Abstract
OBJECTIVE—The prevalence of abdominal obesity exceeds that of general obesity. We sought to determine the prevalence of abdominal subcutaneous and visceral obesity and to characterize the different patterns of fat distribution in a community-based sample.
RESEARCH DESIGN AND METHODS—Participants from the Framingham Heart Study (n = 3,348, 48% women, mean age 52 years) underwent multidetector computed tomography; subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) volumes were assessed. Sex-specific high SAT and VAT definitions were based on 90th percentile cut points from a healthy referent sample. Metabolic risk factors were examined in subgroups with elevated SAT and VAT.
RESULTS—The prevalence of high SAT was 30% (women) and 31% (men) and that for high VAT was 44% (women) and 42% (men). Overall, 27.8% of the sample was discordant for high SAT and high VAT: 19.9% had SAT less than but VAT equal to or greater than the 90th percentile, and 7.9% had SAT greater than but VAT less than the 90th percentile. The prevalence of metabolic syndrome was higher among women and men with SAT less than the 90th percentile and high VAT than in those with high SAT but VAT less than the 90th percentile, despite lower BMI and waist circumference. Findings were similar for hypertension, elevated triglycerides, and low HDL cholesterol.
CONCLUSIONS—Nearly one-third of our sample has abdominal subcutaneous obesity, and >40% have visceral obesity. Clinical measures of BMI and waist circumference may misclassify individuals in terms of VAT and metabolic risk.
Obesity is associated with an increased risk of multiple cardiometabolic risk factors. The prevalence of obesity in the U.S. has increased over the last two decades, with one-third of adults having a BMI ≥30 kg/m2 (1). However, obesity is a heterogeneous condition with individual differences in the pattern of adipose tissue deposition. Accumulation of abdominal fat, particularly in the visceral compartment, may confer the majority of obesity-associated health risks (2).
The prevalence of abdominal obesity (defined as waist circumference ≥88 cm in women and ≥102 cm in men) has increased over the last decade and now exceeds the prevalence of overall obesity, with rates of 42.4% in men and 61.3% in women (1,3). Notably, the largest relative increase in the prevalence of abdominal obesity has been among individuals with BMI <30 kg/m2 (3). Although waist circumference is an easily obtainable index of abdominal adiposity, it does not distinguish between the subcutaneous and visceral adipose tissue compartments. We and others have previously reported that visceral adipose tissue (VAT) has a stronger association with metabolic risk factors and metabolic syndrome than subcutaneous adipose tissue (SAT) (4–6). These studies are limited, however, by the high correlations between SAT and VAT that make it difficult to distinguish between the contribution of SAT compared with that of VAT with regard to metabolic risk.
Thus, the objectives of the present study were twofold. First, we sought to define the prevalence of abdominal obesity in terms of elevated volumes of VAT and SAT, as measured by a volumetric computed tomography (CT) method. To do this, we developed cut points for elevated SAT and VAT based on a healthy referent sample. Second, we examined the occurrence of different patterns of adipose tissue distribution and concomitant metabolic risk factor profiles. We hypothesized that metabolic risk factors would be more likely to track with elevated levels of VAT than with SAT.
RESEARCH DESIGN AND METHODS
The study sample consisted of women and men enrolled in the community-based Framingham Heart Study Offspring and Third Generation cohorts who participated in a multidetector computed tomography (MDCT) substudy. As part of the MDCT substudy, 3,529 participants (2,111 Third Generation and 1,418 Offspring participants) underwent MDCT scanning of the chest and abdomen for assessment of coronary and aortic calcium between June 2002 and April 2005. Of the total 3,529 subjects imaged, 3,371 had interpretable CT measures and 3,348 had both SAT and VAT measured, resulting in a total sample size of 3,348 individuals for the present investigation.
The study protocol was approved by the institutional review boards of the Boston University Medical Center and Massachusetts General Hospital. All subjects provided written informed consent.
