Abstract
Background/Aims
Lamivudine has been shown to improve liver disease and survival of hepatitis B (HBV) patients on the liver-transplant (OLT) waiting list, but liver failure may worsen in patients with drug resistance. Use of antiviral salvage therapy may decrease this risk.
Methods
We analyzed data from patients enrolled in the NIH HBV OLT cohort to study the effects of pre-transplant antiviral therapy on transplant-free survival and survival without transplant. We also compared the clinical outcomes of those who did or did not develop antiviral failure (virologic breakthrough or genotypic resistance) while awaiting transplant.
Results
One hundred twenty-two eligible patients received antiviral therapy pre-OLT and were followed for a median of 40.5 months (0.4–123.0) after initiation of antiviral therapy. Forty-four (36.1%) patients developed antiviral failure; all had lamivudine monotherapy as initial treatment. Forty-two patients started salvage therapy a median of 5 months after lamivudine failure; the median MELD score was 12. Twenty-one (50%) patients had a full response to salvage therapy. Eleven (26.2%) patients had a suboptimal virologic response but remained clinically compensated. Antiviral failure was not a significant predictor of transplant or death (p=0.09) or death without transplant (p=0.39). Multivariate predictors of transplant or death were high MELD score, HCC, and low albumin. High MELD score and low albumin were predictors of death without transplant.
Conclusion
Antiviral failure in patients with HBV on the OLT waiting list did not impair clinical outcome if recognized early and if salvage therapy is promptly initiated.
Keywords: survival, lamivudine, adefovir, cirrhosis, liver failure
Introduction
Decompensated liver disease secondary to hepatitis B virus (HBV) accounts for 4.3% of liver transplants performed in the United States.1 The use of lamivudine in patients with decompensated cirrhosis has been shown to improve or stabilize liver disease, with studies documenting decreases in Child-Turcotte-Pugh (CTP) score,2–4 and resolution of clinical complications.5,6 In some cases, improvements permitted removal of patients from the liver transplant (OLT) waiting list.3,4 However, the effect of lamivudine on survival without transplant and transplant-free survival is not clear since treatment has not been randomized, and patients who received treatment generally had more advanced liver disease and higher HBV DNA levels than those who did not receive treatment.4,6
Lamivudine resistance is known to develop in up to 70% of patients after five years of treatment, and can lead to hepatitis flares, worsening liver failure, and death.7–10 Furthermore, the waiting time to OLT varies markedly. Due to these concerns, prior to the availability of antiviral salvage therapy, initiation of lamivudine was often delayed until OLT was imminent. Delay in starting antiviral therapy in patients with decompensated cirrhosis may diminish the survival benefits since several studies have shown that clinical improvement takes 3 to 6 months.3,11
Several antiviral salvage agents are now available for patients who develop lamivudine resistance. Adefovir dipivoxil alone or in combination with lamivudine has been effective in decreasing serum HBV DNA levels in patients with lamivudine-resistant HBV.12–14 In patients with lamivudine-resistant HBV and cirrhosis, adefovir can provide clinical benefits including reduction of CTP and Model for Endstage Liver Disease (MELD) scores,15 and in some patients reversal of liver failure permitting removal from the transplant list.15–17 Entecavir18 and tenofovir19,20 are also effective in decreasing serum HBV DNA levels in patients with lamivudine-resistant HBV. However, data on the safety and efficacy of the latter two antiviral therapies in patients with decompensated cirrhosis are limited. Furthermore, entecavir is less effective and the risk of drug resistance is higher in patients with lamivudine resistance compared to those with wild type HBV. 18
The availability of new antiviral agents for patients with lamivudine-resistant HBV may permit earlier initiation of antiviral therapy in hepatitis B patients waiting for OLT and enable patients with virologic breakthrough to be salvaged. Thus, antiviral therapy may have a greater benefit on survival among patients with decompensated HBV cirrhosis treated in recent years.
The National Institutes of Health (NIH) HBV OLT study is a multicenter observational study of pre- and post- OLT patients with hepatitis B. The study provides a large number of patients with a long duration of follow-up which allows us to determine the impact of pre-transplant antiviral therapy. The aims of this analysis were to describe the transplant-free survival and survival on the waiting list without transplant among this cohort and to compare the outcomes between those who did versus those who did not develop antiviral resistance while waiting for transplant.
Patients and Methods
Patient Population
The NIH HBV OLT study is a retrospective-prospective observational study that enrolled hepatitis B surface antigen (HBsAg) positive patients >13 years old from 15 centers in the United States, who were listed for OLT for hepatitis B between November 2001 and June 2005.21 The study was approved by the Institutional Review Board of each of the participating centers, and written informed consent was obtained from all patients. For patients enrolled at the time of listing, data were collected prospectively. For patients enrolled after varying durations on the OLT waiting list, data after enrollment were collected prospectively while data prior to enrollment were collected retrospectively up to the time of listing.
For this analysis, only patients with greater than six months of follow-up on the waiting list were included. Due to variations in the onset of antiviral therapy, not all patients had greater than six months of follow-up after the initiation of antiviral therapy. Patients were excluded if they were listed for fulminant hepatitis B or a second transplant, or if they were coinfected with human immunodeficiency virus or hepatitis C virus. Patients who were enrolled after transplant were also excluded. Data on demographics (gender, race/ethnicity, age at listing); outcome (death, transplant, withdrawal from the OLT waiting list); presence of hepatocellular carcinoma (HCC) at listing based on the United Network of Organ Sharing (UNOS) criteria22; hepatitis B e antigen (HBeAg) status and HBV DNA levels at listing were extracted from a computerized database. In addition, start and stop dates of initial and any subsequent antiviral therapies, and dates in which virologic breakthrough or genotypic resistance was detected were recorded. Laboratory values at the time of listing, antiviral failure, and initiation of antiviral salvage therapy were also collected. The MELD score was calculated from laboratory values and did not consider MELD exceptions.
