Abstract
This review critically evaluates current knowledge of molecularly targeted therapies of malignant gliomas. Various molecularly targeted single-agent therapies, including targeted therapies of growth and survival, have been evaluated in clinical trials but have failed to demonstrate a significant survival benefit compared with standard treatment regimens. The efficacy of multi-targeted kinase inhibitors or combinations of single-targeted kinase inhibitors is a promising strategy, but requires additional clinical evaluation before definitive conclusions can be made. Important areas for further research include the assessment of serum or tissue biomarkers, the elucidation of prognostic molecular markers, and the determination of whether the mechanism of action of a drug is appropriate to the genetic alterations observed within individual tumors.
INTRODUCTION
Malignant gliomas (MGs), including glioblastomas (GBMs) and anaplastic astrocytomas (AAs), are the most common primary brain tumors (1). The prognosis for patients diagnosed with MG remains poor, with a median survival time of up to 3 years (2,3). Current conventional treatment protocols include maximally safe surgical resection followed by fractioned radiation therapy of the tumor and surrounding brain parenchyma and systemic chemotherapy with alkylating compounds. The efficacy of alkylating compounds, however, such as nitrosoureas or temozolamide, is fairly limited by the epigenetic inactivation of the DNA repair enzyme methylguanine methyltransferase (MGMT). Other DNA repair pathways, such as the DNA mismatch repair and the base excision repair pathways, have also been proposed as significant mechanisms of resistance to alkylating agents. Defects in these pathways can cause errors in DNA base pairing, which arise during DNA replication, and consequent chemoresistance to alkylating agents (4).
In this review, developments in molecularly targeted therapies for MGs are critically evaluated, and advances in the molecular and genetic pathogenesis of these lethal brain malignancies are also discussed.
MOLECULAR PATHOGENESIS OF GLIOMAS
The biological features of MGs consist of high resistance to apoptosis and florid necrosis (5). Briefly, common molecular, genetic, and epigenetic alterations in primary GBMs include amplification of the epidermal growth factor receptor (EGFR), deletion or mutation of homozygous cyclin-dependent kinase (CDK) inhibitor p16INK4A (CDKN2A), and alterations in tumor suppressor phosphatase and tensin homolog (PTEN) on chromosome 10 (6). Primary and secondary GBMs share similar characteristics, and few molecular and genetic alterations make them distinguishable from one another. For instance, human double-minute 2 (HDM2) and p53 mutations are often observed to be amplified in secondary GBMs (7).
In regard to AAs, inactivating mutations of tumor-suppressor gene TP53 and elevated expression of platelet-derived growth factor (PDGF) ligands and receptors are commonly observed in grade III AAs (8). Loss of heterozygosity in chromosome 10q has also been detected in primary high-grade AAs, and the inactivation of PTEN is observed in approximately 40% of AAs that have lost chromosome 10q (9).
Mutations in p16 are also involved, because hypermethylation in the promotor region of p16 has been detected in several cases of MGs, thus silencing p16 expression and possibly contributing to tumor genesis (10). Additionally, Bcl2-like 12 (Bcl2L12) interacts with and neutralizes caspase-7; and increased Bcl2L12 expression inhibits apoptosis (11). The astrocyte elevated gene-1 (AEG-1) has also been implicated in the pathogenetic hallmark of MGs (12). AEG-1 is overexpressed in the majority of human MG samples, and cooperates with the Haras family of retrovirus-associated DNA sequences (RAS) to promote cellular transformation and subsequently to augment invasion and growth of transformed cells (8,9). Furthermore, oncogenic Haras induces AEG-1 expression by modulating the phosphatidylinositol 3-kinase (PI3K)-Akt signaling pathway, thus contributing to the growth of MGs (13).
MOLECULARLY TARGETED THERAPY
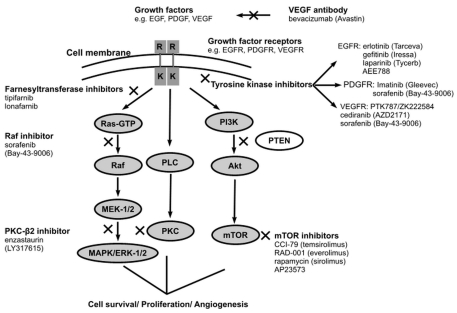
Elevated expression or mutation of receptors and intracellular downstream effectors has been observed in MGs (14). These pathways are regulated by several growth factors linked to tyrosine kinase, such as the EGFR, insulin-like growth factor receptor (IGFR), PDGF receptor (PDGFR), and vascular EGF receptor (VEGFR). Specific targeting of these signaling pathways that lead to uncontrolled cellular proliferation and cell migration and invasion could provide new molecularly targeted treatment options for MGs. The growth factor signaling pathways and their inhibition in MGs are shown in Figure 1 (14), and Table 1 summarizes the major clinical trials of molecularly targeted therapies in MGs.
Figure 1.