Additional details regarding the study sample selection, abdominal adipose tissue imaging and volumetric measurements, risk factor assessment, and statistical analysis can be found in the supplemental methods (available in an online appendix at http://dx.doi.org/10.2337/dc08-1359).
RESULTS
Overall, 1,611 women and 1,737 men were available for analysis; study sample characteristics are shown in Table 1. SAT and VAT percentiles in women and men by age are shown in supplemental Table A1.
Table 1.
Clinical characteristics of overall sample
| Women | Men | |
|---|---|---|
| n | 1,611 | 1,737 |
| Age (years) | 52.2 ± 9.9 | 49.8 ± 10.7 |
| BMI (kg/m2) | 27.1 ± 5.8 | 28.4 ± 4.5 |
| Waist circumference (cm) | 93 ± 15 | 101 ± 12 |
| Low HDL cholesterol (%)* | 26 | 33 |
| Elevated triglycerides (%)† | 27 | 44 |
| Hypertension (%) | 26.8 | 32.0 |
| Impaired fasting glucose (%)‡ | 19 | 40 |
| Diabetes (%) | 5.6 | 7.4 |
| Metabolic syndrome (%) | 28 | 38 |
| CVD (%) | 4.3 | 7.8 |
| Hypertension treatment (%) | 18.7 | 19.8 |
| Lipid treatment (%) | 10.7 | 17.7 |
| Diabetes treatment (%) | 3.3 | 3.9 |
| SAT (cm3) | 3,148 ± 1,519 | 2,640 ± 1,206 |
| VAT (cm3) | 1,365 ± 832 | 2,243 ± 1,023 |
Data are means ± SD or %.
Low HDL defined as <40 mg/dl (men) and <50 (women).
Elevated triglycerides defined as ≥150 mg/dl or lipid treatment.
Defined as fasting plasma glucose 100–125 mg/dl in the absence of diabetes treatment.
Healthy referent group
The healthy referent sample was composed of 471 women and 285 men. The 90th percentile cutoffs of SAT and VAT for this healthy referent group were 3,735 and 1,359 cm3, respectively, in women and 2,979 and 2,323 cm3 in men.
Prevalence of elevated SAT and VAT
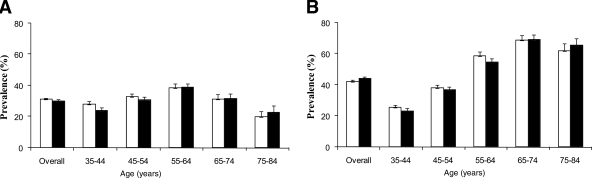
The prevalence of subcutaneous abdominal obesity (high SAT) in the overall sample was 30% in women and 31% in men. The prevalence of visceral obesity (high VAT) was 44% in women and 42% in men. The prevalence of high SAT and high VAT by age-group is presented in Fig. 1.
Figure 1.
Prevalence of high SAT (A) and high VAT (B) by age-group in women (▪) and men (□). Error bars represent SE. For SAT, the linear trends were not significant (P = 0.76 for men and P = 0.11 for women). For VAT, the linear trends were significant for both men (P < 0.0001) and women (P < 0.0001).
In a secondary analysis, the lean healthy referent (further excluding individuals with BMI ≥25 kg/m2) 90th percentile cut points in this sample were 2,883 and 2,031 cm3 for SAT and 1,062 and 1,715 cm3 for VAT in women and men, respectively. Applying these cut points to the overall sample would result in the prevalence of high SAT of 50% in women and 66% in men and high VAT of 56% in women and 67% in men.
