Abstract
OBJECTIVE—Increased availability of fatty acids is important for accumulation of intracellular lipids and development of insulin resistance in human myotubes. It is unknown whether different types of fatty acids like eicosapentaenoic acid (EPA) or tetradecylthioacetic acid (TTA) influence these processes.
RESEARCH DESIGN AND METHODS—We examined fatty acid and glucose metabolism and gene expression in cultured human skeletal muscle cells from control and type 2 diabetic individuals after 4 days of preincubation with EPA or TTA.
RESULTS—Type 2 diabetes myotubes exhibited reduced formation of CO2 from palmitic acid (PA), whereas release of β-oxidation products was unchanged at baseline but significantly increased with respect to control myotubes after preincubation with TTA and EPA. Preincubation with TTA enhanced both complete (CO2) and β-oxidation of palmitic acid, whereas EPA increased only β-oxidation significantly. EPA markedly enhanced triacylglycerol (TAG) accumulation in myotubes, more pronounced in type 2 diabetes cells. TAG accumulation and fatty acid oxidation were inversely correlated only after EPA preincubation, and total level of acyl-CoA was reduced. Glucose oxidation (CO2 formation) was enhanced and lactate production decreased after chronic exposure to EPA and TTA, whereas glucose uptake and storage were unchanged. EPA and especially TTA increased the expression of genes involved in fatty acid uptake, activation, accumulation, and oxidation.
CONCLUSIONS—Our results suggest that 1) mitochondrial dysfunction in diabetic myotubes is caused by disturbances downstream of fatty acid β-oxidation; 2) EPA promoted accumulation of TAG, enhanced β-oxidation, and increased glucose oxidation; and 3) TTA improved complete palmitic acid oxidation in diabetic myotubes, opposed increased lipid accumulation, and increased glucose oxidation.
Type 2 diabetes is characterized by hyperglycemia, reduced ability to oxidize fat, and accumulation of triacylglycerol (TAG) in skeletal muscle fibers. The increased deposition of intramyocellular TAG (imTAG) has received special interest, because several studies have demonstrated a positive association between insulin resistance and imTAG storage (1,2). Accumulation of imTAG depends on the availability and uptake of fatty acids, the rate of fatty acid oxidation, and the rate of synthesis and hydrolysis of TAG. Increased availability of plasma free fatty acid (FFA) during lipid infusion or high-fat feeding is associated with development of insulin resistance and accumulation of imTAG in vivo (3). Moreover, studies have shown impaired capacity for fatty acid oxidation in skeletal muscle from insulin-resistant/type 2 diabetic individuals (4,5), and reduced mitochondrial fatty acid oxidation in skeletal muscle and myotubes is associated with increased deposition of imTAG (6–8). Fatty acids may promote insulin resistance via intracellular intermediates such as acyl-CoA, diacylglycerol (DAG), and ceramides, interfering with insulin signaling and glucose metabolism (9).
Previous studies have demonstrated positive effects on skeletal muscle insulin sensitivity of mono- and polyunsaturated fatty acids (PUFAs) compared with saturated fatty acids (10–12). Very long–chain ω-3 fatty acids, including eicosapentaenoic acid (EPA), may protect against skeletal muscle insulin resistance caused by high-fat feeding in vivo (1,13). PUFAs may also promote increased TAG accumulation without impairing insulin-stimulated glucose uptake in myotubes (10,11). The sulfur-substituted fatty acid analog tetradecylthioacetic acid (TTA) is a pan–peroxisome proliferator–activated receptor (pan-PPAR) activator that reduces plasma lipids and enhances hepatic fatty acid oxidation in rodents (14). Dual and pan-PPAR agonists are currently being developed for treatment of type 2 diabetes (15), and TTA has been shown to improve glucose metabolism in insulin-resistant rats (16) and to stimulate mitochondrial proliferation in rat skeletal muscle (17). We have recently demonstrated that TTA may increase fatty acid oxidation in human myotubes similar to the PPARδ-specific agonist GW501516 (18).
Skeletal muscle metabolism is influenced by physical activity, hormonal status, and muscle fiber type, rendering it difficult to determine the impact of EPA and TTA on basal and insulin-stimulated intermediary metabolism. Cultured human myotubes display the morphological, metabolic, and biochemical properties of adult skeletal muscle (19) and offer a unique model to distinguish between genetic and environmental factors in the etiology of insulin resistance (20). We and others have reported several potential intrinsic deficiencies in myotubes from individuals with type 2 diabetes, including lower basal palmitate oxidation (21) and impaired insulin-stimulated glucose metabolism (20,22). It is unknown whether EPA or TTA may improve insulin resistance or other characteristics of type 2 diabetes, such as decreased lipid oxidation in myotubes.
To identify the potential effects of EPA and TTA on the intermediary energy metabolism and insulin resistance, we compared the effect of TTA, EPA, and oleic acid in myotubes established from obese individuals with type 2 diabetes and obese healthy subjects.
RESEARCH DESIGN AND METHODS
Dulbecco's modified Eagle's medium (DMEM)-Glutamax, FCS, Ultroser G, penicillin-streptomycin-amphotericin B, and trypsin-EDTA were obtained from Gibco, Invitrogen (Paisley, U.K.). 2-[3H(G)]deoxy-d-glucose (6.00 Ci/mmol) and d-[14C(U)]glucose (5 mCi/mmol) were purchased from PerkinElmer, NEN (Boston, MA). [1-14C]acetate (55 mCi/mmol), [1-14C]PA (55 mCi/mmol), and d-[1-14C]glucose (55 mCi/mmol) were obtained from American Radiolabeled Chemicals (St. Louis, MO). Palmitic acid, oleic acid, BSA (essentially fatty acid free), cytochalasin B, and extracellular matrix gel were purchased from Sigma-Aldrich (St. Louis, MO). Insulin Actrapid was from Novo-Nordisk (Bagsvaerd, Denmark). Agilent Total RNA Isolation Mini kit was purchased from Matriks (Oslo). The primers, SYBR Green and TaqMan reverse-transcription reagents kit were obtained from Applied Biosystems (Warrington, U.K.), and the protein assay kit was purchased from BioRad (Copenhagen). EPA was purchased from NU-Chek-Prep, Ida kjemi (Ås, Norway). TTA and [1-14C]TTA were provided by R.K.B.
Biopsies.
Skeletal muscle biopsies were obtained from eight obese type 2 diabetic patients (49.2 ± 1.8 years) and eight obese control subjects (50.3 ± 1.8 years) taken from musculus vastus lateralis in the fasted state by needle biopsy under local anesthesia. Only sedentary subjects were recruited. Diabetic individuals were treated either with diet alone or in combination with sulfonylurea, metformin, or insulin, which was withdrawn 1 week before taking the biopsies. The patients had no diabetic complications apart from simple retinopathy. The control subjects had normal glucose tolerance and no family history of type 2 diabetes. The groups were matched with respect to age and BMI but differed by fasting plasma glucose concentrations (5.5 ± 0.2 vs. 10.4 ± 0.7 mmol/l, P < 0.001, t test), fasting serum insulin levels (50.5 ± 5.6 vs. 96.1 ± 12.5 pmol/l, P < 0.05), glucose disappearance rate during euglycemic-hyperinsulinemic clamp (280.0 ± 34.8 vs. 121.1 ± 23.2 mg · min−1 · m−2, P < 0.001), and A1C (5.4 ± 0.1 vs. 7.6 ± 0.6%, P < 0.05). All subjects gave written informed consent, and the local ethics committee of Funen and Vejle County approved the study.