The NIH HBV OLT study is an observational study, thus no specific antiviral treatment was tested. The study protocol did provide guidelines on the use of antiviral therapy pre- and post- OLT. Lamivudine was the first-line antiviral therapy in all centers until 2003. Adefovir was used as rescue therapy for patients with breakthrough during lamivudine therapy, initially through a compassionate use protocol and subsequently as standard therapy after its approval in the fall of 2002. Some patients were switched from lamivudine to adefovir with durations of overlapping treatment varying from 1 to 124 weeks while others continued lamivudine indefinitely. A few patients received tenofovir or entecavir as salvage therapy. Dose adjustments were made according to renal function as recommended by the manufacturers.
All laboratory tests except for HBV DNA and antiviral-resistant mutations were performed using commercially available assays at the participating centers. An additional 10 ml blood was collected at each visit, centrifuged, divided into aliquots and stored at −70C in the participating centers, and batch-shipped to the central laboratory at the University of Michigan, where serum samples were stored at −80C until testing.
Outcomes
Virologic breakthrough was defined as an increase in serum HBV DNA by >1 log10 copies/mL from nadir in a patient who had previously responded to antiviral therapy with complete virologic suppression. Genotypic resistance to lamivudine was defined as detection of substitutions of methionine to valine or isoleucine (M204V/I) in the tyrosine-methionine-aspartate-aspartate (YMDD) motif of the reverse transcriptase region of the HBV polymerase.23 Genotypic resistance to adefovir was defined as detection of substitutions of asparagine for threonine (N236T) and/or substitution of alanine for valine or threonine (A181V/T).24 Antiviral failure was a composite endpoint of either virologic breakthrough or genotypic resistance, and the earliest date of detection was recorded. All cases of antiviral failure were considered to be secondary treatment failure unless specified otherwise although laboratory data documenting initial response to antiviral therapy were not available in some patients.
Virologic breakthrough was determined based on serum HBV DNA values available to the participating investigators (including tests at the participating centers and central laboratory as well as local laboratories outside the participating sites) while genotypic resistance was determined based on testing for resistant mutations in the central laboratory.
Tests for HBV DNA and Antiviral-resistant Mutations
Serum HBV DNA levels were quantified by the Cobas Amplicor HBV Monitor assay (Roche Molecular Systems, Inc., Branchburg, NJ) at the central laboratory. The lower limit of detection of this assay is 200 copies/mL. Samples with values >100,000 copies/mL were diluted 1:1,000 to 1:100,000 fold and retested. For patients with missing central laboratory samples, HBV DNA results at the participating centers were used and the results converted into log10 copies/mL using conversion formulae provided by the manufacturers.
All samples from patients with virologic breakthrough and all samples from patients with detectable serum HBV DNA by the Amplicor assay after ≥6 months of antiviral treatment were tested for antiviral-resistant mutations using a line probe assay, INNO-LiPA DRv2 (Innogenetics, Ghent, Belgium).25 All breakthrough samples were also tested by direct sequencing to detect any mutations not included in INNO-LiPA DRv2.
Statistical Analysis
Transplant-free survival and survival without transplant were estimated using Kaplan-Meier methods. For both analyses, the start of follow-up was the date when the first course of antiviral therapy was begun. Patients in whom the antiviral start date was unknown (n=8) were excluded from the survival analysis. For transplant-free survival, the outcomes were death or transplant, and patients were censored at the time of withdrawal from the OLT waiting list or the date of last follow-up. For survival without transplant, the outcome was death, and patients were censored at the time of transplant, withdrawal from the OLT waiting list, or the date of last follow-up. Comparison was made between patients who experienced antiviral failure and those that did not. Other covariates considered were race, gender, HCC at listing, age at listing, and the following laboratory values at listing: MELD score, aspartate (AST) and alanine (ALT) aminotransferases, platelets, and albumin. Variables with a significance level of p≤0.2 by the log-rank test on Kaplan-Meier analysis were entered into a Cox regression model. Variables were removed from the model using backwards elimination for variables with p>0.05. Hazard ratios were calculated for each five point increase in MELD and each increase of 1 g/L for albumin. All analyses were done using SAS, version 9.1.3 (Cary, NC).
Results
One-hundred forty-four patients met the inclusion criteria for this analysis. One-hundred twenty-two patients (84.7%) received pre-transplant antiviral therapy. The characteristics of the entire cohort are shown in Table 1.
Table 1.
Characteristics of the Cohort
| Characteristic | All patients (n=144) | No antivirals (n=22) | Antivirals (n=122) |
|---|---|---|---|
| At Listing | |||
| Race, n (%) Asian
Non-Asian |
66 (44.6)
78 (54.2) |
8 (36.4)
14 (63.4) |
58 (47.5)
64 (52.5) |
| Gender, n (%) Male
Female |
117 (81.2)
27 (18.8) |
18 (81.8)
4 (18.2) |
99 (81.1)
23 (18.9) |
| Age, years mean (std dev) | 50.4 (±9.2) | 48.9 (±6.9) | 50.6 (±9.6) |
| HCC, n (%) Yes
No |
32 (22.2)
112 (77.8) |
5 (22.7)
17 (77.3) |
27 (22.1)
95 (77.9) |
| HBeAg, n (%) Positive
Negative |
36 (37.1)
61 (62.9) |
1 (10.0)
9 (90.0) |
35 (40.2)
52 (59.8) |
| HBV DNA, n (%) Detectable
Not detectable |
95 (97.9)
2 (2.1) |
12 (92.3)
1 (7.7) |
83 (98.8)
1 (1.2) |
| Labs at listing
Median (range) MELD AST, IU/L ALT, IU/L Bilirubin, mg/dL Albumin, g/L INR Platelets, 103/mm3 Creatinine, mg/dL |
12 (6–39) 66 (17–693) 60 (6–1772) 1.7 (0.4–32.8) 3.2 (0.7–4.6) 1.3 (0.9–3.1) 76 (23–315) 0.9 (0.4–10.2) |
12.0 (6–26) 72 (33–249) 58 (20–406) 2.0 (0.9–10.0) 3.1 (2.0–4.5) 1.3 (0.9–1.8) 65 (26–141 0.8 (0.5–1.0) |
12.4 (6–39) 66 (17–693) 59 (6–1772) 1.6 (0.4–32.8) 3.3 (0.7–4.6) 1.3 (0.9–3.1) 78 (23–315) 0.9 (0.4–10.2) |
| Follow-up time from listing, mos, median (range) | 31.5 (range 0–112.7) | 29.4 (3.2–112.7) | 31.9 (0–110.4) |
| Outcome, n (%)
Transplanted Withdrawn from Study Died Still on OLT waiting list |
33 (22.9) 22 (15.3) 25 (17.4) 64 (44.4) |
4 (18.2) 4 (18.2) 6 (27.3) 8 (33.4) |
29 (23.8) 18 (14.8) 19 (15.6) 56 (45.9) |
HCC=hepatocellular carcinoma, HBeAg=hepatitis B e antigen, MELD=Model for Endstage Liver Disease score, AST=aspartate aminotransferase, ALT=alanine aminotransferase, INR=international normalized ratio, OLT=orthotopic liver transplant
Antiviral Therapy
Of the 122 patients that received antiviral therapy, 81% were men, 48% were Asians, and mean age was 50.6 years (Table 1). At listing, 40% were HBeAg positive and 99% of those tested had detectable serum HBV DNA. Twenty-seven (22%) patients had HCC at listing and median laboratory MELD score was 12.
