Abstract
Purpose
The Vision First program began in the fall of 2002 as a community outreach initiative by the Cleveland Clinic Cole Eye Institute in partnership with the Cleveland Metropolitan School District. It was designed to provide free eye examinations to all prekindergarten, kindergarten, and first grade students enrolled in Cleveland City public schools in order to diagnose refractive errors, amblyopia, and strabismus, so that treatment is instituted and the best possible visual outcome attained.
Methods
Examinations are performed in 2 lanes of a specially outfitted recreational vehicle. All children undergo monocular visual acuity testing at distance and near, stereopsis testing, cover testing at distance and near, testing of versions, and external ocular inspection. If a child fails any part of this examination according to the guidelines set by the American Academy of Pediatrics, cycloplegic drops are instilled and an optometrist refracts the child on location and performs indirect ophthalmoscopy. Glasses are prescribed and follow-up with a pediatric ophthamologist is arranged.
Results
During the first 4 years of the program, 22,988 examinations were performed. Seven percent of children had errors of refraction that necessitated optical correction, about 2.1% had strabismus, and 1.7% had amblyopia. The cost per student per year was around $23 excluding glasses.
Conclusions
About 10% of 5- and 6-year-old schoolchildren have eye problems that require either glasses or treatment for strabismus or amblyopia. The Vision First model brings eye care professionals to the schools and provides effective comprehensive screening of all children, as well as detailed examination and referral of those with significant eye problems.
INTRODUCTION
In 1899, Connecticut instituted the first state-supported school vision screening test, setting an important precedent despite problems with poorly standardized testing conditions and insufficient funds for following up those who failed the vision screening. Over 100 years later, rates of vision screening among school-aged children remain relatively low, in part because of the controversy over the effectiveness of screening techniques as compared with examinations based on symptoms, and the unclear relationship between undiagnosed visual impairment and academic performance.1,2 While some studies have linked undetected or uncorrected visual impairment to poor academic performance, high school dropout rates, and even juvenile delinquency, others have argued that there is little evidence to support such a link.2–5 What is irrefutable is that undetected amblyopia, strabismus, and significant refractive errors can have significant long-term effects on visual function and in some patients can cause permanent unilateral or bilateral vision loss.
Few studies have examined the prevalence of common visual problems in US inner city schoolchildren.6,7 We present 4-year data from the Vision First project that serves the Cleveland Metropolitan School District (CMSD). The information we provide will hopefully give a better understanding of the prevalence of common visual problems among children living in the inner city of Cleveland, particularly those of the African American majority. We also present data on the administration and cost of this unique program and offer it as one model for effective detection and treatment of eye problems in young children. A greater understanding of the eye problems in this population of children should aid pediatricians and vision specialists in caring for inner city pediatric populations. It could also aid in advocating for greater funding and support for mass vision screening and examination programs in both the public and private sectors.
METHODS
Because the data in this paper are being analyzed retrospectively and anonymously, no institutional review board (IRB) consent form needed to be signed. IRB approval for an exemption from consent has been obtained. Written consent to participate in the screening/examination was obtained, and parents/guardians were informed of minor risks, such as an allergic reaction to the eye drops used in the eye examination.
We targeted the Vision First program to children in prekindergarten, kindergarten, and first grade in the CMSD because younger and older children were already receiving services through other private and public programs. Funding was obtained through private donors and organizations and was supplemented by the City of Cleveland. A number of organizational meetings occurred between the Cleveland Clinic team and the school nurses and administrators.
The Vision First personnel work closely with the nurses from the CMSD to coordinate the school visits. A schedule for the visits is prepared in the summer and the van travels to the schools on predetermined dates. There are no exclusion criteria, and all children enrolled in the 3 first grades at the CMSD schools are invited to participate. Permission slips for ocular examinations and eye drop administration are sent home with the children by the school nurses and are signed by the children’s caregivers. The van is parked close to one of the school exits, and children are escorted by school nurses to the vehicle where testing is conducted. Eye examinations are performed by trained ophthalmic personnel, including an ophthalmic technician (who also serves as the coordinator of the program and the driver of the van) and an optometrist, out of a specially outfitted recreational vehicle (Figure). Children with strabismus, amblyopia, or other medical eye problems are referred to pediatric ophthalmologists for specialty eye care and follow-up. Children with simple refractive errors had been given prescriptions and vouchers for eyeglasses until 2007, when additional funding was obtained that provides a pair of glasses for each student. These are made to order and delivered to the schools after the completion of the examinations, where they are distributed to the students.
