in biobehavioral reactivity to stress (Boyce, Barr, & Zeltzer, 1992), which may also contribute to the development and exacerbation of abdominal pain symptoms. To date, few studies have examined stress recovery in these populations. Because parasympathetic activation is required for both stress recovery and processes relating to digestion and to reducing overall arousal, it remains a promising avenue of research particularly for distinguishing the mechanisms that are common to or discriminate between RAP and anxiety in children.
The present study has several limitations. First, our sample size is relatively small, making it difficult to detect effects that were small to medium in magnitude. Small sample size may have particularly limited our statistical power in analyses of child self-report questionnaire data. We administered the YSR to all children 11 years of age or older, which excluded those children in our sample ages 8–10. Our sample in each of the three groups dropped nearly by half, thus decreasing power to detect differences between groups.
A second limitation is in the difficulty of determining the degree of overlap between RAP and anxiety disorders in this study. This is in part because we drew our RAP and anxiety sample from a tertiary care setting for the treatment of pediatric gastrointestinal problems (RAP group) and from a community mental health center that treats children with anxiety (anxiety group). As a result, children in this study are likely to differ from children in the general population who suffer from RAP or anxiety who have not sought or been referred for medical or psychiatric care. “Berkson's bias” suggests that it is the confluence of problems that initiates patients to seek or be referred for professional care when symptoms arise, increasing the likelihood of comorbid problems in clinical samples (McConaughy & Achenbach, 1994). Since our sample was drawn from a tertiary care clinic, Berkson's bias would predict the comorbidity of RAP and anxiety to be higher in samples presented in this study than would be found in the general population of children with either of these disorders. The degree of overlap between RAP and diagnoses of anxiety disorders may thus be inflated. Despite this concern, data from this study do suggest that children who are treated in tertiary care clinics for their abdominal pain are likely to have symptoms of anxiety. Further, our well sample was not community based but rather was selected to include only children without abdominal pain and anxiety to provide a comparison group that was free of the RAP and anxiety disorders. Thus, our comparison group was highly selected and not representative of the general population of children. It should be noted that, despite our selective recruitment process, one child in the well group did meet criteria for Specific Phobia.
These limitations notwithstanding, the present study extends the pediatric literature on psychological factors involved in chronic pain. Our use of multi-method and cross-informant methods (child-report, parent-report, and use of both questionnaire and diagnostic data) has allowed us to more reliably measure psychological factors involved in recurrent abdominal pain in children.
Further understanding of the links between RAP and anxiety is essential to understanding the development and progression of RAP, and in informing the prevention and treatment of the disorder. Oftentimes, psychosocial problems are not addressed in primary or tertiary care pediatric clinics. However, as findings summarized in this article suggest, psychosocial concerns are not only present in children with RAP, they may also contribute to the exacerbation or maintenance of the disorder. Using a biopsychosocial approach when assessing and treating RAP in children could lead to interventions with children with RAP and their caregivers targeting anxiety. Understanding RAP as associated with underlying anxiety disorders may encourage providers to assess for anxiety and, if appropriate, facilitate referral for psychiatric evaluation and treatment.
Conflicts of interest: None declared.
References
- Achenbach TM, McMonaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. Burlington, VT: ASEBA; 2001. [Google Scholar]
- Apley J. The child with abdominal pain. 2nd. Oxford: Blackwell Scientific Publications; 1975. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: 1994. [Google Scholar]
- Biederman J, Rosenbaum JF, Bolduc-Murphy EA, Faraone SV, Chaloff J, Hirshfeld DR, et al. A 3-year follow-up of children with and without behavioral inhibition. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:814–821. doi: 10.1097/00004583-199307000-00016. [DOI] [PubMed] [Google Scholar]
- Boyce WT, Barr RG, Zeltzer LK. Temperament and the psychobiology of childhood stress. Pediatrics. 1992;90:483–486. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral analyses. 2nd. Hillsdale, NJ: Laurence Erlbaum Associates; 1988. [Google Scholar]
- Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(7):878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113(4):817–824. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:873–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Colletti RB. Recurrent abdominal pain. In: Burg FD, Ingelfinger JR, Wald ER, Polin RA, editors. Current pediatric therapy. Philadelphia, PA: W.B. Saunders; 1998. [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: Critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Devanarayana NM, de Silva DGH, de Silva HJ. Recurrent abdominal pain syndrome in a cohort of Sri Lankan children and adolescents. Journal of Tropical Pediatrics. 2008;54(3):178–183. doi: 10.1093/tropej/fmm114. [DOI] [PubMed] [Google Scholar]
