Abstract
Background
We determined whether patients with lower-extremity peripheral arterial disease (PAD) who are more physically active during daily life have lower mortality rates than PAD patients who are less active.
Methods and Results
Participants were 460 men and women with PAD (mean age 71.9±8.4 years) followed up for 57 months (interquartile range 36.6 to 61.9 months). At baseline, participants were interviewed about their physical activity. Vertical accelerometers measured physical activity continuously over 7 days in 225 participants. Analyses were adjusted for age, sex, race, body mass index, hypertension, smoking, comorbidities, total cholesterol, HDL cholesterol, leg symptoms, and ankle-brachial index. At 57-month follow-up, 134 participants (29%) had died, including 75 participants (33%) who wore accelerometers. Higher baseline physical activity levels measured by vertical accelerometer were associated with lower all-cause mortality (Ptrend=0.003). Relative to PAD participants in the highest quartile of accelerometer-measured physical activity, those in the lowest quartile had higher total mortality (hazard ratio 3.48, 95% confidence interval 1.23 to 9.87, P=0.019). Similar results were observed for the combined outcome of cardiovascular events or cardiovascular mortality (Ptrend=0.005). Higher numbers of stair flights climbed during 1 week were associated with lower total mortality (Ptrend=0.035).
Conclusions
PAD patients with higher physical activity during daily life have reduced mortality and cardiovascular events compared with PAD patients with the lowest physical activity, independent of confounders. Further study is needed to determine whether interventions that increase physical activity during daily life are associated with improved survival in patients with PAD.
Keywords: claudication, mortality, peripheral vascular disease, physical activity
Lower-extremity peripheral arterial disease (PAD) affects ≈8 million men and women in the United States.1 In primary care medical practices, 20% to 25% of older men and women have a low ankle-brachial index (ABI) consistent with PAD.2,3 Men and women with PAD have higher mortality rates than persons without PAD.4,5
In healthy populations, higher physical activity levels are associated with lower all-cause and cardiovascular disease mortality6–13; however, it is unknown whether higher physical activity levels are associated with lower mortality in patients with PAD. PAD patients have significantly reduced activity levels compared with individuals without PAD.14 It is unclear whether, across the range of activity levels observed in patients with PAD, persons with higher physical activity levels have better outcomes than those with lower physical activity levels. In addition, although supervised exercise rehabilitation improves functional performance in persons with PAD,15 the benefits of higher physical activity levels during daily life among persons with PAD are unknown.
We determined whether, among patients with PAD, higher levels of physical activity during daily life were associated with lower mortality. If higher physical activity levels are associated with lower mortality in patients with PAD, then interventions to increase daily physical activity levels in this population may be beneficial.
Methods
Participant Identification
The institutional review boards of Northwestern University and Catholic Health Partners Hospital approved the protocol. Participants gave written informed consent.
Participants were part of the Walking and Leg Circulation Study (WALCS),16,17 a prospective, observational study designed to identify predictors of functional decline in PAD. Participants were identified from among consecutive patients aged 55 years and older diagnosed with PAD in 3 Chicago-area noninvasive vascular laboratories. All participants had an ABI <0.90 at their baseline visit. Exclusion criteria have been reported previously.16
ABI Measurement
A handheld Doppler probe (Nicolet Vascular Pocket Dop II; Nicolet Biomedical Inc, Golden, Colo) was used to obtain systolic pressures in the right and left brachial, dorsalis pedis, and posterior tibial arteries.18,19 Each pressure was measured twice: in the order listed and in reverse order. The ABI was calculated by dividing the mean of the dorsalis pedis and posterior tibial pressures in each leg by the mean of the 4 brachial pressures.18 Average brachial pressures in the arm with highest pressure were used when one brachial pressure was higher than the opposite brachial pressure in both measurement sets and the 2 brachial pressures differed by 10 mm Hg or more in at least 1 measurement set, because in such cases, subclavian stenosis was possible.18,19 The lowest leg ABI was used in analyses.
Comorbidities
Comorbidities assessed were diabetes mellitus, angina, myocardial infarction, heart failure, cancer, chronic lung disease, and stroke. Disease-specific algorithms that combine data from patient report, medical record review, medications, laboratory values, and a questionnaire completed by the participant’s primary care physician were used to verify and document baseline and incident comorbidities on the basis of criteria developed previously.20 History of coronary revascularization was considered present if reported by the patient or the primary care physician or identified during medical record review.
Blood Collection
Blood was collected into citrate evacuated tubes and immediately put on ice. Tubes were spun at 3000 rpm for 20 minutes at 4°C in a refrigerated centrifuge. Blood was stored at −70°C until analyses were completed up to 3 years after blood collection.
Total Cholesterol and HDL Levels
Total cholesterol levels were measured with an enzymatic reaction (peroxidase/phenol-4-aminoiphenazone indicator reaction).21,22 HDL cholesterol was measured with a direct enzymatic colorimetric assay.22
C-Reactive Protein
High-sensitivity C-reactive protein (hsCRP) levels were determined by an immunotechnique on the Behring BN II analyzer (Dade Behring, Wilmington, Del).