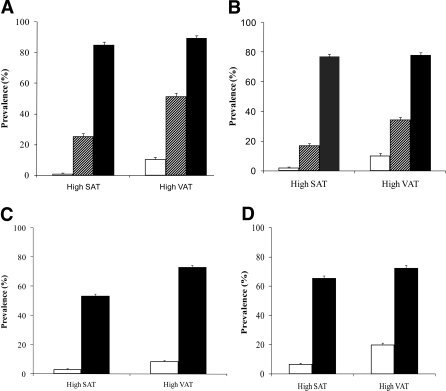
Prevalence of high SAT and high VAT by BMI and waist circumference categories
The prevalence of high SAT and VAT increased with increasing BMI category (Fig. 2A). Among obese individuals, 22% of men and 10% of women did not have high VAT. Similarly, among individuals with a high waist circumference, 28% of men and 27% of women did not have high VAT (Fig. 2B). Conversely, 10% of men and 11% of women who are of normal BMI had high VAT, and 22% of men and 8% of women with a normal waist circumference had high VAT.
Figure 2.
Prevalence of high SAT or high VAT by BMI category in women (A) and men (B) and by waist circumference category in women (C) and men (D). Error bars represent SE. A and B: □, normal weight;  , overweight; ▪, obese. C and D: □, normal waist circumference; ▪, high waist circumference.
, overweight; ▪, obese. C and D: □, normal waist circumference; ▪, high waist circumference.
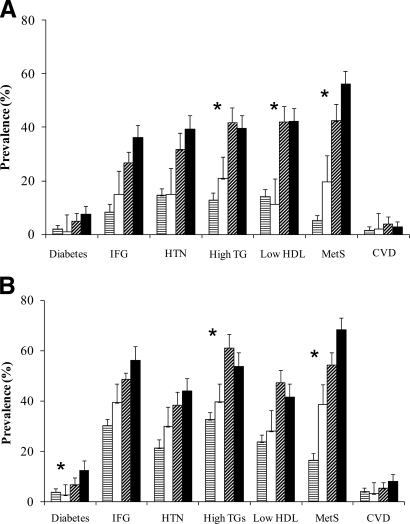
Metabolic risk factor prevalence among SAT and VAT subgroups
The prevalence of metabolic syndrome was significantly different across the four SAT/VAT groups (P < 0.0001 across the four groups) (Fig. 3); clinical characteristics of these groups are shown in Table 2. Overall, 49.3% of the sample had both SAT and VAT <90th percentile, whereas 22.9% had both high SAT and VAT. Nearly 28% of the sample was discordant in terms of SAT and VAT: 7.9% had high SAT and VAT <90th percentile, whereas 19.9% had SAT <90th percentile but high VAT. The mean age was higher among those with SAT <90th percentile and high VAT compared with those with high SAT and VAT <90th percentile. The prevalence of metabolic syndrome was higher among those with SAT <90th percentile and high VAT compared with the group with high SAT and VAT <90th percentile (Fig. 3); similar patterns were noted for elevated triglycerides and low HDL cholesterol. This pattern was not explained by a higher body weight or abdominal girth in the group with SAT <90th percentile but with high VAT: those with SAT <90th percentile and high VAT had a lower BMI and smaller waist circumference. Results for cardiovascular disease (CVD) prevalence by the four SAT/VAT groups are presented in Fig. 3.
Figure 3.
Prevalence of metabolic risk factors (MetS) and CVD by SAT/VAT concordant and discordant categories in women (A) and men (B). Age-adjusted P < 0.0001 across all four categories for each risk factor except cardiovascular disease (P = 0.01 for men and P = 0.05 for women). *P < 0.01 for the low SAT/high VAT and high SAT/low VAT comparisons. Error bars represent upper one-sided 97.5% CIs. HTN, hypertension; IFG, impaired fasting glucose; TG, triglyceride.  , low SAT and VAT; □, high SAT and low VAT;
, low SAT and VAT; □, high SAT and low VAT;  , low SAT and high VAT; ▪, high SAT and VAT.
, low SAT and high VAT; ▪, high SAT and VAT.
Table 2.
