Abstract
Nephron-sparing surgery can permit functional preservation of the kidney in carefully selected patients. We report nephron-sparing surgery in two patients with renal tumours ≥ 5 cm. Both patients were successfully treated, with kidney salvage facilitated through the use of the fibrinogen- and thrombin-coated collagen sponge, TachoSil® (Nycomed UK Ltd, UK).
Keywords: Kidney, Nephron, Neoplasm, Nephrectomy, Haemostatic techniques
Surgical resection is the only effective therapy for renal cell carcinoma.1 Radical nephrectomy is considered the gold standard curative technique for tumour excision.2 However, with advances in renal imaging and improved surgical techniques, nephron-sparing surgery is emerging as a successful treatment option for selected patients with renal cell carcinoma.1,2 The absolute indications for nephron-sparing surgery are those where radical nephrectomy would cause the patient to be either anatomically or functionally anephric with subsequent need for dialysis.3 This includes patients with bilateral tumours, tumours in a solitary kidney or significant renal failure.3 Nephron-sparing surgery, therefore, not only represents an alternative to renal replacement therapy, but also significantly reduces the cost burden to the NHS, and greatly improves patient quality of life.1,4
The performance of nephron-sparing surgery, however, can be technically challenging.1 Haemorrhage is a major complication of surgery and current techniques such as renal occlusion, electrocautery, argon beam coagulation and sutures may be insufficient to prevent haemorrhage or may even induce further damage.5 The use of advanced tools to ensure haemostasis and prevent the need for renal occlusion greatly reduces the risk of renal failure.5
The TachoSil® patch provides such a tool, consisting of an absorbable collagen sponge, coated with human fibrinogen and thrombin, facilitating sealing and haemostatic wound dressing.6 TachoSil® is the first fibrin sealant to be licensed in the UK, developed as a third generation product from TachoComb and TachoComb H, containing purely human coagulation factor components.7 Interestingly, TachoSil® does not contain bovine apoprotein because non-clinical studies of stress and hyperfibrinolytic conditions indicate that apoprotein is not necessary for efficacious haemostasis and tissue sealing, as well as allowing the elimination of the last remaining bovine substance. However, as with any protein product, allergic type hypersensitivity reactions, although rare, are possible.7–9 Care has to be taken to use the correct amount of saline to moisten TachoSil® before application, and surgeons have to take extra care not to have blood on their gloves when applying pre-moistened TachoSil® in situ due to the strong affinity of collagen to blood.9
We report two cases where nephron-sparing surgery was performed to preserve as much functioning parenchyma as possible. In both cases, TachoSil® was used as a supportive treatment in surgery to enhance haemostasis and promote optimal wound healing.
Case report 1
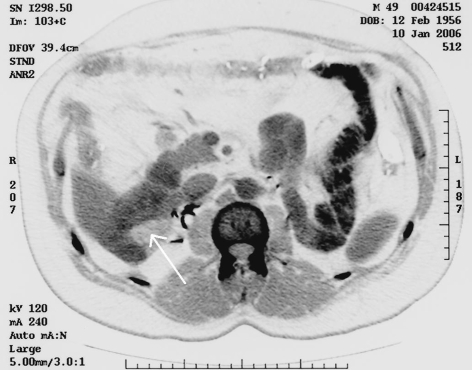
A 49-year-old man with suspected bilateral renal cell carcinoma had a computerised tomography (CT) scan to determine tumour size, depth and extension into the parenchyma. On imaging, a 6-cm diameter tumour on the right kidney (Fig. 1A) and an 11-cm diameter tumour on the left kidney were detected. Without successful functional preservation of the right kidney, the patient would face dialysis and renal transplantation. Following pre-operative evaluation, the patient underwent nephron-sparing surgery of the right kidney, and a tumour 6.5 cm in diameter was excised. Primary control of haemorrhage was ensured by temporary occlusion of the renal vessels using vascular clamps. Ice-slush cooling was used for 30 min. A ‘rolled-up’ surgical bolster was applied to the parenchymal surface of the kidney along with one sheet of TachoSil® to enhance haemostasis (Fig. 1B) which was achieved almost immediately. Bleeding points from the calyces were controlled with 4/0 Vicryl sutures while monopolar diathermy forceps were used to control smaller bleeding points. The operation lasted 85 min and was uneventful. The patient did not require an intra- or postoperative blood transfusion. A surgical drain was inserted and removed 5 days postoperatively. Creatinine levels at baseline were 130 μmol/l and remained stable following the first procedure. Six weeks after nephron-sparing surgery of the right kidney, the patient underwent successful radical nephrectomy of the left kidney. Postoperative serum creatinine levels were 170 μmol/l. The patient's recovery was uneventful and he was discharged from hospital 1 week after the operation. A follow-up CT scan at 9 months did not show tumour recurrence in the right kidney.
