Abstract
Background
Low levels of high density lipoprotein cholesterol (HDL-C) are associated with increased incidence of coronary heart disease (CHD). A better understanding of the mechanisms leading to low HDL-C and CHD is essential for planning treatment strategies. Clinical studies have demonstrated that cytokines might affect both concentration and composition of plasma lipoproteins, including HDLs.
Methods
We investigated the possible association between low HDL-C levels, defined as ≤10th gender specific percentile, and circulating markers of inflammation (IL-1β, TNF-α, IL-6, IL-10, IL-18, and CRP) in a population of 1044 community dwelling older Italian subjects from the InChianti study.
Results
Using logistic regression analysis we demonstrated that IL-6 levels (III versus I tertile, OR: 2.10; 1.10–3.75), TG (III versus I tertile OR: 27.45; 8.47–88.93), fasting insulin (III versus I tertile OR: 2.84; 1.50–5.42), and age (OR: 1.038; 1.002–1.075) were associated with low HDL-C independent of smoking, BMI, waist circumference, hypertension, diabetes, physical activity, alcohol intake, oral hypoglycaemics, CRP, IL-18, and TNF-α levels. The adjusted attributable risk of low HDL-C in the exposed group (III tertile of IL-6) was 54%.
Conclusions
The present study provides the epidemiological evidence that besides triglycerides, fasting insulin, and age, IL-6 is one of the main correlates of low HDL-C levels in older individuals.
Keywords: HDL-cholesterol, Inflammation, Interleukin 6, Metabolic syndrome
1. Introduction
Large epidemiological studies have shown that low plasma levels of high density lipoprotein cholesterol (HDL-C) are associated with increased incidence of coronary heart disease (CHD) [1,2]. It has been also reported that low HDL-C levels represent one of the most prevalent lipid abnormality in the subjects affected by CHD [3,4], and unlike high total cholesterol (TC) levels, low HDL-C levels seem to maintain a significant predictive value for CHD in the older population [5]. Therefore, several recent guidelines [6–8] consider low HDL-C levels a strong and independent risk factor for CHD.
The fact that low HDL-C is a powerful predictor of CHD has generated a considerable and growing interest about possible interventions aimed to increase circulating HDL-C levels. Very recently it has been reported that increasing HDL-C by pharmacological and life style interventions helps to prevent the angiographic progression of coronary stenosis and cardiovascular events [9].
Therefore, a better understanding of the pathophysiologic mechanisms leading to low HDL-C levels and eventually to CHD in the population is essential in order to plan effective treatment strategies.
Besides genetics, several conditions may influence HDL-C levels including body composition, smoking habit, alcohol consumption, physical activity, and some alterations of lipid/glucose metabolism such as hypertriglyceridemia and diabetes mellitus [10,11]. Recently, a growing level of attention has been devoted to the relationship between acute phase reaction (APR) and lipid metabolism, since it has been demonstrated that cytokines may affect both concentration and composition of plasma lipoproteins, including high density lipoproteins [12,13].
Low HDL-C is one of the main features of the metabolic syndrome (syndrome X), a frequent pathological condition characterized by the co-occurrence of several risk factors for atherosclerosis and CHD arising from a condition of insulin-resistance [11]. Interestingly, it has been shown that a chronic low inflammatory state, reflected by increased levels of C reactive protein (CRP) or other cytokines, is associated not only with atherosclerosis and cardiovascular disease [14,15], but also with the presence of the metabolic syndrome [16,17]. Noteworthy, the aging process itself is associated with both an increase in the plasma concentration of several pro-inflammatory cytokines [18], and a progressive decrease in plasma HDL-C concentration [19]; nevertheless, the possible co-occurrence of these two phenomena in older age has never been exhaustively investigated in population-based epidemiological studies.
The aim of the present study was to evaluate the relationship between inflammation and HDL-C levels in a large sample of community dwelling older Italian subjects. We focused our attention on the possible association between several circulating markers of inflammation and low HDL-C levels, accounting for the effect of important confounders including the principal features of the metabolic syndrome.
2. Materials and methods
This study is part of the “Invecchiare in Chianti” (Aging in the Chianti area, InChianti) study, a prospective population-based study of older people, designed by the Laboratory of Clinical Epidemiology of the Italian National Research Council of Aging (INRCA, Florence, Italy).
