Abstract
OBJECTIVE— The purpose of this study was to assess the relationship between lifestyle factors and abdominal subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) in a community-based setting.
RESEARCH DESIGN AND METHODS— Cross-sectional associations between lifestyle factors (dietary quality, physical activity, smoking, and alcohol consumption) and SAT and VAT volumes were examined in 2,926 Framingham Heart Study participants (48.6% women, aged 50 ± 10 years).
RESULTS— Diets consistent with the 2005 Dietary Guidelines Adherence Index and greater physical activity were inversely associated with SAT and VAT (P < 0.0001–0.002). In men, former smoking was associated with higher SAT (2,743 ± 56 cm3) compared with current smokers (2,629 ± 88 cm3) or those who never smoked (2,538 ± 44 cm3; P = 0.02). Both former and current smoking was associated with higher VAT (P = 0.03 [women]; P = 0.005 [men]). Women with high amounts of alcohol intake (>7 drinks/week) had lower SAT (2,869 ± 106 cm3) than those who consumed less alcohol (3,184 ± 44 cm3, P = 0.006); significant differences in VAT were not observed (P = 0.18). In men, high amounts of alcohol intake (>14 drinks/week) were associated with higher VAT (2,272 ± 59 cm3) compared with intake of ≤14 drinks/week (2,139 ± 25 cm3, P = 0.04), whereas SAT did not differ (P = 0.91). An increasing number of healthy lifestyle factors were associated with lower SAT and VAT volumes (all P < 0.003).
CONCLUSIONS— Adherence to recommended dietary guidelines and physical activity are associated with lower SAT and VAT volumes. However, both smoking and high alcohol intake are differentially associated with VAT volumes. Further research to uncover the putative mechanisms is warranted.
Abdominal adiposity is strongly associated with metabolic and cardiovascular disease (CVD) risk (1) and all-cause mortality (2). Visceral adipose tissue (VAT) in particular may be a pathogenic fat compartment (3). Numerous studies have demonstrated that central obesity is associated with lifestyle factors (4–6). However, the majority of these studies used waist circumference as a proxy for abdominal obesity, which does not allow for the differentiation between subcutaneous adipose tissue (SAT) and VAT. As VAT is more strongly associated with metabolic risk factors than SAT (3), it is important to identify whether VAT is more correlated with lifestyle factors. This information may provide more understanding of the relationship between a healthy lifestyle and VAT and the contribution of individual lifestyle factors to cardiometabolic risk.
Thus, the aim of the present study was to examine the relation between lifestyle factors (dietary quality, physical activity, smoking, and alcohol consumption) and SAT and VAT volumes, as assessed by multidetector computed tomography (MDCT), in a large population-based cohort of women and men free of CVD.
RESEARCH DESIGN AND METHODS
Participants for this study were part of the Framingham Heart Study MDCT Study, a substudy of the population-based Framingham Heart Offspring and Third Generation study cohorts. Starting in 1948, 5,209 men and women were enrolled in the original cohort of the Framingham Heart Study. In 1971, the offspring and spouses of the offspring of the original cohort enrolled in the Framingham Offspring Study. Selection criteria and study design have been described previously (7). Beginning in 2002, 4,095 adults who had at least one parent in the Offspring cohort were enrolled in the Framingham Heart Study Third Generation cohort and underwent standard clinic examinations (8). The examination included a physician interview, a physical examination, and laboratory tests. The study sample for the current study consisted of women and men from the Offspring and Third Generation study cohorts who participated in the MDCT study. The study protocol was approved by the institutional review boards of Boston University Medical Center and Massachusetts General Hospital. All subjects provided written informed consent before study participation.
In total, 1,418 Offspring and 2,111 Third Generation participants underwent MDCT measurements of coronary and aortic calcium between June 2002 and April 2005; subcutaneous and visceral fat measures were ascertained secondarily after study completion. Men had to be 35 years of age; women had to be 40 years of age and not pregnant; and all participants had to be free of CVD and weigh <352 lbs. Of the total 3,529 participants imaged, 3,394 had interpretable computed tomographic measures, 3,370 of those had both SAT and VAT measured, 3,164 of those were free of CVD, 3,142 of those attended the contemporaneous examination, and 3,141 of those had at least one of the lifestyle factor variables. Of these 3,141 participants, 2,926 had a complete covariate profile. Data on dietary intake were only available for a subset of the Offspring cohort (n = 925 participants). Nearly all participants were white (8).