Figure 1.
(A) CT scan of the right kidney prior to surgery demonstrating the location of a 6-cm tumour. (B) CT scan of the right kidney post-surgery demonstrating the placement of TachoSil®. TachoSil® has a unique radiological density that should not be confused with other body tissue densities such as fat, fluid and muscle.
Case report 2
An 80-year-old man was admitted to hospital with renal cell carcinoma and multiple co-morbidities, including heart failure. A pre-operative CT scan revealed a 5-cm diameter tumour on the left kidney (Fig. 2A). Both kidneys were partially functioning. Nephron-sparing surgery was performed and the operation proceeded successfully. Primary haemostasis was achieved by short (< 30 min) clamping of the renal vessels; therefore, cooling was not used. A surgical bolster along with one sheet of TachoSil® were applied to augment haemostasis and reduce the risk of postoperative bleeding (Fig. 2B). Haemostasis was achieved immediately. Vicryl 4/0 sutures were used to control calyceal bleeding and monopolar diathermy forceps for other minor bleeding. The operation lasted for 90 min. The patient did not require blood transfusion. A surgical drain was left in situ for 4 weeks as result of a continuous serous fluid drainage proved on drain fluid biochemistry. The patient was discharged in a good condition, and follow-up assessment by CT at 4 months showed soft tissue thickening consistent with postoperative changes. Tests of renal function showed creatinine levels had returned to baseline levels of 160 μmol/l within 3 months of surgery.
Figure 2.
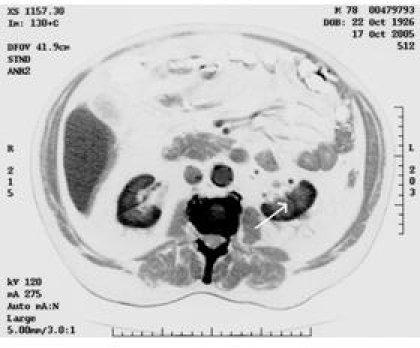
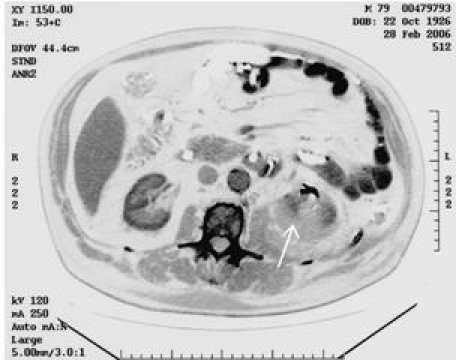
(A) CT scan of the left kidney prior to surgery demonstrating the location of a 5-cm tumour. (B) CT scan of the left kidney post-surgery demonstrating the placement of TachoSil®.