Sixty-five patients (56%) started therapy prior to 2002, the year adefovir was approved. Sixty-eight patients had a change in treatment regimen; the majority of changes were made for antiviral failure, but a few changes were made due to concerns for lamivudine resistance after a long duration of therapy. The most common first antiviral regimen was lamivudine monotherapy, in 110 (90.2%) patients. Other first regimens were adefovir in 7 patients, lamivudine plus adefovir in 3 patients, entecavir in 1 patient, and tenofovir in 1 patient.
Eighteen patients (15.8%) had 0 to 1 year of pre-transplant follow-up after initiation of antiviral therapy, 31 (27.2%) had 1 to 3 years, 33 (28.9%) had 3 to 5 years, 20 (17.5%) had 5 to 7 years, and 12 (10.5%) had greater than 7 years of follow up. The median duration of pre-transplant follow up after the onset of antiviral therapy was 40.5 months (range 0.4–123.0). Those who started antiviral therapy prior to listing had been on therapy for a median of 9.0 months (range 0.03 to 87.5) at the time of listing.
Of the 78 patients who did not develop antiviral failure, 33 were still awaiting OLT at the time of data analysis with a median follow up on the waiting list of 31.5 months, 21 had been transplanted with no recurrences after a median post-OLT follow up of 11.7 months, 14 died without OLT (10 from liver failure), and 10 were withdrawn from the study (none for worsening liver disease, 2 for improvement).
Antiviral Failures
Forty-four (36.1%) treated patients experienced antiviral failure while on the transplant waiting list. All 44 received lamivudine monotherapy as their first antiviral regimen. There were no antiviral failures among the 12 patients who received other regimens as their initial therapy. Thirty-seven (84%) patients with lamivudine failure had a virologic breakthrough with confirmed genotypic resistance. Five patients had a breakthrough documented by the clinical site with no sample available for resistance testing. An additional 2 patients were switched from lamivudine to adefovir for suspected lamivudine resistance but evidence in support of virologic breakthrough or genotypic resistance was not available.
The median time to lamivudine failure from the start of lamivudine therapy was 55.4 months. The probability of lamivudine failure at 1, 2 and 3 years was 5%, 27% and 36%, respectively. At the time of lamivudine failure, the median laboratory values were MELD score 12.7, AST 47 IU/L, ALT 47 IU/L, bilirubin 1.6 mg/dL, albumin 3.3 g/dL INR 1.3, Cr 0.9 mg/dL, and serum HBV DNA 7.2 log10 copies/mL.
Of the 44 patients with lamivudine failure, nine subsequently experienced treatment failure to salvage adefovir (1 primary failure, 5 secondary failures, 2 unknown). Seven patients had genotypic resistance and of these three had documented virologic breakthrough; two patients had virologic breakthrough documented by HBV DNA results at the clinical site but blood samples for confirmatory testing were not available. Of the nine patients with virologic breakthrough or genotypic resistance to adefovir, 3 received combination of adefovir and lamivudine, 5 were switched to adefovir monotherapy and the remaining patient was switched to tenofovir monotherapy.
None of the six patients who received de novo adefovir therapy had virologic breakthrough or genotypic resistance.
Response to Salvage Therapy
Antiviral failure was diagnosed after FDA approval of adefovir in 29 of 44 patients. Salvage therapy was initiated in 42 patients a median of 5.2 months (range 0–79.4) after the diagnosis of antiviral failure (Figure 1). Two patients did not receive salvage therapy: one patient removed himself from the waiting list and the other received a transplant for HCC before salvage therapy was initiated. The latter patient received adefovir in combination with HBIG post-OLT. The median time to initiation of salvage therapy was longer in those who developed antiviral failure before adefovir approval than after (20.7 months vs. 3.7 months). At the time salvage therapy was initiated, the median lab values were MELD 12, AST 68 IU/L, ALT 76 IU/L, bilirubin 1.5 mg/dL, albumin 3.3 g/dL and INR 1.2. Salvage therapy was initiated in 8 patients when serum HBV DNA level was less than 106 copies/mL; 3 of these 8 patients had normal ALT. Twenty-five patients had HBV DNA levels that exceeded 106 copies/mL before initiation of salvage therapy, of whom 5 had normal ALT, 7 had ALT 1–2 times normal and 13 had ALT >2 times normal.