Abdominal adipose tissue measurement
Imaging of the chest and abdomen was performed using an eight-slice MDCT (LightSpeed Ultra, GE Healthcare, Milwaukee, WI) as described previously (9). In brief, 25 contiguous 5-mm thick slices (120 kVp, 400 mA, gantry rotation time 500 ms, and table feed 3:1) were obtained covering 125 mm above the level of S1. Volumes of SAT and VAT were assessed (Aquarius 3D Workstation; TeraRecon Inc., San Mateo, CA) as described previously. In brief, fat pixels were identified (image display window width −195 to −45 Hounsfield units [HU]; window center of −120 HU), and the abdominal muscular wall was manually traced to separate the visceral from the subcutaneous compartment (9). Inter-reader reproducibility was high, with interclass correlations of 0.992 for VAT and 0.997 for SAT (9).
Lifestyle factors and covariate assessment
Lifestyle factors and covariates were measured at the contemporaneous examination cycles.
Diet.
Dietary intake was assessed using a semiquantitative food frequency questionnaire consisting of 126 items developed by Willett et al. (10) Then, the recently validated 2005 Dietary Guidelines Adherence Index (DGAI) (4) was used as a summary measure of adherence to the 2005 Dietary Guidelines (11). In brief, the DGAI consists of a total of 20 items. Eleven index items assess adherence to energy-specific food intake recommendations, and nine assess adherence to healthy choice nutrient intake recommendations. Each item is scored from a minimum of 0 to a maximum of 1, with a maximum score of 20 points.
Physical activity.
Habitual physical activity was assessed using a structured questionnaire. Subsequently, the average daily number of hours at different levels of activity (sleep, sedentary, slight, moderate, and heavy activity) was determined. A physical activity index (PAI) score was calculated by summing the reported numbers for each level of activity, weighted by their estimated metabolic expenditure, as described previously (12). The PAI ranges from a minimum score of 24, indicating 24 h of sleeping, to a maximum score of 120, indicating 24 h of heavy physical activity (12).
Smoking.
Participants were questioned in detail about current and prior cigarette smoking habits and were considered to be current smokers if they reported smoking at least one cigarette per day for the last year, former smokers if they were not smoking at present but had previously smoked as much as one cigarette per day for as long as 1 year, and never smokers if they smoked neither at present nor in the past. In addition, cumulative exposure (pack-years of smoking) was calculated by multiplying the number of cigarettes smoked per day by the number of years smoked. One pack-year was equivalent to 1 cigarette pack per day for 1 year.
Alcohol consumption.
Information on the amount of alcohol consumption was obtained from a physician-administered questionnaire in which participants were asked to report on the average number of drinks per week over the previous year. Based on current alcohol guidelines (11), women consuming ≤7 drinks/week and men consuming ≤14 drinks/week were defined as light-to-moderate drinkers; participants exceeding these cutoff points were defined as high alcohol consumers.
Healthy lifestyle factors.
Healthy lifestyle habits were defined as the upper quartile of the PAI, abstinence from smoking, and moderate alcohol consumption (1 to ≤7 drinks/week for women and 1 to ≤14 drinks/week for men) (11). Quartiles were selected for ease of data presentation.
Covariates.
Women were considered to be postmenopausal if their periods had stopped for at least 1 year. Information on hormone replacement therapy was obtained from the physician-administered questionnaire. Information on education was obtained by asking the participants to report their highest educational level.