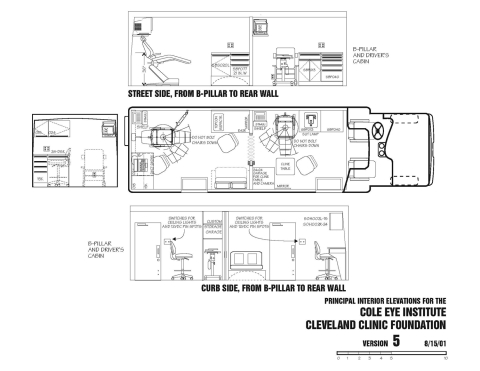
FIGURE.
Floor plan of the customized recreational vehicle used for Vision First eye examinations. There are two examination lanes. Students enter from the rear door, where part 1 of the examination is done. The front examination lane is used by the optometrist for refraction and fundus examination.
The examination consists of 2 parts. The first part is administered by an ophthalmic technician or an optometrist, who tests one child at a time. Monocular distance visual acuity is measured using Snellen letters or Allen figures, depending on the child’s age and ability. Monocular near visual acuity is obtained using Allen figures or numbers. Stereopsis is assessed using the Titmus test. Cover and alternating cover tests for distance and near are performed to detect strabismus. Extraocular movements are evaluated using a broad H pattern and a near target. Pupillary responses are checked using a transilluminator. External observation is used to detect facial abnormalities such as ptosis or microphthalmia. If an error of refraction is suspected, dry retinoscopy is performed. All boys undergo Ishihara color vision test. Children who fail the first part of the examination (see Table 1 for failure criteria) are given cycloplegic eye drops (cyclopentolate 1% drops alone or, in darkly pigmented eyes, in combination with tropicamide 1%). After 30 minutes, the optometrist performs retinoscopy for the presence of a refractive error. The retina and optic nerve are examined with the binocular indirect ophthalmoscope and/or a direct ophthalmoscope. Prescriptions are given for significant errors of refraction (myopia, hypermetropia, and astigmatism) as outlined in Table 2. Children with amblyopia or any ocular pathology are referred to a pediatric ophthalmologist.
TABLE 1.
FAILURE CRITERIA FOR VISION FIRST EYE EXAMINATIONS*
| PART 1 |
| Any external abnormalities, such as ptosis, microphthalmia, anomalous head position, or lacrimal and lid anomalies |
| Visual acuity difference of 2 Snellen lines between eyes or visual acuity less than 20/40 in either eye |
| Stereo acuity less than 400 seconds of arc |
| Any nystagmus |
| Manifest ocular deviation of any type or magnitude with or without fixation preference |
| Any vertical phoria; any esophoria more than 8 prism diopters or exophoria more than 15 prism diopters at near or distance |
| Any restricted eye movement or muscle overaction |
| Any heterochromia, anisocoria, or afferent pupillary defect |
| PART 2 |
| Anisometropia of 1.00 D or greater with any best-corrected visual acuity difference between the 2 eyes |
| Abnormalities of the ocular media |
| Abormal fundus examination |
| Myopia greater than 0.50 D |
| Astigmatism greater than 1.25 D |
| Hypermetropia greater than 1.50 D |
| Any difference between the 2 eyes of 0.75 D or more with corresponding acuity difference |
Children who fail part 1 are dilated and undergo cycloplegic refraction and fundus examination. All children who fail part 1 and/or part 2 are referred to a pediatric ophthalmologist. Glasses are prescribed to those with significant refractive errors immediately.
TABLE 2.
PRESCRIBING CRITERIA FOR GLASSES IN CHILDREN WITH REFRACTIVE ERRORS IN THE VISION FIRST PROGRAM
| FAILING VISUAL ACUITY | CRITERIA |
|---|---|
| Myopia | Any amount |
| Hypermetropia | Reduce cycloplegic retinoscopic amount by +1.50 as long as there is no strabismus |
| Astigmatism | Full amount if over +0.50 |
| PASSING VISUAL ACUITY | |
| Myopia | Usually not a factor; but if child squints, cycloplegic refraction is performed, and if myopia is detected, glasses are prescribed |
| Hypermetropia | Full amount if vision is normal but there is accommodative esotropia |
| Astigmatism | Usually not a factor; but if child squints, cycloplegic refraction is performed and if astigmatism is detected, glasses are prescribed |
| WITH STRABISMUS | |
| Any esodeviation | Full cycloplegic hypermetropic correction |
| Large exophoria (more than 10 prism diopters) | Full myopic correction if present. Reduce hypermetropic correction as much as possible without reducing visual acuity |
The information from each encounter is recorded on a sheet and later entered in a database so that arrangements are made with the school and the parents for the follow-up of children who need medical attention. The results of the examination are sent to the parents on a card. An additional referral form for those children who need to be examined by the pediatric ophthalmologist is also sent to their caregivers. The program coordinator follows up with those who fail the examination and assists in securing a follow-up visit with the ophthalmologist.