Cell culture and fatty acid incubation.
Myotubes were established from satellite cells (19). Human myoblasts from control and type 2 diabetic subjects were differentiated to myotubes at a physiological concentration of insulin (25 pmol/l) and glucose (5.5 mmol/l) for 4 days. Myotubes were then exposed to BSA (40 μmol/l), oleic acid (100 μmol/l), TTA (100 μmol/l), or EPA (100 μmol/l) for another 4 days. Stock solutions of fatty acid sodium salts (6 mmol/l) and BSA (2.4 mmol/l) were heated to 45°C and rapidly mixed (molar ratio of 2.5:1). Only optically clear solutions were used. There were no differences between the myotubes after preincubation with fatty acids as evaluated by microscopic inspection searching for floating cells or cells with lipid droplets. The myotubes had similar protein content independent of incubation medium.
Palmitic acid uptake and distribution of radiolabel in lipids
Palmitic acid uptake.
Myotubes were incubated in DMEM supplemented with 0.24 mmol/l BSA, 0.5 mmol/l l-carnitine, 20 mmol/l HEPES, [1-14C]PA (0.5 μCi/ml, 0.6 mmol/l), and 25 pmol/l or 1.0 μmol/l insulin for 4 h, to study basal and insulin-mediated uptake and lipid distribution of palmitate.
De novo lipid synthesis.
Myotubes preincubated with fatty acids were further incubated 4 h in medium containing [1-14C]acetate (3–4 μCi/ml, 100 μmol/l). After incubation, myotubes were placed on ice, washed three times with 1 ml PBS, scraped twice with 250 μl distilled water, and homogenized. The cell homogenates were assayed for protein and extracted for lipids, and the radiolabeled lipids were separated by thin-layer chromatography (21) and quantified by liquid scintillation. Total lipid uptake is the sum of oxidation and storage products.
Measures of fatty acid oxidation
Acid-soluble metabolites.
Myotubes were incubated in DMEM supplemented with 0.24 mmol/l BSA, 0.5 mmol/l l-carnitine, [1-14C]PA (0.5 μCi/ml, 0.6 mmol/l), and 25 pmol/l or 1.0 μmol/l insulin for 4 h to study cellular release of excess 14C–palmitic acid–derived acid-soluble metabolites (ASMs) to the media. The incubation media were transferred to new tubes and assayed for labeled ASMs, which mainly are byproducts of β-oxidation remaining in solution after precipitation of the radiolabeled fatty acid with perchloric acid (PCA) (23).
CO2 and total oxidation.
Myotubes were incubated in DMEM supplemented with 0.24 mmol/l BSA, 0.5 mmol/l l-carnitine, 20 mmol/l HEPES, [1-14C]PA (0.5 μCi/ml, 0.6 mmol/l), and 25 pmol/l insulin for 4 h to study CO2 formation (21). PCA was added to the cells to measure both intra- and extracellular (total) ASMs from palmitic acid. Thus, total palmitic acid oxidation is the sum of CO2 and total ASMs.
Glucose metabolism.
Glucose uptake, glycogen synthesis, and glucose oxidation were determined as previously described (7).
RNA isolation and real-time RT-PCR.
Myotubes were washed and centrifuged to a pellet before total RNA was isolated by Total RNA Isolation Mini kit (Agilent), according to the supplier protocol. Total RNA (0.05 μg/μl) was reversely transcribed with a TaqMan reverse-transcription reagents kit (7). Quantitative RT-PCR was performed using an ABI PRISM 7000 Detection System. DNA expression was determined by SYBR Green (7), and primers for uncoupling protein 2 (UCP2), fatty acid translocase (CD36/FAT), carnitine palmitoyl transferase (CPT)-1a, CPT2, fatty acid binding protein 3 (FABP3), long-chain acyl-coenzyme A synthetase 1 (ACSL1), ACSL3, mitochondrial trifunctional protein β-subunit (HADHB), acyl-coenzyme A dehydrogenase medium-chain (ACADM), DGAT1, DGAT2, hexokinase II (HKII), GLUT1, GLUT4, actin-β (ACTβ), and ribosomal protein, large, P0 (RPLP0) (supplemental Table 1, available in an online appendix at http://dx.doi.org/10.2337/db08-1043) were designed using Primer Express (Applied Biosystems). In addition, expression of CPT1b, citrate synthase (CS), malate dehydrogenase 2 (MDH2), ACC2, UCP3, stearoyl-coenzyme A desaturase 1 (SCD1), PGC1a, ACTB, and RPLP0 (supplemental Table 1) were analyzed with the inventoried TaqMan gene expression assays of Applied Biosystems on a 7900HT Fast Real-Time PCR system with 96-well block module following standard protocols. The transcription levels were normalized to ACTB and RPLP0.
Analysis of acyl-CoA fractions.
Cells were harvested by centrifugation and washed twice with 10 mmol/l PCA and stored at −80°C until long-chain fatty acyl-CoA (LCFA-CoA) extraction. Heptadecanoyl-CoA (33 pmol) and H2O were added to a final volume of 800 μl before addition of 3 ml chloroform:methanol (2:1). Cells were then homogenized with an Ultraturrax homogenizer. Chloroform (1 ml) and H2O (1 ml) were added and vortexed vigorously. After centrifugation (3,000 rpm/10 min/4°C), the interphase was recovered and dried under a stream of N2. The LCFA-CoAs were further extracted and derivatized to fluorescent acyl etheno-CoA esters using 0.5 mol/l chloroacetaldehyde, 0.5% SDS, and 0.15 mol/l citrate, pH 4 (200 μl), and then separated and analyzed by reverse-phase chromatography (24). Peak areas were integrated using Chromeleonc version 6.50 (Dionex) and quantified relative to the internal heptadecanoyl-CoA standard. Identification of individual LCFA-CoA was performed using standard LCFA-CoA mixtures. The detection level of our methods was 0.5 pmol/l.
Scintillation proximity assay.
We applied this method because it provides accurate and reproducible cell data with limited use of resources for quite extensive analyses (25). In short, radiolabeled substrates taken up and accumulated by adherent cells are concentrated close to the scintillator embedded in the plastic bottom of each well and thus provide a stronger signal than the radiolabel dissolved in the medium alone (25). Myotubes were preincubated with 100 μmol/l oleic acid for 4 days with addition of 100 μmol/l TTA the last 24 h. Then myotubes were washed with PBS, medium containing [1-14C]PA (1 μCi/ml, 100 μmol/l) was added, and myotubes were incubated up to 4 h. Fatty acid was bound to BSA at a ratio of 2.5:1.