Exertional Leg Symptoms
Leg symptoms were classified on the basis of responses to the San Diego Claudication Questionnaire, according to prior study.16,17,23
Other Measures
Body mass index (BMI) was calculated as weight (kilograms)/height (meters)2. Pack-years of cigarette smoking and history of hypertension were determined by patient report.
Functional Measures
Six-Minute Walk
Following a standardized protocol,24,25 participants walked up and down a 100-ft hallway for 6 minutes after being given instructions to cover as much distance as possible.
Physical Activity
Accelerometer-Measured Physical Activity
Physical activity levels were measured objectively and continuously over 7 days with a vertical accelerometer (Caltrac, Muscle Dynamics Fitness Network, Inc, Torrance, Calif).26–31 After 7 days, participants reported the number of activity units displayed on the accelerometer by telephone to investigators and mailed their accelerometer back to the investigators. We programmed the accelerometer identically for all participants, which allowed us to compare physical activity levels between participants, irrespective of individual variation in age, weight, height, and sex.26,27,30,31 Programmed in this way, the accelerometers measured “activity units.”26,27,30,31 This method of measuring physical activity in patients with PAD has been demonstrated previously.14,30,31 For example, in one study, there were no differences in accelerometer scores between persons with and without PAD over a fixed distance of 800 feet; however, over a period of 7 days, PAD participants had substantially lower Caltrac-assessed activity than non-PAD participants.31 Because of limited numbers of accelerometers, we distributed them to participants (49%) whenever available.
Patient-Reported Physical Activity Measures
At the initial visit, participants were asked, “During the last week, how many city blocks or their equivalent did you walk? Let 12 city blocks equal 1 mile.” Participants were also asked, “In the last week, about how many flights of stairs did you climb up? A flight is 10 steps.” Participants were asked to report the number of times they went walking for exercise during the prior week.
Death
We used the Social Security Administration death database to search for deaths through December 31, 2003. At baseline, each participant provided the names of 3 proxies not living with them to assist with the ascertainment of complete follow-up data. Information on deaths was also obtained from family members, proxies, and primary care physicians. Death certificates were obtained from the state of Illinois or from the patients’ medical records.
Statistical Analyses
Baseline characteristics between decedents and survivors were compared with general linear models for continuous variables and χ2 tests for categorical variables, with adjustment for age and sex. Person-time for each participant was calculated as the number of months from the baseline visit to the date of the most recent visit (last seen) or the date of death, whichever came first. Baseline physical activity levels for each physical activity measure were categorized into quartiles. The fourth quartile represented the highest activity level and the first quartile the lowest activity. Proportional hazards analyses were used to compare differences in survival across quartiles of baseline activity levels, with adjustment for age, sex, race, comorbidities, cigarette smoking, BMI, total cholesterol, high-density lipoprotein (HDL) cholesterol, leg symptoms, and ABI. We tested the proportional hazards assumption for total mortality using martingale residuals–based methods, and we did not find any evidence of significant deviation from the proportional hazards assumption.32
Analyses were repeated for the combined outcome of cardiovascular events or cardiovascular mortality. Cardiovascular events were myocardial infarction, coronary revascularization, or hospitalization for angina or heart failure. Cardiovascular death was defined as death due to myocardial infarction, stroke, or heart failure or sudden death. The causes of 33 of the observed 134 deaths were unknown in the overall population (including 19 of the 75 deaths within the population that wore the vertical accelerometer).
We used multiple imputation methods (10 repeated imputations were used in the analyses) in competing risk analyses to handle the missing cause of death when death certificates were unobtainable.33 Missing data were considered missing at random in that the conditional probability of cardiovascular death among participants with missing death certificates can be modeled with logistic regression with a set of baseline covariates as independent variables.
To determine whether inflammation mediated the associations between physical activity and mortality or cardiovascular events, analyses were repeated with adjustment for hsCRP. We also evaluated associations between baseline physical activity and mortality, adjusting for baseline 6-minute walk performance. Finally, proportional hazards analysis was conducted to determine the association between baseline 6-minute walk performance and total mortality, with adjustment for age, sex, race, comorbidities, ABI, BMI, smoking, total cholesterol, HDL cholesterol, and leg symptoms.
The authors had full access to the data and take full responsibility for its integrity. All authors have read and agree to the manuscript as written.
Results
The study included 460 participants with PAD, 134 of whom died during follow-up. Median follow-up was 57 months (interquartile range 36.6 to 61.9 months). Of the 460 participants, 225 wore the vertical accelerometer for 7 days (75 of whom died during follow-up). Forty percent of deaths were due to cardiovascular disease, and 31% were due to cancer.