The study included 1156 older participants (age 65–102 years), randomly selected from residents in two towns of the Chianti area (Greve In Chianti and Bagno a Ripoli, Tuscany, Italy)[20]. The collection of the data started in September 1998 and was completed in March 2000. A detailed description of the sampling procedure and data collection method has been previously published [20]. The Italian National Research Council on Aging (INRCA) Ethical Committee ratified the entire study protocol.
In the present study 1044 individuals aged 65 years and older in which inflammatory markers and plasma lipids had been measured at baseline were included. One hundred and twelve participants could not be included into the present study as they had refused to provide blood sample for analysis at baseline. They were characterized by older age (mean 79.9, S.D. 8.6 years), while no differences in socio-demographic characteristics emerged.
2.1. Markers of inflammation
Blood was drown in the morning after a 12-h fasting, and after the patient has been sedentary in sitting or supine position for at least 15 min. Sampled blood was transferred, making it flowing down the side of the tube, never directly squirted into the center, in order to minimize mechanical disruption or turbulence that may result in haemolysis or activation. After having been aliquoted, serums was frozen and stored at −80 °C till the tests were performed.
IL-6, IL-1β, and TNF-α were quantified with immunoassay kits (BioSource Cytoscreen human IL-6 and human TNF-α UltraSensitive kits). The minimum detectable concentrations were 0.10, 8, and 0.09 pg/ml, respectively. The interassay coefficient of variation was 7% for all three kits.
Serum interleukin 10 (IL-10) was detected by Human IL10 CytoSETS TM ELISA kits (BIOSOURCE Internetional Inc., Camarillo, CA, USA). The minimum detectable concentration was 1.00 pg/ml; the inter-assay CV was 8.6%.
Serum interleukin 18 (IL-18) level was detected in duplicate using highly sensitive quantitative sandwich assays (ELISA) (Quantikine HS, R&D Systems, Minneapolis, MN). The lower limits of detection were 0.7 pg/mL; the coefficient of variation for IL-18 test was approximately 7%. Determination of CRP level was based on a high sensitivity enzyme-linked immunosorbent assay, a competitive immunoassay that uses purified protein and polyclonal anti-CRP antibodies. The interassay CV was 5.0%. The minimum detectable concentration was 0.03 mg/L.
All assays were done in duplicate (except IL-10) and were repeated if the second measure was >10% or <10% compared to the first. The average of the two measures was used in the analyses. The cut-off values for tertiles distribution (pg/ml) for each of the cytokines considered in the study was the following:
- IL-6: I <1.06; II 1.06–1,91; III >1.91;
- IL-10: I <1. 39; II 1.39–2.49; III >2.49;
- IL-18: I <332; II 332–442; III >442;
- IL-1β: I <0.12; II 0.12–0.16; III >0.16;
- TNFα: I <3.51; II 3.51–5.74; III >6.74;
- CRP: I <1.68; II 1.68–4.49; III >4.49.
2.2. Other clinical chemistry parameters
All parameters were measured on serum from fresh samples (not frozen) drawn after 12 h overnight fasting. Commercial enzymatic tests (Roche Diagnostics) were used for determining serum total cholesterol (TC), triglycerides (TG), and HDL-C concentrations. The interassay coefficient of variation was less than 3.8% for total cholesterol and less than 5.0% for HDL cholesterol.
For triglycerides, the analytical sensitivity (lower detection limit) was 4.0 mg/dL; the intra-assay CV was 3.1%, the inter-assay CV was 1.8%.
Low-density lipoprotein cholesterol (LDL-C) was calculated by the Friedewald's formula as follows: LDL-C: TC – (TG/5) – HDL-C. Low HDL-C was defined as ≤10th gender specific percentile (36 mg/dL for males, 41 mg/dL for females).
Fasting insulin was determined using a commercial double-antibody, solid-phase radioimmunoassay (Sorin Biomedica, Milan, Italy) with an intra-assay coefficient of 3.1%. Fasting blood glucose was determined by an enzymatic colorimetric assay using a modified glucose oxidase-peroxidase method (Roche Diagnostics, GmbH, Mannheim, Germany) and a Roche-Hitachi 917 analyzer.
2.3. Other covariates
Weight and height were measured by using standard techniques. Body mass index (BMI) was calculated as weight (kg) divided by the square of height (m). Waist circumference was measured to the nearest 0.5 cm by using a non-elastic plastic tape, at the midpoint between the lower rib margin and the iliac crest (normally umbilical level).