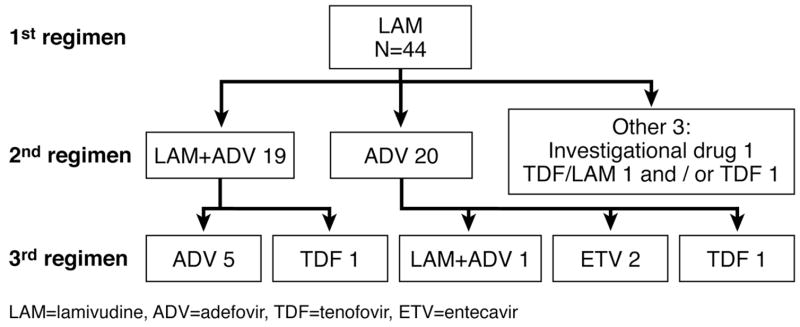
Figure 1.
Antiviral regimens for 110 patients who received lamivudine as their initial regimen.
Among 19 patients who received lamivudine plus adefovir, 8 had a virologic response, 7 had a suboptimal response (serum HBV DNA >104 copies/mL after >6 months) but remained compensated, 1 had a suboptimal response and required transplant, 1 had no viral suppression and died from hepatitis B flare. No information on virologic response to salvage treatment was available for 2 patients. Among the 20 patients who received adefovir monotherapy, 11 had a virologic response, 4 had a suboptimal response but remained compensated, one had a suboptimal response and went on to transplant, and one had a hepatitis flare that responded to salvage therapy. Response was not assessed in 3 patients: one was transplanted for HCC 2 months after salvage therapy, and 2 patients started salvage therapy at the last follow-up visit. Both patients who received tenofovir had a virologic response. The patient who received an investigational drug was transplanted 3 days after start of salvage therapy.
Outcome of Patients with Antiviral Failure
Five (11.4%) of the 44 patients with antiviral failure had a hepatitis flare (defined as elevation of AST and ALT >3 times the nadir). One patient, in whom salvage therapy was delayed by 16 months, developed hepatic decompensation and died before a transplant was available. Three patients responded to salvage therapy. The fifth patient was transplanted eight months after initiation of salvage therapy with no available information on virologic response, though AST and ALT were improved. The MELD score at transplant was 18.
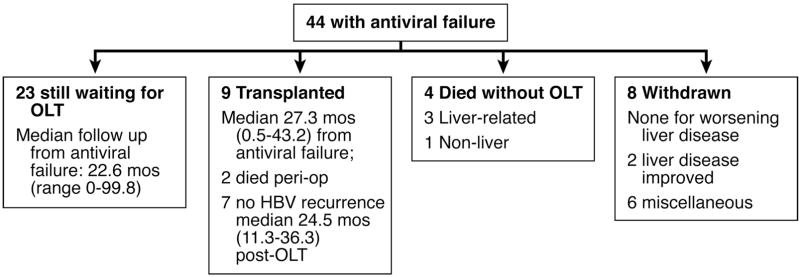
Outcomes of the patients who developed antiviral failure are shown in Figure 2. Of the 44 patients who developed antiviral failure, 9 underwent OLT after a median of 27 months from the time of diagnosis of antiviral failure, 3 of whom were transplanted for HCC. Two patients did not respond to salvage therapy and were transplanted with MELD scores of 32 and 27. Both patients had delay in initiation of salvage therapy - 20 and 27 months after detection of lamivudine breakthrough. One patient responded to salvage adefovir, but developed adefovir resistance 20 months later with decompensation requiring transplant. Three others had virologic response to salvage therapy but continued to have mild to moderate hepatic decompensation and were transplanted with MELD scores of 15, 18 and 20. Post-OLT, all patients received hepatitis B immune globulin (HBIG) and tenofovir or adefovir with or without lamivudine except one patient who received high-dose HBIG, lamivudine, and an experimental monoclonal antibody. None of the patients had HBV recurrence post-OLT after a median follow-up of 24.5 months after transplant. Four patients with antiviral failure died without OLT, 3 from liver failure (including 1 with a fatal hepatitis flare mentioned above and two from hepatic decompensation 8 and 16 months after beginning salvage therapy secondary to adefovir resistance) and one from complications of non-transplant surgery.
Figure 2.
Outcomes of the 44 patients with antiviral failure
Eight patients with antiviral failure were withdrawn from the waiting list (none for worsening liver disease). The remaining 23 patients were still on the waiting list with stable liver disease, after a median of 22.6 months from the time of diagnosis of antiviral failure. At the last follow up visit, the median laboratory values for these 23 patients were MELD 9 (range 6–18), AST 43 IU/L (range 22–149 IU/L), and albumin 3.7 g/dL (range 2.1–4.9 g/dL).