Statistical analysis.
The effect of group and incubations was evaluated by linear mixed models analysis in SPSS (v12.0.1), monitoring group and treatment effects based on all available data from each experiment and taking into account the correlation between measurements/myotubes from the same subjects. Some acyl-CoA values were below detection limit and were assigned the value 0.5 pmol/l in accordance to the detection level. Nonparametric statistical analyses (Mann-Whitney and Wilcoxon's signed-rank test) were performed on the acyl-CoA data for evaluation of group and treatment differences, respectively. A P value ≤0.05 was considered significant.
RESULTS
Effect of fatty acids on uptake and oxidation of fatty acids.
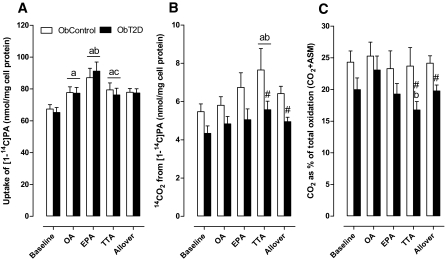
We observed enhanced uptake of 14C–palmitic acid in cultured myotubes from controls and type 2 diabetic subjects after 4 days of preincubation with oleic acid, EPA, or TTA (Fig. 1A), showing that fatty acid availability is important for cellular lipid uptake. By adding 1 μmol/l insulin acutely, 14C–palmitic acid accumulation was further enhanced by 15–30% (data not shown; P < 0.05). There was an allover significant 20% reduction in 14C–palmitic acid–derived CO2 released from type 2 diabetes vs. control myotubes (Fig. 1B), indicating that type 2 diabetes cells exhibit reduced complete palmitic acid oxidation. However, after incubation with TTA, control and type 2 diabetes myotubes showed enhanced 14CO2 production from 14C–palmitic acid compared with baseline or preincubation with oleic acid (Fig. 1B), suggesting that TTA may improve mitochondrial fatty acid oxidation. The percentage of palmitic acid that was oxidized completely to CO2 compared with total oxidation [sum of complete (CO2) plus incomplete fatty acid oxidation (ASMs)] was lower in type 2 diabetes myotubes, especially after preincubation with TTA (Fig. 1C). Preincubation with EPA and TTA enhanced 14C–palmitic acid–derived ASMs recovered in the media, and the response was significantly stronger in type 2 diabetes myotubes (EPA 125% and TTA 128%) compared with control myotubes (EPA 45% and TTA 47%; Fig. 2A). In the presence of insulin, preincubation with EPA, TTA, and oleic acid enhanced ASM release, with a stronger allover response in type 2 diabetes compared with control myotubes (Fig. 2B). We also observed similar effects of EPA and TTA on ASMs derived from 14C–oleic acid, with significantly stronger release from type 2 diabetes than control myotubes in the presence of insulin (data not shown).
FIG. 1.
Palmitate uptake and oxidation. Differentiated myotubes from type 2 diabetic or control subjects were preincubated with 40 μmol/l BSA, 100 μmol/l oleic acid, 100 μmol/l TTA, or 100 μmol/l EPA for 4 days and incubated with 0.6 mmol/l [1-14C]PA for 4 h. The panels show palmitate uptake, which is the sum of total recovered CO2, ASMs, and total lipids (A); oxidation to CO2 (B); CO2 from palmitic acid as percentage of total oxidation (C). Results present means ± SE (n = 8). a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; c, P ≤ 0.05 vs. EPA; #P ≤ 0.05 vs. ObControl, analyzed by linear mixed models statistics (SPSS), which also calculated the allover results based on all available data. T2D, type 2 diabetes.
FIG. 2.
Palmitate-derived ASMs release to the medium. Differentiated myotubes from type 2 diabetes or control subjects were preincubated with fatty acids as described in Fig. 1 and then acutely incubated with 0.6 mmol/l [1-14C]PA ± 1 μmol/l insulin for 4 h. The panels show ASMs released from the cells, derived from 14C–palmitic acid without (A) and with (B) 1 μmol/l insulin. Results represent means ± SE (n = 6–7). a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; #P ≤ 0.05 vs. ObControl, analyzed by linear mixed models statistics (SPSS), which also calculated the allover results based on all available data.
Accumulation of TAG.
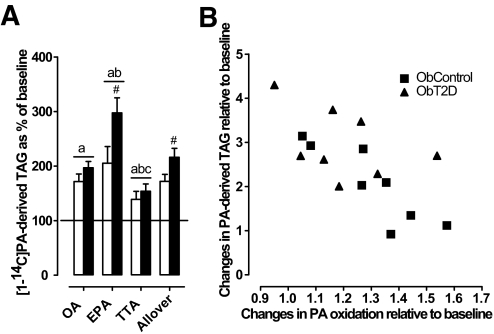
Preincubation of myotubes with oleic acid and EPA enhanced 14C–palmitic acid accumulation into lipids compared with baseline by 23–32% and 29–53%, respectively (results not shown; P < 0.05). The enhanced lipid accumulation might be explained by a strong increment in TAG accumulation after preincubation with oleic acid (7.4 and 7.9 nmol/mg cell protein, control, and type 2 diabetes, respectively) and EPA (10.9 and 17.5 nmol/mg cell protein, control, and type 2 diabetes, respectively) compared with baseline (results not shown; P < 0.05). The relative increase in TAG accumulation was significantly higher in type 2 diabetes than control myotubes after preincubation with EPA (Fig. 3A). Preincubation with TTA did not increase total 14C–palmitic acid lipid accumulation, although radiolabeled TAG was slightly increased compared with baseline but reduced compared with oleic acid and EPA (Fig. 3A). Similar effects of oleic acid, EPA, and TTA on lipid synthesis were observed using 14C–oleic acid (data not shown). Moreover, preincubation with EPA caused a negative correlation between relative change in total oxidation and TAG synthesis from 14C–palmitic acid (r = −0.69, P < 0.005) (Fig. 3B), but not with oleic acid or TTA (results not shown).
FIG. 3.
Changes in TAG accumulation from 14C–palmitic acid relative to baseline (A) and negative correlation between changes in 14C–palmitic acid oxidation and TAG accumulation after preincubation with EPA (B). Differentiated myotubes from type 2 diabetic or control subjects were preincubated with fatty acids as described in Fig. 1 and then acutely incubated with [1-14C]PA (0.6 mmol/l) for 4 h. The panels show changes in 14C–palmitic acid–derived TAGs as percentage of baseline (BSA) (A) and a negative correlation between changes in total 14C–palmitic acid oxidation and TAG accumulation in myotubes preincubated with EPA (r = −0.69, P < 0.001). Results represent means ± SE (n = 8). a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; c, P ≤ 0.05 vs. EPA; #P ≤ 0.05 vs. ObControl, analyzed by linear mixed models statistics (SPSS), which also calculated the allover results based on all available data.