The growth factor signaling pathways and their inhibition in malignant gliomas (MGs). Growth-factor binding stimulates receptor tyrosine kinase activity, leading to the activation of multiple downstream signaling cascades. These signaling pathways regulate processes such as cell survival, proliferation, and angiogenesis. Moreover, various intra-and extracellular proteins of these signaling pathways are also potential therapeutic targets for the treatment of malignant gliomas. X indicates the site of inhibition of targeted molecular agents; R, receptor; K, kinase; EGFR, epidermal growth factor receptor; EGF, epidermal growth factor; PDGFR, platelet-derived growth factor receptor; PDGF, platelet-derived growth factor; mTOR, mammalian target of rapamycin; PTEN, tumor-suppressor phosphatase and tensin homolog; PKC, protein kinase C; PI3K, phosphatidylinositol-3-kinase; PLC, phospholipase C; Akt, protein kinase B; MEK-1/2, mitogen-activated protein kinase and extracellular signal-regulated protein kinase-1/2 kinase; MAPK/ERK-1/2, mitogen-activated protein kinase/extracellular signal-regulated protein kinase-1/2.
Table 1.
Major clinical trials (completed and/or are ongoing) and their main efficacy results with each drug category.a
| Target | Agent (phase of trial) | Results | Reference |
|---|---|---|---|
| EGFR | Gefitinib (II) | Rec GBM; PFS-6: 13–14.3%, mOS: 24.6–39.4 weeks | 16,17 |
| Erlotinib + TMZ (I) | Rec GBM; mOS: 55 weeks | 19,20 | |
| Cetuximab (II) | Ongoing | — | |
| PDGFR | Imatinib ± hydr/rea (II) | Rec GBM; PFS-6: 3%, mPFS: 14.4 weeks, mOS: 48.9 weeks. Rec AAs; PFS-6: 10% | 25,26 |
| VEGFR | Bevacizumab + IRI (II) | Rec GBM; RR: 63%, PFS-6: 38%–46%, PR: 57% | 29,30 |
| Vatalanib (I/II) | Rec GBM; PR: 4%, stable disease: 56% | 32 | |
| MTOR | Temsirolimus (II) | Rec GBM; PFS-6: 7.8%, mOS: 44 months | 37 |
| Tems. + erlotinib (I/II) | Ongoing | — | |
| RAS | Tipifarnib (II) | Rec GBM; PFS-6: 33% | 40 |
| Tipifarnib + TMZ (I) | Rec GBM; PFS-6: 12% | 41 | |
| PKC-b | Enzastaurin vs lomustine (III) | Terminated because of equal efficacy results | 45 |
| RAF | Sorafenib (I/II) | Ongoing | — |
| EGFR/HER-2 | Lapatinib (II) | Ongoing | — |
| HER-1/EGFR | 125I-MAb 425 (I/II) | Rec GBM/AAs; OS range: 4–150/4–270 months | 47 |
| Tenascin-C | 131I-81C6 (II) | Rec GBM; mOS: 78 weeks | 49 |
| Integrins | Cilengitide (I/II) | Rec MGs; CR: 4%, PR: 6%, stable disease: 8% | 55 |
| Cilengitide + RT (II) | Ongoing | — |
EGFR, epidermal growth factor receptor; PDGFR, platelet-derived growth factor receptor; VEGFR, vascular endothelial growth factor receptor; mTOR, mammalian target of rapamycin; HER, human epidermal growth factor receptor; TMZ, temozolamide; hydr/rea, hydroxyurea; IRI, irinotecan; Tems, temsirolimus; RT, radiation; Rec, recurrent; GBM, glioblastoma multiforme; AAs, anaplastic astrocytomas; MGs, malignant gliomas; PFS-6, 6-month progression-free survival; mPFS, median progression-free survival; mOS, median overall survival; RR, response rate; PR, partial response; C, complete response.
EGFRs
The EGFR belongs to the ErbB family of tyrosine kinase receptors. The presence of EGFRvIII, a specific variant of the EGFR lacking exons 2 to 7, is an independent predictor of poor survival in patients with primary MGs (15). Treatment options that target EGFRs include gefitinib (ZD-1839) and erlotinib (OSI-774). However, efficacy of these agents is modest.
Gefitinib was evaluated in an open-label, single-center phase II clinical trial in patients (n = 57) with the first recurrence of a GBM (16). Each patient initially received 500 mg of gefitinib (orally, once a day), and the dose was escalated up to 1000 mg in patients receiving enzyme-inducing antiepileptic drugs or dexamethasone. Quantification of gefitinib antiglioma efficacy was assessed by 6-month progression-free survival (PFS-6) and brain magnetic resonance imaging (MRI) quantification of tumor response (radiographic response). The study population had a PFS-6 of 13% (7 of 53 patients) and a median overall survival (OS) time from treatment initiation of 39.4 weeks, but no radiographic response was observed (16). In a multi-center, open-label, single-arm phase II clinical trial of gefitinib in patients (n = 28) with recurrent MG after surgery plus radiotherapy and first-line chemotherapy, overall median time to progression (TTP)was 8.4 weeks, PFS-6 was 14.3%, and median OS was 24.6 weeks (17). None of the patients presented objective radiographic response (17), and it was concluded that gefitinib demonstrated limited efficacy against GBM compared with the standard Stupp regimen (radiotherapy plus temozolamide; median PFS 6.9 months; PFS-6 53.9%, and median OS 58 weeks) (18).