RESULTS
More than 80 schools in the CMSD were visited every year, and 50 to 80 children were examined on any given day on the Vision First vehicle. About 50% of parents of all children in prekindergarten, kindergarten, and first grade returned signed consent forms for examinations and eye drop administration (data not shown). Table 3 provides the total number of children examined each school year and the proportion of them who failed the examination, as well as the percentage of students with amblyopia and strabismus. We divided amblyopia into refractive (includes anisometropic and bilateral ametropic), strabismic, and deprivational. The yearly cumulative results for each type are given in Table 4.
TABLE 3.
SELECTED STATISTICS FROM THE VISION FIRST PROGRAM
| 2002–2003 | 2003–2004 | 2004–2005 | 2005–2006 | AVERAGE/TOTAL | |
|---|---|---|---|---|---|
| Number of schools | 81 | 86 | 88 | 80 | 84 |
| Children examined | 5085 | 6387 | 6218 | 5298 | 5747/22988 |
| % who failed part 1 of exam | 9.6% | 7.5% | 10.6% | 11.3% | 9.7% |
| % with amblyopia | 1.4% | 1.85% | 1.6% | 1.7% | 1.7% |
| % with strabismus | 2.6% | 1.9% | 1.7% | 2.2% | 2.1% |
TABLE 4.
AMBLYOPIA IN 4- TO 8-YEAR-OLD SCHOOLCHILDREN IN THE CLEVELAND PUBLIC SCHOOLS
| TYPE OF AMBLYOPIA | PERCENTAGE OF SCHOOLCHILDREN
|
|||
|---|---|---|---|---|
| 2002–2003 | 2003–2004 | 2004–2005 | 2005–2006 | |
| Refractive | 64% | 69% | 69% | 79% |
| Strabismic | 29% | 24% | 26% | 19% |
| Deprivational | 7% | 7% | 5% | 2% |
The expenses of the Vision First program consisted of an initial investment in the purchase of the customized vehicle and of major equipment, in addition to the salaries of the operating personnel, disposables, insurance, and fuel. We estimated the cost of examining each child by dividing the yearly expenses by the number of children who participated in the program. This data is given in Table 5.
TABLE 5:
COST PER STUDENT TO RUN THE VISION FIRST PROGRAM
| 2003 | 2004 | 2005 | 2006 | Average | |
|---|---|---|---|---|---|
| Cost per pupil in US$ | $22.45 | $20.31 | $22.24 | $27.58 | $23.14 |
DISCUSSION
There is no disagreement about the utility of early detection of amblyopia and amblyogenic factors, and although some have expressed doubt over the need for screening for amblyopia in younger children, asserting that many mild cases of amblyopia may resolve on their own, a study examining children with untreated amblyopia due to poor compliance found no evidence of spontaneous improvement.8 Of 18 4- to 6-year-old children who were reexamined a year after their initial screening, visual acuity improved in none except a child whose compliance had been sporadic; 7 (41%) of the remaining 17 children had actually shown a deterioration of visual acuity in the amblyopic eye.9 Because of the benefit of early detection and treatment of amblyopia, the American Association for Pediatric Ophthalmology and Strabismus, the American Academy of Ophthalmology (AAO), the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Association of Certified Orthoptists all recommend early vision screening (AAO policy). Despite these recommendations, the American Academy of Pediatrics estimates that only 21% of children are adequately screened for amblyopia.10
In 1999, 45 states did not require screening of all preschool children, making access to vision screening programs very difficult for most preschool-aged children.11 The Ohio Department of Health (ODH) has instituted Vision Conservation Programs and has set policies for vision screening, education, referral, and follow-up of children (see http://www.odh.state.oh.us). In its Status of Vision and Hearing Screening in Ohio’s Schools 1996–1997 survey report, the Ohio Department of Health reports that compliance with vision screening is highest in kindergarten.