Gene expression related to mitochondrial function and lipid metabolism.
There were no differences between the two groups in expression of several genes important for mitochondrial function and fatty acid metabolism (Table 1). Preincubation with fatty acids increased the expression of CPT1-α/β (1.5- to 2-fold) and HADHB (30%). However, UCP2 and -3 were moderately increased with respect to baseline by 43 and 24%, respectively, only after preincubation with TTA.
TABLE 1.
Gene expression relative to baseline
| Baseline (Ct no.) | Oleic acid | EPA | TTA | |
|---|---|---|---|---|
| CPT1α | 1.00 (27) | 2.25 ± 0.09a | 2.24 ± 0.11a | 2.23 ± 0.11a |
| CPT1β | 1.00 (33) | 1.71 ± 0.10a | 1.42 ± 0.07ab | 1.78 ± 0.15ac |
| CPT2 | 1.00 (30) | 1.08 ± 0.03a | 1.04 ± 0.03 | 1.05 ± 0.03 |
| ACADM | 1.00 (28) | 1.08 ± 0.08 | 1.05 ± 0.08 | 0.97 ± 0.06 |
| HADHB | 1.00 (24) | 1.32 ± 0.06a | 1.38 ± 0.06a | 1.31 ± 0.06a |
| CS | 1.00 (26) | 1.10 ± 0.04a | 0.99 ± 0.03b | 1.12 ± 0.04ac |
| MDH2 | 1.00 (25) | 1.04 ± 0.02 | 1.00 ± 0.02b | 1.04 ± 0.02a |
| UCP2 | 1.00 (28) | 1.14 ± 0.10 | 0.84 ± 0.06ab | 1.43 ± 0.08abc |
| UCP3 | 1.00 (34) | 1.11 ± 0.07 | 0.96 ± 0.06b | 1.24 ± 0.07ac |
| CD36/FAT | 1.00 (29) | 2.05 ± 0.11a | 2.01 ± 0.10a | 4.41 ± 0.32abc |
| ACSL1 | 1.00 (25) | 1.25 ± 0.04a | 1.21 ± 0.05a | 1.13 ± 0.04ab |
| ACSL3 | 1.00 (24) | 1.51 ± 0.11a | 1.63 ± 0.09a | 2.01 ± 0.13abc |
| FABP3 | 1.00 (25) | 1.33 ± 0.06a | 1.56 ± 0.06ab | 2.75 ± 0.26abc |
| SCD1 | 1.00 (24) | 0.88 ± 0.07 | 1.05 ± 0.08b | 2.50 ± 0.26abc |
| DGAT1 | 1.00 (34) | 1.00 ± 0.13 | 1.29 ± 0.21 | 1.26 ± 0.11a |
Data are means ± SE (n = 16). Individual results were normalized to baseline (set to 1; average baseline Ct numbers for the investigated genes are shown in brackets, giving an impression of relative expression levels).
P ≤ 0.05 vs. baseline;
P ≤ 0.05 vs. oleic acid;
P ≤ 0.05 vs. EPA analyzed by linear mixed models statistics (SPSS).
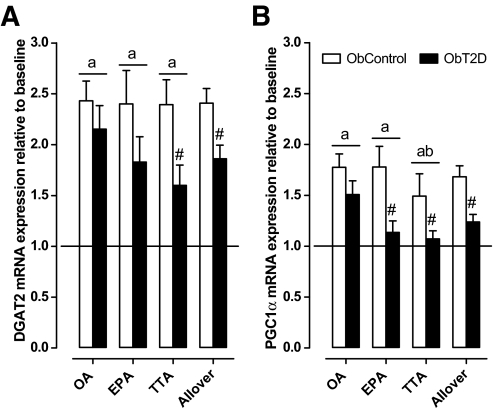
Expression of CD36/FAT, ACSL, and FABP3 was increased after preincubation with TTA more so than oleic acid and EPA (Table 1). Preincubation with TTA also promoted a 2.5-fold induction in SCD1 compared with the other fatty acids (Table 1). DAG acyltransferase 2 (DGAT2), responsible for the final step in TAG synthesis, was increased similarly by all fatty acids in control myotubes, whereas type 2 diabetes myotubes displayed a reduced response, especially during incubation with TTA (Fig. 4A). The nuclear transcription factor PPARγ coactivator α (PGC1α) had a similar expression pattern to DGAT2, with enhanced expression after fatty acid preincubation in control cells and reduced response in type 2 diabetes myotubes (Fig. 4B).
FIG. 4.
Gene expression of DGAT2 and PGC1α. Panels show changes in DGAT2 (A) and PGC1α (B) gene expression relative to baseline (set to 1) for control and type 2 diabetes myotubes. Cells were preincubated as described in research design and methods. Results represent means ± SE (n = 8). a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; #P ≤ 0.05 vs. ObControl, analyzed by linear mixed models statistics (SPSS), which also calculated the allover results based on all available data.
Acyl-CoA fractions.
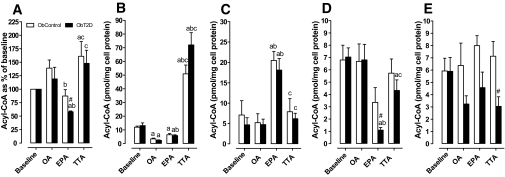
Total acyl-CoA was increased relative to baseline after preincubation with TTA, whereas preincubation with EPA reduced acyl-CoA by >40% in type 2 diabetes myotubes but significantly less in control cells (Fig. 5A). Preincubation with EPA reduced C18:1-CoA by an average of 61% (not shown; P < 0.05) and C16:0-CoA by 46–55% (Fig. 5B) relative to baseline, whereas C16:1-CoA was markedly increased (Fig. 5C). EPA also substantially reduced the level of C18:2-CoA relative to baseline in type 2 diabetes myotubes, to a level significantly lower than in control myotubes (Fig. 5D). Preincubation with oleic acid reduced C16:0-CoA by 71–82% (Fig. 5B) and increased C18:1-CoA by an average of 75% (not shown; P < 0.05) relative to baseline. TTA-CoA and C16:0-CoA had similar retention times and therefore appeared in the same peak on the chromatogram. The relative increase in acyl-CoA after preincubation with TTA (Fig. 5A) could be ascribed to a marked increase in the combined TTA/C16:0-CoA peak compared with C16:0-CoA at baseline (Fig. 5B). Interestingly, C20:4-CoA was decreased in type 2 diabetes compared with control myotubes after fatty acid preincubations and significantly after TTA (Fig. 5E).
FIG. 5.
Cellular acyl-CoA relative to baseline. Differentiated myotubes were preincubated as described in Fig. 1 before the cells were harvested for measurement of acyl-CoA. A: shows total acyl-CoA relative to baseline; and B–E: display C16:0-CoA (and TTA-CoA where preincubated with TTA), C16:1-CoA, C18:2-CoA, and C20:4-CoA, respectively. Results represent means ± SE (n = 6–8). a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; c, P ≤ 0.05 vs. TTA. #P ≤ 0.05 vs. ObControl. Evaluated by nonparametric Mann-Whitney and Wilcoxon's signed-rank test.