The mean age of survivors and decedents was 71.1±8.1 and 73.8±9.0 years, respectively (P=0.001). Table 1 compares other characteristics of survivors and decedents, with adjustment for age and sex. Fifty-six percent of survivors were men versus 68% of decedents (P=0.017). Compared with survivors, decedents included a higher proportion of blacks, and they had a lower ABI, a higher number of cardiac or cerebrovascular diseases, and lower accelerometer-measured physical activity (Table 1). Decedents had higher baseline prevalences of hypertension, cancer, pulmonary disease, and diabetes mellitus (Table 1). Participants who wore a vertical accelerometer had significantly higher HDL levels than those who did not (Table 2). There were no other differences in characteristics of participants who wore the accelerometer versus those who did not (Table 2). Across the quartiles of accelerometer-measured physical activity levels, we observed significant associations between higher accelerometer-measured physical activity levels with more blocks walked, more stair flights climbed, and better 6-minute walk performance (Table 3).
TABLE 1.
Characteristics of Study Participants With PAD According to Survivor Status*
| All Participants (n=460) | Survivors (n=326) | Decedents (n=134) | P† | |
|---|---|---|---|---|
| Black race, % | 15.6 | 13.3 | 21.3 | 0.040 |
| ABI | 0.65 | 0.66±0.01 | 0.62±0.01 | 0.017 |
| BMI, kg/m2 | 27.3 | 27.5±0.27 | 26.7±0.43 | 0.109 |
| Cigarette smoking, pack-years | 39.0 | 38.3±1.86 | 40.8±2.92 | 0.476 |
| No. of cardiac or cerebrovascular diseases | 1.05 | 0.96±0.06 | 1.27±0.09 | 0.005 |
| Hypertension, % | 80.9 | 77.2 | 89.7 | 0.002 |
| Cancer, % | 16.0 | 12.8 | 23.8 | 0.005 |
| Pulmonary disease, % | 32.5 | 28.5 | 42.1 | 0.007 |
| Diabetes, % | 31.0 | 26.1 | 43.0 | 0.001 |
| History of coronary revascularization, % | 35.7 | 37.6 | 31.2 | 0.205 |
| Total cholesterol, mg/dL | 180.1 | 178.4±2.2 | 182.9±3.6 | 0.301 |
| HDL, mg/dL | 40.3 | 40.8±0.82 | 37.7±1.33 | 0.052 |
| Accelerometer-measured physical activity level, activity units‡ | 784.0 | 844.6±33.5 | 662.4±47.7 | 0.002 |
Values shown are mean±SE or as indicated. Cardiac or cerebrovascular disease is expressed as the number of types of cardiac or cerebrovascular disease participants had (among congestive heart failure, myocardial infarction, stroke, and angina).
Comparisons were made between survivors and decedents.
Based on 225 participants who wore the vertical accelerometer.
TABLE 2.
Characteristics of Study Participants With PAD According to Use of Vertical Accelerometers*
| All Participants (n=460) | Vertical Accelerometer Use (n=225) | No Accelerometer Use (n=235) | P | |
|---|---|---|---|---|
| Age, y | 71.9±8.4 | 72.3±8.4 | 71.4±8.5 | 0.268 |
| Male, % | 59.4 | 63.1 | 55.7 | 0.108 |
| Black race, % | 16.5 | 16.8 | 16.2 | 0.836 |
| ABI | 0.649±0.15 | 0.644±0.15 | 0.653±0.15 | 0.467 |
| BMI, kg/m2 | 27.3±4.9 | 27.3±5.1 | 27.3±4.7 | 0.917 |
| Cigarette smoking, pack-years | 39.0±34.9 | 41.1±35.7 | 37.0±34.2 | 0.992 |
| No. of cardiac or cerebrovascular diseases | 1.05±1.08 | 1.07±1.06 | 1.03±1.09 | 0.683 |
| Hypertension, % | 80.4 | 80.9 | 80.0 | 0.810 |
| Cancer, % | 16.1 | 16.0 | 16.2 | 0.960 |
| Pulmonary disease, % | 32.8 | 32.0 | 33.6 | 0.712 |
| Diabetes, % | 32.0 | 33.3 | 30.6 | 0.536 |
| Total cholesterol, mg/dL | 180±38.5 | 182±37.5 | 177±39.4 | 0.218 |
| HDL, mg/dL | 39.9±15.1 | 41.7±17.0 | 38.2±12.6 | 0.021 |
| Intermittent claudication, % | 19.8 | 19.6 | 20.0 | 0.909 |
| No exertional leg symptoms, % | 19.1 | 19.1 | 19.2 | 0.992 |
Values are expressed as mean±SD unless otherwise indicated.
TABLE 3.
Associations Between 7-Day Physical Activity Quartiles and Patient-Reported Activity and Functional Performance Among Participants Who Wore Vertical Accelerometers*
| No. of People | Blocks Walked per Week | Stair Flights Climbed per Week | 6-Minute Walk Performance, m | |
|---|---|---|---|---|
| 4th (highest) quartile of physical activity (≥1113 activity units)† | 40 | 30 (14–80) | 17 (3–42) | 434 (398–482) |
| 3rd quartile of physical activity (788 to <1113 activity units) | 57 | 13 (5–38) | 5 (0–21) | 346 (294–418) |
| 2nd quartile of physical activity (540 to <788 activity units) | 63 | 14 (6–40) | 7 (1–21) | 339 (259–399) |
| 1st (lowest) quartile of physical activity (<540 activity units) | 65 | 8 (1.5–20) | 3 (0–28) | 277 (221–335) |
| Ptrend | … | <0.001 | 0.026 | <0.001 |
Results for blocks walked, stair flights climbed, and 6-minute walk performance are presented as median (interquartile range). Differences in medians were evaluated with nonparametric Kruskal-Wallis tests.
