Objective
Antenatal hydronephrosis (ANH) affects approximately 1% of pregnancies.1 Controversies exist as to the postnatal investigation and management of these children. The CUA Guidelines Committee has reviewed the updated literature to provide recommendations.
ANH as a predictor of postnatal pathology/need for further investigation
ANH can represent a number of renal pathologies, the most common being ureteropelvic junction obstruction (UPJO), vesico–ureteral reflux (VUR), posterior urethral valves (PUV) and ureteral–vesical junction obstruction (UVJO).2 Anterior–Posterior Diameter (APD) is the most common method for reporting antenatal ANH. The grades of ANH have been defined as follows (Table 1).2
Table 1.
Definition of the grades of antenatal hydronephrosis
| ANH grade | APD second trimester, mm | APD third trimester, mm | % with postnatal pathology |
|---|---|---|---|
| Mild | ≤ 7 | ≤ 9 | 12 |
| Moderate | 7–10 | 9–15 | 45 |
| Severe | > 10 | > 15 | 88 |
| All | — | — | 36 |
ANH = antenatal hydronephrosis; APD = anterior–posterior diameter.
Note: The antenatal follow-up of ANH is determined by the severity of the diagnosis. For example, patients with renal or bladder ultrasound signs suggestive of posterior urethral valves (males with bilateral ANH, dilated ureters or dilated thick-walled bladder) require formal prenatal follow-up by fetal–maternal medicine.1
Postnatal interventions, investigations and timing
Prophylactic antibiotics
The role of prophylactic antibiotics in children with ANH who are awaiting completion of post-natal investigations is controversial. Children with ANH have been shown to have a significantly higher risk of developing a urinary tract infection (UTI) than controls.3 While it is believed that prophylactic antibiotics will prevent urinary tract infections in children with VUR, it has yet to be proven.4 Therefore, some recommend institution of prophylactic antibiotics at birth;1,5 others instead recommend a low threshold for investigation and treatment of a suspected UTI.3 Commonly used prophylaxes in the neonate include amoxicillin1 50 mg per day and cephalexin6 50 mg per day. Trimethoprim-sulfamatholxazole1 and nitrofurantoin7 should NOT be used in the neonate.
Renal ultrasound (RUS)
RUS allows reassessment of the grade of ANH and may point toward a distinct etiology.
Timing
All children with ANH should have a postnatal RUS. Children with bilateral severe ANH, and children with ANH of any degree in a solitary kidney should have a postnatal RUS prior to discharge from hospital.2 However, ideally, the first post-natal RUS should not be performed within the first 48–72 hours, as relatively low urine output during this period may underestimate the degree of hydronephrosis.1 Therefore, in this situation, if the RUS is normal and the serum creatinine is dropping appropriately, a repeat RUS should be performed the following week. The remainder of children with ANH should have a RUS performed between 7 and 30 days.1,2
Grading
Postnatally, a commonly used system to grade hydronephrosis is that of the Society of Fetal Urology (SFU). The SFU grading system is as follows.8
| Grade | Characteristics of central renal echo complex |
| 0 | Closely apposed |
| 1 | Slight separation |
| 2 | Further separation; one or few calyces may be visualized |
| 3 | Pelviectasis and fluid filled calyces seen throughout kidney |
| 4 | Grade 3 with parenchyma over calyces thinned |
Only grades 3 and 4 are felt to be clinically significant with respect to obstruction.1
All grades of ANH have an increased risk of associated VUR (8.5–15%).2,9 Unlike with obstruction, the grade of ANH does not positively correlate with the likeliness of diagnosing VUR.2
Voiding cystourethrogram (VCUG)
VCUG is the preferred investigation to diagnose and grade VUR. It also allows for anatomical assessment of the urethra (to rule out PUV) and bladder.
Timing and selection
An urgent VCUG before discharge from hospital is essential in any child with ANH where there is a prenatal concern of bladder outlet obstruction (ex: PUV).1 Other absolute indications for a VCUG to investigate ANH include: severe bilateral hydronephrosis (urgent), suspected infravesical obstruction (urgent), dilated ureter, duplex kidney, abnormal echogenicity and abnormal bladder (less urgently, around one month of age).1
Controversy exists around whether children with SFU 0–2 on postnatal RUS should get a VCUG. Reflux will be found in approximately 15%9 of these children in comparison to 1% in the general population.2 What is debated is whether this VUR is clinically significant and in need of being diagnosed.
Children with persistent moderate or severe hydronephrosis should be investigated with a VCUG.2 If VUR is found, it will be of high grade. Additionally, if the refluxed contrast drains freely, concomitant UPJO can be ruled out.
Diuretic renography (DTPA or MAG-3)
DTPA or MAG-3 may help to diagnose, or rule out obstructive uropathy. Unfortunately, diuretic renography is not completely reliable in infants.1,10 However, if the scan suggests obstruction, differential function is a useful tool to determine the need for surgical intervention.1
Timing and selection
SFU grade 3–4 hydronephrosis that is not explained by VUR should be investigated further with diuretic renography at 4–6 weeks of age.1
Need for further investigations following completion of initial investigations
If the initial postnatal RUS shows only isolated SFU 0–2 ANH, and a VCUG is performed, showing no VUR, it is unlikely that the hydronephrosis will become significant. However, some advocate another ultrasound at 6 months.5 While many physicians (and likely parents) would like to see improvement, or confirm stability with a repeat RUS at 6 months, particularly in those with SFU 1–2, it is not clear if this is necessary. However, the event of a systemic urinary tract infection should stimulate re-evaluation, which may include diuretic renography.5
If the initial postnatal RUS shows SFU 0–2 ANH and one elects not to perform a VCUG, reflux may still exist and there is a need to ensure that the parents are vigilant regarding prompt assessment if signs of a UTI develop.6 The event of a systemic UTI should stimulate a VCUG being performed. The role for further RUSs in these children is also unclear.