Survival of Patients with and without Antiviral Failure
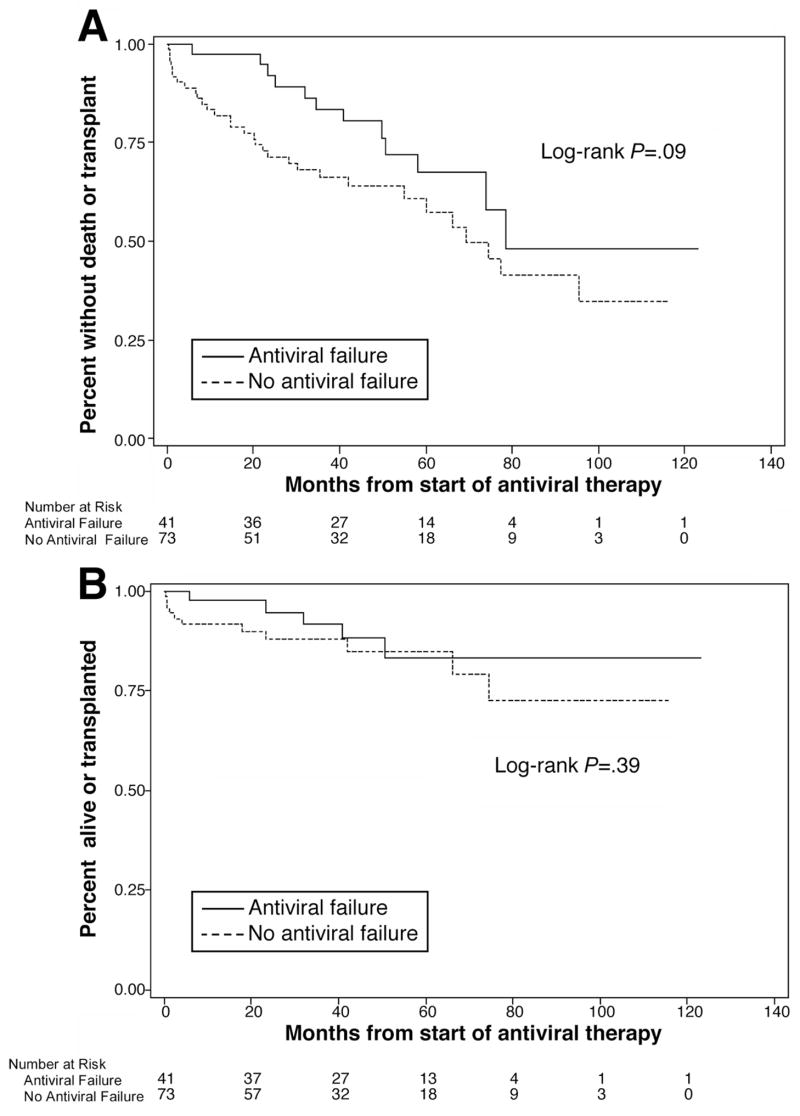
Actuarial estimates of transplant-free survival at 1 year, 3 years and 5 years were 97.6%, 83.5% and 67.5% respectively for those with antiviral failure and 81.9%, 71.3% and 60.8% for those without antiviral failure. (Figure 3a) In univariate analysis of transplant-free survival, HCC (p=0.01), MELD at listing (p=0.001) and albumin (p=0.006) were found to be significant predictors of survival (Table 2) but antiviral failure was not (p=0.09). Cox regression models identified HCC at listing (HR 3.91), MELD at listing (HR 5.34) and albumin at listing (HR 0.49) as independent predictors of liver transplantation or death. (Table 3)
Figure 3.
(A). Kaplan-Meier estimates of transplant-free survival comparing those who developed antiviral failure (solid line) and those who did not develop antiviral failure (dashed line), p=0.09 by log-rank test. (B). Kaplan-Meier estimates of survival without transplant comparing those with antiviral failure (solid line) and those without antiviral failure (dashed line), p=0.39 by log-rank test. Eight patients for whom the antiviral start date was not known were excluded from the survival analyses.
Table 2.
Kaplan-Meier (univariate) analyses for transplant-free survival and survival without transplant.
| Variable | n | Transplant-Free Survival p-value, log-rank | Survival without Transplant p-value, log-rank |
|---|---|---|---|
| Antiviral failure
No Yes |
74 43 |
0.09 | 0.46 |
| Gender
Male Female |
94 23 |
0.09 | 0.96 |
| Race
Asian Non-Asian |
56 61 |
0.79 | 0.09 |
| HCC at listing
No Yes |
91 26 |
0.01 | 0.61 |
| Age * | 117 | 0.90 | 0.13 |
| MELD * | 114 | 0.0010 | 0.0001 |
| AST * | 103 | 0.91 | 0.92 |
| ALT * | 100 | 0.46 | 0.86 |
| Platelets * | 103 | 0.33 | 0.96 |
| Albumin * | 105 | 0.006 | 0.003 |
Values at listing
HCC=hepatocellular carcinoma, MELD=Model for Endstage Liver Disease Score, AST=aspartate aminotransferase, ALT=alanine aminotransferase
Table 3.
Cox regression models for predictors of adverse outcomes
| Variable | Hazard Ratio (95% CI) | p |
|---|---|---|
| OLT or Death | ||
| Hepatocellular carcinoma at listing | 3.91 (1.80–8.49) | 0.02 |
| Listing MELD | 5.34 (5.05–5.64) | 0.0006 |
| Albumin at listing | 0.49 (0.30–0.79) | 0.004 |
| Death Without Transplant | ||
| Listing MELD | 5.40 (5.01–5.77) | 0.02 |
| Albumin at listing | 0.42 (0.23–0.80) | 0.008 |
Actuarial estimates of survival without transplant were 97.5%, 91.6% and 83.3% at 1, 3 and 5 years for those with antiviral failure. Among those without antiviral failure, the corresponding probabilities were 91.6%, 87.9% and 84.9%. (Figure 3b) For survival without transplant, only MELD (p=0.0001) and albumin (p=0.003) at listing were significant in univariate analysis. Antiviral failure was again not significant (p=0.46). Both MELD (HR 5.4) and albumin (HR 0.42) remained significant in the multivariate model. (Table 3)
Discussion
In this study of 122 hepatitis B patients on the OLT waiting list followed for up to 123 months after the initiation of antiviral therapy (median 40.5), 36% of patients experienced antiviral failure but outcomes were not different between patients who did and those who did not develop antiviral failure. Neither transplant-free survival nor survival without transplant was negatively impacted by antiviral failure. Independent predictors of transplant-free survival included HCC, MELD and serum albumin at listing: variables that reflected the severity of liver disease and ranking on the OLT waiting list. Similarly, serum albumin and laboratory MELD at listing were independent predictors of survival without transplant.
The finding that antiviral failure had no impact on survival of HBV patients on the OLT waiting list was unexpected since virologic breakthrough due to emergence of antiviral-resistant mutations had been reported to result in deaths from severe hepatitis flares.7–10,26 This may be explained in part by the inclusion of patients with low MELD scores; of the 53 patients with no documented HCC, 36 (68%) had MELD score <15 at listing. The generally favorable outcome of patients with antiviral failure may also be related to the administration of salvage therapy in 42/44 patients and the fact that most patients had compensated liver disease at the time when salvage therapy was initiated (median MELD score of 12), despite high HBV DNA and elevated ALT levels in most patients. However, not all patients with antiviral failure had a favorable outcome. Three patients died of liver failure before they could be transplanted, 6 underwent OLT due to liver failure: 2 failed to achieve initial virologic response, 3 achieved initial virologic response but remained decompensated and 1 developed subsequent adefovir resistance. The high rate of salvage therapy failure may be due to delays in initiating adefovir particularly in the era prior to its approval, the high percent of patients receiving adefovir monotherapy, and the weak antiviral activity of 10 mg doses of adefovir. These data highlight the importance of frequent monitoring of serum HBV DNA levels so that antiviral failure can be detected early and salvage therapy initiated promptly. A recent study showed that salvage therapy was more effective in patients who had low serum HBV DNA and normal ALT levels.27
A cumulative probability of lamivudine failure of 36% after 3 years of antiviral therapy in this study is lower than that reported in other studies of lamivudine.28 This is likely because virologic breakthrough was not as closely monitored prior to enrollment into this study and diagnosis of antiviral failure may have been delayed in some patients.