Distribution of risk factors and clinical characteristics by SAT/VAT categories*
| Risk factor | Low SAT/low VAT | High SAT/low VAT | Low SAT/high VAT | High SAT/high VAT | P value comparing discordant SAT and VAT | P value across groups |
|---|---|---|---|---|---|---|
| n | 1,650 | 266 | 666 | 766 | ||
| Men | ||||||
| Age (years) | 49 | 47 | 58 | 54 | <0.0001 | <0.0001 |
| BMI (kg/m2) | 25.6 | 30.2 | 28.5 | 34.0 | <0.0001 | <0.0001 |
| Waist circumference (cm) | 93 | 107 | 101 | 116 | <0.0001 | <0.0001 |
| SAT (cm3) | 1,861 | 3,753 | 2,317 | 4,190 | <0.0001 | <0.0001 |
| VAT (cm3) | 1,532 | 1,898 | 2,959 | 3,315 | <0.0001 | <0.0001 |
| Women | ||||||
| Age (years) | 51 | 51 | 61 | 56 | <0.0001 | <0.0001 |
| BMI (kg/m2) | 23.2 | 29.5 | 27.1 | 34.4 | <0.0001 | <0.0001 |
| Waist circumference (cm) | 83 | 99 | 95 | 112 | 0.0002 | <0.0001 |
| SAT (cm3) | 2,088 | 4,530 | 2,955 | 5,157 | <0.0001 | <0.0001 |
| VAT (cm3) | 773 | 1,103 | 1,831 | 2,283 | <0.0001 | <0.0001 |
SAT and VAT categories are defined as high if ≥90th percentile cut points in healthy referent sample: SAT, men = 2,979 cm3; women = 3,735 cm3; VAT, men = 2,323 cm3; women = 1,359 cm3.
CONCLUSIONS
Major findings
Volumetric measures of both SAT and VAT revealed a prevalence of high SAT of ∼30% and a prevalence of high VAT of just more than 40% as defined by 90th percentile cut points in a healthy referent sample. The prevalence of elevated VAT rises with age, whereas elevated SAT declines among elderly individuals. Nearly one-quarter of obese individuals or individuals with a large waist do not have elevated VAT, whereas 10% of women and 20% of men with a normal waist circumference have high VAT, suggesting that misclassification exists within clinically useful adiposity categories. Discordant amounts of SAT and VAT exist in nearly 30% of our sample, and adverse metabolic risk factor profiles are more likely to track with those with elevated VAT compared with elevated SAT. Last, among these discordant obesity subgroups, BMI and waist circumference were actually lower among higher risk groups.
We secondarily evaluated a “lean healthy referent” sample and found that the prevalence of elevated VAT and SAT was even higher than that for the sample that included overweight individuals in the healthy referent sample. Given that the lean healthy referent sample excluded overweight individuals, this result is not surprising. However, the lean healthy referent sample consisted of <500 individuals, and the robustness of these estimates is not clear.
The prevalence of elevated SAT declines with age, whereas elevated VAT rises among older individuals. These findings are consistent with the observation that the aging process is associated with loss of subcutaneous fat and gain of fat accumulation in the visceral depot. Despite more visceral fat but less subcutaneous fat among older individuals, BMI actually declines with age (7) primarily because of loss of fat-free mass and fat mass. Both BMI and waist circumference are more strongly correlated with subcutaneous than with visceral fat (4). Therefore, both anthropometric measures may be less reliable in aging individuals, as BMI and waist circumference may be more dependent on the relative loss of SAT over time. This is consistent with the observation in the present article that although individuals with high VAT and SAT <90th percentile had more adverse risk factor profiles, BMI and waist circumference were actually lower compared with those in individuals with high SAT and VAT <90th percentile.