Daily alcohol intake (expressed in g/day) was calculated by using a specific food questionnaire validated in the Italian population (EPIC questionnaire) [21].
Physical activity was assessed from self-report of recreational and work-related activities. For each activity, we estimated the metabolic equivalent tasks (METs), frequency (times per month), and time of exposure (years), and calculated the average METs consumed per year from the age of 60.
The presence of specific diseases was established by standardized criteria combining information obtained from self-reported history, medical records, and from clinical examination. The following diseases were assessed in this study: angina, acute myocardial infarction, peripheral arterial disease, stroke and transient ischemic attack, arterial hypertension, congestive heart failure, renal insufficiency, cancer, and dementia.
All participants were asked about smoking habits and pack-years (measure that combines intensity and duration) was calculated as packs smoked per day × years of smoking.
Drugs were coded according to the Anatomical Therapeutic and Chemical codes. The medications considered in the present study were: insulin, hypoglycemics, statins, fibrates, and beta-blockers.
Systolic and diastolic blood pressures were calculated from the mean of the three measures taken during physical examination. Hypertension was defined as the presence of at least one of the following conditions: systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg; documented history of hypertension; current use of antihypertensive drugs. Diabetes mellitus was defined as the presence of at least one of the following conditions: previous physician's diagnosis, current treatment with insulin or oral hypoglycemics, self-report of diabetes mellitus, and fasting blood glucose ≥ 126 mg/dL.
2.4. Statistical analysis
Continuous variables were expressed as mean (S.D.). Due to the skewed distribution, cytokines, TG, and insulin values were log-transformed in order to approximate a normal distribution. Means were compared by the unpaired t-test, while prevalences were compared by the χ2-test.
The association (odds ratio) between low HDL-C levels and each inflammatory marker levels (expressed as tertiles) was evaluated by univariate logistic regression analysis.
In order to select the variables independently associated with low levels of HDL-C we calculated the odds ratio by using a multivariate logistic regression analysis (method: stepwise forward Wald). The independent variables included in the model were the following: age (years), smoking (three categories: current, former, never), alcohol intake (g/day), physical activity (METs per year), hypertension (yes/no), diabetes (yes/no), CHD (yes/no), stroke (yes/no), peripheral arterial disease (PAD: yes/no), plasma triglycerides, fasting insulin, oral hypoglycaemic drugs, BMI, waist circumference, IL-6, CRP, IL-18, and TNF-α levels.
Systat for Windows, version 5.0, and SPSS for Windows, version 7.0 (SPSS, Inc., Chicago, IL) statistical packages were used.
3. Results
The principal characteristics of the sample according to HDL-C groups (low: n 115, normal–high: n 929) are reported in Table 1. Compared to subjects with normal–high HDL-C levels, subjects with low HDL-C levels were characterized by older age, lower TC and LDL-C levels, higher TG (63% had TG > 200 mg/dL), fasting glucose, fasting insulin, BMI, and waist circumference values. No differences in gender distribution or in smoking habits emerged between the two groups.
Table 1.
