In 2006, the Alabama Department of Public Health, through the University of Alabama at Birmingham's South Central Center for Public Health Preparedness, sponsored a series of infectious disease outbreak exercises in Alabama's six hospital planning regions. The six exercises were conducted in rural and metropolitan areas and were designed to be full-scale assessments of multiagency and multijurisdictional responses to an infectious disease outbreak.
This article details the lessons learned from the exercises and collaborations of academia with the public health practice and emergency response communities. We provide the results for our qualitative assessment with the hope that this information can identify trends and potential issues applicable to regions and future disasters outside of Alabama. Thus, while these exercises took place in one state, the trends we observed may be generalizable to other locales as well.
THE SIMULATED OUTBREAK
Each of the six exercises began with a simulated bus accident that prompted a call to an emergency 911 call center by either a passenger or the bus driver. The caller had a script of information to offer the emergency operator and was instructed to clearly communicate the trauma and apparent illnesses of the accident survivors.
The response phase of the simulation began when the first responding unit arrived at the exercise scene and the actors (portraying bus passengers) were in full character. Each of the actors—many of whom were graduate students of public health—was prepared with an exercise-unique script of the bus route and its destination. They were instructed on what, where, and when they recently ate, and they were given their professions and other personal information. Most often, the student actors portrayed a group of church members and friends of varying professions who were returning home from a festival or outdoor event. In addition to their scripts, the actors carried information cards noting health indicators such as blood pressure and other medical test results that could be given to prehospital and hospital care providers if requested during the exercise.
The actors were trained by the exercise clinical coordinators (a nurse, emergency room physician, and psychologist) to role-play the physical and behavioral patterns associated with influenza and traffic accident trauma. In each exercise, more than half of the 28 exercise victims portrayed signs and symptoms of influenza, while several participants simulated trauma injuries sustained in a bus accident.
The actors exhibited fear, worry about trying to get home, or the need to contact family members. Some bus passengers were extremely nervous about contracting the sickness from fellow passengers. Several actors were fluent in other languages such as Russian, Spanish, and German, which presented additional communication challenges.
The field exercise evaluation team documented and recorded all aspects of the exercise, including the initial emergency response and the establishment of incident command, triage procedures, prehospital treatment, and transport operations. One of the exercises included a chemical release and decontamination, which was monitored and documented during the exercise.
Exercise evaluators were stationed at additional venues such as receiving hospital emergency departments (EDs) and the local public health department to evaluate surge capacity issues and monitor communication between responding agencies. Additionally, evaluators assessed the adequacy of existing local emergency response plans, the inclusion of appropriate response agencies (e.g., Emergency Management Agency [EMA], public health), the utilization of a joint information system, and the establishment of a Joint Information Center to coordinate and disseminate consistent public information.1
Exercise development and team structure
The six exercises in the series were developed and evaluated by a multidisciplinary team of health academics, professionals, and emergency response experts. As part of the preparation, the development team assembled a detailed situational manual, simulated victim profiles, and victim medical charts. Agencies participating in each region included fire, law enforcement, prehospital care providers, first receivers, the local EMA, local and state public health, broadcast and print media, and public officials. Planning conferences allowed the exercise development team to understand local response customs and practices, the physical attributes of the exercise sites, and how to develop a master scenario events list that could meet objectives important to participants in each region. These efforts helped establish community commitment and allowed for joint decision-making on the exercises' logistical details. On the day before each exercise, the development team briefed key local participants on any last-minute details of the simulation without informing them of the exact nature of the emergency.
The degree of trauma resulting from the accident and portrayed by the simulated victims was customized for each exercise location. For example, at one exercise location, the simulated scenario included deaths among some passengers, while others suffered only minor physical injuries and exhibited signs and symptoms of influenza. More often, bus passengers experienced non-life-threatening injuries such as fractures and contusions along with influenza symptoms. At the request of local agencies, one exercise accident involved another multiple-passenger vehicle transporting a white, powdery substance that resulted in a chemical release at that scene. The release prompted the inclusion of hazardous materials protocols and responders.