Glucose metabolism.
Diabetic myotubes displayed an allover (basal and insulin-stimulated) 10% decreased glucose oxidation compared with control cells (results not shown; P < 0.05). Basal and insulin-mediated glucose oxidation was enhanced after preincubation with EPA (24%) and TTA (28%) in myotubes from both groups (results not shown, P < 0.05). Glucose uptake and glycogen synthesis, however, were mostly unaffected by preincubations with fatty acids (data not shown). Thus, preincubation with EPA and TTA may have reduced nonoxidized glucose metabolites like lactate and pyruvate, accounting for the increased glucose oxidation. Moreover, the mRNA expression of GLUT4, GLUT1, and HKII were unchanged after fatty acid preincubations (results not shown).
TTA inhibits the oleic acid–mediated increase of cell-associated 14C–palmitic acid.
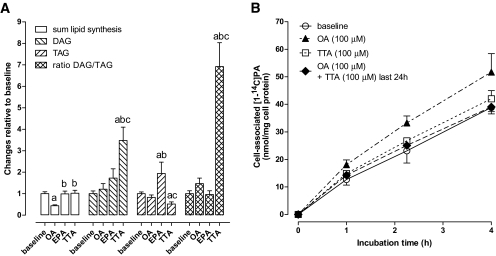
We monitored incorporation of 14C-TTA into complex cellular lipids and found that only a minimal amount was recovered in the TAG fraction, whereas most was found in phospholipids (not shown). De novo synthesis of fatty acids from 14C-acetate was similar after 4 days of preincubation of myotubes with TTA compared with baseline (Fig. 6A), but the ratio between radioactivity recovered in DAG and TAG was sevenfold higher after TTA (Fig. 6A). To further elucidate the impact of TTA on cellular fatty acid accumulation, we monitored the time course for cell-associated 14C–palmitic acid by scintillation proximity assay (SPA). As expected, 4 days of preincubation with oleic acid caused enhanced cell-associated 14C–palmitic acid (Fig. 6B). TTA itself caused no change compared with baseline, and addition of TTA for the last 24 h of the oleic acid preincubation period was sufficient to inhibit the oleic acid–mediated increase in cell-associated 14C–palmitic acid (Fig. 6B). Together, these data suggest that TTA or TTA-CoA may reduce fatty acid–stimulated TAG synthesis, possibly by inhibiting DGAT activity as also suggested previously in rat livers (26).
FIG. 6.
Partitioning of de novo synthesized fatty acids in DAG and TAG (A) and effect of TTA on oleic acid–mediated increase in cell-associated 14C–palmitic acid (B). A: Distribution of de novo synthesized 14C-acetate–derived fatty acids after 4 h in complex lipids (DAG and TAG) after 4-day preincubation of human myotubes from healthy donors with 40 μmol/l fatty acid–free BSA (baseline), 100 μmol/l oleic acid, 100 μmol/l EPA, or 100 μmol/l TTA (n = 4). B: Cell-associated 14C–palmitic acid measured by SPA in human myotubes from healthy donors preincubated 4 days with 40 μmol/l BSA (baseline), 100 μmol/l oleic acid, 100 μmol/l TTA, or 100 μmol/l oleic acid + 100 μmol/l TTA the last day (n = 4). Results represent means ± SE. a, P ≤ 0.05 vs. baseline; b, P ≤ 0.05 vs. oleic acid; c, P ≤ 0.05 vs. EPA, analyzed by linear mixed models statistics (SPSS).
DISCUSSION
Cultured human myotubes is the most similar cell system to intact skeletal muscle that can be modulated ex vivo. Compared with rodent models, they express the right genetic background and the specific skeletal muscle phenotype. The extracellular environment can be controlled precisely and kept relatively constant over time, without interference by systemic homeostatic compensatory mechanisms. We and others have reported several potential intrinsic deficiencies in myotubes from individuals with type 2 diabetes (20–22). These differences appear most obvious when comparing myotubes established from lean with obese type 2 diabetic subjects but are not always significant when comparing obese with obese type 2 diabetes (27). We studied the effects of EPA and TTA on the intermediary energy metabolism and insulin resistance in myotubes established from obese subjects with type 2 diabetes and obese healthy subjects. We have previously demonstrated reduced capacity for complete oxidation of labeled palmitic acid to CO2 in myotubes from obese type 2 diabetic subjects compared with obese control myotubes (21), and this dysfunction was reproduced in our present study. Here, we observed that CO2 production from labeled palmitic acid was reduced for diabetic myotubes (Fig. 7A vs. B). Furthermore, the release of fatty acid β-oxidation products (ASMs) was increased by type 2 diabetes compared with control myotubes after preincubation with fatty acids (Fig. 7C vs. D). Our data suggest that mitochondrial dysfunction in type 2 diabetes myotubes is probably caused by disturbances downstream of fatty acid β-oxidation leading to excess production and release of ASMs during increased influx and/or β-oxidation of fatty acids. In support for this, several studies have suggested a mitochondrial dysfunction in the etiology of insulin resistance and type 2 diabetes (4,6,28). Moreover, increased levels of β-oxidation products have been found in both murine skeletal muscle and plasma, probably reflecting mitochondrial overload due to excess availability of fatty acids (29,30).
FIG. 7.
Changes in energy metabolism in human myotubes after preincubation with fatty acids. We observed a reduced oxidative metabolism (CO2 formation) of fatty acids and glucose in obese type 2 diabetes myotubes compared with obese control cells (A vs. B). Incubation with EPA or TTA promoted increased β-oxidation in diabetic cells (C vs. D). EPA enhanced lipid uptake, accumulation of TAG (especially in diabetic cells), and fatty acid β-oxidation in both groups of myotubes (C and D). TTA “normalized” complete lipid oxidation in diabetic myotubes to baseline level in control cells (A and B vs. D) and opposed increased lipid accumulation (C and D). Glucose oxidation was enhanced after chronic exposure to EPA and TTA, reducing nonoxidized glucose (NOG; C and D). NOG consists mostly of lactate and pyruvate. dotted arrows, reduced; fortified arrows, increased; boxes labeled with EPA and TTA, effects of preincubation.
Excess FFA taken up by myotubes may either be oxidized or stored as TAG. PGC1α is an important regulator of muscle oxidative capacity, mitochondrial content, and fiber type (31,32), and insulin resistance may be negatively associated with PGC1α expression in skeletal muscle (33,34). In the present study, gene expression of PGC1α was increased in response to fatty acids, but the relative response was blunted in diabetic myotubes compared with control cells. In C2C12 myotubes, PGC1α expression was enhanced after 4 h but reduced after 16 h of incubation with palmitic acid (35), whereas unsaturated fatty acids like oleic acid and linoleic acid enhanced PGC1α expression in human myotubes (36). Our data suggest that the reduced capacity for complete mitochondrial fatty acid oxidation observed for type 2 diabetes myotubes might be related to suboptimal responses in expression of PGC1α, e.g., when the myotubes are exposed to fatty acids. DGAT2, which is involved in TAG formation (37), showed a similar expression pattern to PGC1α, and the expression of these genes correlated well (r = 0.81, P < 0.0001). Reduced DGAT2 gene expression after preincubation with fatty acids in diabetic cells, together with impaired complete fatty acid oxidation, may contribute to enhanced levels of potentially lipotoxic intracellular fatty acid intermediates and might play a role in lipid-induced insulin resistance.