Statistical analysis
SAT and VAT were normally distributed. In addition, the lifestyle factors with the exception of pack-years of smoking were normally distributed. Multivariable linear regression was used to assess the significance of covariate-adjusted cross-sectional relations between the continuous lifestyle factors (DGAI and PAI) and SAT and VAT. We estimated the covariate-adjusted mean volume of SAT and VAT associated with a 1-SD-higher DGAI and PAI. For the categorical lifestyle factors (smoking and alcohol), least-squares means were calculated to assess the relative amounts of SAT and VAT in current, former, and never smokers and by categories of alcohol consumption; ANOVA P values are presented. All models were adjusted for age, menopause, hormone replacement therapy, education, alcohol, and smoking. All analyses were sex specific, given our prior observation that relations between metabolic risk factors and VAT were stronger in women than in men (13). Tests for the significance of the difference between the β coefficients of the lifestyle factors in the models with SAT versus the models with VAT as outcome (in which SAT and VAT were first standardized to a mean of 0 and an SD of 1) were performed in situations in which SAT and VAT were both associated with the individual lifestyle factor. To determine the relation between the number of healthy lifestyle factors and SAT and VAT, age-adjusted mean volumes of SAT and VAT associated with practicing zero, one, two, or three healthy lifestyle habits were calculated; age-adjusted P values for trend were calculated as well. Dietary data were only available for a subset of the Offspring cohort and therefore were not included in the number of healthy lifestyle factors analysis.
Secondary analyses were performed. All models were additionally adjusted for physical activity. The above multivariable regressions and least-squares means were repeated using the general estimating equation procedure to account for familial correlations in the study sample. Interactions for the associations between the individual lifestyle factors and SAT and VAT with age (equal to or older than/younger than the median age of 50 years) and BMI (<25, 25 to <30, or ≥30 kg/m2) were tested in multivariable adjusted models.
SAS (version 8.0; SAS Institute, Cary, NC) was used to perform all computations. Two-tailed P < 0.05 and < 0.01 were considered significant for primary and secondary analyses, respectively.
RESULTS
The study sample consisted of 1,421 women and 1,505 men with a mean age of 50 ± 10 years (Table 1), with the exception of the dietary analysis, which was limited to only 925 participants.
Table 1.
Characteristics of study participants
| Women | Men | |
|---|---|---|
| n | 1,421 | 1,505 |
| Age (years) | 51 ± 9 | 48 ± 10 |
| BMI (kg/m2) | 27.0 ± 5.9 | 28.3 ± 4.5 |
| Waist circumference (cm) | 93 ± 15 | 100 ± 12 |
| Postmenopausal (%) | 46.2 | — |
| Hormone replacement therapy (%) | 22.9 | — |
| Education (%) | ||
| ≤11th grade | 0.8 | 1.6 |
| High school or equivalent degree | 22.8 | 17.9 |
| College grade/trade school | 33.2 | 27.0 |
| College grade/postgraduate | 43.1 | 53.4 |
| DGAI score* | 10.0 ± 2.6 | 8.5 ± 2.6 |
| PAI score† | 37 ± 6 | 38 ± 8 |
| Smoking (%) | ||
| Current | 12.3 | 13.0 |
| Former | 41.6 | 34.2 |
| Never | 46.1 | 52.8 |
| Smoking (pack-years) | ||
| Current | 26 | 28 |
| Former | 13 | 19 |
| Alcohol (drinks/week, %)‡ | ||
| 0 | 29.7 | 19.3 |
| <1 | 9.9 | 4.7 |
| 1 to <4 | 28.8 | 19.8 |
| 4–7 | 16.8 | 20.1 |
| >7–14 | 11.3 | 20.7 |
| ≥14 | 3.6 | 15.4 |
| SAT (cm3) | 3,137 ± 1,548 | 2,620 ± 1,212 |
| VAT (cm3) | 1,308 ± 813 | 2,160 ± 969 |
Data are means ± SD for continuous variables or percent for dichotomous and categorical variables.
Data only available for Offspring cohort (n = 925); scores range from 0–20 to points.
Scores range from 24 to 120 points.
One drink is equivalent to 12 g of alcohol.
SAT, VAT, and dietary quality
In women, higher DGAI (i.e., a diet more adherent to healthy guidelines) was associated with lower SAT (232 cm3 lower per 1 SD of DGAI, P = 0.002) and lower VAT (139 cm3 lower, P = 0.001) (Table 2). Similar results were obtained in men. The difference between the magnitude of the association between DGAI and VAT versus SAT was not significant (P = 0.19 for women and P = 0.78 for men).
Table 2.