The impact of pre-transplant antiviral therapy on the rate of HBV recurrence post-OLT could not be assessed in this analysis because only 30 patients underwent OLT. Of the 9 patients with antiviral failure who underwent OLT, none had HBV recurrence after a median post-OLT follow-up of 24.5 months. The excellent results are likely a result of salvage therapy pre- and post- OLT along with HBIG.
The strengths of the current study include the large number of patients studied and the long duration of follow-up, with some patients having outcome data available up to 10 years after starting antiviral therapy. Moreover, 84% of patients with virologic breakthrough had confirmed genotypic resistance. Finally, almost all (42/44) patients with antiviral failure received salvage therapy, a practice that is now standard but not possible in earlier studies.2–6,11
Our study has several limitations. First, the retrospective-prospective design did not allow for confirmatory testing in all patients with antiviral failure. However, most cases of virologic breakthrough in which samples were available for testing were due to antiviral resistance. Second, antiviral therapy was initiated prior to enrollment in 86 patients. For these patients, data on serum HBV DNA levels prior to start of treatment were incomplete, serum HBV DNA monitoring prior to enrollment was not systematic, and blood samples were not available for central laboratory testing. Finally, although treatment guidelines were included in the protocol, the observational nature of the study meant that the choice of initial antiviral therapy and salvage therapy was left to the discretion of the investigators.
Our study was not designed to determine the benefits of antiviral therapy since the patients were not randomized. Among the patients meeting the criteria for this analysis, 85% received antiviral therapy. Our data suggest that the availability of salvage therapy for lamivudine resistance and more potent antiviral therapy with lower risks of drug resistance will allow an increasing proportion of HBV patients on the transplant waiting list to receive antiviral therapy. Antiviral treatment can now be initiated early in an attempt to prevent the need for OLT. In this study, 56 (46%) patients receiving antiviral therapy were still on the waiting list (33 without antiviral failure and 23 with antiviral failure), a median of 48.4 months (range 0.5–123) after initiation of antiviral therapy. Four patients were removed from the waiting list due to improvement in liver disease.
In conclusion, our study showed that HBV patients on the transplant waiting list who developed antiviral failure did not have worse outcomes, including death or liver transplant compared to those with no antiviral failure. While most patients received salvage therapy when they were still compensated and benefited from the salvage therapy, a few patients decompensated before or despite salvage therapy. Our findings highlight the importance of careful monitoring of serum HBV DNA levels in HBV patients who are waiting for OLT and prompt initiation of salvage therapy when virologic breakthrough is diagnosed. The role of lamivudine as initial therapy should also be re-examined. Newer antiviral agents that are more potent with lower risks of drug resistance such as adefovir, entecavir or tenofovir or de novo combination therapy may be more appropriate. Results of studies on these treatments in the transplant population are eagerly awaited.
Acknowledgments
Funding: Supported by an NIH grant U01 DK57577; Innogenetics provided reagents for line probe assays to detect antiviral resistant mutations; Roche Molecular Diagnostics provided Amplicor kits for quantitative HBV DNA assays
We would like to thank all the investigators and study staff at the participating sites: California Pacific Medical Center, San Francisco – Natalie Bzowej, MD and Nata Devole, RN
Cedars Sinai Medical Center, Los Angeles – Tram Tran, MD and Amy Crumley, RN
Columbia University, New York – Paul Gaglio, MD and Maria Martin
Massachusetts General Hospital, Boston – Raymond T. Chung, MD, Diana Tsui and Marian Bihrle
Mayo Clinic, Rochester – Michael Ishitani, MD and Linda Lairson, RN
Mount Sinai University Medical Center, New York – Sukru Emre, MD and Ilhan Karabicak
Ochsner Clinic, New Orleans – Robert Perrillo, MD and Cheryl Denham, LPN
Stanford University, Palo Alto – Emmet Keeffe, MD and Dana Supan, RN
University of California, Los Angeles – Steve Han, MD, Pearl Kim-Hong, and Val Peacock, RN
University of Florida, Gainesville - Consuelo Soldevila-Pico, MD and Joy Peter, RN, BSN
University of Miami, Miami – Arie Regev, MD and Maria Torres
University of Pennsylvania, Philadelphia – Rajender Reddy, MD and Elliott Kozin
University of Virginia, Charlottesville – Timothy Pruett, MD and Meredith Gross
Virginia Commonwealth University, Richmond – Velimir A.C. Luketic, MD and Stacy McLeod
University of Michigan, Ann Arbor – Terese Howell, Donna Harsh, Amy Randall-Ray, Douglas
Armstrong, Munira Hussain, Jim Imus and Morton Brown, PhD
Abbreviations
- HbeAg
hepatitis B e antigen
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HIV
human immunodeficiency virus
- MELD
Model for end-stage liver disease
- OLT
orthotopic liver transplantation
Footnotes
Financial Disclosures (email address)
Melissa Osborn (mkosbor@emory.edu): Nothing to disclose
Steven Han (shbhan@ucla.edu): Research Grant/Consultant for Gilead, BMS, and Idenix.
Arie Regev (aregev@med.miami.edu): Receives research support, member of speakers’ bureau, and/or serves on advisory board of Gilead, Roche Pharmaceuticals, Valeant and Bristol-Myers Squibb
Natalie Bzowej (BzowejN@sutterhealth.org): Speakers’ Bureau Schering, Glaxo, Intarcia; Research grant/consultant: Celera, BMS, Schering, Gilead, Roche, Sciclone, Idenix Michael Ishitani (ishitani.michael@mayo.edu): Nothing to disclose.