In several phase I/II clinical trials, OS rates for erlotinib and gefitinib treatment were similar, but erlotinib was more effective than gefitinib treatment in terms of objective radiographic responses (19,20). A multicenter, open-label phase I clinical trial evaluated the efficacy of erlotinib plus radiation therapy in patients (n = 19) with GBM. With a median follow-up of 52 weeks, progression was assessed in 16 patients and 13 deaths occurred. Median TTP was 26 weeks and median OS was 55 weeks (19). Additionally, in an open-label phase I dose-escalation clinical trial, patients (n = 83) with stable or progressive malignant primary gliomas received erlotinib alone or combined with temozolomide (20). Of the patients assessed (n = 57), eight patients demonstrated a PR and six patients demonstrated a median PFS of greater than 6 months, which included four patients with a PR (20). Erlotinib treatment was equally as effective as the standard Stupp regimen (median OS 58 weeks; median PFS 6.9 months; 7 [11.3%] CRs and 17 [27.4%] PRs) (18). The favorable tolerability profile and evidence of antitumor activity suggest that additional evaluation of erlotinib treatment is warranted. However, it should also be noted that responders to drugs targeting EGFR usually have intact PTEN and EGFRvIII and no phospho-Akt (21,22).
In an in vitro study, administration of cetuximab, a human-murine chimeric anti-EGFR mAb, increased apoptosis in EGFR-amplified GBM cells (23). Cetuximab treatment alone or in combination with radiation therapy or chemotherapy was also assessed in vivo in female athymic nude mice 4 to 6 weeks old (23). Treated mice received cetuximab (0.5 mg, intraperitoneal injection twice weekly) for 5 wk, and the control group received an IgG-1 isotype-matched antibody (0.5 mg, intraperitoneal injection twice weekly) for the same period. Treatment with cetuximab significantly increased median OS compared with the control treatment, with median survival for cetuximab-treated mice (65 days) increased by more than 200% compared with IgG-treated mice (24 days) (23).
PDGFR
PDGFRs regulate angiogenesis and are overexpressed in approximately 75% of MGs (24). Administration of imatinib (STI-571), a PDGFR inhibitor, either as monotherapy or in combination with hydroxyurea or radiotherapy, has been associated with modest activity in open-label, phase II clinical trials in patients with MG (25,26).
An open-label phase II trial of imatinib monotherapy (400 mg, once a day) in patients (n = 55) with anaplastic glioma or GBM demonstrated minimal efficacy (25). Radiographic response was <6% for both types of brain tumors; in patients with GBM (n = 34) two patients (6%) demonstrated partial responses (PRs) and six patients (18%) demonstrated stable disease, but there were no complete responses (CRs) (25). One patient with GBM was removed from the study because of toxicity. Among the patients (n = 21) with anaplastic glioma, there were no CRs or PRs, and five patients had stable disease (25). The PFS-6 was 10% (2 of 21) in patients with anaplastic glioma, and PFS-6 was just 3% (1 of 33) in patients with GBM (25). In an open-label, single-arm phase II clinical trial, patients with recurrent GBM (n = 33) received imatinib mesylate (500 mg, twice a day) plus hydroxyurea (orally) on a continuous daily schedule (26). At a median follow-up of 58 weeks, 27% of patients (9 of 33) were progression free at 6 months, with a median PFS of 14.4 weeks (26). Radiographic responses were observed in 3 patients (9%), 14 (42%) achieved stable disease, and the median OS rates were 48.9 weeks (26). In all cases, the responses observed in these clinical trials in patients with recurrent GBM were inferior to those observed with the standard Stupp regimen (PFS-6, 53.9%; median, PFS 6.9 months; overall response rate 38.7%, including 7 [11.3%] CRs and 17 [27.4%] PRs) (18,27).
VEGFR
VEGFRs are overexpressed in MGs (14); therefore, inhibiting their function may block angiogenesis and limit peritumoral edema. A phase II clinical trial in patients (n = 16) with recurrent GBM used a series of MRI protocols to assess the efficacy of cediranib (AZD-2171; AstraZeneca, Wilmington, DE, USA), a rapid-onset, reversible, orally administered VEGFR tyrosine kinase inhibitor, as indicated by relative vessel size and permeability, tumor contrast enhancement, and edema-associated parameters (28). Relative cerebral blood volume of larger vessels (gradient echo images) and smaller vessels (spin echo images), as well as cerebral blood flow, were calculated by use of a standard deconvolution technique. Permeability was measured by using dynamic contrast-enhanced MRI techniques. In addition, correlations between temporal changes in these parameters and molecular markers in blood (angiogenic cytokines) and cellular bio-markers of vascular response were assessed. Cediranib treatment normalized tumor blood vessels in patients with recurrent GBM and alleviated edema (28). Moreover, relative tumor vessel size significantly decreased as early as 1 day after the onset of AZD-2171 treatment (P < 0.05), and remained decreased at day 28. At day 56, the relative vessel size reversed (day 56 versus day 28; P < 0.05) toward abnormal values (28).