Sex-specific multivariable-adjusted mean difference in volumes of SAT and VAT per 1-SD increment in DGAI and PAI and least-squares mean volumes of SAT and VAT by smoking and alcohol categories
| Women
|
Men
|
P for sex interaction | |||
|---|---|---|---|---|---|
| Multivariable-adjusted residual effect size* | P† | Multivariable-adjusted residual effect size* | P† | ||
| DGAI‡ | |||||
| SAT (cm3) | −232 (−375 to −88) | 0.002 | −217 (−339 to −95) | 0.0006 | 0.87 |
| VAT (cm3) | −139 (−222 to −57) | 0.001 | −243 (−353 to −132) | <0.0001 | 0.14 |
| PAI | |||||
| SAT (cm3) | −253 (−333 to −173) | <0.0001 | −128 (−193 to −63) | 0.0001 | 0.0002 |
| VAT (cm3) | −100 (−140 to −60) | <0.0001 | −85 (−133 to −37) | 0.0006 | 0.05 |
| Least squares* | P§ | Least squares* | P§ | P for sex interaction | |
| Smoking | |||||
| SAT (cm3) | |||||
| Current | 2,976 ± 117 | 0.06 | 2,629 ± 88 | 0.02 | 0.46 |
| Former | 3,247 ± 63 | 2,743 ± 56 | |||
| Never | 3,081 ± 60 | 2,538 ± 44 | |||
| VAT (cm3) | |||||
| Current | 1,393 ± 59 | 0.03 | 2,188 ± 66 | 0.005 | 0.10 |
| Former | 1,348 ± 32 | 2,262 ± 42 | |||
| Never | 1,250 ± 30 | 2,086 ± 33 | |||
| Alcohol (drinks/week) | |||||
| SAT (cm3) | |||||
| Light/moderate‖ | 3,184 ± 44 | 0.006 | 2,622 ± 34 | 0.91 | 0.02 |
| High | 2,869 ± 106 | 2,612 ± 80 | |||
| VAT (cm3) | |||||
| Light/moderate‖ | 1,320 ± 22 | 0.18 | 2,139 ± 25 | 0.04 | 0.01 |
| High | 1,243 ± 53 | 2,272 ± 59 | |||
Data are mean difference (95% CI) or mean ± SEM.
Adjusted for age, menopause (women only), hormone replacement therapy (women only), smoking, alcohol, and education.
ANOVA P value.
Data only available for Offspring cohort (n = 925).
Global P value.
Light-to-moderate alcohol consumption (≤7 drinks/week for women and ≤14 drinks/week for men).
SAT, VAT, and physical activity
Higher PAI (i.e., more physical activity) was inversely associated with SAT in both women (P < 0.0001) and men (P = 0.0001) (Table 2), although the association was more pronounced in women (P for sex interaction = 0.0002). For VAT, similar results were obtained (P < 0.0001 for women and P = 0.0006 for men), although the sex interaction did not reach statistical significance (P = 0.05). No difference was observed in the strength of the association of PAI with SAT versus VAT (P = 0.21 for women, P = 0.27 for men).
SAT, VAT, and smoking
In women, former smokers tended to have the highest mean SAT compared with current or never smokers, although the difference did not meet statistical significance (P = 0.06) (Table 2). Similar results were observed in men, with a significant difference observed among the three groups (P = 0.02). In women, mean VAT was higher in current smokers and former smokers compared with those who never smoked (P = 0.03 for both pairwise comparisons), whereas in men, mean VAT was higher in former smokers (P = 0.001 for pairwise comparison) but not in current smokers.
SAT, VAT, and alcohol consumption
In women, participants with light-to-moderate alcohol intake had higher mean SAT compared with those with high alcohol intake (P = 0.006), whereas there was no difference in mean VAT (P = 0.18) (Table 2). In contrast, SAT did not differ according to alcohol intake in men (P = 0.91), whereas men with light-to-moderate alcohol intake had lower mean VAT compared with those with high alcohol intake (P = 0.04).