Tram Tran (Tram.Tran@cshs.org): Research grant/consultant for Gilead, Bristol-Myers Squibb, Idenix
Anna Lok (aslok@med.umich.edu): Receives research support and/or serves on advisory board of GlaxoSmithKline, Gilead, Bristol-Myers Squibb, Idenix, Nabi, Innogenetics, Roche Molecular Diagnostics
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Camci C, Gurakar A, Rose J, Rizvi S, Wright H, Bader T, Monlux R, Schade RR, Nour BM, Sebastian A. Liver transplantation for hepatitis B in the United States. Transplantation Proceedings. 2005;37:4350–3. doi: 10.1016/j.transproceed.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Hann HW, Fontana RJ, Wright T, Everson G, Baker A, Schiff ER, Riely C, Anschuetz G, Gardner SD, Brown N, Griffiths D United States Lamivudine Compassionate Use Study G. A United States compassionate use study of lamivudine treatment in nontransplantation candidates with decompensated hepatitis B virus-related cirrhosis. Liver Transplantation. 2003;9:49–56. doi: 10.1053/jlts.2003.50005. [DOI] [PubMed] [Google Scholar]
- 3.Villeneuve JP, Condreay LD, Willems B, Pomier-Layrargues G, Fenyves D, Bilodeau M, Leduc R, Peltekian K, Wong F, Margulies M, Heathcote EJ. Lamivudine treatment for decompensated cirrhosis resulting from chronic hepatitis B. Hepatology. 2000;31:207–10. doi: 10.1002/hep.510310130. [DOI] [PubMed] [Google Scholar]
- 4.Yao FY, Terrault NA, Freise C, Maslow L, Bass NM. Lamivudine treatment is beneficial in patients with severely decompensated cirrhosis and actively replicating hepatitis B infection awaiting liver transplantation: a comparative study using a matched, untreated cohort. Hepatology. 2001;34:411–6. doi: 10.1053/jhep.2001.26512. [DOI] [PubMed] [Google Scholar]
- 5.Perrillo RP, Wright T, Rakela J, Levy G, Schiff E, Gish R, Martin P, Dienstag J, Adams P, Dickson R, Anschuetz G, Bell S, Condreay L, Brown N Lamivudine North American Transplant G. A multicenter United States-Canadian trial to assess lamivudine monotherapy before and after liver transplantation for chronic hepatitis B. Hepatology. 2001;33:424–32. doi: 10.1053/jhep.2001.21554. [DOI] [PubMed] [Google Scholar]
- 6.Fontana RJ, Keeffe EB, Carey W, Fried M, Reddy R, Kowdley KV, Soldevila-Pico C, McClure LA, Lok AS for the National Institutes of Health Hepatitis BVOLTSG. Effect of lamivudine treatment on survival of 309 North American patients awaiting liver transplantation for chronic hepatitis B. Liver Transplantation. 2002;8:433–9. doi: 10.1053/jlts.2002.32983. [DOI] [PubMed] [Google Scholar]
- 7.Liaw YF, Chien RN, Yeh CT, Tsai SL, Chu CM. Acute exacerbation and hepatitis B virus clearance after emergence of YMDD motif mutation during lamivudine therapy. Hepatology. 1999;30:567–72. doi: 10.1002/hep.510300221. [DOI] [PubMed] [Google Scholar]
- 8.Lok AS, Lai CL, Leung N, Yao GB, Cui ZY, Schiff ER, Dienstag JL, Heathcote EJ, Little NR, Griffiths DA, Gardner SD, Castiglia M. Long-term safety of lamivudine treatment in patients with chronic hepatitis B. Gastroenterology. 2003;125:1714–22. doi: 10.1053/j.gastro.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Bartholomew MM, Jansen RW, Jeffers LJ, Reddy KR, Johnson LC, Bunzendahl H, Condreay LD, Tzakis AG, Schiff ER, Brown NA. Hepatitis-B-virus resistance to lamivudine given for recurrent infection after orthotopic liver transplantation. Lancet. 1997;349:20–2. doi: 10.1016/S0140-6736(96)02266-0. [DOI] [PubMed] [Google Scholar]
- 10.Tipples GA, Ma MM, Fischer KP, Bain VG, Kneteman NM, Tyrrell DL. Mutation in HBV RNA-dependent DNA polymerase confers resistance to lamivudine in vivo. Hepatology. 1996;24:714–7. doi: 10.1002/hep.510240340. [DOI] [PubMed] [Google Scholar]
- 11.Fontana RJ, Hann HW, Perrillo RP, Vierling JM, Wright T, Rakela J, Anschuetz G, Davis R, Gardner SD, Brown NA. Determinants of early mortality in patients with decompensated chronic hepatitis B treated with antiviral therapy. Gastroenterology. 2002;123:719–27. doi: 10.1053/gast.2002.35352. [DOI] [PubMed] [Google Scholar]
- 12.Peters MG, Hann Hw H, Martin P, Heathcote EJ, Buggisch P, Rubin R, Bourliere M, Kowdley K, Trepo C, Gray Df D, Sullivan M, Kleber K, Ebrahimi R, Xiong S, Brosgart CL. Adefovir dipivoxil alone or in combination with lamivudine in patients with lamivudine-resistant chronic hepatitis B. Gastroenterology. 2004;126:91–101. doi: 10.1053/j.gastro.2003.10.051. [DOI] [PubMed] [Google Scholar]
- 13.Perrillo R, Hann HW, Mutimer D, Willems B, Leung N, Lee WM, Moorat A, Gardner S, Woessner M, Bourne E, Brosgart CL, Schiff E. Adefovir dipivoxil added to ongoing lamivudine in chronic hepatitis B with YMDD mutant hepatitis B virus. Gastroenterology. 2004;126:81–90. doi: 10.1053/j.gastro.2003.10.050. [DOI] [PubMed] [Google Scholar]