Represents physical activity level measured over 7 days with a vertical accelerometer (activity units); n=225.
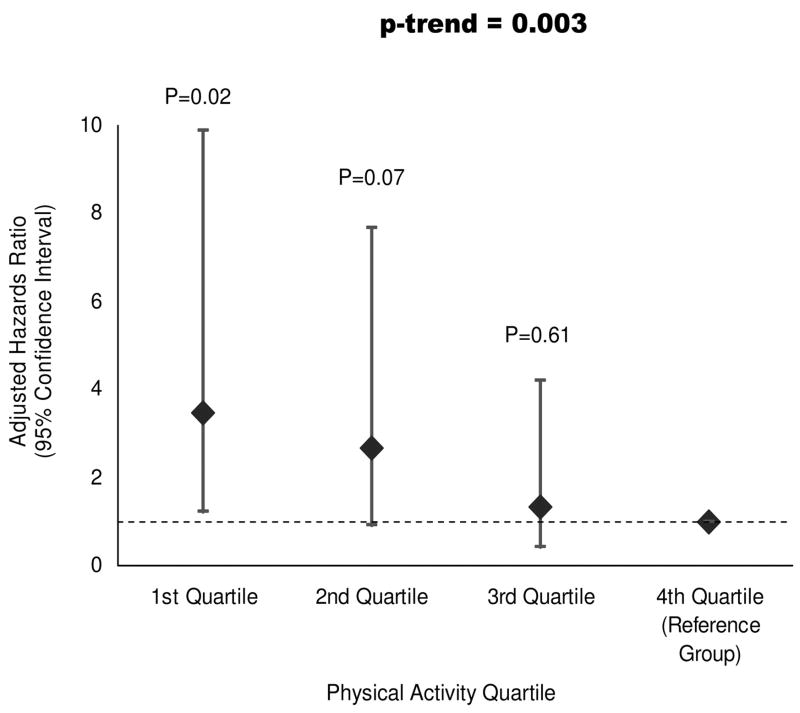
Figure 1 shows associations between baseline physical activity levels, measured by the vertical accelerometer, and total mortality. With adjustment for age, sex, race, BMI, ABI, pack-years of smoking, comorbidities, total cholesterol, HDL cholesterol, and leg symptoms, higher physical activity levels were associated with lower mortality at 57-month follow-up (Ptrend=0.003). Compared with the highest (4th) quartile of physical activity levels, participants in the lowest (1st) quartile had a significantly higher risk of mortality (hazard ratio (HR) 3.48, 95% confidence interval(CI) 1.23 to 9.87, P=0.019). Additional covariates associated significantly with mortality were diabetes mellitus (P=0.002) and pulmonary disease (P=0.035; Table 4). The results were not changed substantially after adjustment for hsCRP (overall Ptrend=0.015; HR for the 1st versus 4th quartile 3.09, 95% CI 1.06 to 8.99, P=0.039). In these latter analyses, hsCRP was not associated significantly with mortality (P=0.663).
Figure 1.
Adjusted associations between baseline physical activity and total mortality among men and women with PAD. Ptrend=0.003.
TABLE 4.
Results of Proportional Hazards Analyses Relating Clinical Characteristics to Mortality Among Men and Women With PAD*
| Covariates | Hazard Ratios (95% CI) | P |
|---|---|---|
| Age (per year) | 1.01 (0.98–1.05) | 0.560 |
| Male gender | 1.23 (0.57–2.67) | 0.604 |
| Black | 1.52 (0.76–3.06) | 0.236 |
| BMI (kg/m2) | 0.95 (0.89–1.01) | 0.112 |
| Diabetes mellitus | 2.50 (1.40–4.45) | 0.002 |
| HDL cholesterol (mg/dL) | 0.98 (0.96–1.00) | 0.104 |
| Total cholesterol (mg/dL) | 1.01 (1.00–1.02) | 0.082 |
| Hypertension | 2.18 (0.88–5.42) | 0.092 |
| No. of cardiovascular diseases | 1.24 (0.95–1.62) | 0.108 |
| Cigarette smoking (pack-years) | 1.00 (0.99–1.01) | 0.704 |
| ABI | 2.89 (0.42–20.18) | 0.284 |
| History of coronary revascularization | 0.61 (0.31–1.17) | 0.137 |
| Pulmonary disease | 1.95 (1.05–3.63) | 0.035 |
| Cancer | 1.60 (0.78–3.26) | 0.199 |
| Leg symptoms | ||
| No exertional pain | 0.36 (0.11–1.15) | 0.083 |
| Pain relieved with rest | 0.65 (0.19–2.18) | 0.481 |
| Intermittent claudication | 0.63 (0.20–1.95) | 0.420 |
| Pain at rest | 0.59 (0.20–1.77) | 0.349 |
| Physical activity | ||
| 4th quartile of physical activity (≥1113 activity units) | 1.0 (Referent) | N/A |
| 3rd quartile of physical activity (788 to <1113 activity units) | 1.34 (0.43–3.18) | 0.609 |
| 2nd quartile of physical activity (540 to<788 activity units) | 2.66 (0.92–7.67) | 0.070 |
| 1st quartile of physical activity (<540 activity units) | 3.48 (1.23–9.87) | 0.019 |
Results of multivariable Cox model including variables listed in Table. Model corresponds to analyses presented in Figure 1.