Preincubation of myotubes with EPA led to increased production of ASMs, whereas TTA increased both ASMs and CO2 production (Fig. 7C and D). Increased formation of β-oxidation intermediates may cause mitochondrial stress and induce skeletal muscle insulin resistance (30,38). However, we did not observe any detrimental effects of chronic preincubation with either EPA or TTA on insulin-stimulated glucose metabolism in human myotubes. This does not exclude any such link, because we did not coincubate with fatty acids during the glucose experiments that might be a prerequisite for negative effects to occur. Nevertheless, Power et al. (39) showed that supplementation with l-carnitine could ameliorate rather than worsen insulin resistance in mice, despite increased levels of β-oxidation products in plasma and skeletal muscle. Furthermore, preincubation with EPA and TTA increased glucose oxidation, suggesting improved instead of reduced capacity for glucose handling (Fig. 7C and D).
Preincubation of myotubes with the naturally occurring fatty acids enhanced 14C–palmitic acid uptake in line with previous observations (8,10), and EPA was more effective than oleic acid (Fig. 7C and D). Preincubation with oleic acid, and especially EPA, also promoted increased incorporation of 14C–palmitic acid into TAG, and the response to EPA was more pronounced in diabetic myotubes (Fig. 7C vs. D). We observed a negative correlation between total fatty acid oxidation and TAG synthesis in the presence of EPA, suggesting that EPA may redirect excess fatty acids into TAG. Storage of excess fatty acids such as TAG may protect against cell damage due to neutralization of lipotoxic intermediates (40,41). Furthermore, EPA reduced the total amount of acyl-CoA, in particular C18:2-CoA, and the reduction was greatest for diabetic myotubes. Increased levels of acyl-CoA and especially C18:2-CoA have been associated with insulin resistance (42,43). Moreover, EPA markedly increased the level of C16:1-CoA, which has recently been shown to function as a lipokine improving peripheral insulin action (44) and glucose metabolism in L6 rat myotubes (45). In addition, incubation of myotubes from normal lean subjects with EPA improved glucose uptake, despite an increased incorporation of 14C–oleic acid into TAG (10). In rats, EPA also improved insulin resistance while increasing imTAG levels (46).
Preincubation with TTA increased complete oxidation of 14C–palmitic acid to CO2 to a similar degree in control and diabetic myotubes. Thus, TTA “restored” complete palmitic acid oxidation in diabetic cells to baseline level of control myotubes (Fig. 7A and B vs. D). The uptake of palmitic acid was increased after preincubation with TTA but did not lead to similar accumulation of 14C–palmitic acid into TAG compared with preincubation with oleic acid or EPA. The reduced TAG accumulation may reflect enhanced fatty acid oxidation, and we have data showing increased TAG accumulation from 14C–palmitic acid after TTA preincubation when myotubes were acutely coincubated with the CPT1 inhibitor etomoxir (A.J.W., A.C.R., unpublished observations). Alternatively, TTA-CoA may inhibit DGAT activity (26), as also suggested by the markedly increased cellular DAG-to-TAG recovery ratio of 14C-acetate in the presence of TTA, without changes in lipid synthesis. Furthermore, we observed that 14C-TTA itself could not be efficiently incorporated into TAG in human myotubes and that coincubation with TTA prevented the oleic acid–induced increase in cell-associated 14C–palmitic acid. Moreover, myotubes preincubated with TTA had enhanced levels of acyl-CoA and TTA-CoA probably accounted for most of the difference because 3-thia fatty acids cannot undergo β-oxidation (14). However, preincubation of myotubes with TTA neither impaired insulin-stimulated glucose uptake nor glycogen synthesis, whereas glucose oxidation was increased in cells from both donor groups (Fig. 7C and D).
TTA may enhance mitochondrial proliferation in skeletal muscle (17), and activation of PPAR nuclear receptors probably mediates much of the effects of TTA on gene expression (16,18,26). Because there were no differences in induction of CPT1 expression after preincubation with TTA relative to oleic acid and EPA, the enhanced β-oxidation after TTA may be explained by the twofold higher induction of CD36/FAT expression. CD36 may facilitate fatty acid transport across the plasma membrane in response to contraction and insulin (47), but CD36 may also reside on the outer mitochondrial membrane (48) in colocalization with CPT1 to facilitate mitochondrial fatty acid influx (48,49). In rats, the PPARγ agonist rosiglitazone increased skeletal muscle fatty acid oxidation and mitochondrial CD36 amount, but not CPT1 protein expression or activity (49), which is in line with our observations. Part of the increased oxidation of 14C–palmitic acid to CO2 after preincubation with TTA may be related to the increased UCP2 expression and mitochondrial uncoupling (50). Thus, preincubation with the synthetic fatty acid analog TTA enhanced complete fatty acid and glucose oxidation in diabetic myotubes and opposed the increased lipid accumulation observed after preincubation with oleic acid and especially EPA.
In summary, type 2 diabetes myotubes seem to have an impaired mitochondrial capacity for fatty acid oxidation and glucose (Fig. 7A vs. B), linked to defects downstream of fatty acid β-oxidation, leading to increased release of ASMs during high fatty acid availability (Fig. 7C vs. D). Reduced response of PGCα to fatty acids in diabetic myotubes may be associated with reduced mitochondrial function and reduced DGAT activity, creating lipid intermediates and consequently insulin resistance. TTA and EPA might execute beneficial effects by increasing complete fatty acid oxidation and TAG formation, respectively (Fig. 7C and D), thereby improving overall energy metabolism and fatty acid handling in type 2 diabetes skeletal muscle.
Supplementary Material
Acknowledgments
Lipgene (Integrated Project 6th Framework Programme, Food Quality, and Safety; FOOD-CT-2003-505944), Freia Chocolade Fabriks Medical Foundation, The Johan Throne Holst Foundation for Nutrition Research, The Danish Medical Research Council, the Danish Diabetes Association, and the Novo-Nordisk Foundation provided financial support.
R.K.B. and the University of Bergen, Haukeland University Hospital, are shareholders of THIA MEDICA, which holds patents regarding effects of TTA. No other potential conflicts of interest relevant to this article were reported.
We thank Irene Lynfort for excellent technical assistance. We thank Kurt Højlund and Klaus Levin for the muscle biopsies and Jens Knudsen for assisting in measurements of acyl-CoA.