- 14.Rapti I, Dimou E, Mitsoula P, Hadziyannis SJ. Adding-on versus switching-to adefovir therapy in lamivudine-resistant HBeAg-negative chronic hepatitis B. Hepatology. 2007;45:307–13. doi: 10.1002/hep.21534. [DOI] [PubMed] [Google Scholar]
- 15.Schiff E, Lai CL, Hadziyannis S, Neuhaus P, Terrault N, Colombo M, Tillmann H, Samuel D, Zeuzem S, Villeneuve JP, Arterburn S, Borroto-Esoda K, Brosgart C, Chuck S. Adefovir dipivoxil for wait-listed and post-liver transplantation patients with lamivudine-resistant hepatitis B: final long-term results. Liver Transpl. 2007;13:349–60. doi: 10.1002/lt.20981. [DOI] [PubMed] [Google Scholar]
- 16.Lo CM, Liu CL, Lau GK, Chan SC, Ng IO, Fan ST. Liver transplantation for chronic hepatitis B with lamivudine-resistant YMDD mutant using add-on adefovir dipivoxil plus lamivudine. Liver Transplantation. 2005;11:807–13. doi: 10.1002/lt.20416. [DOI] [PubMed] [Google Scholar]
- 17.Schiff ER, Lai CL, Hadziyannis S, Neuhaus P, Terrault N, Colombo M, Tillmann HL, Samuel D, Zeuzem S, Lilly L, Rendina M, Villeneuve JP, Lama N, James C, Wulfsohn MS, Namini H, Westland C, Xiong S, Choy GS, Van Doren S, Fry J, Brosgart CL Behalf of the Adefovir Dipovoxil Study 435 International Investigators G. Adefovir dipivoxil therapy for lamivudine-resistant hepatitis B in pre- and post-liver transplantation patients. Hepatology. 2003;38:1419–27. doi: 10.1016/j.hep.2003.09.040. [DOI] [PubMed] [Google Scholar]
- 18.Sherman M, Yurdaydin C, Sollano J, Silva M, Liaw YF, Cianciara J, Boron-Kaczmarska A, Martin P, Goodman Z, Colonno R, Cross A, Denisky G, Kreter B, Hindes R. Entecavir for treatment of lamivudine-refractory, HBeAg-positive chronic hepatitis B. Gastroenterology. 2006;130:2039–49. doi: 10.1053/j.gastro.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 19.van Bommel F, Wunsche T, Mauss S, Reinke P, Bergk A, Schurmann D, Wiedenmann B, Berg T. Comparison of adefovir and tenofovir in the treatment of lamivudine-resistant hepatitis B virus infection. Hepatology. 2004;40:1421–5. doi: 10.1002/hep.20464. [DOI] [PubMed] [Google Scholar]
- 20.Peters MG, Andersen J, Lynch P, Liu T, Alston-Smith B, Brosgart CL, Jacobson JM, Johnson VA, Pollard RB, Rooney JF, Sherman KE, Swindells S, Polsky B. Randomized controlled study of tenofovir and adefovir in chronic hepatitis B virus and HIV infection: ACTG A5127. Hepatology. 2006;44:1110–6. doi: 10.1002/hep.21388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong SN, Reddy KR, Keeffe EB, Han SH, Gaglio PJ, Perrillo RP, Tran TT, Pruett TL, Lok AS. Comparison of clinical outcomes in chronic hepatitis B liver transplant candidates with and without hepatocellular carcinoma. Liver Transpl. 2007;13:334–42. doi: 10.1002/lt.20959. [DOI] [PubMed] [Google Scholar]
- 22.UNOS. Policies and Bylaws. Vol. 2007. 2006. [Google Scholar]
- 23.Allen MI, Deslauriers M, Andrews CW, Tipples GA, Walters KA, Tyrrell DL, Brown N, Condreay LD. Identification and characterization of mutations in hepatitis B virus resistant to lamivudine. Lamivudine Clinical Investigation Group. Hepatology. 1998;27:1670–7. doi: 10.1002/hep.510270628. [DOI] [PubMed] [Google Scholar]
- 24.Angus P, Vaughan R, Xiong S, Yang H, Delaney W, Gibbs C, Brosgart C, Colledge D, Edwards R, Ayres A, Bartholomeusz A, Locarnini S. Resistance to adefovir dipivoxil therapy associated with the selection of a novel mutation in the HBV polymerase. Gastroenterology. 2003;125:292–7. doi: 10.1016/s0016-5085(03)00939-9. [DOI] [PubMed] [Google Scholar]
- 25.Hussain M, Fung S, Libbrecht E, Sablon E, Cursaro C, Andreone P, Lok AS. Sensitive line probe assay that simultaneously detects mutations conveying resistance to lamivudine and adefovir. J Clin Microbiol. 2006;44:1094–7. doi: 10.1128/JCM.44.3.1094-1097.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen CH, Lee CM, Lu SN, Wang JH, Tung HD, Hung CH, Chen WJ, Changchien CS. Comparison of clinical outcome between patients continuing and discontinuing lamivudine therapy after biochemical breakthrough of YMDD mutants. J Hepatol. 2004;41:454–61. doi: 10.1016/j.jhep.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 27.Lampertico P, Vigano M, Manenti E, Iavarone M, Lunghi G, Colombo M. Adefovir rapidly suppresses hepatitis B in HBeAg-negative patients developing genotypic resistance to lamivudine. Hepatology. 2005;42:1414–9. doi: 10.1002/hep.20939. [DOI] [PubMed] [Google Scholar]
- 28.Leung NW, Lai CL, Chang TT, Guan R, Lee CM, Ng KY, Lim SG, Wu PC, Dent JC, Edmundson S, Condreay LD, Chien RN On behalf of the Asia Hepatitis Lamivudine Study G. Extended lamivudine treatment in patients with chronic hepatitis B enhances hepatitis B e antigen seroconversion rates: results after 3 years of therapy. Hepatology. 2001;33:1527–32. doi: 10.1053/jhep.2001.25084. [DOI] [PubMed] [Google Scholar]