Because participants who were ill at baseline were likely both to be inactive and to have a higher mortality risk, we repeated analyses after excluding participants who died during the first 2 years. A similar, significant trend remained between higher physical activity levels and lower mortality (Ptrend=0.028), even after we excluded individuals who died during the first 2 years of follow-up. In these analyses, the HR for participants in the lowest versus highest quartile of physical activity at baseline was 4.22 (95% CI 1.09 to 16.3, P=0.037). To adjust for the effects of better physical performance on the relationship between physical activity and mortality, analyses were repeated with additional adjustment for 6-minute walk performance. Associations between accelerometer-measured activity and total mortality were somewhat attenuated but remained statistically significant overall (overall Ptrend for association between accelerometer-measured physical activity and mortality 0.018; HR for participants in the lowest versus highest quartile of physical activity 2.81, 95% CI 0.93 to 8.49, P=0.067).
Table 5 shows associations between patient-reported physical activity and total mortality. After adjustment for confounders, fewer flights of stairs climbed during the previous week were associated with higher mortality (Table 5).
TABLE 5.
Associations Between Patient-Reported Physical Activity Levels and Total Mortality in Persons With PAD*
| No. of People | No. of Deaths | Hazard Ratios (95% CI)† | P‡ | Ptrend | |
|---|---|---|---|---|---|
| City blocks walked during the past 7 days (n=453) | 0.096 | ||||
| 4th quartile of city blocks walked (≥48) | 86 | 19 | 1.0 (Referent) | … | |
| 3rd quartile of city blocks walked (18 to <48) | 113 | 21 | 0.93 (0.45–1.93) | 0.844 | |
| 2nd quartile of city blocks walked (6 to <18) | 126 | 44 | 1.79 (0.94–3.42) | 0.078 | |
| 1st quartile of city blocks walked (<6) | 128 | 47 | 1.47 (0.75–2.87) | 0.265 | |
| 7-Day stair flights climbed (1 flight=10 steps, n=458) | 0.035 | ||||
| 4th quartile of flights climbed (≥28) | 111 | 26 | 1.0 (Referent) | … | |
| 3rd quartile of flights climbed (7 to <28) | 114 | 28 | 1.12 (0.61–1.03) | 0.713 | |
| 2nd quartile of flights climbed (1 to<7) | 124 | 37 | 1.26 (0.70–2.27) | 0.435 | |
| 1st quartile of flights climbed <1) | 109 | 42 | 1.84 (1.03–3.29) | 0.038 |
Results of multivariable proportional hazards regression models.
Model adjusted for covariates in age, gender, race, BMI, and baseline covariates (ABI, pack-years of smoking, leg symptoms, comorbidities, total cholesterol, and HDL cholesterol).
Pairwise comparison with referent group.
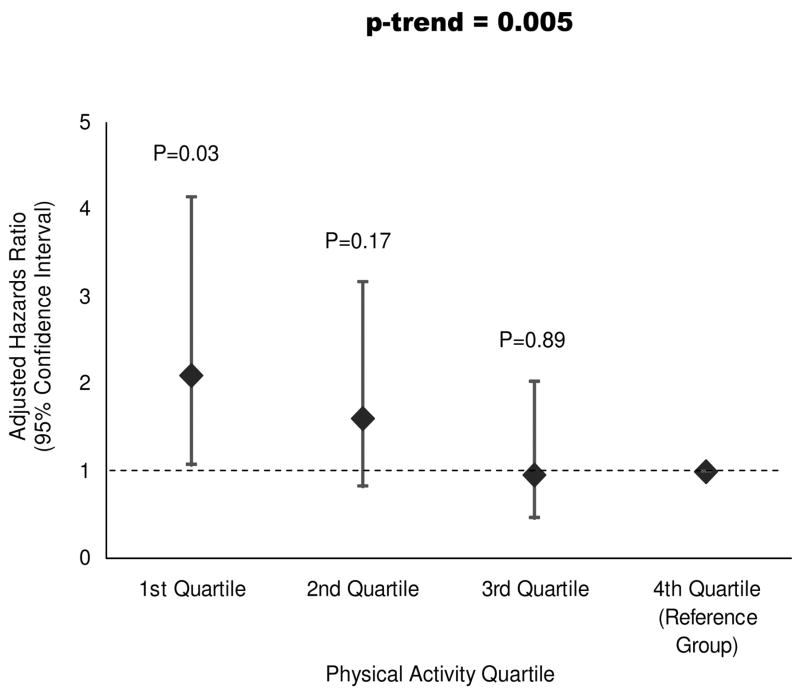
Higher baseline accelerometer-measured physical activity levels during daily life were associated with lower cardiovascular events or cardiovascular mortality at 57-month follow-up, after adjustment for confounders (Ptrend=0.005; HR for participants in the lowest versus highest quartile of physical activity 2.10, 95% CI 1.06 to 4.14, P=0.033; Figure 2). There were no significant associations between stair flights climbed or blocks walked during the past week with the combined outcome of cardiovascular events or mortality (data not shown).