Discussion
Haemorrhage is the most common complication of nephron-sparing surgery in the early postoperative period and occurs more frequently in imperative resections.3 While the majority of complications can be managed conservatively, intrarenal bleeding can result in life-threatening hypotension and shock; in these cases, open surgical exploration is the only solution and renal preservation may be compromised.1
TachoSil®, a ready-to-use haemostatic sponge coated with thrombin and fibrinogen, is indicated for use in surgery when standard techniques are insufficient.9 There is strong evidence supporting the use of TachoSil® in kidney surgery.10,11 Comparator products such as FloSeal,12,13 Quixil14,15 and Beriplast P16,17 are supported by evidence in other areas of surgery, but TachoSil® is the only product supported by randomised controlled trials in the kidney surgery setting. Randomised controlled trials have also shown the effectiveness of TachoSil® in liver7 and lung18 surgery. In addition, a prospective observational cost–benefit analysis of the impact of the use of TachoSil® in a variety of surgical settings on operating time, length of hospital stay, transfusions required, and resource use was performed in 185 centres in Germany. The data revealed a cost reduction of ₠531 per patient, whilst resource use through administration of TachoSil® or its precursor, TachoComb®, amounted to approximately ₠257.8 We report two cases where nephron-sparing surgery was performed successfully with excellent outcomes. In both cases, follow-up revealed no local tumour recurrence and stable renal function. The efficacy of nephron-sparing surgery is often reported in relation to small, < 4 cm, low-stage localised renal cell cancers.19 However, we report the successful performance of nephron-sparing surgery for the excision of tumours ≥ 5 cm. Pre-operatively, both patients had limited kidney function; consequently, renal preservation and even survival were not assured. In both cases, the application of TachoSil® achieved rapid intra-operative haemostasis, promoted wound healing, reduced postoperative bleeding, and facilitated the preservation of renal function.
Conclusions
To our knowledge, these are the first case studies to report the successful use of TachoSil® in patients undergoing critical nephron-sparing surgery whereby immediate haemostasis was achieved and the risk of postoperative complications reduced. It is anticipated that haemostatic agents such as TachoSil® will play an important role where surgery is performed in vulnerable patients at risk of coagulopathies and other postoperative complications, either alone or as adjunct to standard techniques, as well as enabling cost savings from the healthcare providers' perspective.8
Acknowledgments
The authors gratefully acknowledge Strategen Ltd, for providing writing and editorial support in preparing this manuscript.
References
- 1.Van Poppel H. Nephron sparing surgery in renal cell carcinoma. Braz J Urol. 2000;26:342–53. [Google Scholar]
- 2.Novick AC. Laparoscopic and partial nephrectomy. Clin Cancer Res. 2004;10:6322–7. doi: 10.1158/1078-0432.CCR-050003. [DOI] [PubMed] [Google Scholar]
- 3.Van Poppel H. Conservative vs. radical surgery for renal cell carcinoma. BJU Int. 2004;94:766–8. doi: 10.1111/j.1464-410X.2004.05029.x. [DOI] [PubMed] [Google Scholar]
- 4.Blake C, Codd MB, Cassidy A, O'Meara YM. Physical function, employment and quality of life in end-stage renal disease. J Nephrol. 2000;13:142–9. [PubMed] [Google Scholar]
- 5.Triaca V, Zagha RM, Libertino JA. Does thrombin sealant allow nephron-sparing surgery with no renal artery occlusion? A description of technique and initial results. BJU Int. 2005;95:1273–5. doi: 10.1111/j.1464-410X.2005.05517.x. [DOI] [PubMed] [Google Scholar]
- 6.Haas S. The use of a surgical patch coated with human coagulation factors in surgical routine: a multicenter postauthorization surveillance. Clin Appl Thromb Hemost. 2006;12:445–50. doi: 10.1177/1076029606293420. [DOI] [PubMed] [Google Scholar]
- 7.Frilling A, Staveou GA, Mischinger HJ, de Hemptinne B, Rokkjaer M, Klempnauer J, et al. Effectiveness of a new carrier-bound fibrin sealant versus argon beamer as haemostatic agent during liver resection: a randomized prospective trial. Langenbecks Arch Surg. 2005;390:114–20. doi: 10.1007/s00423-005-0543-x. [DOI] [PubMed] [Google Scholar]
- 8.Kallinowski F, Pfeil T, Ulbrich W. Quality management in surgical intervention – a prospective outcomes research study of fleece-bound tissue gluing (TachoSil®) Gesundh ökon Qual Manag. 2005;10:151–9. [Google Scholar]
- 9.TachoSil. Summary of Product Characteristics. 2005.
