Abstract
A 34-year-old woman with cystic fibrosis presented with bilateral femoral hernias, which were found to be retrovascular at operation. The hernias were not amenable to conventional open or laparoscopic repair, and were repaired using pre-peritoneal mesh inserted deep to transversalis fascia. The anatomical basis and management of uncommon variants of femoral hernia are discussed.
Keywords: Femoral hernia, Prosthesis
Femoral hernias are common in patients with a chronic cough, and their repair has been well described. We report a case of bilateral prevascular femoral hernias in a young woman with cystic fibrosis, and discuss its anatomical basis and management.
Case report
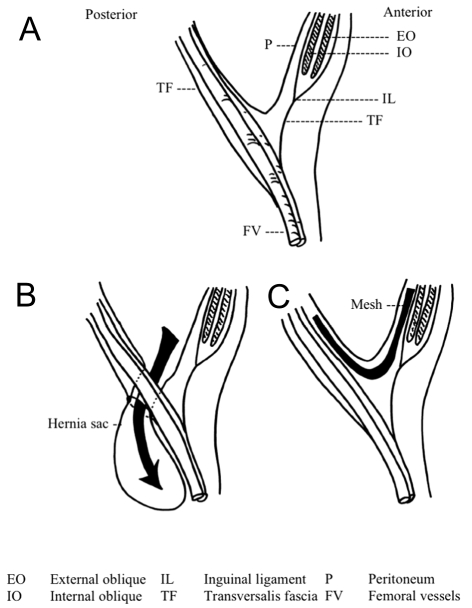
A 34-year-old woman presented with bilateral groin swellings. Past history included cystic fibrosis that had resulted in recurrent chest sepsis and chronic respiratory insufficiency. Physical examination revealed bilateral groin swellings with positive cough impulses, located below and lateral to the pubic tubercles, consistent with femoral hernias. Due to poor respiratory function, she was considered unfit for general anaesthetic, and underwent bilateral groin exploration under spinal anaesthesia. At operation, she was found to have bilateral retrovascular femoral hernias. The necks of the hernial sacs were located immediately posterior to the femoral vessels and were, therefore, not amenable to anterior mesh repair. Each hernia was repaired using a prolene mesh inserted preperitoneally via an incision in transversalis fascia in the inguinal canal (Fig. 1). She made a good postoperative recovery and there was no evidence of recurrence at 6-month follow-up.
Figure 1.
Anatomy of the inguinal and femoral regions. (A) Transversalis fascia becomes continuous with the femoral sheath both anteriorly and posteriorly and prevascular and retrovascular hernias develop at a point of weakness of this fascia. (B) In the presented case, a prosthetic mesh was inserted into the preperitoneal space via an incision in transversalis fascia within the inguinal canal. (C) After reducing the hernial sac, the mesh was positioned across the defect and anchored above by suturing it to transversalis fascia.
Discussion
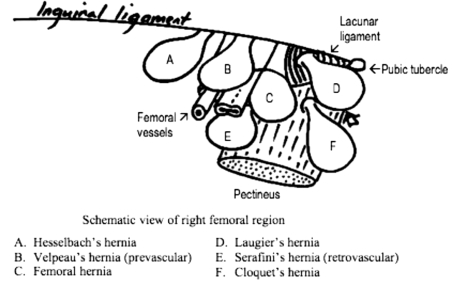
A femoral hernia is a protrusion of pelvic peritoneum through the femoral canal, and is usually located medial to the femoral vessels. The neck of the femoral canal (femoral ring) is formed by rigid structures medially, anteriorly and posteriorly (lacunar ligament, inguinal ligament and pectineal fascia, respectively), which predisposes femoral hernias to the risks of strangulation and obstruction. Rarely, a femoral hernia may arise in different locations (Fig. 2), developing through the lacunar ligament (Laugier's hernia), through the pectineal fascia (Cloquet's hernia), or in relation to the femoral vessels – lateral (Hesselbach's hernia), prevascular (Velpeau's hernia) or retrovascular (Serafini's hernia).1 Diagnosis of these variants may not be possible pre-operatively due to their rarity and similar clinical appearance to conventional femoral hernias. Although a retrovascular femoral hernia has been described in the past, there have been no recent reports. Abdominal wall hernias are well recognised in patients with a chronic cough and respiratory disorders, and presumably this was the precipitating factor in this case. The presence of the same defect bilaterally in the same patient is interesting, and suggests that there may have been a congenital weakness in transversalis fascia in the region of the femoral vessels.2 Indeed, it has been previously suggested that femoral hernias may develop from a congenital peritoneal diverticulum,1 although the evidence for this is not convincing.