The exercise evaluation team documented the involvement, timing, communication, and response of all participating agencies. The exercise phases considered for evaluation were (1) emergency 911 notification, (2) initial response, (3) triage, treatment, and transport, (4) hospital triage and treatment, (5) public health response, (6) sentinel laboratory, (7) media interactions, and (8) poison center collaboration. Public health was further evaluated on the effectiveness of its interface with other responding agencies and hospitals, use of public health knowledge, preliminary disease identification, and post-response epidemiologic investigation and contact tracing.
At the conclusion of each exercise, a “hot wash” (debriefing) was held for all exercise participants. At the hot wash, the project team reported on the timing and events of the exercise. Representatives from participating agencies also initiated discussions among participants regarding issues and questions that arose during the exercise.
EVALUATION METHODS
Evaluation was conducted consistent with the Homeland Security Exercise and Evaluation guidelines.2 Evaluators observed the exercises and recorded response actions and the time at which they were taken. After each exercise, the research team further discussed qualitative observations for the purpose of recognizing response trends. The research team included experienced response and evaluation experts including a fire chief, public health experts, and an emergency room physician.
RESULTS OF THE EXERCISE EVALUATION
The evaluation discussions are organized by each of the eight phases of the exercise, and pinpoint areas that were successful and those that need improvement.
911 notification phase
In all six exercises, 911 operators gathered information about the accident but failed to establish a list of passenger symptoms and communicate clues of a possible infectious disease outbreak to responding agencies, despite concern by the caller. As a result, first responders were not aware of the need for use of personal protective equipment upon arriving at the scene. The 911 operators either consistently failed to gather enough pertinent symptom information from the caller or were unable to clearly convey these symptoms to first responders.
Initial response phase
Based on our evaluation, first-responder agencies in all six exercise locations were appropriate in their speed of response, number of personnel dispatched, and initial on-scene proficiency. They established hazard zones and secured the perimeter; however, in most cases the initial accountability of passengers was incomplete.
The first arriving unit quickly and successfully established single command and prepared for unified command by contacting other agencies appropriate for the initial response. However, in some exercises there were territorial disputes among agencies and operational disparities among jurisdictions, which prevented them from achieving effective, unified command. For example, in one location, the responding fire chief refused to actively communicate with both the director of the private emergency medical services and the EMA director during the exercise. In our debriefing, it was discovered that prior individual interpersonal conflicts were at the root of these and other similar issues observed during the exercises. As a result, in this instance, there were three separate responses with little coordination—a problem that could have been resolved by a quick and cooperative unified command system.
Triage, treatment, and transport phase
Taking a census of the victims is necessary in the initial response phase and has implications for triage, treatment, and transport. Knowing how many victims are involved, the incident commander can identify and manage available resources. In several of the exercises, an initial census was not taken, and personnel and resources could not be effectively managed.
It is important that first responders gather information from victims, ask pertinent questions concerning the incident and individual medical histories, and recognize the signs and symptoms of infectious diseases. In the six exercises, several of the ill victims were employed in the poultry industry. However, first responders often did not request this information, so the possibility and consequences of avian influenza were not considered.
In most cases, the use of the Mass Casualty Incident (MCI)3 triage system was adequate, but often there were problems with the use of “all-risk” triage tickets, which categorize victims by severity of symptoms. The all-risk triage ticket is designed to clearly indicate to receiving medical personnel the nature of a victim's injury and other vital personal and health information. MCI triage systems can speed on-scene response and transport, but some of the responding agencies were unfamiliar with using all-risk triage tickets. And several agencies were unaware of new documentation requirements and procedures associated with the all-risk triage ticket. For example, if a person is not contaminated, the pink portion of the tickets that states “contaminated” should be removed during triage. In some exercises, actors were sent to receiving hospitals with the contaminated portion still attached, which prompted first receivers to needlessly decontaminate victims.
In all six exercises, it was difficult to separate the performance of the discrete functions of triage, treatment, and transport. In some instances, treatment occurred before mass triage was complete. The purpose of triage is to classify the victims by level of need; thus, triage responders should not begin treatment during triage, as there may be victims with more urgent medical needs. Additionally, a census should be taken during each of the triage, treatment, and transport functions and counts should be reconciled, which was inconsistently done during the exercises.