SAT, VAT, and number of healthy lifestyle factors
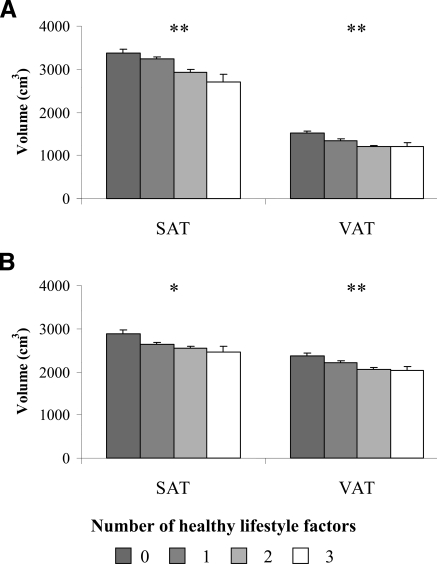
In both women and men, practicing a higher number of healthy lifestyle habits was significantly associated with lower mean SAT (P < 0.0001 for women and P < 0.01 for men) and VAT (P < 0.0001) (Fig. 1A and B).
Figure 1.
Age-adjusted mean (± 1 SE) volumes of SAT and VAT in women (A) and men (B) associated with practicing zero, one, two, or three healthy lifestyle habits. Age-adjusted P values for trend are presented. *P < 0.01; **P < 0.001.
Secondary analysis
The additional inclusion of physical activity as a covariate did not materially change the associations between the lifestyle factors and SAT and VAT (data not shown). When the general estimating equation procedure was used to repeat the analyses, the results did not substantially differ from the findings reported above (data not shown). Significant effect modification of BMI on the association between DGAI and SAT and PAI and VAT was observed (supplemental Table A1, available in an online appendix at http://dx.doi.org/10.2337/dc08-1382). The strongest association between DGAI and SAT was in overweight individuals, whereas the strongest association between PAI and VAT was observed in normal-weight individuals.
CONCLUSIONS
In a large, cross-sectional, population-based study, our findings were fourfold. First, a diet consistent with recommended dietary guidelines and greater physical activity were associated similarly with lower volumes of SAT and VAT. Second, both current and former smokers had higher levels of VAT. Third, men who consumed higher amounts of alcohol had higher VAT, whereas women who consumed higher amounts of alcohol had lower SAT. Last, an increasing number of healthy lifestyle factors overall was associated with lower SAT and VAT volumes.
Diet
In the present study, a diet consistent with the 2005 DGAI was associated similarly with lower volumes of SAT and VAT. Although our findings are concordant with prior cross-sectional and prospective studies that documented similar findings using conventional measures of adiposity (4), we extend the current literature by demonstrating an equivalent association between dietary quality and SAT and VAT on a population-based level.
The present findings are supported by some small randomized clinical trials and metabolic studies (n = 32–78) that have focused on the effects of diet-induced weight loss on different abdominal fat compartments (14). The results of these trials demonstrated similar relative reductions in VAT and SAT in overweight and obese individuals after consumption of a very-low-energy diet for 3–6 months. However, other studies have demonstrated a greater relative reduction in VAT compared with SAT (15). More research is needed to determine whether different dietary components, in addition to total energy intake, are differentially associated with SAT and VAT volumes to gain more insight into the contribution of specific nutrients to cardiometabolic risk.
Physical activity
A higher level of physical activity was associated similarly with lower SAT and VAT volumes in both sexes, extending the results from prior small cross-sectional studies in men (16) and older individuals to a large population-based study of both women and men. Results from prospective studies have consistently demonstrated that greater physical activity is associated with less weight gain and lower abdominal adiposity (5). In addition, several small randomized controlled trials demonstrated a greater relative reduction in VAT compared with SAT (15), whereas results from a relatively larger trial suggested equal relative reductions in SAT and VAT (17). The latter study is concordant with our findings that SAT and VAT are associated similarly with physical activity.
The reductions in SAT and VAT induced by physical activity may occur with concomitant weight loss (15,17), although results from several exercise studies demonstrated that reductions may also occur in the absence of weight loss (15). These findings suggest that physical activity may affect SAT and VAT through a mechanism above and beyond reductions in body weight. Future researchers should investigate whether different types of physical activity are differentially associated with SAT and VAT to gain more insight into the magnitude of the effect of different types of physical activity on cardiometabolic risk.