Published ahead of print at http://diabetes.diabetesjournals.org on 9 December 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Storlien LH, Jenkins AB, Chisholm DJ, Pascoe WS, Khouri S, Kraegen EW: Influence of dietary fat composition on development of insulin resistance in rats: relationship to muscle triglyceride and ω-3 fatty acids in muscle phospholipid. Diabetes 40: 280–289, 1991 [DOI] [PubMed] [Google Scholar]
- 2.Pan DA, Lillioja S, Kriketos AD, Milner MR, Baur LA, Bogardus C, Jenkins AB, Storlien LH: Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 46: 983–988, 1997 [DOI] [PubMed] [Google Scholar]
- 3.Boden G: Interaction between free fatty acids and glucose metabolism. Curr Opin Clin Nutr Metab Care 5: 545–549, 2002 [DOI] [PubMed] [Google Scholar]
- 4.Simoneau JA, Kelley DE: Altered glycolytic and oxidative capacities of skeletal muscle contribute to insulin resistance in NIDDM. J Appl Physiol 83: 166–171, 1997 [DOI] [PubMed] [Google Scholar]
- 5.He J, Watkins S, Kelley DE: Skeletal muscle lipid content and oxidative enzyme activity in relation to muscle fiber type in type 2 diabetes and obesity. Diabetes 50: 817–823, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI: Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science 300: 1140–1142, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kase ET, Wensaas AJ, Aas V, Hojlund K, Levin K, Thoresen GH, Beck-Nielsen H, Rustan AC, Gaster M: Skeletal muscle lipid accumulation in type 2 diabetes may involve the liver X receptor pathway. Diabetes 54: 1108–1115, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Gaster M, Beck-Nielsen H: Triacylglycerol accumulation is not primarily affected in myotubes established from type 2 diabetic subjects. Biochim Biophys Acta 1761: 100–110, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Kraegen EW, Cooney GJ: Free fatty acids and skeletal muscle insulin resistance. Curr Opin Lipidol 19: 235–241, 2008 [DOI] [PubMed] [Google Scholar]
- 10.Aas V, Rokling-Andersen MH, Kase ET, Thoresen GH, Rustan AC: Eicosapentaenoic acid (20:5 n-3) increases fatty acid and glucose uptake in cultured human skeletal muscle cells. J Lipid Res 47: 366–374, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Lee JS, Pinnamaneni SK, Eo SJ, Cho IH, Pyo JH, Kim CK, Sinclair AJ, Febbraio MA, Watt MJ: Saturated, but not n-6 polyunsaturated, fatty acids induce insulin resistance: role of intramuscular accumulation of lipid metabolites. J Appl Physiol 100: 1467–1474, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Coll T, Eyre E, Rodriguez-Calvo R, Palomer X, Sanchez RM, Merlos M, Laguna JC, Vazquez-Carrera M: Oleate reverses palmitate-induced insulin resistance and inflammation in skeletal muscle cells. J Biol Chem 283: 11107–11116, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Storlien LH, Kraegen EW, Chisholm DJ, Ford GL, Bruce DG, Pascoe WS: Fish oil prevents insulin resistance induced by high-fat feeding in rats. Science 237: 885–888, 1987 [DOI] [PubMed] [Google Scholar]
- 14.Berge RK, Tronstad KJ, Berge K, Rost TH, Wergedahl H, Gudbrandsen OA, Skorve J: The metabolic syndrome and the hepatic fatty acid drainage hypothesis. Biochimie 87: 15–20, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Balakumar P, Rose M, Ganti SS, Krishan P, Singh M: PPAR dual agonists: are they opening Pandora's Box? Pharmacol Res 56: 91–98, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Madsen L, Guerre-Millo M, Flindt EN, Berge K, Tronstad KJ, Bergene E, Sebokova E, Rustan AC, Jensen J, Mandrup S, Kristiansen K, Klimes I, Staels B, Berge RK: Tetradecylthioacetic acid prevents high fat diet induced adiposity and insulin resistance. J Lipid Res 43: 742–750, 2002 [PubMed] [Google Scholar]
- 17.Totland GK, Madsen L, Klementsen B, Vaagenes H, Kryvi H, Froyland L, Hexeberg S, Berge RK: Proliferation of mitochondria and gene expression of carnitine palmitoyltransferase and fatty acyl-CoA oxidase in rat skeletal muscle, heart and liver by hypolipidemic fatty acids. Biol Cell 92: 317–329, 2000 [DOI] [PubMed] [Google Scholar]
- 18.Løvås K, Røst TH, Skorve J, Ulvik RJ, Gudbrandsen OA, Bohov P, Wensaas AJ, Rustan AC, Berge RK, Husebye ES: Tetradecylthioacetic acid attenuates dyslipidemia in male patients with type 2 diabetes mellitus, possibly by dual PPARα/δ activation and increased mitochondrial oxidation. Diabetes Obes Metab. In press. Available from http://dx.doi.org/10.1111/j.1463-1326.2008.00958.x [DOI] [PubMed]
- 19.Gaster M, Kristensen SR, Beck-Nielsen H, Schroder HD: A cellular model system of differentiated human myotubes. APMIS 109: 735–744, 2001 [DOI] [PubMed] [Google Scholar]
- 20.Henry RR, Abrams L, Nikoulina S, Ciaraldi TP: Insulin action and glucose metabolism in nondiabetic control and NIDDM subjects: comparison using human skeletal muscle cell cultures. Diabetes 44: 936–946, 1995 [DOI] [PubMed] [Google Scholar]
- 21.Gaster M, Rustan AC, Aas V, Beck-Nielsen H: Reduced lipid oxidation in skeletal muscle from type 2 diabetic subjects may be of genetic origin: evidence from cultured myotubes. Diabetes 53: 542–548, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Gaster M, Petersen I, Hojlund K, Poulsen P, Beck-Nielsen H: The diabetic phenotype is conserved in myotubes established from diabetic subjects: evidence for primary defects in glucose transport and glycogen synthase activity. Diabetes 51: 921–927, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Skrede S, Bremer J, Berge RK, Rustan AC: Stimulation of fatty acid oxidation by a 3-thia fatty acid reduces triacylglycerol secretion in cultured rat hepatocytes. J Lipid Res 35: 1395–1404, 1994 [PubMed] [Google Scholar]
- 24.Just M, Faergeman NJ, Knudsen J, Beck-Nielsen H, Gaster M: Long-chain Acyl-CoA is not primarily increased in myotubes established from type 2 diabetic subjects. Biochim Biophys Acta 1762: 666–672, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Wensaas AJ, Rustan AC, Lovstedt K, Kull B, Wikstrom S, Drevon CA, Hallen S: Cell-based multiwell assays for the detection of substrate accumulation and oxidation. J Lipid Res 48: 961–967, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Berge RK, Madsen L, Vaagenes H, Tronstad KJ, Gottlicher M, Rustan AC: In contrast with docosahexaenoic acid, eicosapentaenoic acid and hypolipidaemic derivatives decrease hepatic synthesis and secretion of triacylglycerol by decreased diacylglycerol acyltransferase activity and stimulation of fatty acid oxidation. Biochem J 343: 191–197, 1999 [PMC free article] [PubMed] [Google Scholar]