In several exercises, there was no clear designation of a medical communication/transportation officer to properly route the field-triaged and treated victims. This incident officer is responsible for knowing the number of victims in each category of medical need, communicating with first receivers to route victims to appropriate hospitals, and keeping records of patient destinations. The lack of designation of a medical communication/transportation officer led to confusion and prevented first receivers from knowing time-sensitive, pertinent information.
Hospital triage and treatment phase
In some instances, first receivers at participating hospitals had no previous experience with all-risk triage tickets and had considerable confusion interpreting their meaning. The issue also raised concerns about the overall lack of MCI event experiences in many rural hospitals.
First receivers discovered that their makeshift triage areas had no suitable means of receiving first-responder communication concerning arriving victims or the incident. In addition, because most of the makeshift triage areas were outside the ED, there was no system for communicating with those inside who were receiving information from the incident field.
First receivers generally used personal protective equipment when notified of the infectious hazards from the field responders. The surge nature of the event led first receivers to limit their history and physical exams, thereby missing important clues (e.g., occupational history), which would have revealed the victims' exposure to poultry and possibly guided physicians to consider a diagnosis of avian influenza.
It was evident that there were no clear procedures concerning when, if, or how first responders or hospitals should communicate with public health in an event of this nature. In some instances, hospital infection control nurses contacted the public health department immediately after receiving reports of the cluster illness in the ED. Others reported that the public health department would not be contacted until a diagnosis was confirmed, which could take days. The variability in hospital-initiated public health involvement was often dependent on the relationship between the hospitals' infection control nurses and their local public health representatives. In one exercise, an ED physician was unable to reach the local health department for advice because the public health official was in the Emergency Operation Center located in the basement of the county courthouse, and his mobile phone did not receive a signal.
Public health response phase
Communicating the signs and symptoms of an infectious disease to public health is vital for detecting type and severity, tracking exposures, and preventing the spread of illness to others. Public health's strength during the exercises was its ability to organize and activate the incident command system (ICS) within its organization. Public health also responded quickly and effectively to analyze the data being received from the hospitals. In addition, it appropriately involved the state epidemiologists so the emergency response plan could be activated. Although the bus passengers represented a sizable disease cluster, response protocols often did not include notifying public health of the event until well after the victims were discharged from the hospitals, which delayed public health's involvement in the response.
During one exercise, a Spanish-speaking victim attempted to place a call to the local health department to report the possibility of an infectious disease outbreak. The caller failed to reach a live person and was instead offered a recording that was only provided in English.
Sentinel laboratory phase
In the sentinel laboratory phase, mock specimens were delivered to the hospital sentinel laboratories. As part of our evaluation, we attempted to monitor the time it took to get these samples to the state laboratory; however, no samples were ever received. At the time of the exercises, it was found that the Centers for Disease Control and Prevention and Alabama Department of Public Health websites had contradictory instructions about how to handle samples of this nature.
Media phase
In all exercises, an incident public information officer (PIO) was identified; however, participating PIOs were not prepared to handle the arrival of journalists or answer their questions about the infectious disease outbreak. Additionally, not every PIO was familiar with the Joint Information System processes as detailed in the National Incident Management System and National Response Plan (now the National Response Framework). PIOs showed limited empathy toward the role that journalists play in disasters, even though most journalists who arrived on the scene were prepared and asked appropriate questions.
Poison control center phase
Simulated phone calls were placed to two separate specialists in poison information systems (SPISs) at a statewide poison control center. These SPISs previously received training on pandemic influenza and were provided fact sheets containing frequently asked questions. Forty calls were made to the poison control center during two one-hour sessions. Five of these calls were made in Spanish, Arabic, or French, for which the SPISs used the language line they refer to during poisoning inquiries. Questions were diverse and included specifics about antivirals, such as adverse effects and the safety of using them while pregnant or breastfeeding. All calls were appropriately answered consistent with the provided fact sheet.
LESSONS LEARNED
One lesson that transcended all of the phases was that particular attention must be given to the process, style, and message of responder communication. For example, there were often technical problems with communication at the command posts due to poor reception of radios and mobile phones. In addition, communication among responding agencies was difficult because of radio interoperability and the use of different frequencies. By establishing the ICS and using the ICS forms (e.g., ICS 205 communication plan), agencies should enhance their ability to communicate and establish designated operational frequencies.