An open-label phase II trial in patients (n = 23) with MG assessed the efficacy of bevacizumab (10 mg/kg administered every 21 days), a humanized mAb antibody against VEGF, and irinotecan (CPT-11) (29). Patients administered enzyme-inducing antiepileptic drugs (EIAEDs) received a 340-mg/m2 dose of irinotecan, whereas patients not taking EIAEDs received 125 mg/m2. A response rate of 63%, a median PFS time of 23 weeks and a PFS-6 of 38%, were observed (29). The synergistic beneficial effect was confirmed by the same researchers in a second phase II clinical trial in patients with recurrent GBM (n = 35). Two cohorts of patients were included. The initial cohort of patients (n = 23) received bevacizumab (10 mg/kg) plus irinotecan every 2 wk. After this regimen was deemed safe and effective, the irinotecan schedule was changed to a regimen of 4 doses in 6 weeks. The second cohort of patients (n = 12) received bevacizumab (15 mg/kg) every 21 days and irinotecan on days 1, 8, 22, and 29. Each cycle was 6 wk long. Patients in the second cohort (n = 35) demonstrated a PFS-6 of 46% and a 6-month OS of 77%, and PRs were observed in 57% of patients (30). Overall, regimens consisting of bevacizumab plus irinotecan demonstrated similar survival and progression rates compared with the standard Stupp regimen (18). Of note, however, is that trials assessing the efficacy of bevacizumab plus irinotecan (29,30) enrolled a relatively small number of patients and therefore were not powered adequately to provide more significant results.
Vatalanib (PTK-787; ZK-222584; Novartis AG, Basel, Switzerland), an oral controlled-release PDGF/VEGF-receptor tyrosine kinase angiogenesis inhibitor, was assessed in preclinical models for efficacy against VEGF-dependent glioma vascularization and growth. Vatalanib significantly limited VEGF-mediated glioma growth, thereby providing a promising new treatment option for MGs (31). Vatalanib was evaluated in patients with recurrent MGs in a open-label, non-randomized phase I/II clinical trial as a monotherapy (32) as well as in a similarly designed phase I/II clinical trial with temozolamide or lomustine (33). Preliminary results showed that vatalanib monotherapy (1200 or 1500 mg/d; n = 47) led to 2 patients (4%) with PRs, 31 patients (56%) with stable disease, and 14 patients (25%) with disease progression (32), compared with the standard Stupp regimen (OR rate of 38.7%, including 11.3% CRs and 27.4% PRs) (18,26). However, final results from these trials are awaited to potentially support the significance of using vatalanib in patients with recurrent MSs, because disappointing efficacy data were obtained in other clinical trials in patients with primary and recurrent MGs (5,14,34).
Mammalian Target of Rapamycin Signaling
Mammalian target of rapamycin (mTOR) is a critical downstream kinase in the PI3K/Akt/mTOR pathway (35). Combination therapy of AEE-788 (Novartis AG), an EGFR/VEGFR-2 inhibitor, and everolimus (RAD-001), an inhibitor of mTOR, inhibited the tumor growth of GBM in an in vitro study (36). The combination of AEE-788 and RAD-001 increased rates of cell-cycle arrest and apoptosis and reduced proliferation more than either agent alone (36). In a single-arm, open-label phase II clinical trial in patients (n = 65) with GBM, temsirolimus (CCI-779; 250 mg intravenously once a week) demonstrated modest efficacy, with 20 patients (36%) demonstrating radiographic improvement (37). Observed radiographic indications of improvement consisted of significant decreases in T2 signal abnormality (tumor volume) and/or improvement in gadolinium (contrast medium) enhancement in patients receiving stable or decreased steroid doses. The PFS-6 was 7.8% and the median OS was 4.4 months (37). Similarly, in another open-label, nonrandomized phase II clinical trial to determine the efficacy of temsirolimus in patients (n = 43) with recurrent GBM, 1 patient remained progression free at 6 months, and of the patients (n = 41) assessable for response, 2 PRs were observed and 20 patients had stable disease (38). In addition, the median time to progression was 9 weeks (38); therefore, compared with the standard Stupp regimen (PFS-6 53.9, median OS 58 weeks, median PFS 6.9 months; OR rate of 38.7%) (18,26), there was no evidence of an improved response to temsirolimus treatment in patients with recurrent GBM (38). Overall, temsirolimus treatment appears to be less effective than the standard Stupp regimen.
RAS
MGs often show increased RAS activity (cell growth and differentiation) because of mutation or amplification of upstream growth factor receptors (39). Farnesyltransferases are part of the RAS signal transduction pathway, and farnesyltransferase inhibitors, including tipifarnib (R-115777; Johnson and Johnson Pharmaceutical Research and Development, Brunswick, NJ, USA), and lonafarnib (Sch-66336), have been assessed and shown to have modest survival benefits in phase I and II clinical trials in patients with recurrent MGs (40,41). For example, in an open-label, nonrandomized, phase II clinical trial to determine the efficacy and safety of tipifarnib in patients (n = 67) with recurrent GBM, eight patients (11.9%) had a PFS of >6 months (40). In addition, a PFS-6 of 33% was observed in a nonrandomized phase I clinical trial of temozolamide and lonafarnib in patients (n = 15) with recurrent GBM (41). However, PFS rates following administration of tipifarnib or temozolamide plus lonafarnib were inferior to those observed after administration of the standard Stupp regimen (18).