Principal characteristics of 1044 Italian community dwelling older subjects aged 65–102 years from the InChianti study according to levels of HDL-C
| Whole sample (n 1044) | Low HDL-C (n 115) | Normal–high HDL-C (n 929) | p | |
|---|---|---|---|---|
| Gender (female %) | 57.1 | 56 | 57.3 | 0.44 |
| Age (years) | 75.9 (7.6) | 77.5 (7.2) | 75.2 (8.1) | 0.01 |
| Total cholesterol | 217 (40) | 196 (42) | 220 (39) | 0.01 |
| Triglycerides | 128 (70) | 203 (117) | 119 (55) | 0.01 |
| LDL-C | 136 (34) | 120 (36) | 138 (34) | 0.01 |
| HDL-C | 55.7 (15) | 34.6 (4.6) | 58 (14) | 0.01 |
| Fasting blood glucose | 96 (26) | 103 (36) | 95 (24) | 0.01 |
| Fasting insulin | 11.3 (6.1) | 15.1 (10) | 10.7 (5.2) | 0.01 |
| BMI | 27.4 (4) | 29 (4.6) | 27.2 (3.9) | 0.01 |
| Waist circumference | 93 (10) | 97 (10) | 92 (10) | 0.01 |
| Smokers (%) | ||||
| Current | 10.9 | 11 | 10.8 | |
| Former | 29.7 | 26.1 | 30.5 | |
| Never | 59.4 | 62.6 | 58.8 | 0.60 |
| Daily alcohol intake (g) | 13.7 (19) | 10 (12) | 15 (20) | 0.01 |
| Hypertension (%) | 69.0 | 73.9 | 68.4 | 0.13 |
| Diabetes (%) | 11.7 | 20 | 11 | 0.01 |
| CHD (%) | 7.6 | 8.3 | 7.4 | 0.42 |
| Previous stroke/TIA (%) | 6.6 | 14 | 6 | 0.01 |
| Chronic liver disease (%) | 0.4 | 0.4 | 0.0 | 0.63 |
| Insulin therapy (%) | 1.2 | 3.5 | 1.0 | 0.56 |
| Oral hypoglycemic (%) | 6.7 | 12 | 6 | 0.01 |
| Statins/fibrates (%) | 4.3 | 4.5 | 4.3 | 0.58 |
| Beta-blockers (%) | 3.7 | 5.2 | 3.6 | 0.25 |
As regards to comorbidity, the prevalence of diabetes mellitus and previous TIA/stroke was higher in the low HDL-C compared to the normal HDL-C group, while no differences emerged in the prevalence of CHD, hypertension, and chronic liver diseases.
With respect to pharmacological therapy, subjects with low HDL-C were more frequently treated with oral hypoglycaemic drugs, while no differences in the prescription of insulin, statins/fibrates, and beta-blockers were found between the two groups.
The correlations between markers of inflammation, metabolic parameters and anthropometrics with HDL-C levels are reported in Table 2. HDL-C was negatively correlated with IL-6, IL-18, IL-1β, CRP, TG, fasting blood glucose, fasting insulin, BMI, and waist circumference values, and positively correlated with TC levels. On the contrary, HDL-C was not significantly correlated with IL-10, TNF-α, and LDL-C plasma levels.
Table 2.
Correlations between markers of inflammation, metabolic parameters and anthropometrics with HDL-C plasma levels in 1044 Italian community dwelling older subjects aged 65–102 years from the InChianti study
| HDL-C | p | |
|---|---|---|
| IL-6 | −0.23 | 0.01 |
| IL-10 | 0.01 | 0.76 |
| IL-18 | −0.25 | 0.01 |
| IL-1β | −0.09 | 0.01 |
| TNF-α | −0.04 | 0.68 |
| CRP | −0.22 | 0.01 |
| TC | 0.28 | 0.01 |
| LDL-C | 0.05 | 0.73 |
| TG | −0.44 | 0.01 |
| GLUC | −0.12 | 0.01 |
| INS | −0.13 | 0.01 |
| BMI | −0.23 | 0.01 |
| WAIST | −0.33 | 0.01 |
TC, total cholesterol; TG, triglycerides; GLUC, fasting plasma glucose; INS, fasting insulin; BMI, body mass index.
After adjusting for age, the logistic regression analysis-showed that IL-6 (III tertile versus I tertile, OR: 3.24; 95% CI: 1.91–5.47), IL-18 (III tertile versus I tertile, OR: 2.30; 95% CI: 1.39–3.81), TNF-α (III tertile versus I tertile, OR: 1.75; 95% CI: 1.09–2.81), and CRP (III tertile versus I tertile, OR: 2.98; 95% CI: 1.77–4.99) were significantly associated with low HDL-C (Table 3).
Table 3.