Figure 2.
Adjusted associations between baseline physical activity and cardiovascular disease events or cardiovascular mortality among men and women with PAD. Ptrend=0.005.
Better 6-minute walk performance at baseline was associated with lower mortality at 57-month follow-up, after adjustment for age, sex, race, ABI, BMI, smoking, comorbidities, total cholesterol, HDL cholesterol, and leg symptoms. The HR was 0.76 per SD higher increment of 6-minute walk performance (95% CI 0.59 to 0.97, P=0.027). The SD for the 6-minute walk was 376 feet. In analyses that included adjustment for accelerometer-measured physical activity in addition to the 6-minute walk, the association between 6-minute walk performance and total mortality was no longer significant (P=0.085).
Discussion
Among persons with PAD, lower physical activity levels during daily life, measured by a vertical accelerometer, were associated with significantly higher mortality at 5-year follow-up compared with higher physical activity during daily life. Individuals in the lowest baseline quartile of physical activity had a 3-fold higher mortality rate than those in the highest baseline quartile. Results were largely unchanged even after the exclusion of participants who died during the first 2 years of follow-up. Similarly, individuals in the lowest baseline quartile of physical activity had an increased risk of cardiovascular events or cardiovascular deaths relative to participants in the highest baseline quartile. Participants with the best 6-minute walk performance at baseline had lowest mortality at follow-up, but these findings were attenuated after additional adjustment for physical activity. Our findings suggest that clinicians should encourage patients with PAD to increase their physical activity during daily life.
Supervised treadmill walking substantially improves walking performance in patients with intermittent claudication15; however, barriers such as cost and transportation limit access to exercise rehabilitation programs for most patients with PAD.34,35 Supervised treadmill walking exercise is a relatively intense intervention that differs substantially from physical activity during daily life. To the best of our knowledge, no prior studies have assessed the relationship between physical activity levels during daily life and outcomes in persons with PAD.
The present results are important in part because patients with PAD have substantially higher mortality than individuals without PAD.4,5 In addition, persons with PAD have substantially lower physical activity levels than individuals without PAD.17,30,36,37 In one study of persons aged 55 years and older, 20 PAD participants had less than half of the activity observed in 21 non-PAD participants (803 activity units/week versus 1750 activity units/week, P<0.001).30 Another study found similar results when comparing physical activity levels measured by an accelerometer for 85 PAD patients with intermittent claudication versus 59 patients without PAD (357 kcal/d versus 616 kcal/d, P<0.001).37
Study Limitations
The present study has limitations. Only 49% of participants wore the vertical accelerometer device because of the limited availability of these monitors. Vertical accelerometers were provided to each participant at the end of their study visit on the basis of availability. However, except for a higher HDL cholesterol level among participants who wore the accelerometer, there were no differences in baseline characteristics between participants who wore the accelerometer versus those who did not. A second limitation is that the present study was observational. Unidentified confounders associated with higher physical activity levels may have contributed to the differences observed here. A third limitation is that we did not collect data on intensity of physical activity levels. A fourth limitation is that our multivariate proportional hazards analyses included up to 21 covariates, which may result in model overfitting; however, we conducted additional analyses in which potential confounders were entered sequentially into the regression model. Results showed that the adjusted associations between physical activity and mortality (or cardiovascular events) were not sensitive to the number of covariates in the multivariate analyses. Nonetheless, our findings require confirmation in other PAD populations. Finally, our findings may be due to greater illness severity among PAD patients, who are both less physically active and at higher mortality risk. However, the exclusion of deaths during the first 2 years of follow-up did not change our findings.
In conclusion, PAD patients with higher levels of physical activity during daily life have reduced mortality rates. Future study with a clinical trial is necessary to determine whether interventions that increase physical activity levels during daily life reduce mortality in patients with PAD. In the meantime, the present findings suggest that clinicians should encourage patients with PAD to increase their physical activity during daily life.