Protein Kinase C
Enzastaurin (LY-317615; Eli Lilly, Indianapolis, IN, USA), a selective inhibitor of activated protein kinase C (PKC)β suppressed tumor cell proliferation (42). In addition, enzastaurin treatment suppressed the phosphorylation of glycogen synthase kinase 3β (GSK3β), a serine/threonine PK, in GBM xenograft tumor tissues. Enzastaurin also limited the growth of human GBM xenografts (43). These effects are supported by data from a preclinical study that investigated the effects of enzastaurin and radiotherapy in vitro, and in vivo compared with either treatment alone (44). This study demonstrated that combining cerebral irradiation with enzastaurin decreased the following parameters: tumor volume, irradiation-induced tumor satellite formation, upregulation of VEGF expression in vitro and in vivo, and enhanced microvessel density in vivo (44). However, in an open-label, multicenter phase III clinical trial that compared enzastaurin with lomustine treatment in patients (n = 266) with recurrent GBM, treatment effects were modest (45). Median PFS, OS, and PFS-6 rates were not significantly different between treatment arms, and therefore enzastaurin was not superior to lomustine in patients with recurrent GBM (45).
Ligand–Toxin Conjugates
The Her1/EGFR-expressing tumors are specifically targeted by radioisotopes or toxic compounds conjugated to Her1/EGFR-specific antibodies or ligands, including 125iodine (I)-MAb 425, TP-38, and DAB389-EGF (46). Regional administration of radiolabeled mAbs targeting tumor-specific antigens expressed by MGs has demonstrated encouraging antitumor activity and acceptable toxicity in clinical trials (34).
The 125I-MAb 425, an IgG2a antibody that binds to a protein determinant on the external domain of human EGFRs, is internalized upon binding to EGFRs and downregulates EGFR expression without stimulating receptor tyrosine kinase activity (47). In an open-label, nonrandomized phase I/II clinical trial, adjuvant administration of 125I-MAb 425 (50 μCi, intravenous, once a week) in patients (n = 180) with MGs significantly increased median survival compared with controls receiving radiotherapy alone (47). The actuarial OS range for GBM and AA patients was 4 to 150 and 4 to 270 months, respectively (47). A similar study investigated the putative benefits of teleradiotherapy and 125I-MAb 425 radioimmunotherapy administered after neurosurgery in high-grade gliomas compared with teleradiotherapy alone (48). A median OS of 14 months for both treatment groups was observed, with no improvement in disease-free survival or OS in either treatment group after neurosurgery (48). Therefore, radiotherapy and radioimmunotherapy with anti-EGFR 125I-MAb 425 was not beneficial compared with radiotherapy alone for the adjuvant treatment of high-grade gliomas following neurosurgery (48). Therefore, compared with the standard Stupp regimen (OS range for GBM was 13.2 to 16.8 months) (18), 125I-MAb 425 greatly increased the OS range. In addition, mAb-806 (Life Science Pharmaceuticals) and 3C10 mAb are mAbs directed against EGFR-vIII with conjugated toxins or radioisotopes and may represent other targeted treatment options for MGs (34).
The administration of the mAb against tenascin-C, an extracellular matrix glycoprotein ubiquitously expressed by malignant gliomas, has also been evaluated in clinical trials (49,50). In a nonrandomized, phase II, dose-response clinical trial in patients (n = 33) with primary MGs, 131I-81C6 (Bradmer Pharmaceuticals, Toronto, Canada), a radiolabeled mAb-targeting tenascin (an extracellular matrix protein present in MGs, but not in normal brain tissue), was injected directly into surgically created resection cavities followed by conventional external-beam radiotherapy and chemotherapy (49). This treatment strategy demonstrated a median survival of 86 weeks for patients with either anaplastic astrocytomas (n = 4) or AAs (n = 2). In patients with GBM (n = 27) a median OS of 79 weeks was observed (49). Therefore, 131I-81C6 increased the median survival of GBM patients compared with the standard Stubb regimen (49). Furthermore, histopathological analyses were conducted in patients (n = 28) treated with combined external-beam radiotherapy and a brachytherapy consisting of 131I-81C6 injected into surgically created resection cavities during brain tumor resections (50). Histological tissue classification outcomes included “proliferative glioma,” “quiescent glioma,” and “negative for neoplasm”. Median survival with tissue classified as proliferative glioma, quiescent glioma, and negative for neoplasm were 3.5, 15, and 27.5 months, respectively (50). Median survival in patients receiving a total radiation dose greater than 86 Gy)was 19 months, compared with 7 months for those receiving less than 86 Gy, thus suggesting that the total dose of radiotherapy was a significant predictor of survival (P < 0.002) (50). Therefore, additional clinical trials are warranted to determine the effectiveness of 131I-81C6 for the treatment of MGs.