Age-adjusted association between acute phase markers and gender specific low HDL-C levels in a sample of 1044 community dwelling older Italian subjects aged 65–102 years from the InChianti study
| Variable | Odds ratio | 95% CI |
|---|---|---|
| Interleukin 6 | ||
| • I tertile (<1.06 pg/ml) | 1 | – |
| • II tertile (1.06–1.91 pg/ml) | 1.18 | 0.65–2.13 |
| • III tertile (>1.91 pg/ml) | 3.24 | 1.91–5.47 |
| Interleukin 10 | ||
| • I tertile (<1.39 pg/ml) | 1 | – |
| • II tertile (1.39–2.49 pg/ml) | 0.81 | 0.45–1.48 |
| • III tertile (>2.49 pg/ml) | 0.69 | 0.44–1.08 |
| Interleukin 18 | ||
| • I tertile (<332 pg/ml) | 1 | – |
| • II tertile (332–442 pg/ml) | 1.39 | 0.81–2.39 |
| • III tertile (>442 pg/ml) | 2.30 | 1.39–3.81 |
| Interleukin 1-β | ||
| • I tertile (<0.12 pg/ml) | 1 | – |
| • II tertile (0.12–0.16 pg/ml) | 1.41 | 0.87–2.30 |
| • III tertile (>0.16 pg/ml) | 1.57 | 0.95–2.58 |
| TNF-α | ||
| • I tertile (<3.51 pg/ml) | 1 | – |
| • II tertile (3.51–6.74 pg/ml) | 1.08 | 0.64–1.81 |
| • III tertile (>6.74 pg/ml) | 1.75 | 1.09–2.81 |
| CRP | ||
| • I tertile (<1.68 pg/ml) | 1 | – |
| • II tertile (1.68–4.49 pg/ml) | 1.46 | 0.82–2.57 |
| • III tertile (>4.49 pg/ml) | 2.98 | 1.77–4.99 |
Results of stepwise multivariate logistic regression analysis are reported in Table 4.
Table 4.
Multivariate logistic regression analysis (forward Wald) for gender specific low HDL-C levels in a sample of 1044 community dwelling older Italian subjects aged 65–102 years from the InChianti study
| Variable | Odds ratio | 95% CI |
|---|---|---|
| IL-6 | ||
| • I tertile | 1 | – |
| • II tertile | 0.89 | 0.46–1.74 |
| • III tertile | 2.10 | 1.09–3.75 |
| Triglycerides | ||
| • I tertile | 1 | – |
| • II tertile | 6.79 | 1.98–23.27 |
| • III tertile | 26.78 | 8.26–86.82 |
| Fasting insulin | ||
| • I tertile | 1 | – |
| • II tertile | 1.59 | 0.79–3.21 |
| • III tertile | 3.01 | 1.57–5.84 |
| Age | 1.03 | 1.001–1.074 |
Variables included into the model: smoking, body mass index, waist circumference, hypertension, diabetes, physical activity, alcohol intake, oral hypoglycaemic drugs, coronary heart disease, stroke, peripheral arterial disease, CRP, IL-18, and TNF-α levels.
IL-6 levels (III versus I tertile, OR: 2.10; 1.10–3.75), TG (II versus I tertile OR: 6.82; 1.99–23.34; III versus I tertile OR: 27.45; 8.47–88.93), fasting insulin (III versus I tertile OR: 2.84; 1.50–5.42), and age (OR: 1.038; 1.0023–1.075) were associated with gender specific low HDL-C levels independent of smoking, BMI, waist circumference, hypertension, diabetes, physical activity, alcohol intake, oral hypoglycaemic drugs, CHD, stroke, PAD, CRP, IL-18, and TNF-α levels.
When the cut-off for low HDL-C defined by NCEP/ATP III (<50 mg/dL in females, <40 in males) was used in the same logistic model, the association between low HDL-C and IL-6 was still significant (III versus I tertile, OR: 1.91; 1.21–2.89).
The prevalence of gender specific low HDL-C levels in the sample divided by IL-6 tertiles is reported in Fig. 1; a significant trend toward an increase in the prevalence of low HDL-C levels from I to III IL-6 tertile was observed (p < 0.001).
Fig. 1.
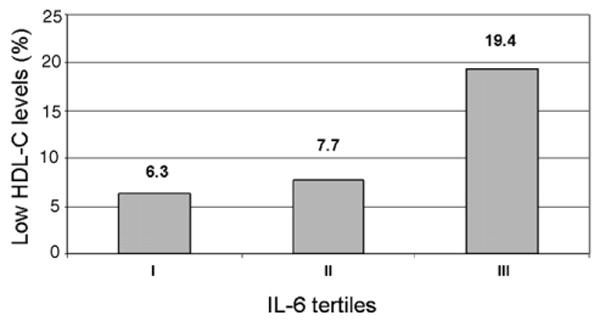
Pervalence of gender specific low HDL-C levels by tertiles of IL-6 in a sample of 1044 community dwelling older Italian subjects aged 65–102 years from the InChianti study.