CLINICAL PERSPECTIVE
Supervised walking exercise programs are associated with improved treadmill walking performance in patients with lower-extremity peripheral arterial disease (PAD); however, the benefits of greater walking activity during daily life for patients with PAD are unknown. Four hundred sixty men and women with PAD were followed up prospectively to determine the association between physical activity during daily life at baseline and mortality at 57-month follow-up. Physical activity was measured continuously over 7 days with a vertical accelerometer in 225 participants. Lower baseline physical activity during daily life, measured by the accelerometer, was associated with significantly higher mortality at follow-up. Relative to participants in the highest baseline quartile of accelerometer-measured physical activity, those in the lowest quartile at baseline had a 3.5-fold increased risk of mortality. Similar associations were observed between lower accelerometer-measured physical activity and higher rates of the combined outcome of cardiovascular events or mortality. Among all 460 participants, fewer stair flights climbed during the prior week were associated with increased total mortality. In conclusion, our findings suggest that greater physical activity during daily life is associated with lower mortality in persons with PAD. Clinicians should advise their patients with PAD to increase their walking activity and stair flights climbed during daily life. Because data reported here are observational, additional study with a randomized controlled clinical trial is warranted.
Acknowledgments
Sources of Funding
This study was supported by grants R01-HL58099, R01-HL64739, and R01-HL71223 from the National Heart, Lung, and Blood Institute and by grant RR-00048 from the National Center for Research Resources, National Institutes of Health. Drs McDermott, Tian, Liu, Criqui, Ferrucci, and Guralnik are investigators on R01-HL073351 from the National Heart, Lung, and Blood Institute (NHLBI). J. Tan is a member of the data management team for R01-HL073351. Dr McDermott is also principal investigator on R01-HL073912 from the NHLBI.
Footnotes
Disclosures
Drs Tian and Liu are coinvestigators and Dr McDermott is Principal Investigator for the “Improving Functioning in Peripheral Arterial Disease” research grant (R01-HL073351) from the NHLBI. Drs Criqui, Ferrucci, and Guralnik serve as consultants for and J. Tan is part of the data management team for this same research grant.
References
- 1.Allison MA, Criqui MH, Ho E, Denenberg J. The estimated ethnic-specific prevalence of peripheral arterial disease in the United States, 2000. Circulation. 2004;110(suppl III):III-817. doi: 10.1016/j.amepre.2006.12.010. Abstract. [DOI] [PubMed] [Google Scholar]
- 2.Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 3.McDermott MM, Kerwin DR, Liu K, Martin GJ, O’Brien E, Kaplan H, Greenland P. Prevalence and significance of unrecognized lower extremity peripheral arterial disease in general medicine practice. J Gen Intern Med. 2001;16:384–390. doi: 10.1046/j.1525-1497.2001.016006384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, Browner D. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381–386. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 5.Newman AB, Sutton-Tyrrell K, Vogt MT, Kuller LH. Morbidity and mortality in hypertensive adults with a low ankle/arm blood pressure index. JAMA. 1993;270:487–489. [PubMed] [Google Scholar]
- 6.Johansson SE, Sundquist J. Change in lifestyle factors and their influence on health status and all-cause mortality. Int J Epidemiol. 1999;28:1073–1080. doi: 10.1093/ije/28.6.1073. [DOI] [PubMed] [Google Scholar]
- 7.Andersen LB, Schnohr P, Schroll M, Hein HO. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch Intern Med. 2000;160:1621–1628. doi: 10.1001/archinte.160.11.1621. [DOI] [PubMed] [Google Scholar]
- 8.Dorn JP, Cerny FJ, Epstein LH, Naughton J, Vena JE, Winkelstein W, Jr, Schisterman E, Trevisan M. Work and leisure time physical activity and mortality in men and women from a general population sample. Ann Epidemiol. 1999;9:366–373. doi: 10.1016/s1047-2797(99)00025-3. [DOI] [PubMed] [Google Scholar]
- 9.Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 10.Fang J, Wylie-Rosett J, Cohen HW, Kaplan RC, Alderman MH. Exercise, body mass index, caloric intake, and cardiovascular mortality. Am J Prev Med. 2003;25:283–289. doi: 10.1016/s0749-3797(03)00207-1. [DOI] [PubMed] [Google Scholar]
- 11.Oguma Y, Sesso HD, Paffenbarger RS, Jr, Lee IM. Physical activity and all cause mortality in women: a review of the evidence. Br J Sports Med. 2002;36:162–172. doi: 10.1136/bjsm.36.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaplan GA, Strawbridge WJ, Cohen RD, Hungerford LR. Natural history of leisure-time physical activity and its correlates: associations with mortality from all causes and cardiovascular disease over 28 years. Am J Epidemiol. 1996;144:793–797. doi: 10.1093/oxfordjournals.aje.a009003. [DOI] [PubMed] [Google Scholar]
- 13.Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. Characteristics of leisure time physical activity associated with decreased risk of premature all-cause and cardiovascular disease mortality in middle-aged men. Am J Epidemiol. 1996;143:870–880. doi: 10.1093/oxfordjournals.aje.a008830. [DOI] [PubMed] [Google Scholar]