Figure 2.
Schematic view of right femoral region illustrating variants of femoral hernia. (A) Hesselbach's hernia; (B) Velpeau's hernia (prevascular); (C) femoral hernia; (D) Laugier's hernia; (E) Serafini's hernia (retrovascular); and (F) Cloquet's hernia.
The most commonly used operative approaches for repairing conventional femoral hernias is either via a vertical or transverse incision.3 The hernial sac is mobilised and reduced, and the femoral canal is then obliterated either by suturing the inguinal ligament to pectineal fascia, or by using a prosthetic mesh.3 The surgical management of prevascular or retrovascular hernias is more challenging, and requires a thorough knowledge of the anatomy of the inguinal and femoral regions. It is important to appreciate that transversalis fascia becomes continuous with the femoral sheath both anteriorly and posteriorly (Fig. 1), and that prevascular and retrovascular hernias develop at a point of weakness of this fascia (Fig. 1).4 The approach to the repair of pre- and retrovascular hernias is, therefore, markedly different from conventional femoral hernia repairs.5 In the presented case, a prosthetic mesh was inserted into the preperitoneal space via an incision in transversalis fascia within the inguinal canal. After reducing the hernial sac, the mesh was positioned across the defect and anchored above by suturing it to transversalis fascia (Fig. 1). In theory, laparoscopic repair of a retrovascular hernia may be possible, but was contra-indicated in this case due to the risks associated with general anaesthesia and pneumoperitoneum.
General surgeons should be alert to the possibility of rare variants of femoral hernia when examining patients with groin swellings, since the operative approach may need to be modified. Care must be taken to determine the precise location of the cough impulse, and its relationship to adjacent anatomical structures, particularly the femoral vessels. If the diagnosis of retrovascular femoral hernia is made intra-operatively, the surgeon should make no attempt to repair it via an infra-inguinal approach, due to the risk of neurovascular injury. Instead, we recommend using a trans-inguinal approach, via the same skin incision (extending it if required), incising transversalis fascia and proceeding with the repair as described above.
Conclusions
Although rarely encountered, pre- and retrovascular femoral hernias are important to recognise since repair of these variants may present a challenge to the inexperienced surgeon. A thorough understanding of the anatomical relations within the inguinal region is essential, and repair can be achieved using a pre-peritoneal mesh with good results.
References
- 1.Keynes G. Prevascular femoral hernia. Br J Surg. 1932;20:55–7. [Google Scholar]
- 2.Cox KR. Bilateral pre-vascular femoral hernia. Aust NZ J Surg. 1962;31:318–21. doi: 10.1111/j.1445-2197.1962.tb03279.x. [DOI] [PubMed] [Google Scholar]
- 3.Hachisuka T. Femoral hernia repair. Surg Clin North Am. 2003;83:1189–205. doi: 10.1016/S0039-6109(03)00120-8. [DOI] [PubMed] [Google Scholar]
- 4.Moschcowitz AV. Prevascular femoral hernia. Ann Surg. 1912;4:848–56. doi: 10.1097/00000658-191206000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams GL, Riddell A, Coulston J, Frost B, Stephenson BM. Prosthetic repair of prevascular femoral herniation. Hernia. 2007;11:513–5. doi: 10.1007/s10029-007-0263-y. [DOI] [PubMed] [Google Scholar]