4. Discussion
In the present study we investigated the possible influence of inflammation on HDL-C levels, strong risk factors for CHD, in a large sample of more than one thousand community-dwelling Italian older adults participating to the InChianti study. The older population is particularly important in terms of prevalence of CHD, as the majority of clinical events occur in this age group. Furthermore, older individuals are more prone to develop both chronic inflammatory conditions and alterations of lipid/glucose metabolism that are potentially able to modify HDL-C levels.
We found that low HDL-C is associated with the presence of high plasma levels of IL-6, independent of the effect of a large number of possible confounders including the main traits of the metabolic syndrome (triglycerides, fasting insulin, diabetes, hypertension, BMI, waist circumference), and life style habits (smoking, alcohol intake, physical activity), that are frequent conditions associated with significant modifications in both HDL-C and IL-6 plasma levels [10,22,23]. To the best of our knowledge, the present study provides the first epidemiological evidence that, in individuals over 65 years of age, IL-6 is one of the factors that independently contribute to low HDL-C levels.
In our sample more than half of the subjects with low HDL-C (58%) had high IL-6 levels, compared with one third of subjects with normal–high HDL-C. Furthermore, the prevalence of low HDL-C progressively increased from 6.3% in I tertile to 7.7% in II tertile to 19.4% in III tertile of the IL-6 distribution (Fig. 1). The crude risk of low HDL-C attributable to IL-6 plasma levels (III tertile compared to I + II tertiles) was 12.4%. By multivariate analysis (see model in Table 4 for covariates) we found that the attributable risk in the exposed group (III tertile IL-6) was 54%; in other words, more than 50% of the cases of low HDL-C may be attributable to the effect of IL-6 in this group of subjects, independent of possible confounders.
The biological plausibility of our results is supported by a number of mechanisms that are known to be involved in the relationship between HDL-C and IL-6 levels.
Interleukin 6, together with other cytokines, might influence HDL-C levels by modifying the activity of the triglycerides lipases. It has been shown that pro-inflammatory cytokines inhibit the activity of lipoprotein lipase (LPL) [24,12], and enhance the lipolytic activity of endothelial lipase (EL) [25,26], Both these actions have been associated with low HDL-C levels during acute or chronic inflammatory states.
Low HDL-C levels might results from the modifications induced by IL-6 and other cytokines in these particles. During APR, high density lipoproteins undergo important changes, acquiring serum amyloid A and losing most of apoprotein A-I and A-II [27,28]; the content in paraoxonase and PAF acetylhydrolase is substantially reduced, while ceruloplasmin tends to increase [29]. Unlike normal HDL particles, high density lipoproteins modified by APR do not display any in vitro anti-inflammatory property, while are converted to pro-inflammatory molecules, perhaps as a consequence of their increased ceruloplasmin content [29]. Furthermore, these structural changes are associated with accelerated HDL clearance leading to low levels [30], reduced affinity for hepatocytes, and increased affinity for macrophages [31,27].
All these observations raise the possibility that in the presence of high IL-6 levels HDL particles might be modified (as reported above) and therefore might contribute to maintain the inflammatory process in a kind of vicious circle.
The hypothesis that IL-6 might influence HDL-C levels is indirectly supported by the recent finding of Popa et al. [32]; these authors found that the treatment of patients affected by rheumatoid arthritis with monoclonal anti-TNF antibodies decreases IL-6 and specifically increases HDL-C plasma levels, while LDL-C and triglycerides levels are not changed [32].
A different but not mutually exclusive possibility is that low levels of HDL-C might contribute to the increase of IL-6 plasma levels either directly or through its relationship with atherosclerosis. As response to stressors (including arterial wall damage) IL-1β and TNF-α stimulate the production of IL-6 which activates the APR. It has been demonstrated that Apo A-I, the principal apoprotein of HDL particles, has a strong anti-inflammatory activity by specifically blocking the contact-mediated activation of monocytes by stimulated T cells, thus inhibiting IL-1β and TNF-α production [33]. In the presence of low HDL-C, and consequently of apo A-I levels, this inhibitory mechanism would be impaired, and the activation of the inflammatory cascade would be easier.
Because of the cross-sectional study, we cannot define any cause–effect relationship; in particular, based on the available data we could not distinguish whether high IL-6 levels causes low HDL-C, low HDL-C levels causes increased plasma concentrations of IL-6, or a third unmeasured factor causes both high IL-6 and low HDL-C.