- 14.McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, Chan C, Martin GJ, Schneider J, Pearce WH, Taylor LM, Clark E. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med. 2002;136:873–883. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- 15.Gardner AW, Poehlman ET. Exercise rehabilitation programs for the treatment of claudication pain: a meta-analysis. JAMA. 1995;274:975–980. [PubMed] [Google Scholar]
- 16.McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR, Sharma L, Clark E, Gibson D, Martin GJ. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 17.McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, Chan C, Pearce WH, Schneider JR, Ferrucci L, Celic L, Taylor LM, Vonesh E, Martin GJ, Clark E. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–461. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 18.McDermott MM, Criqui MH, Liu K, Guralnik JM, Greenland P, Martin GJ, Pearce W. Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32:1164–1171. doi: 10.1067/mva.2000.108640. [DOI] [PubMed] [Google Scholar]
- 19.Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on the prevalence of peripheral arterial disease: the San Luis Valley Diabetes Study. Circulation. 1995;91:1472–1479. doi: 10.1161/01.cir.91.5.1472. [DOI] [PubMed] [Google Scholar]
- 20.Guralnik J, Fried LP, Simonsick EM, Kaspar JD, Lafferty ME, editors. The Women’s Health and Aging Study: Health and Social Characteristics of Older Women with Disability. Bethesda, Md: National Institute on Aging, National Institutes of Health; 1995. [Google Scholar]
- 21.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–475. [PubMed] [Google Scholar]
- 22.Sugiuchi H, Uji Y, Okabe H, Irie T, Uekama K, Kayahara N, Miyauchi K. Direct measurement of high-density lipoprotein cholesterol in serum with polyethylene glycol-modified enzymes and sulfated alpha-cyclodextrin. Clin Chem. 1995;41:717–723. [PubMed] [Google Scholar]
- 23.Criqui MH, Denenberg JO, Bird CE, Fronek A, Klauber MR, Langer RD. The correlation between symptoms and non-invasive test results in patients referred for peripheral arterial disease testing. Vasc Med. 1996;1:65–71. doi: 10.1177/1358863X9600100112. [DOI] [PubMed] [Google Scholar]
- 24.Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46:706–711. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- 25.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson MT, Leon AS, Jacobs DR, Jr, Ainsworth BE, Serfass R. Ability of the Caltrac accelerometer to assess daily physical activity levels. J Cardiopulm Rehabil. 1995;15:107–113. doi: 10.1097/00008483-199503000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Miller DJ, Freedson PS, Kline GM. Comparison of activity levels using the Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc. 1994;26:376–382. [PubMed] [Google Scholar]
- 28.Sallis JF, Buono MJ, Roby JJ, Carlson D, Nelson JA. The Caltrac accelerometer as a physical activity monitor for school-age children. Med Sci Sports Exerc. 1990;22:698–703. doi: 10.1249/00005768-199010000-00023. [DOI] [PubMed] [Google Scholar]
- 29.Swan PD, Byrnes WC, Haymes EM. Energy expenditure estimates of the Caltrac accelerometer for running, race walking, and stepping. Br J Sports Med. 1997;31:235–239. doi: 10.1136/bjsm.31.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDermott MM, Liu K, O’Brien E, Guralnik JM, Criqui MH, Martin GJ, Greenland P. Measuring physical activity in peripheral arterial disease: a comparison of two physical activity questionnaires with an accelerometer. Angiology. 2000;51:91–100. doi: 10.1177/000331970005100201. [DOI] [PubMed] [Google Scholar]
- 31.McDermott MM, Ohlmiller SM, Liu K, Guralnik JM, Martin GJ, Pearce WH, Greenland P. Gait alterations associated with walking impairment in people with peripheral arterial disease with and without intermittent claudication. J Am Geriatr Soc. 2001;49:747–754. doi: 10.1046/j.1532-5415.2001.49151.x. [DOI] [PubMed] [Google Scholar]
- 32.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 33.Lu K, Tsiatis AA. Multiple imputation methods for estimating regression coefficients in the competing risks model with missing cause of failure. Biometrics. 2001;57:1191–1197. doi: 10.1111/j.0006-341x.2001.01191.x. [DOI] [PubMed] [Google Scholar]
- 34.Falcone RA, Hirsch AT, Regensteiner JG, Treat-Jacobson D, Williams MA, Hiatt WR, Stewart KJ. Peripheral arterial disease rehabilitation: a review. J Cardiopulm Rehabil. 2003;23:170–175. doi: 10.1097/00008483-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Regensteiner JG. Exercise rehabilitation for the patient with intermittent claudication: a highly effective yet underutilized treatment. Curr Drug Targets Cardiovasc Haematol Disord. 2004;4:233–239. doi: 10.2174/1568006043336195. [DOI] [PubMed] [Google Scholar]
- 36.McDermott MM, Liu K, Guralnik JM, Mehta S, Criqui MH, Martin GJ, Greenland P. The ankle brachial index independently predicts walking velocity and walking endurance in peripheral arterial disease. J Am Geriatr Soc. 1998;46:1355–1362. doi: 10.1111/j.1532-5415.1998.tb06001.x. [DOI] [PubMed] [Google Scholar]
- 37.Sieminski DJ, Gardner AW. The relationship between free-living daily physical activity and the severity of peripheral arterial occlusive disease. Vasc Med. 1997;2:286–291. doi: 10.1177/1358863X9700200402. [DOI] [PubMed] [Google Scholar]