TP-38 is a recombinant chimeric protein composed of transforming growth factor α combined with a mutated form of Pseudomonas exotoxin (51). Binding specificity of TP-38 for cells in the brain was demonstrated by the ability of non-radiolabeled TP-38 to block the binding of 125I-EGF to EGFR-expressing non–small cell lung cancer cell lines (51). TP-38 has also demonstrated toxicity to human glioma cell lines (51). However, in a pilot phase I clinical trial, TP-38 was associated with an inferior clinical response (52), compared with the Stupp regimen (18). Efficacy results of this pilot study (52) showed that after TP-38 administration, the median OS of patients (n = 20) with recurrent malignant brain tumors was 23 weeks. Median OS for patients with residual disease at the time of TP-38 therapy was 18.7 wk, whereas for those without radiographic evidence of residual disease median survival was 32.9 weeks. Overall, 2 of 15 patients (14%) with residual disease at the time of therapy demonstrated radiographic responses. One patient (7%) had CR and another (7%) had a PR with >50% tumor shrinkage 34 weeks after TP-38 therapy (52).
However, interpretation of data from trials, such as those described above, is challenging because of methodological problems, mainly consisting of the small sample sizes enrolled and the open-label study design (48–50,52).
Integrins
Integrins are cell surface receptors that play important roles in tumor invasion (53). Cilengitide has demonstrated some efficacy against MGs in both a preclinical study (54) and in a nonrandomized phase I clinical trial of cilengitide (2400 mg/m2) for treating 51 patients with MGs, including 37 with GBMs (55). Among the evaluable patients, 2 patients (4%) demonstrated CRs, 3 patients demonstrated PRs (6%), and 4 (8%) demonstrated stable disease. Considering these preliminary results, cilengitide appears to be a promising treatment agent against MGs, and therefore the final results of this study are awaited before definite conclusions can be drawn. To our knowledge, a larger randomized phase II trial of cilengitide is currently ongoing in patients with newly diagnosed GBMs concurrent with radiation therapy.
Histone Deacetylase Inhibitors
Epigenetic changes to the genome through DNA methylation and covalent modification of the histones that form the nucleosome are key to maintenance of the differentiated state of the cell. Thus, inhibition of deacetylation, which is controlled by histone deacetylases, may lead to chromatin remodeling, up-regulation of key tumor repressor genes, differentiation, or apoptosis. Histone deacetylase inhibitors, by altering functional epigenetic modifications, are additional potential anticancer agents for the treatment of MGs.
Structurally diverse histone deacetylase inhibitors, including vorinostat and romidepsin (FK-228; Gloucester Pharmaceuticals, Cambridge, MA, USA) have demonstrated their ability to inhibit proliferation and induce differentiation and/or apoptosis of tumor cells in culture and in animal models (56), suggesting that treatment with vorinostat may enhance radiation-induced cytotoxicity in MGs (57).
MONITORING RESPONSE TO MOLECULARLY TARGETED THERAPIES
A critical issue that remains to be fully explored is the identification of the optimal method to evaluate the response and biologic activity of molecularly targeted therapies in gliomas (58). Because antiangiogenic therapy is acknowledged to be the most promising treatment approach against MGs, research has been focused in the development of objective methods to evaluate its efficacy.
Pharmacodynamic Surrogate Markers
Measurements of serum levels of VEGF and other angiogenic cytokines have been considered to provide useful information toward the monitoring of response of molecularly targeted therapies in solid tumors (58). This method is not applied in MGs, however, because the levels of VEGF are not increased in patients with MGs (59). Levels of VEGF and basic FGF in cerebrospinal fluid have been associated with brain tumor vascularity and patient survival (60). Therefore measurement of VEGF and basic FGF in cerebrospinal fluid may be a suitable method to clinically monitor the response to antiangiogenic therapy. In addition, the levels of circulating endothelial progenitor cells (CEPs) in the peripheral blood correlate with anti-angiogenic drug activity (61), and therefore CEPs have been measured to clinically monitor response to antiangiogenic therapy (58). Results were conflicting, however, and therefore the significance of CEPs as pharmacodynamic markers to monitor antiangiogenic drug activity in MGs remains to be conclusively demonstrated.
Radiological Functional Techniques
Apart from the standard MRI imaging techniques, novel molecular imaging techniques—such as arterial spin labeling, perfusion MRI (62), 1H-magnetic resonance spectroscopy (63), and blood oxygenation level–dependent imaging (64)—have recently been shown to provide quantitative measurements of brain tumor perfusion. Single-photon emission computed tomography and positron emission tomography imaging have been recently applied in the clinical setting and may be sensitive quantitative techniques to objectively assess the efficacy of antiangiogenic therapy in MGs, providing some useful information (65). Recently, coupling of antibodies against αvβ3-integrin and the intercellular adhesion molecule-1, and the E-selectin adhesion molecule with paramagnetic liposomes or nanoparticles have been applied and assessed in experimental animal models to molecularly image angiogenesis (66,67). Overall, the significance of the above-mentioned techniques is mainly degraded by the preliminary or experimental results and the limited availability in the general setting. In any case, this issue of great importance warrants further study.
CONCLUSIONS
Various single-agent therapies, such as gefitinib and imatinib, that target growth and survival pathways have failed to demonstrate a significant survival benefit. Therefore, more effective therapies may be those that target multiple signaling pathways simultaneously by multi-targeted kinase inhibitors or combinations of kinase inhibitors that target single kinases. Additional clinical trials are required to elucidate whether multi-targeting strategies will improve survival rates in patients with MGs.