We propose that a number of factors including aging per se, age-related pathological processes, atherosclerosis, and increased abdominal fat, might produce a chronic proinflammatory state which is reflected by increased circulating levels of IL-6. This systemic and chronic inflammation might contribute to the development of atherosclerosis and CHD both directly and by reducing HDL-C levels, as suggested by our epidemiological study.
Further longitudinal studies are needed in order to confirm our results in different populations, and to better understand the causal pathway that links IL-6 and HDL-C levels in older adults.
References
- 1.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham study. Am J Med. 1977;62:707–14. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 2.Assmann G, Schulte H. Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary heart disease (the PROCAM experience) Prospective Cardiovascular Munster study. Am J Cardiol. 1992;70:733–7. doi: 10.1016/0002-9149(92)90550-i. [DOI] [PubMed] [Google Scholar]
- 3.Genest JJ, Jr, Martin-Munley SS, McNamara JR, et al. Familial lipoprotein disorders in patients with premature coronary heart disease. Circulation. 1992;85:2025–33. doi: 10.1161/01.cir.85.6.2025. [DOI] [PubMed] [Google Scholar]
- 4.Rubins HB, Robins SJ, Collins D, et al. Department of veterans affairs HDL intervention Trial Study Group. Distribution of lipids in 8500 men with coronary artery disease. Am J Cardiol. 1995;75:1196–201. doi: 10.1016/s0002-9149(99)80761-9. [DOI] [PubMed] [Google Scholar]
- 5.Corti MC, Guralnik JM, Salive ME, et al. HDL cholesterol predicts coronary heart disease mortality in older persons. JAMA. 1995;274:539–44. [PubMed] [Google Scholar]
- 6.Expert panel on detection evaluation and treatment of high blood cholecterol in adults: executive summary of the third National Cholesterol Education Program (NCEP) (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 7.Wood D, De Backer G, Faergeman O, et al. Prevention of coronary heart disease in clinical practice recommendations of the second joint task force of European societies on coronary prevention. Atherosclerosis. 1998;140:199–270. doi: 10.1016/s0021-9150(98)90209-x. [DOI] [PubMed] [Google Scholar]
- 8.The international task force for prevention of coronary heart disease: the scientific background for primary and secondary prevention of coronary heart disease. Nutr Metab Cardiovasc Dis. 1998;8:205–71. [Google Scholar]
- 9.Whitney EJ, Krasuski RA, Personius BE, et al. A randomized trial of a strategy for increasing high density lipoprotein cholesterol levels: effects on progression of coronary heart disease and clinical events. Ann Intern Med. 2005;142:45–104. doi: 10.7326/0003-4819-142-2-200501180-00008. [DOI] [PubMed] [Google Scholar]
- 10.Schaefer EJ, Lamon-Fava S, Ordovas JM, et al. Factors associated with low and elevated plasma high density lipoprotein cholesterol and apolipoprotein A-I levels in the Framingham offpring study. J Lipid Res. 1994;35:871–82. [PubMed] [Google Scholar]
- 11.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 12.Hardardottir I, Grunfeld C, Feingold KR. Effects of endotoxins and cytokines on lipid metabolism. Curr Opin Lipidol. 1994;5:207–15. doi: 10.1097/00041433-199405030-00008. [DOI] [PubMed] [Google Scholar]
- 13.Volpato S, Palmieri E, Fellin R, Zuliani G. Acute phase markers are associated with reduced plasma lipid levels in a population of hospitalized elderly patients. Gerontology. 2000;46:22–7. doi: 10.1159/000022129. [DOI] [PubMed] [Google Scholar]
- 14.Ridker PM, Stampfer MJ, Rifai N. Novel risk factor for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein (a), and standar cholesterol screening as predictors of peripheral arterial disease. JAMA. 2001;285:2481–5. doi: 10.1001/jama.285.19.2481. [DOI] [PubMed] [Google Scholar]
- 15.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 16.Frohlich M, Imhof A, Berg G, et al. Association between C-reactive protein and features of the metabolic syndrome: a population-based study. Diabetes Care. 2000;23:1935–9. doi: 10.2337/diacare.23.12.1835. [DOI] [PubMed] [Google Scholar]