- Dorn LD, Campo JC, Thato S, Dahl RE, Lewin D, Ramamurti C, et al. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(1):66–75. doi: 10.1097/00004583-200301000-00012. [DOI] [PubMed] [Google Scholar]
- Dufton L, Compas BE. Recurrent abdominal pain in children: Biopsychosocial processes. Manuscript submitted for publication; 2008. [Google Scholar]
- Egger HL, Costello JE, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: Stomach aches, musculoskeletal pains, and headaches. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(7):852–860. doi: 10.1097/00004583-199907000-00015. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(6):1127–1134. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- Garber J, Zeman J, Walker LS. Recurrent abdominal pain in children: Psychiatric diagnoses and parental psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;29:648–656. doi: 10.1097/00004583-199007000-00021. [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin. 2007;133(4):581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Riddle MA, Davies M. Somatic symptoms in children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(10):1179–1187. doi: 10.1097/01.chi.0000231974.43966.6e. [DOI] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Merikangas K, Woods SW, Davis M. Measuring the time course of anticipatory anxiety unsing the fear-potentiated startle reflex. Psychophysiology. 1993;30(4):340–346. doi: 10.1111/j.1469-8986.1993.tb02055.x. [DOI] [PubMed] [Google Scholar]
- Hirshfeld DR, Rosenbaum JF, Biederman J, Bolduc EA, Faraone SV, Snidman N, et al. Stable behavioral inhibition and its association with anxiety disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:103–111. doi: 10.1097/00004583-199201000-00016. [DOI] [PubMed] [Google Scholar]
- Hollingshead AA. New Haven, CT: Yale University; 1975. Four-factor index of social status. Unpublished manuscript. [Google Scholar]
- Huguet A, Mori J. The severity of chronic pediatric pain: An epidemiological study. The Journal of Pain. 2007;9(3):226–236. doi: 10.1016/j.jpain.2007.10.015. [DOI] [PubMed] [Google Scholar]
- Kagan J. Biology, context, and developmental inquiry. Annual Review of Psychology. 2003;54:1–23. doi: 10.1146/annurev.psych.54.101601.145240. [DOI] [PubMed] [Google Scholar]
- Kagan J, Reznick JS, Snidman N. Biological bases of childhood shyness. Science. 1988:240. doi: 10.1126/science.3353713. 167–171. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konijnenberg AY, de Graeff-Meeder ER, van der Hoeven J, Kimpen JLL, Buitelaar JK, Uiterwaal CSPM. Psychiatric morbidity in children with medically unexplained chronic pain: Diagnosis from the pediatrician's perspective. Pediatrics. 2006;117:889–897. doi: 10.1542/peds.2005-0109. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Liakopoulou-Kairis M, Alifieraki T, Protagora D, Korpa T, Kondyli K, Dimosthenous E, et al. Recurrent abdominal pain and headache: Psychopathology, life event, and family functioning. European Child and Adolescent Psychiatry. 2002;11:115–122. doi: 10.1007/s00787-002-0276-0. [DOI] [PubMed] [Google Scholar]
- March JS, Albano AM. Assessment of anxiety disorders in children and adolescents. In: Riddle M, editor. Annual review of psychiatry. Washington, DC: American Psychiatric Association; 1996. pp. 415–427. [Google Scholar]
- McConaughy SH, Achenbach TM. Comorbidity of empirically based syndromes in matched general population and clinical samples. Journal of Child Psychology and Psychiatry. 1994;35(6):1141–1157. doi: 10.1111/j.1469-7610.1994.tb01814.x. [DOI] [PubMed] [Google Scholar]
- McGrath PJ. Paedriatric pain: A good start. Pain. 1990;41(3):253–254. doi: 10.1016/0304-3959(90)90001-T. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J. Schedule for affective disorder and schizophrenia for school-age children-epidemiologic 4th version. Ft. Lauderdale: Nova University, Center for Psychological Study; 1987. [Google Scholar]
- Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, et al. Childhood functional gastrointestinal disorders. Gut. 1999;45(Suppl II):II60–II68. doi: 10.1136/gut.45.2008.ii60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. The American Journal of Psychiatry. 1997;154(11):1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Safford SM, Kendall PC, Flanner-Schroeder E, Webb A, Sommer H. A longitudinal look at parent-child diagnostic agreement in youth treated for anxiety disorders. Journal of Clinical Child & Adolescent Psychology. 2005;34(4):747–757. doi: 10.1207/s15374424jccp3404_16. [DOI] [PubMed] [Google Scholar]
- Starfield B, Katz H, Gabriel A. Morbidity in childhood: A longitudinal review. New England Journal of Medicine. 1984;310:824–829. doi: 10.1056/NEJM198403293101305. [DOI] [PubMed] [Google Scholar]
- Stickler GB, Murphy DB. Recurrent abdominal pain. American Journal of Disease in Childhood. 1979;133(5):486–489. doi: 10.1001/archpedi.1979.02130050030006. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Friedman BH, Borkovec TD. Autonomic characterics of generalized anxiety disorder and worry. Biological Psychiatry. 1996;39(4):255–266. doi: 10.1016/0006-3223(95)00136-0. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Van Slyke DA, Greene JW. Long-term health outcomes in patients with recurrent abdominal pain. Journal of Pediatric Psychology. 1995;20(2):233–245. doi: 10.1093/jpepsy/20.2.233. [DOI] [PubMed] [Google Scholar]