- 10.Seimer S, Lahme S, Altzieber S, Machtens S, Strohmaier W, Wechsel HW, et al. Efficacy and safety of Tachosil as haemostatic treatment versus standard suturing in kidney tumour resection: a randomised prospective trial. Eur Urol. 2007;52:1156–63. doi: 10.1016/j.eururo.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 11.Van Poppel H, Siemer S, Lahme S, Altziebler S, Machtens S, Strohmaier W, et al. Kidney tumour resection with use of TachoSil® as haemostatic treatment. Presented at the European Association of Urology Annual Congress; 5–8 April 2006; France. [Google Scholar]
- 12.Mathiasen RA, Cruz RM. Prospective, randomised, controlled clinical trial of a novel matrix hemostatic sealant in children undergoing adenoidectomoy. Otolaryngol Head Neck Surg. 2004;131:601–5. doi: 10.1016/j.otohns.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 13.Oz MC, Cosgrove DM, 3rd, Badduke BR, Hill JD, Flannery MR, Palumbo R, et al. Controlled clinical trial of a novel hemostatic agent in cardiac surgery. The Fusion Matrix Study Group. Ann Thorac Surg. 2000;69:1376–82. doi: 10.1016/s0003-4975(00)01194-2. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz M, Madariaga J, Hirose R, Shaver TR, Sher L, Chari R, et al. Comparison of a new fibrin sealant with standard topical hemostatic agents. Arch Surg. 2004;139:1148–54. doi: 10.1001/archsurg.139.11.1148. [DOI] [PubMed] [Google Scholar]
- 15.Vaiman M, Evitar E, Segal S. The use of fibrin glue as hemostatic in endonasal operations: a prospective, randomised study. Rhinology. 2002;40:185–8. [PubMed] [Google Scholar]
- 16.Taylor LM, Mueller-Velten G, Koslow A, Hunter G, Naslund T, Kline R, Beriplast B Investigators Prospective randomized multicenter trial of fibrin sealant versus thrombin-soaked gelatin sponge for suture- or needle-hole bleeding from polytetrafluoroethylene femoral artery grafts. J Vasc Surg. 2003;38:766–71. doi: 10.1016/s0741-5214(03)00474-9. [DOI] [PubMed] [Google Scholar]
- 17.Codispoti M, Mankad PS. Significant merits of a fibrin sealant in the presence of coagulopathy following paediatric cardiac surgery: randomised controlled trial. Eur J Cardiothorac Surg. 2002;22:200–5. doi: 10.1016/s1010-7940(02)00271-3. [DOI] [PubMed] [Google Scholar]
- 18.Lang G, Csekeö A, Stamatis G, Lampl L, Hagman L, Marta GM, et al. Efficacy and safety of topical application of human fibrinogen/thrombin coated collagen patch (TachoComb) for treatment of air leakage after standard lobectomy. Eur J Cardiothorac Surg. 2004;25:160–6. doi: 10.1016/j.ejcts.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Richter F, Schnorr D, Deger S, Trk I, Roigas J, Wille A, et al. Improvement of hemostasis in open and laparoscopically performed parital nephrectomy using a gelatin matrix-thrombin tissue sealant (FloSeal) Urology. 2003;61:73–7. doi: 10.1016/s0090-4295(02)02143-x. [DOI] [PubMed] [Google Scholar]