In the context of the current literature
In our cohort, the prevalence of subcutaneous adiposity is ∼30%, which is consistent with current estimates of the prevalence of obesity (as defined by a BMI of at least 30 kg/m2) of 32.2% in U.S. adults (1). The prevalence of visceral obesity in our sample (42% in men and 44% in women) exceeds the prevalence of subcutaneous adiposity. Of note, the prevalence of abdominal obesity in women (defined by a waist circumference >88 cm) in National Health and Nutrition Examination Survey data is higher than the prevalence of visceral obesity (defined by VAT ≥90th percentile healthy referent cut point) in our sample of women (61.3 vs. 44%). This difference was not observed in men. However, clinical anthropometrics are well-known to be poor for estimating VAT, and, thus, it is not surprising that there is a discrepancy between a prevalence based on waist circumference and one based on more precise CT measurements (8).
Clinical categories to classify BMI and waist circumference are useful for predicting risk of adiposity-related disorders in the majority of patients, but misclassification exists (9). Some individuals who have normal BMI and normal waist circumference have an excessive amount of visceral fat that is unrecognized and thus have a significant cardiometabolic risk. This phenotype of a metabolically obese normal-weight individual was first described in the 1980s by Ruderman et al. (10) and was classified as an individual with a nonobese BMI who showed evidence of impaired insulin sensitivity with a hyperinsulinemic-euglycemic clamp. Conversely, the metabolically healthy obese individual (11) represents individuals with a high BMI who seem to be protected from associated metabolic derangements including insulin resistance. These different phenotypes underscore the importance of identifying and treating cardiometabolic risk factors, irrespective of BMI.
To further explore the existence of different fat phenotypes in a community-based setting, we looked at groups that were discordant for SAT and VAT and found that the group with low SAT but high VAT had a greater prevalence of metabolic syndrome than the group with high SAT but low VAT. The collinearity of SAT and VAT (correlations ranging between 0.58 in men and 0.71 in women) (4) makes it difficult to assess the differential contribution of SAT compared with VAT with regard to metabolic risk. However, the examination of risk factors among discordant categories of high SAT and high VAT in our study suggests that a more adverse risk factor profile tracks with high VAT than with high SAT. This suggestion is supported by the extensive literature suggesting a uniquely important contribution of visceral fat to metabolic risk and a correlation of excess VAT with metabolic risk independent of SAT (12–16). Nonetheless, it is important to note that the mean BMI and waist circumference were actually lower among participants with elevated VAT and normal SAT, highlighting the potential misclassification in clinical anthropometrics.
Compared with the high SAT and high VAT group, the low SAT and high VAT group had a higher prevalence of hypertriglyceridemia. These findings may be consistent with a pattern similar to the metabolic abnormalities present in partial lipodystrophy. The lack of sufficient adipocytes and the limited capacity to store fat in nonlipodystrophic adipose tissue may result in ectopic fat storage around other tissues and organs such as the heart, the liver, skeletal muscles, blood vessels, and kidneys (17,18). This ectopic fat storage may lead to organ dysfunction (19).
Implications: limitations of BMI and waist circumference, particularly among older individuals
Clinical categories of BMI and waist circumference may be useful to estimate overall metabolic risk in the general population, but there may be individuals who develop cardiometabolic complications related to adiposity without a BMI or waist circumference in the high-risk range. In particular, we observed that among individuals discordant for high SAT and VAT, BMI and waist circumference were actually lower among those with high VAT and low SAT, despite having a higher prevalence of metabolic risk factors. Therefore, the reliance on BMI and waist circumference in the aging population may misclassify metabolic risk.
Strengths and limitations
Strengths of our study include the use of a large community-based sample with detailed risk factor assessment. We used a highly reproducible CT assessment of SAT and VAT volumes, which accounts for heterogeneity of fat distribution throughout the abdomen. Our sample size was large enough to explore differences within obesity subgroups. Our study is a population-based epidemiologic study without ascertainment for obesity-related conditions, which increases the generalizability of our findings. Limitations include the use of cross-sectional data, as causality cannot be inferred. Because the Framingham Offspring study is primarily a Caucasian sample, generalizability to other races or ethnic groups is uncertain.
In summary, nearly one-third of our sample has abdominal subcutaneous obesity and more than 40% have visceral obesity. Different patterns of adipose tissue distribution have different metabolic correlates. Clinical measures of BMI and waist circumference may misclassify individuals in terms of metabolic risk.