A study of children treated for amblyopia found that among patients with strabismic amblyopia, less obvious deviations were associated with late diagnosis. Of children with deviations of greater than 10°, 71% were diagnosed before the age of 5, compared with 36% of children with deviations less than 10°.12 This study also provided important support for the role of vision screening in detecting strabismus. Fifty percent of amblyopia cases had originally been identified by school screening, compared to 23% originally detected by primary care pediatricians. The role of school vision screening is especially significant among medically underserved populations. A study of access to care for poor children found that a lower proportion of poor children had normal routine care when compared to children living above the poverty line. This lack of routine care may decrease the chances of vision problems being identified in routine well child checkups and consequently increase the need for school vision screening. It is estimated that only 14% of children younger than 6 years of age undergo an eye examination.13 We estimate that our program provided eye care to 50% of children in the first 3 grades of public school. The parents of the remaining half of this group of students did not provide permission for an examination.
We determined that the most effective way of detecting the great majority of amblyopia and amblyogenic factors, such as anisometropia and strabismus, was to have all children screened by trained ophthalmic personnel who are able to perform accurate and reliable visual acuity testing and who can check for the presence of strabismus. Furthermore, immediate comprehensive eye examinations were necessary to overcome the problems of compliance with recommendations for follow-up with ophthalmologists if a vision screen conducted by a school nurse or volunteer generated a failing result and prompted a referral. We designed the Vision First program to provide a detailed screen (first part of the examination) that was administered to all participating children and a cycloplegic refraction and fundus examination that was given to those children who failed the first part. We provided glasses to those who needed them and referred all children who failed the first part of the examination for a follow-up with community pediatric ophthalmologists.
Visual acuity screening has been found to be less reliable in preschoolers than in school-aged children in detecting significant refractive errors. Comparison of visual acuity screening using Lea Symbols logMAR chart to noncycloplegic autorefraction screening using Nikon Retinomax K-Plus and to cycloplegic retinoscopy was done in 245 Native Americans 3 to 5 years old in a Head Start program.14 Visual acuity screening was possible in 96% of children, and cycloplegic retinoscopy and noncycloplegic autorefraction screening were done on 100% of children. Thirty-one percent of children had significant degrees of astigmatism (more than 50th percentile of what is considered significant according to an American Association of Pediatric Ophthalmology and Strabismus membership survey). Visual acuity screening was 90% sensitive and 44% specific, and noncycloplegic autorefraction screening was 91% sensitive and 86% specific. According to Miller and associates,14 the latter becomes cost-effective after 1000 screens. Cycloplegic retinoscopy was evidently 100% sensitive and specific. This was the main reason for choosing cycloplegic retinoscopy as the means of determining the need for glasses for the Vision First program.
It is not the purpose of this report to compare methods of vision screening but rather to present a program that was designed to provide what we perceived to be the best possible way of detecting eye problems in young children in order to detect errors of refraction, strabismus, and amblyopia, and institute the appropriate management. Children in this 4- to 8-year age-group generally cooperate well with examinations and, with few exceptions, theoretically benefit greatly from the institution of amblyopia therapy. The Vision First program should not be regarded as a simple vision screening program, but rather a comprehensive professional screening and management program.