- 17.Festa A, D'Agostino R, Jr, Howard G, Mykkanen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–7. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 18.Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, Guralnik JM, Longo DL. The origin of age-related pro-inflammatory state. Blood. 2004 doi: 10.1182/blood-2004-07-2599. publ ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson PW, Anderson KM, Harris T, Kannel WB, Castelli WP. Determinants of change in total cholesterol and HDL-C with age: the Framingham Study. Gerontology. 1994 November;49:M252–7. doi: 10.1093/geronj/49.6.m252. [DOI] [PubMed] [Google Scholar]
- 20.Ferrucci L, Bandinelli S, Benvenuti E, et al. for the InCHIANTI group subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–25. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 21.Pisani P, Faggiano F, Krogh V, Palli D, Vineis P, Berrino F. Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centers. Int J Epidemiol. 1997;26:S152–60. doi: 10.1093/ije/26.suppl_1.s152. [DOI] [PubMed] [Google Scholar]
- 22.Fernandez-Real JM, Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev. 2003;24:278–301. doi: 10.1210/er.2002-0010. [DOI] [PubMed] [Google Scholar]
- 23.Volpato S, Pahor M, Ferrucci L, et al. Relationship of alcohol intake with inflammatory markers and plasminogen activator inhibitor-1 in well-functioning older adults: the health, aging, and body composition study. Circulation. 2004;109:607–12. doi: 10.1161/01.CIR.0000109503.13955.00. [DOI] [PubMed] [Google Scholar]
- 24.Grunfield C, Feingold KR. Regulation of lipid metabolism by cytokines during host defence. Nutrition. 1996;12:S24–6. doi: 10.1016/0899-9007(96)90013-1. [DOI] [PubMed] [Google Scholar]
- 25.Jin W, Millar JS, Broedl U, Glick JM, Rader DJ. Inhibition of endothelial lipase causes increased HDL cholesterol levels in vivo. J Clin Invest. 2003;111:357–62. doi: 10.1172/JCI16146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin W, Sun SS, Marchadier D, Octtaviani E, Glick JM, Rader DJ. Endothelial cells secrete triglycerides lipase and phospolipase activities in response to cytokines as a result of endothelial lipase. Circ Res. 2003;92:644–50. doi: 10.1161/01.RES.0000064502.47539.6D. [DOI] [PubMed] [Google Scholar]
- 27.Kisilevski R, Subrahmanyan L. Serum amyloid A changes high density lipoprotein's cellular affinity. Lab Invest. 1992;66:778–85. [PubMed] [Google Scholar]
- 28.Pruzanski W, Stefanski E, deBeer FC, deBeer MC, Ravandi A, Kuksis A. Comparative analysis of lipid composition of normal and acute-phase high density lipoproteins. J Lipid Res. 2000;41:1035–47. [PubMed] [Google Scholar]
- 29.Van Lenten BJ, Hama SY, de Beer FC, et al. Anti-inflammatory HDL becomes pro-Inflammatory during the acute phase response. J Clin Invest. 1995;96:2758–67. doi: 10.1172/JCI118345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malle E, Steinmetz A, Raynes JG. Serum amyloid A (SAA): an acute phase protein and apolipoprotein. Atherosclerosis. 1993;102:131–46. doi: 10.1016/0021-9150(93)90155-n. [DOI] [PubMed] [Google Scholar]
- 31.Shepard EG, deBeer FC, deBeer MC, Jeenach MS, Coetzee GA, van der Westhuyzen DR. Neutrophil association and degradation of normal and acute phase high-density lipoprotein. Biochem J. 1987;248:919–26. doi: 10.1042/bj2480919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Popa C, Netea MG, Radstake T, et al. Influence of anti-tumour necrosis factor therapy on cardiovascular risk factors in patients with active rheumatoid arthritis. Ann Rheum Dis. 2005;64:303–5. doi: 10.1136/ard.2004.023119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hyka N, Dayer JM, Kohno T, Edwards CK, III, Roux-Lombard P, Burger D. Apolipoprotein A-I inhibits the production of interleukin 1-β and tumor necrosis factor-α by blocking contact-mediated activation of monocytes by T lymphocytes. Blood. 2001;97:2381–9. doi: 10.1182/blood.v97.8.2381. [DOI] [PubMed] [Google Scholar]