Pharmacokinetic evaluation of drugs is important to assess therapeutic drug levels and identify potential drug interactions. Important areas for additional pharmacodynamic research include the assessment of serum or tissue biomarkers, the elucidation of prognostic molecular markers, and the use of biomarkers to determine if the mechanism of drug action is appropriate to genetic alterations within individual tumors. Moreover, biological endpoints, such as measures of target inhibition, should be included in the design of clinical trials that evaluate standard or novel targeted therapies against MGs.
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
We declare that the authors have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper. No funding source had a role in the preparation of this paper or in the decision to submit it for publication.
REFERENCES
- 1.Central Brain Tumor Registry of the United States (CBTRUS) Statistical report: primary brain tumors in the United States, 1998–2002. Chicago: CBTRUS; 2006. (Available from: http://www.cbtrus.org/reports//2004-2005/2005report.pdf) [Google Scholar]
- 2.Kleihues P, Cavenee WK. Pathology and genetics: Tumours of the nervous system. 2nd edition. Albany: WHO Publications Centre, USA; 2000. World Health Organization classification of tumors; p. 314. [Google Scholar]
- 3.Stupp R, Reni M, Gatta G, Mazza E, Vecht C. Anaplastic astrocytoma in adults. Crit Rev Oncol Hematol. 2007;63:72–80. doi: 10.1016/j.critrevonc.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Sarkaria JN, et al. Mechanisms of chemoresistance to alkylating agents in malignant glioma. Clin Cancer Res. 2008;14:2900–8. doi: 10.1158/1078-0432.CCR-07-1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Omuro AM, Faivre S, Raymond E. Lessons learned in the development of targeted therapy for malignant gliomas. Mol Cancer Ther. 2007;6:1909–19. doi: 10.1158/1535-7163.MCT-07-0047. [DOI] [PubMed] [Google Scholar]
- 6.Ohgaki H. Genetic pathways to glioblastomas. Neuropathology. 2005;25:1–7. doi: 10.1111/j.1440-1789.2004.00600.x. [DOI] [PubMed] [Google Scholar]
- 7.Houillier C, et al. Prognostic impact of molecular markers in a series of 220 primary glioblastomas. Cancer. 2006;106:2218–23. doi: 10.1002/cncr.21819. [DOI] [PubMed] [Google Scholar]
- 8.Merlo A. Genes and pathways driving glioblastomas in humans and murine disease models. Neurosurg Rev. 2003;26:145–58. doi: 10.1007/s10143-003-0267-8. [DOI] [PubMed] [Google Scholar]
- 9.Ohgaki H, Kleihues P. Genetic pathways to primary and secondary glioblastoma. Am J Pathol. 2007;170:1445–53. doi: 10.2353/ajpath.2007.070011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolter M, et al. Oligodendroglial tumors frequently demonstrate hypermethylation of the CDKN2A (MTS1, p16INK4a), p14ARF, and CDKN2B (MTS2, p15INK4b) tumor suppressor genes. J Neuropathol Exp Neurol. 2001;60:1170–80. doi: 10.1093/jnen/60.12.1170. [DOI] [PubMed] [Google Scholar]
- 11.Stegh AH, et al. Bcl2L12 inhibits post-mitochondrial apoptosis signaling in glioblastoma. Genes Dev. 2007;21:98–111. doi: 10.1101/gad.1480007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emdad L, et al. Astrocyte elevated gene-1: Recent insights into a novel gene involved in tumor progression, metastasis and neurodegeneration. Pharmacol Ther. 2007;114:155–70. doi: 10.1016/j.pharmthera.2007.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang DC, et al. Cloning and characterization of HIV-1-inducible astrocyte elevated gene-1, AEG-1. Gene. 2005;353:8–15. doi: 10.1016/j.gene.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Reardon DA, Wen PY. Therapeutic advances in the treatment of glioblastoma: rationale and potential role of targeted agents. Oncologist. 2006;11:152–64. doi: 10.1634/theoncologist.11-2-152. [DOI] [PubMed] [Google Scholar]
- 15.Pelloski CE, et al. Epidermal growth factor receptor variant III status defines clinically distinct subtypes of glioblastoma. J Clin Oncol. 2007;25:2288–94. doi: 10.1200/JCO.2006.08.0705. [DOI] [PubMed] [Google Scholar]
- 16.Rich JN, et al. Phase II trial of gefitinib in recurrent glioblastoma. J Clin Oncol. 2004;22:133–42. doi: 10.1200/JCO.2004.08.110. [DOI] [PubMed] [Google Scholar]