A number of studies have examined the prevalence of common visual problems among various pediatric populations in the United States and examined the role of vision screening in identifying these disorders.15–17 Yet, variations in prevalence estimates of common visual disorders still remain, and it has been suggested that the demographic makeup of the population may influence the prevalence of some visual problems. A study describing the distribution of visual acuity and causes of visual loss among 6-year-olds in Australia found that visual impairment was more common among children of lower socioeconomic status and among girls than boys.18 One study also examined differences between ethnic groups in the prevalence of common causes of visual impairment. Kleinstein and colleagues19 compared the prevalence of myopia, hyperopia, and astigmatism between African Americans, Asians, Hispanics, and non-Hispanic whites. These investigators found that the prevalence of astigmatism, hyperopia, and myopia was lower among African Americans than the group as a whole. Some of the issues of the association of prevalence with ethnicity and socioeconomic background were also addressed in the Baltimore Vision Screening Project (BVSP), which looked at the prevalence of different causes of visual impairment among children at an inner city school as well as the rates of compliance with recommended treatment.6,7 The BVSP involved one school with a representative population, whereas we present data from all Cleveland elementary schools, giving larger numbers and a better cross section of what is probably a similar population. We believe that our data provide reasonably good estimates of the prevalence of the different eye problems in Cleveland children, particularly African Americans. In the BVSP 75% of 680 students were African American, 22% were white, and 3% were of other ethnicities. The Cleveland public school district serves a socioeconomically deprived population with a similar ethnic makeup, consisting of 70.3% African American, 16.7% white, 10.4% Hispanic, and 2.6% of other ethnicities. The prevalence of errors of refraction, strabismus, and amblyopia in the large sample of children examined in the Vision First program mirrors that of the BVSP conducted in an elementary school in Baltimore.6 Preslan and Novak6 found amblyopia in 3.9% of the school population, with a prevalence of 5.7% in prekindergarten and kindergarten. Strabismus was detected in 3.1% of children and refractive errors that required treatment in 8.2%. We found that 1.7% of children were amblyopic and 2.1% had strabismus. Refractive amblyopia was about twice as common as strabismic amblyopia. Table 6 compares our statistics with those from studies conducted in Turkey,20 Tanzania,21 and Japan.22
TABLE 6.
COMPARISON OF STATISTICS FROM SELECTED STUDIES OF THE PREVALENCE OF EYE PROBLEMS IN CHILDREN FROM AROUND THE WORLD
| COUNTRY | NUMBER OF CHILDREN | % FAILED | % ERRORS OF REFRACTION | % STRABISMUS | % AMBLYOPIA | SOURCE |
|---|---|---|---|---|---|---|
| Turkey | 23,810 | 13% | 11% | 2.5% | 1.1% | Turacli, 199520 |
| Tanzania | 1,386 | 1.7% | 1% | 0.5% | 0.2% | Wedner, 200021 |
| Japan | 84,619 | Not given | Not given | 0.99% | 0.20% | Matsuo, 200722 |
| United States | 22,988 | 9.7% | 7% | 2.1% | 1.7% | Present study |
We encountered a number of problems during the provision of the services by the Vision First program. The most important of these problems relate to parental compliance with recommended follow-up with pediatric ophthalmologists. This was the result of limited access to care as well as simple noncompliance. We tried to address the access problem by offering free examination to those without insurance, and our program coordinator made great efforts to schedule children with amblyopia and/or strabismus for follow-up examinations with varying success. In the Baltimore Vision Screening project, 285 children were screened during the 1994–1995 school year. Of the 68 children who were diagnosed with vision problems, only 30% complied with the recommended treatment, spectacle wear, or both in spite of access to this care through the Baltimore Vision Screening Project.7 For the first 6 years of the Vision First program, vouchers for free spectacles were provided to children who needed them. In the past year and through additional charitable funding, glasses have been made and dispensed after the visit. Data on compliance with recommended follow-up have been difficult to collect and are incomplete, so we cannot provide statistics on this part of the program.
We calculated the cost of providing this service at around $23, excluding glasses. We cannot compare it to the cost of other programs. It was anecdotally estimated that the cost of performing and interpreting photorefraction was around $13. This does not include the cost of performing eye examinations on those who fail this test and the provision of glasses to those who need it. We have not included in our cost estimate the expenses of the city and state on the school nursing personnel who assisted in the administration of the program and the streamlining of the eye examinations.
We believe that the partnership between private charitable organizations and the public school system to support this professional vision care program has been very successful. We continue to struggle with issues of compliance with continuity of care for those children who need it. We are contemplating the addition of a social worker to the program to help address this issue.
PEER DISCUSSION
DR. STEVEN M. ARCHER
The current political reality regarding vision screening is not to question whether it is worth doing, but rather to legislate what type of vision screening program we will spend our surplus tax revenue on. Complete examination of all children is the agenda being championed by organized optometry and eyeglass manufacturers (both of whom stand to benefit financially from a large number of children being examined in optometry offices). Ophthalmology, on the other hand, has generally maintained that a screening test administered by lay personnel is more cost effective and avoids issues of financial conflict of interest; historically, visual acuity has been the test of choice, but various forms of photoscreening have enjoyed recent favor. This paper by Dr. Traboulsi and colleagues suggests that something in between lay screening and a full professional examination may avoid many of the disadvantages of both.