- 27.Gaster M: Insulin resistance and the mitochondrial link: lessons from cultured human myotubes. Biochim Biophys Acta 1772: 755–765, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Mogensen M, Sahlin K, Fernstrom M, Glintborg D, Vind BF, Beck-Nielsen H, Hojlund K: Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 56: 1592–1599, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Koves TR, Li P, An J, Akimoto T, Slentz D, Ilkayeva O, Dohm GL, Yan Z, Newgard CB, Muoio DM: Peroxisome proliferator-activated receptor-gamma co-activator 1alpha-mediated metabolic remodeling of skeletal myocytes mimics exercise training and reverses lipid-induced mitochondrial inefficiency. J Biol Chem 280: 33588–33598, 2005 [DOI] [PubMed] [Google Scholar]
- 30.Koves TR, Ussher JR, Noland RC, Slentz D, Mosedale M, Ilkayeva O, Bain J, Stevens R, Dyck JR, Newgard CB, Lopaschuk GD, Muoio DM: Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab 7: 45–56, 2008 [DOI] [PubMed] [Google Scholar]
- 31.Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM: Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell 98: 115–124, 1999 [DOI] [PubMed] [Google Scholar]
- 32.Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, Michael LF, Puigserver P, Isotani E, Olson EN, Lowell BB, Bassel-Duby R, Spiegelman BM: Transcriptional co-activator PGC-1 alpha drives the formation of slow-twitch muscle fibres. Nature 418: 797–801, 2002 [DOI] [PubMed] [Google Scholar]
- 33.Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC: PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 34: 267–273, 2003 [DOI] [PubMed] [Google Scholar]
- 34.Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ: Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A 100: 8466–8471, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coll T, Jove M, Rodriguez-Calvo R, Eyre E, Palomer X, Sanchez RM, Merlos M, Laguna JC, Vazquez-Carrera M: Palmitate-mediated downregulation of peroxisome proliferator-activated receptor-γ coactivator 1α in skeletal muscle cells involves MEK1/2 and nuclear factor-κB activation. Diabetes 55: 2779–2787, 2006 [DOI] [PubMed] [Google Scholar]
- 36.Staiger H, Staiger K, Haas C, Weisser M, Machicao F, Haring HU: Fatty acid-induced differential regulation of the genes encoding peroxisome proliferator-activated receptor-gamma coactivator-1alpha and -1beta in human skeletal muscle cells that have been differentiated in vitro. Diabetologia 48: 2115–2118, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Man WC, Miyazaki M, Chu K, Ntambi J: Colocalization of SCD1 and DGAT2: implying preference for endogenous monounsaturated fatty acids in triglyceride synthesis. J Lipid Res 47: 1928–1939, 2006 [DOI] [PubMed] [Google Scholar]
- 38.An J, Muoio DM, Shiota M, Fujimoto Y, Cline GW, Shulman GI, Koves TR, Stevens R, Millington D, Newgard CB: Hepatic expression of malonyl-CoA decarboxylase reverses muscle, liver and whole-animal insulin resistance. Nat Med 10: 268–274, 2004 [DOI] [PubMed] [Google Scholar]
- 39.Power RA, Hulver MW, Zhang JY, Dubois J, Marchand RM, Ilkayeva O, Muoio DM, Mynatt RL: Carnitine revisited: potential use as adjunctive treatment in diabetes. Diabetologia 50: 824–832, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Listenberger LL, Han X, Lewis SE, Cases S, Farese RV Jr, Ory DS, Schaffer JE: Triglyceride accumulation protects against fatty acid-induced lipotoxicity. Proc Natl Acad Sci U S A 100: 3077–3082, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu L, Zhang Y, Chen N, Shi X, Tsang B, Yu YH: Upregulation of myocellular DGAT1 augments triglyceride synthesis in skeletal muscle and protects against fat-induced insulin resistance. J Clin Invest 117: 1679–1689, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ellis BA, Poynten A, Lowy AJ, Furler SM, Chisholm DJ, Kraegen EW, Cooney GJ: Long-chain acyl-CoA esters as indicators of lipid metabolism and insulin sensitivity in rat and human muscle. Am J Physiol Endocrinol Metab 279: E554–E560, 2000 [DOI] [PubMed] [Google Scholar]
- 43.Yu C, Chen Y, Cline GW, Zhang D, Zong H, Wang Y, Bergeron R, Kim JK, Cushman SW, Cooney GJ, Atcheson B, White MF, Kraegen EW, Shulman GI: Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem 277: 50230–50236, 2002 [DOI] [PubMed] [Google Scholar]
- 44.Cao H, Gerhold K, Mayers JR, Wiest MM, Watkins SM, Hotamisligil GS: Identification of a lipokine, a lipid hormone linking adipose tissue to systemic metabolism. Cell 134: 933–944, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dimopoulos N, Watson M, Sakamoto K, Hundal HS: Differential effects of palmitate and palmitoleate on insulin action and glucose utilization in rat L6 skeletal muscle cells. Biochem J 399: 473–481, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kusunoki M, Tsutsumi K, Hara T, Ogawa H, Nakamura T, Miyata T, Sakakibara F, Fukuzawa Y, Suga T, Kato K, Hirooka Y, Nakaya Y: Ethyl icosapentate (omega-3 fatty acid) causes accumulation of lipids in skeletal muscle but suppresses insulin resistance in OLETF rats: Otsuka Long-Evans Tokushima Fatty. Metabolism 52: 30–34, 2003 [DOI] [PubMed] [Google Scholar]
- 47.Luiken JJ, Dyck DJ, Han XX, Tandon NN, Arumugam Y, Glatz JF, Bonen A: Insulin induces the translocation of the fatty acid transporter FAT/CD36 to the plasma membrane. Am J Physiol Endocrinol Metab 282: E491–E495, 2002 [DOI] [PubMed] [Google Scholar]
- 48.Campbell SE, Tandon NN, Woldegiorgis G, Luiken JJ, Glatz JF, Bonen A: A novel function for fatty acid translocase (FAT)/CD36: involvement in long chain fatty acid transfer into the mitochondria. J Biol Chem 279: 36235–36241, 2004 [DOI] [PubMed] [Google Scholar]
- 49.Benton CR, Holloway GP, Campbell SE, Yoshida Y, Tandon NN, Glatz JF, Luiken JJ, Spriet LL, Bonen A: Rosiglitazone increases fatty acid oxidation and fatty acid translocase (FAT/CD36) but not carnitine palmitoyltransferase I in rat muscle mitochondria. J Physiol 586: 1755–1766, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Echtay KS, Winkler E, Frischmuth K, Klingenberg M: Uncoupling proteins 2 and 3 are highly active H(+) transporters and highly nucleotide sensitive when activated by coenzyme Q (ubiquinone). Proc Natl Acad Sci U S A 98: 1416–1421, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.