Not all responding agencies recognized the need for unified command, which led to confusion and inefficiencies during response. Resolving this issue will require recognizing what the lack of unified command means to successful response efforts, and meeting with other agencies and jurisdictions to establish mutual aid agreements and identify unified command procedures. Agency leaders should be responsible for communicating the importance of working with partners under unified command in MCIs.
It is essential that first responders understand the three separate functions of triage, treatment, and transport and that each function be practiced sequentially in the event of a disaster. The functions allow victims of an MCI to be classified appropriately, treated according to need, and transported to first receivers who are ready and able to continue treatment. Additionally, a medical communication or transportation officer must be assigned in an MCI to prevent confusion when communicating with hospitals.
Results of our exercises suggest that first responders and first receivers need additional interdisciplinary MCI training and exercises specifically incorporating the use of all-risk triage tickets and ICSs. Such training will help to identify and resolve problems concerning communication between hospitals and first responders.
Public health's involvement in mass casualty and disease outbreak events should be initiated earlier than experienced in these exercises so that the spread of disease can be better controlled in the community. It is important that a community member who attempts to report an unusual clustering of symptoms or a potential disease outbreak is able to reach someone within the public health department. It would be advantageous for public health to make both Spanish and English options available at the beginning of automated, call-answering systems and to have an emergency number available for reaching a live person after hours.
Poison control centers can play a role in pandemic influenza preparedness by appropriately responding to inquiries made by the public. Formal training, accompanied by an algorithm that enhances their response capabilities, would be beneficial.
CONCLUSION
A significant challenge to improving preparedness and response is resolving the problems identified during exercises. Part of this challenge is disseminating the findings to all levels of the public health and response communities so that they can utilize the lessons to make improvements and procedural changes. Further, the effectiveness of local response networks can be affected by local politics, interpersonal conflicts, and jurisdictional boundaries, which can be delicate issues requiring resolution by local leaders and agency officials. Leaders can work with partner response agencies to develop mutual aid agreements and to plan and conduct exercises together. Response partnerships are important in preparedness planning and emergency response. In a pandemic influenza outbreak event, counties will likely be dependent on local response efforts; therefore, community cohesion needs to be improved for better planning and improved response efforts.
Mass casualty triage does the most good for the largest number of victims.Photo courtesy of Steve Wood, UAB Publications.
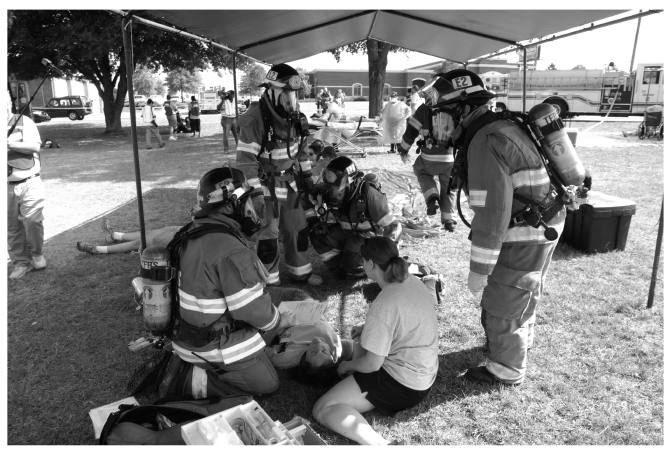
Teams gear up for tactical operations using personal protective equipment.Photo courtesy of Mike Strawn, UAB Publications.
REFERENCES
- 1.Department of Homeland Security (US). National Response Plan. December 2004. [cited 2008 Nov 11]. Available from: URL: http://www.iir.com/global/FusionCenter/NRPbaseplan.pdf.
- 2.Federal Emergency Management Agency (US). Homeland Security Exercise and Evaluation Program. [cited 2007 Jul 1]. Available from: URL: https://hseep.dhs.gov/pages/1001_HSEEP7.aspx.
- 3.Oldfield KW, Veasey DA, McCormick LC, Krayer TH, Hansen LS, Martin BN, et al., editors. Emergency responder training manual for the hazardous materials technician. Hoboken (NJ): John Wiley & Sons, Inc.; 2004. [Google Scholar]