A major drawback of lay screening, be it visual acuity testing or photoscreening, is the low positive predictive value (the fraction of children referred who actually have a targeted condition). This is statistically inevitable. If we generously assume, for example, a screening test that has 90% specificity and sensitivity and the conditions we are screening for have 10% prevalence, the positive predictive value is only 50%. Anecdotally, those of us who get referrals from screening programs know that in practice, the percentage of referred children who actually have pathology is not nearly this high. This has two negative effects on the screening program. First, the unnecessary referrals become the biggest cost of such a screening program, although still less than a complete examination of all children. Second, it erodes confidence in the program to the point that parents may be less likely to have their children participate or to act on the recommendation for follow-up of a failed screening.
An important goal of any screening program must therefore be to minimize the number of unnecessary referrals for subsequent examination. Traboulsi and colleagues’ use of an ophthalmic technician as a front-line screener yields a higher-quality examination than could be performed by a lay screener that essentially eliminates false positive referrals, but at a fraction of the cost of a full examination of all children by an ophthalmologist or optometrist. With an optometrist on site to perform cycloplegic retinoscopy on selected cases, even referrals for simple refractive errors—which constitute the majority of legitimate referrals from other screening programs—are eliminated.
The other important factor that limits the efficacy of a screening program is parental apathy. For example, a similar project in Baltimore had essentially no effect on visual morbidity because of poor compliance with follow-up visits and treatment.1 Traboulsi and colleagues eliminate some of these issues by integrating prescribing and dispensing of spectacles into the program instead of depending upon a follow-up visit to an ophthalmology or optometry office. But the greatest weakness of this program was the 50% rate of parental consent for participation; thus, roughly half of the target population went unscreened. However, the problem of consent is not specific to this program and may require a legislative solution, since parents apparently do not feel that vision screening is as important as politicians do.
The belief that all problems have a technological solution has led to the recent proliferation of photoscreening devices. As it turns out, superior techniques for measuring refractive errors and detecting strabismus have been available for well over a century. I applaud Traboulsi and colleagues for resisting the temptation to substitute technology for physical examination, and instead working to solve the logistical problems of delivering vision screening with proven methods.
ACKNOWLEDGMENTS
Funding/Support: None
Financial Disclosures: None.
REFERENCES
- 1.Preslan MW, Novak A. Baltimore vision screening project. Phase 2. Ophthalmol. 1998;105:150–153. doi: 10.1016/s0161-6420(98)91813-9. [DOI] [PubMed] [Google Scholar]
DR. MALCOLM R. ING
I have no financial conflicts. I believe that this is a possible solution to our problems, but like every solution, there may be more problems that arise. One of the consequences in our community, for instance, has been a large effort driven by the optometrists to insist that the state legislature mandate complete eye examinations for every child. This has become a huge problem for ophthalmologists, who are called upon by the American Academy of Ophthalmology to defend our position of screening versus full examinations, which we want to emphasize.
I would like to discuss a specific issue in your patients’ first four years of life. You mentioned you performed stereo acuity testing, so I would like to know what method of stereo acuity testing you used. For example, in my experience five year olds sometimes have trouble with stereoscopic acuity. If I use Titmus stereo acuity testing, the only way I can confirm the finding is to rotate the card 180º.
This technique was Bob Reinecke’s idea. If they can see the dot behind rather than in front of the card after you have turned it around, then you have some assurance that they have normal stereoscopic acuity. Alternatively, you can close one eye of the child and ask them to pick out one of those dots. This may also provide some assurance. I find stereo acuity testing of young children a big challenge. If you are performing these tests during the first four years, I really want to know what method you are using and what kind of controls you have employed. I have found this to be a big headache in that age group. Thank you.
DR. RICHARD A. LEWIS
Speaking from the perspective of someone whose interest is medical retina and genetics, but also speaking from the perspective of someone who is interested in medical education, and from perspective of my wife and our dealing with indigent families and populations in a city that is probably four times the size of Cleveland, my question is: do you have a sense from your data, or do you have the data analyzed to know, how many of these children have a primary physician provider? Where among the percentage of patients did you identify with pathology, particularly amblyopia and strabismus? What fraction of those should have been detected by their primary provider and was missed? Where are we missing this problem in medical education?