Smoking
Despite the abundance of data showing that current smokers have a lower BMI compared with former and never smokers (18), data from the present study show that smokers have more VAT. These findings are supported by the work of others who have shown that higher waist circumference and waist-to-hip ratio are present in current smokers (6). Further, a recent study of 450 Japanese men with an extremely high smoking prevalence of nearly two-thirds of the sample demonstrated more VAT but less SAT among heavier smokers (16). Our findings extend the results of this study by demonstrating associations between smoking and larger amounts of VAT in a large population-based study of both women and men, accounting for multiple potential covariates and generalizing these findings to a study sample with a lower prevalence of smoking.
Smoking may affect VAT by reducing the bioavailability of endogenous estrogen (19) and increasing the production of adrenal androgens in women and men. Estrogens are implicated in the pathogenesis of adiposity, as postmenopausal women tend to have increased visceral abdominal adipose tissue compared with premenopausal women (20).
Alcohol
The present study is notable for higher levels of VAT among men who consume higher amounts of alcohol. VAT has been positively correlated with higher amounts of daily alcohol intake (21). In a study of 450 Japanese men with high levels of smoking, men consuming alcohol had significantly more VAT than alcohol abstainers (16). Habitual high alcohol intake may cause fatty liver, which can result in hepatic insulin resistance and subsequent weight gain (22).
The finding that women who consume higher amounts of alcohol have lower SAT is surprising. A possible explanation for this may be an overall lower energy intake in women who consume higher amounts of alcohol (23). However, further studies are required to confirm our finding.
Healthy lifestyle factors
In the present study, practicing a higher number of healthy lifestyle habits was associated with lower mean SAT and VAT. These findings are supported by a large prospective study that demonstrated a considerable decrease in waist circumference with changes in a combination of lifestyle factors (24). In addition, several studies showed that adherence to a higher number of healthy lifestyle habits is associated with a reduced risk of coronary heart disease and myocardial infarction and lower mortality (25).
Strength and limitations
Strengths of our study include the examination of the association between several lifestyle factors and radiographically assessed adipose tissue compartments, the statistical power provided by the use of a large population-based sample of women and men, the ability to adjust for several potential confounders, and the assessment of SAT and VAT volumes using a highly reproducible method.
Some notable limitations of our study include the cross-sectional design, which does not allow us to make causal inferences between lifestyle factors and SAT and VAT. The study sample was primarily Caucasian; therefore, the results may not be generalizable to other ethnicities.
In summary, adherence to recommended dietary guidelines and physical activity is associated similarly with lower SAT and VAT volumes. However, both smoking and high alcohol intake are differentially associated with VAT volumes. Further research to uncover the putative mechanisms is warranted.
Supplementary Material
Acknowledgments
The Framingham Heart Study is supported by the National Heart, Lung, and Blood Institute (NHLBI) (N01-HC-25195). E.A.M. is supported by the Netherlands Organization for Scientific Research and the Dutch Heart Foundation. R.S.V. is supported in part by 2K24 HL 04334 (NHLBI).
No potential conflicts of interest relevant to this article were reported.