Supplementary Material
Acknowledgments
The Framingham Heart Study is supported by the National Heart, Lung, and Blood Institute (NHLBI) (N01-HC-25195). R.S.V. is supported in part by 2K24HL04334 (NHLBI/National Institutes of Health).
No potential conflicts of interest relevant to this article were reported.
Published ahead of print at http://care.diabetesjournals.org on 15 December 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL: Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288:1723–1727, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Bjorntorp P: Metabolic implications of body fat distribution. Diabetes Care 14:1132–1143, 1991 [DOI] [PubMed] [Google Scholar]
- 3.Li C, Ford ES, McGuire LC, Mokdad AH: Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring) 15:216–224, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB Sr, O'Donnell CJ: Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116:39–48, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, Nevitt M, Holvoet P, Newman AB: Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med 165:777–783, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Pascot A, Lemieux S, Lemieux I, Prud’homme D, Tremblay A, Bouchard C, Nadeau A, Couillard C, Tchernof A, Bergeron J, Despres JP: Age-related increase in visceral adipose tissue and body fat and the metabolic risk profile of premenopausal women. Diabetes Care 22:1471–1478, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Rissanen A, Heliovaara M, Aromaa A: Overweight and anthropometric changes in adulthood: a prospective study of 17,000 Finns. Int J Obes 12:391–401, 1988 [PubMed] [Google Scholar]
- 8.Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ: Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol 73:460–468, 1994 [DOI] [PubMed] [Google Scholar]
- 9.Ross R, Rissanen J, Hudson R: Sensitivity associated with the identification of visceral adipose tissue levels using waist circumference in men and women: effects of weight loss. Int J Obes Relat Metab Disord 20:533–538, 1996 [PubMed] [Google Scholar]
- 10.Ruderman NB, Schneider SH, Berchtold P: The “metabolically-obese,” normal-weight individual. Am J Clin Nutr 34:1617–1621, 1981 [DOI] [PubMed] [Google Scholar]
- 11.Karelis AD, St. Pierre DH, Conus F, Rabasa-Lhoret R, Poehlman ET: Metabolic and body composition factors in subgroups of obesity: what do we know? J Clin Endocrinol Metab 89:2569–2575, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, Adams PW: Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab 54:254–260, 1982 [DOI] [PubMed] [Google Scholar]
- 13.Carr DB, Utzschneider KM, Hull RL, Kodama K, Retzlaff BM, Brunzell JD, Shofer JB, Fish BE, Knopp RH, Kahn SE: Intra-abdominal fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III criteria for the metabolic syndrome. Diabetes 53:2087–2094, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Goodpaster BH, Krishnaswami S, Resnick H, Kelley DE, Haggerty C, Harris TB, Schwartz AV, Kritchevsky S, Newman AB: Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care 26:372–379, 2003 [DOI] [PubMed] [Google Scholar]
- 15.Brochu M, Tchernof A, Turner AN, Ades PA, Poehlman ET: Is there a threshold of visceral fat loss that improves the metabolic profile in obese postmenopausal women? Metabolism 52:599–604, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Vega GL, Adams-Huet B, Peshock R, Willett D, Shah B, Grundy SM: Influence of body fat content and distribution on variation in metabolic risk J Clin Endocrinol Metab91:4459–4466, 2006 [DOI] [PubMed]
- 17.Garg A: Adipose tissue dysfunction in obesity and lipodystrophy. Clin Cornerstone 8 (Suppl 4):S7–S13, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Unger RH: The physiology of cellular liporegulation. Annu Rev Physiol 65:333–347, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Montani JP, Carroll JF, Dwyer TM, Antic V, Yang Z, Dulloo AG: Ectopic fat storage in heart, blood vessels and kidneys in the pathogenesis of cardiovascular diseases. Int J Obes Relat Metab Disord 28 (Suppl 4):S58–S65, 2004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.