DR. MARILYN B. METS
The legislative solution that was referred to, specifically to engage the other 50% of children, has been passed in Illinois. I am not sure if it is a solution, but here it is. The child eye care bill that requires an examination of every child was a state bill that we tried to fight it. The bill went to the governor’s office and he vetoed it. The legislature then over rode that veto, so now every child in the state of Illinois and in the city of Chicago must have a full comprehensive eye examination in order to receive their report card, even for the first year of education in kindergarten. We suddenly are going to have an enormous number of children showing up at our doors. My question for Dr. Traboulsi is, should we buy a van? I really do not know how this is going to work. The optometrists, of course, pushed for this bill in Illinois, and maybe the pediatric ophthalmologists did, as well. I do not know. Marilyn Miller is still here in Chicago, and we should try to generate some monies to develop an intermediate kind of approach. I would like advice on a solution to this problem. Thank you.
DR. ELIAS I. TRABOULSI
I thank Dr. Archer for his kind comments. I believe that when we started this program, the goal was really just to take care of the children in the best way we could, and this is why we did not want to compromise. We knew it was going to be hard to get the money to do this program, but we did not want to have either a photoscreener or just a screening type of program. We wanted to make sure that they were cared for in the best possible way. We have learned quite a bit over the last few years. The way we now follow up on appointments and how the nurses contact the families, over and over, to get them to come, especially with the ones that we know have a serious eye problem, has changed.
Regarding Dr. Ing’s comments about how we test stereo acuity, we do use the Titmus test. My technician knows how to flip it upside down, and she does that from time to time. I honestly do not remember at this moment if not having stereo acuity is a failing part of the examination. I do not believe that it is. We rely more on visual acuity and on the presence of strabismus, rather than on just not being able to do the Titmus test. This is a point well taken. We will have more data in the future to address this question.
With respect to Dr. Lewis’ inquiry, I do not have the data on whether these children have a primary care provider or on how many would have been missed or were missed or who have had eye examinations with their pediatrician. We have not collected that data. I think we could probably do that prospectively with IRB approval.
As far as Dr. Mets’ comments about the new law in Illinois, I can tell that in other parts of the world in the developed countries, such as England, they have done away with vision screenings in the schools for the most part. They have shown that it really does not make a difference. The number of newly discovered children with previously undetected poor visual acuity or abnormalities in children who are older than six or seven years of age that you determine with vision screening is negligible. Usually children with some visual system pathology would already have been detected by their primary care physician or in some other way. This is why they stopped performing vision screening. I believe that whenever we consider implementing a new program, we must first think of where the program is going will be applied. I believe that for patients living in inner cities and in areas with poor access to health care, transportation problems, and financial problems, our program is a good model. I am biased, and this is one conflict of interest that I acknowledge: I want this program to work. I believe that the other people who work with me also want it to work, and maybe this is why it been successful so far.
I agree with Dr. Archer that we do not have use very complex or advanced technology to provide good clinical care; however, if you walked into our van, you would be very surprised. It is very nicely equipped and we have computerized vision screening machines and computers, so we use a combination of both techniques. I thank you all for your attention.
ACKNOWLEDGMENTS
Funding/Support: The Vision First program was supported by grants from the Cuyahoga County Board of County Commissioners and the Cleveland Foundation; and by charitable contributions from Ohio Savings Bank, Forest City Enterprises, The Mount Sinai Health Care Foundation, Keybank, and most currently by a 5-year grant from the Cleveland Browns Foundation. We thank Mr Richard Byers for his administration of the program and Ms J.T. Garabrant for her fundraising efforts.
Financial Disclosures: None.
Author Contributions: Design and conduct of the study (E.I.T., C.M., H.L.); Collection, management, analysis, and interpretation of data (E.I.T., C.M., R.W., H.C.); Preparation, review, and approval of the manuscript (E.I.T., C.M., R.W., H.C., H.L.).