Published ahead of print at http://care.diabetesjournals.org on 15 December 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Janssen I, Katzmarzyk PT, Ross R: Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med 162:2074–2079, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R: Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 14:336–341, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Pascot A, Lemieux S, Lemieux I, Prud'homme D, Tremblay A, Bouchard C, Nadeau A, Couillard C, Tchernof A, Bergeron J, Despres JP: Age-related increase in visceral adipose tissue and body fat and the metabolic risk profile of premenopausal women. Diabetes Care 22:1471–1478, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Fogli-Cawley JJ, Dwyer JT, Saltzman E, McCullough ML, Troy LM, Jacques PF: The 2005 Dietary Guidelines for Americans Adherence Index: development and application. J Nutr 136:2908–2915, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Samaras K, Kelly PJ, Chiano MN, Spector TD, Campbell LV: Genetic and environmental influences on total-body and central abdominal fat: the effect of physical activity in female twins. Ann Intern Med 130:873–882, 1999 [DOI] [PubMed] [Google Scholar]
- 6.Shimokata H, Muller DC, Andres R: Studies in the distribution of body fat. III. Effects of cigarette smoking. JAMA 261:1169–1173, 1989 [PubMed] [Google Scholar]
- 7.Dawber TR, Kannel WB, Lyell LP: An approach to longitudinal studies in a community: the Framingham Study. Ann NY Acad Sci 107:539–556, 1963 [DOI] [PubMed] [Google Scholar]
- 8.Splansky GL, Corey D, Yang Q, Atwood LD, Cupples LA, Benjamin EJ, D'Agostino RB Sr, Fox CS, Larson MG, Murabito JM, O'Donnell CJ, Vasan RS, Wolf PA, Levy D: The Third Generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 165:1328–1335, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Maurovich-Horvat P, Massaro J, Fox CS, Moselewski F, O'Donnell CJ, Hoffmann U: Comparison of anthropometric, area- and volume-based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi-detector computed tomography. Int J Obes (Lond )31:500–506, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE: Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 122:51–65, 1985 [DOI] [PubMed] [Google Scholar]
- 11.Dietary Guidelines for Americans 2005, 6th ed. Washington, DC, Department of Agriculture and Department of Health and Human Services, 2005
- 12.Kannel WB, Sorlie P: Some health benefits of physical activity: the Framingham Study. Arch Intern Med 139:857–861, 1979 [PubMed] [Google Scholar]
- 13.Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB Sr, O'Donnell CJ: Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116:39–48, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Redman LM, Heilbronn LK, Martin CK, Alfonso A, Smith SR, Ravussin E: Effect of calorie restriction with or without exercise on body composition and fat distribution. J Clin Endocrinol Metab 92:865–872, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ross R, Dagnone D, Jones PJ, Smith H, Paddags A, Hudson R, Janssen I: Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men: a randomized, controlled trial. Ann Intern Med 133:92–103, 2000 [DOI] [PubMed] [Google Scholar]
- 16.Komiya H, Mori Y, Yokose T, Tajima N: Smoking as a risk factor for visceral fat accumulation in Japanese men. Tohoku J Exp Med 208:123–132, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Irwin ML, Yasui Y, Ulrich CM, Bowen D, Rudolph RE, Schwartz RS, Yukawa M, Aiello E, Potter JD, McTiernan A: Effect of exercise on total and intra-abdominal body fat in postmenopausal women: a randomized controlled trial. JAMA 289:323–330, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Canoy D, Wareham N, Luben R, Welch A, Bingham S, Day N, Khaw KT: Cigarette smoking and fat distribution in 21,828 British men and women: a population-based study. Obes Res 13:1466–1475, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Michnovicz JJ, Hershcopf RJ, Naganuma H, Bradlow HL, Fishman J: Increased 2-hydroxylation of estradiol as a possible mechanism for the anti-estrogenic effect of cigarette smoking. N Engl J Med 315:1305–1309, 1986 [DOI] [PubMed] [Google Scholar]
- 20.Toth MJ, Tchernof A, Sites CK, Poehlman ET: Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes Relat Metab Disord 24:226–231, 2000 [DOI] [PubMed] [Google Scholar]
- 21.Cigolini M, Targher G, Bergamo AI, Tonoli M, Filippi F, Muggeo M, De Sandre G: Moderate alcohol consumption and its relation to visceral fat and plasma androgens in healthy women. Int J Obes Relat Metab Disord 20:206–212, 1996 [PubMed] [Google Scholar]
- 22.Lazarus R, Sparrow D, Weiss S: Temporal relations between obesity and insulin: longitudinal data from the Normative Aging Study. Am J Epidemiol 147:173–179, 1998 [DOI] [PubMed] [Google Scholar]
- 23.Colditz GA, Giovannucci E, Rimm EB, Stampfer MJ, Rosner B, Speizer FE, Gordis E, Willett WC: Alcohol intake in relation to diet and obesity in women and men. Am J Clin Nutr 54:49–55, 1991 [DOI] [PubMed] [Google Scholar]
- 24.Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, Rimm E: Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr 78:719–727, 2003 [DOI] [PubMed] [Google Scholar]
- 25.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC: Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med 343:16–22, 2000 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.