SFU III–IV ANH in the absence of VUR requires ongoing observation with serial RUSs and judicious use of diuretic renography. The details of such observation are beyond the scope of this guideline. These children should be referred to a pediatric urologist.
The follow-up and management of diagnosed UPJO and VUR are beyond the scope of this guideline.
Summary
-
All ANH should be investigated with a post-natal RUS.2
Level 1 Evidence: Grade A Recommendation
-
The role of prophylactic antibiotics initiated at birth is controversial.
Grade D Recommendation
-
The need to further investigate mild postnatal hydronephrosis (SFU 0–II) with a VCUG is controversial, and depends on the physician’s attitude toward diagnosing asymptomatic VUR.
Grade D Recommendation
-
The need to reassess mild postnatal hydronephrosis with a second RUS is unclear, but does provide reassurance to the physician and parent if the ANH remains stable or improves.
Level 4 Evidence: Grade C Recommendation
-
Persistent moderate or severe hydronephrosis (SFU III–IV) should be investigated with a VCUG, followed by diuretic renography if the hydronephrosis cannot be explained by VUR.1
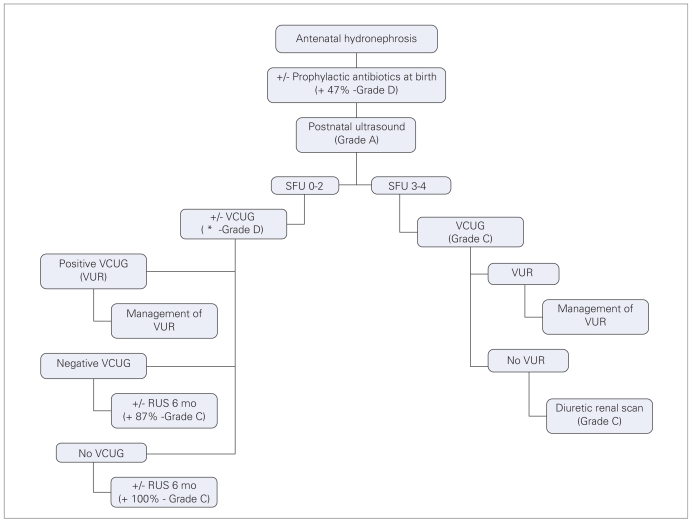
Level 4 Evidence: Grade C Recommendation A summary flow chart is provided (Fig. 1). To assist in the decision-making of controversial areas, members of the Pediatric Urologists of Canada were surveyed in 2007 to determine most common practice patterns. The results, based on the responses of 15 Canadian members, are included in the flow chart.
Fig 1.
Summary flow chart of Levels of Evidence and Grade recommendations for evaluating antenatal hydronephrosis. *93% would not order a voiding cystourethrogram (VCUG) if Society of Fetal Urology (SFU) 0; 80% would not order a VCUG for SFU I; 73% would order or consider ordering a VCUG for SFU II. VUR = vesico–ureteral reflux; RUS = renal ultrasound.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
References
- 1.Belarmino JM, Kogan BA. Management of neonatal hydronephrosis. Early Hum Dev. 2006;82:9–14. doi: 10.1016/j.earlhumdev.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Lee RS, Cendron M, Kinnamon DD, et al. Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatr. 2006;118:586–93. doi: 10.1542/peds.2006-0120. [DOI] [PubMed] [Google Scholar]
- 3.Harding LJ, Malone PSJ, Wellesley DG. Antenatal minimal hydronephrosis: is its follow-up an unnecessary cause of concern? Prenat Diagn. 1999;19:701–5. doi: 10.1002/(sici)1097-0223(199908)19:8<701::aid-pd621>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 4.Garin EH, Olavarria F, Nieto VG, et al. Clinical significance of primary vesicoureteric reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatr. 2006;117:626–32. doi: 10.1542/peds.2005-1362. [DOI] [PubMed] [Google Scholar]
- 5.Aksu N, Yavascan O, Kangin M, et al. Postnatal management of infants with antenatally detected hydronephrosis. Pediatr Nephrol. 2005;20:1253–9. doi: 10.1007/s00467-005-1989-3. [DOI] [PubMed] [Google Scholar]
- 6.Hallerstein S, Nickell E. Prophylactic antibiotics in children at risk for urinary tract infection. Pediatr Nephrol. 2002;17:506–10. doi: 10.1007/s00467-002-0899-x. [DOI] [PubMed] [Google Scholar]
- 7.Consult MD. [(accessed 2008 Mar 18)]; Available: www.mdconsult.com.
- 8.Fernbach SK, Maizels M, Conway JJ. Ultrasound grading of hydronephrosis: introduction to the system used by the Society of Fetal Urology. Pediatr Radiol. 1993;23:478–80. doi: 10.1007/BF02012459. [DOI] [PubMed] [Google Scholar]
- 9.Gloor JM, Ramsey PS, Ogburn PL, Jr, et al. J Matern Fetal Neonatal Med. 2002;12:196–200. doi: 10.1080/jmf.12.3.196.200. [DOI] [PubMed] [Google Scholar]
- 10.Koff SA, Binkovitz L, Coley B, et al. Renal pelvis volume during diuresis in children with hydronephrosis: implications for diagnosing obstruction with diuretic renography. J Urol. 2005;174:303–7. doi: 10.1097/01.ju.0000161217.47446.0b. [DOI] [PubMed] [Google Scholar]