REFERENCES
- 1.Zaba JN, Johnson RA, Reynolds WT. Vision examinations for all children entering public school—the new Kentucky law. Optometry. 2003;74:149–158. [PubMed] [Google Scholar]
- 2.Vaughn W, Maples WC, Hoenes R. The association between vision quality of life and academics as measured by the College of Optometrists in Vision Development Quality of Life questionnaire. Optometry. 2006;77:116–123. doi: 10.1016/j.optm.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Douglas G, Grimley M, McLinden M, Watson L. Reading errors made by children with low vision. Ophthalmol Physiol Optics. 2004;44:319–322. doi: 10.1111/j.1475-1313.2004.00204.x. [DOI] [PubMed] [Google Scholar]
- 4.Dzik D. Vision and the juvenile delinquent. J Behav Optom. 1996;12:66–70. [PubMed] [Google Scholar]
- 5.Helveston EM, Weber JC, Miller K. Visual function and academic performance. Am J Ophthalmol. 1985;99:346–355. doi: 10.1016/0002-9394(85)90368-x. [DOI] [PubMed] [Google Scholar]
- 6.Preslan MW, Novak A. Baltimore vision screening project. Ophthlamology. 1996;103:105–109. doi: 10.1016/s0161-6420(96)30753-7. [DOI] [PubMed] [Google Scholar]
- 7.Preslan MW, Novak A. Baltimore vision screening project. Phase 2. Ophthalmology. 1998;105:150–153. doi: 10.1016/s0161-6420(98)91813-9. [DOI] [PubMed] [Google Scholar]
- 8.Snowdon SK, Brown SL. Preschool vision screening. Health Technol Assess. 1997;1:1–98. [PubMed] [Google Scholar]
- 9.Simons K, Preslan M. Natural history of amblyopia untreated owing to lack of compliance. Br J Ophthalmol. 1999;83:582–587. doi: 10.1136/bjo.83.5.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wall TC, Marsh-Tootle W, Evans HH, Fargason CA, Ashworth CS, Hardin JM. Compliance with vision-screening guidelines among a nation sample of pediatricians. Ambul Pediatr. 2002;2:449–455. doi: 10.1367/1539-4409(2002)002<0449:cwvsga>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.Ciner EB, Dobson V, Schmidt PP, et al. A survey of vision screening policy of preschool children in the United States. Surv Ophthalmol. 1999;43:445–457. doi: 10.1016/s0039-6257(99)00021-1. [DOI] [PubMed] [Google Scholar]
- 12.Campbell LR, Charney E. Factors associated with delay in diagnosis of childhood amblyopia. Pediatrics. 1991;87:178–185. [PubMed] [Google Scholar]
- 13.Ciner EB, Schmidt PP, Orel-Bixler D, et al. Vision screening of preschool children: evaluating the past, looking towards the future. Optom Vis Sci. 1998;75:571–584. doi: 10.1097/00006324-199808000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Miller JM, Harvey EM, Dobson V. Visual acuity screening versus noncycloplegic autorefraction screening for astigmatism in Native American preschool children. J AAPOS. 1999;3:160–165. doi: 10.1016/s1091-8531(99)70062-5. [DOI] [PubMed] [Google Scholar]
- 15.Kerr NC, Arnold RW. Vision screening for children: current trends, technology and legislative issues. Curr Opin Ophthalmol. 2004;15:454–459. doi: 10.1097/01.icu.0000136112.48664.62. [DOI] [PubMed] [Google Scholar]
- 16.Logan NS, Gilmartin B. School vision screening, ages 5–16 years: the evidence base for content provision and efficacy. Ophthalmic Physiol Opt. 2004;24:481–492. doi: 10.1111/j.1475-1313.2004.00247.x. [DOI] [PubMed] [Google Scholar]
- 17.Lee DJ, Gomez-Marin O, Lam BL, Ma F, Vilar NF. Prevalence of usual-corrected distance visual acuity impairment in Hispanic and non-Hispanic children and adolescents. Paedr Perinat Epidemiol. 2000;14:357–362. doi: 10.1046/j.1365-3016.2000.00292.x. [DOI] [PubMed] [Google Scholar]
- 18.Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population based sample of 6-year-old Australian children. Ophthalmology. 2005;112:1275–1282. doi: 10.1016/j.ophtha.2005.01.052. [DOI] [PubMed] [Google Scholar]
- 19.Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121:1141–1143. doi: 10.1001/archopht.121.8.1141. [DOI] [PubMed] [Google Scholar]
- 20.Turacli ME, Aktan SG, Duruk K. Ophthalmic screening of school children in Ankara. Eur J Ophthalmol. 1995;5:181–186. doi: 10.1177/112067219500500307. [DOI] [PubMed] [Google Scholar]
- 21.Wedner SH, Ross DA, Balira R, Kaji L, Foster A. Prevalence of eye diseases in primary school children in a rural area of Tanzania. Br J Ophthalmol. 2000;84:1291–1297. doi: 10.1136/bjo.84.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsuo T, Matsuo C. Comparison of prevalence rates of strabismus and amblyopia in Japanese elementary school children between the years 2003 and 2005. Acta Med Okayama. 2007;61:329–334. doi: 10.18926/AMO/32877. [DOI] [PubMed] [Google Scholar]