- 17.Franceschi E, et al. Gefitinib in patients with progressive high-grade gliomas: A multi-centre phase II study by Gruppo Italiano Cooperativo di Neuro-Oncologia (GICNO) Br J Cancer. 2007;96:1047–51. doi: 10.1038/sj.bjc.6603669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stupp R, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 19.Krishnan S, et al. Phase I trial of erlotinib with radiation therapy in patients with glioblastoma multiforme: Results of North Central Cancer Treatment Group protocol N0177. Int J Rad Oncol Biol Phys. 2006;65:1192–9. doi: 10.1016/j.ijrobp.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 20.Prados MD, et al. Phase 1 study of erlotinib HCl alone and combined with temozolomide in patients with stable or recurrent malignant glioma. Neuro Oncol. 2006;8:67–78. doi: 10.1215/S1522851705000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mellinghoff IK, et al. Molecular determinants of the response of glioblastomas to EGFR kinase inhibitors. N Engl J Med. 2005;353:2012–24. doi: 10.1056/NEJMoa051918. [DOI] [PubMed] [Google Scholar]
- 22.Haas-Kogan DA, et al. Epidermal growth factor receptor, protein kinase B/Akt, and glioma response to erlotinib. J Natl Cancer Inst. 2005;97:880–7. doi: 10.1093/jnci/dji161. [DOI] [PubMed] [Google Scholar]
- 23.Eller JL, et al. Anti-epidermal growth factor receptor monoclonal antibody cetuximab augments radiation effects in glioblastoma multiforme in vitro and in vivo. Neurosurgery. 2005;56:155–62. doi: 10.1227/01.neu.0000145865.25689.55. [DOI] [PubMed] [Google Scholar]
- 24.Ranza E, Facoetti A, Morbini P, Benericetti E, Nano R. Exogenous platelet-derived growth factor (PDGF) induces human astrocytoma cell line proliferation. Anticancer Res. 2007;27:2161–6. [PubMed] [Google Scholar]
- 25.Wen PY, et al. Phase I/II study of imatinib mesylate for recurrent malignant gliomas: North American Brain Tumor Consortium Study 99–08. Clin Cancer Res. 2006;12:4899–907. doi: 10.1158/1078-0432.CCR-06-0773. [DOI] [PubMed] [Google Scholar]
- 26.Reardon DA, et al. Phase II study of imatinib mesylate plus hydroxyurea in adults with recurrent glioblastoma multiforme. J Clin Oncol. 2005;23:9359–68. doi: 10.1200/JCO.2005.03.2185. [DOI] [PubMed] [Google Scholar]
- 27.Yaman E, et al. Temozolomide in newly diagnosed malignant gliomas: administered concomitantly with radiotherapy, and thereafter as consolidation treatment. Onkologie. 2008;31:309–13. doi: 10.1159/000127252. [DOI] [PubMed] [Google Scholar]
- 28.Batchelor TT, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11:83–95. doi: 10.1016/j.ccr.2006.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vredenburgh JJ, et al. Phase II trial of bevacizumab and irinotecan in recurrent malignant glioma. Clin Cancer Res. 2007;13:1253–9. doi: 10.1158/1078-0432.CCR-06-2309. [DOI] [PubMed] [Google Scholar]
- 30.Vredenburgh JJ, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25:4722–9. doi: 10.1200/JCO.2007.12.2440. [DOI] [PubMed] [Google Scholar]
- 31.Goldbrunner RH, et al. PTK787/ZK222584, an inhibitor of vascular endothelial growth factor receptor tyrosine kinases, decreases glioma growth and vascularization. Neurosurgery. 2004;55:426–32. doi: 10.1227/01.neu.0000129551.64651.74. [DOI] [PubMed] [Google Scholar]
- 32.Conrad C, et al. A phase I/II trial of single-agent PTK787/ZK222584, a novel oral angiogenesis inhibitor, in patients with recurrent GBM. Proc. Am. Soc. Clin. Oncol. 2004 Abstract 1512. [Google Scholar]
- 33.Reardon D, Friedman H, Yung WKA. A phase I/II trial of PTK787/ZK222584 (PTK/ZK), a novel oral angiogenesis inhibitor, in combination with either temozolomide or lomustine for patients with recurrent glioblastoma multiforme (GBM) Proc Am Soc Clin Oncol. 2004;23:110. [Google Scholar]
- 34.Argyriou AA, Antonacopoulou A, Iconomou G, Kalofonos HP. Treatment options for malignant gliomas, emphasizing towards new molecularly targeted therapies. Crit. Rev. Oncol. Hematol. 2008 Jul 3; doi: 10.1016/j.critrevonc.2008.05.005. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 35.Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes Dev. 2004;18:1926–45. doi: 10.1101/gad.1212704. [DOI] [PubMed] [Google Scholar]
- 36.Goudar RK, et al. Combination therapy of inhibitors of epidermal growth factor receptor/vascular endothelial growth factor receptor 2 (AEE788) and the mammalian target of rapamycin (RAD001) offers improved glioblastoma tumor growth inhibition. Mol Cancer Ther. 2005;4:101–12. [PubMed] [Google Scholar]
- 37.Galanis E, et al. Phase II trial of temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group Study. J Clin Oncol. 2005;23:5294–304. doi: 10.1200/JCO.2005.23.622. [DOI] [PubMed] [Google Scholar]
- 38.Chang SM, et al. Phase II study of CCI-779 in patients with recurrent glioblastoma multiforme. Invest New Drugs. 2005;23:357–61. doi: 10.1007/s10637-005-1444-0. [DOI] [PubMed] [Google Scholar]
- 39.Adjei AA. Blocking oncogenic Ras signaling for cancer therapy. J Natl Cancer Inst. 2001;93:1062–74. doi: 10.1093/jnci/93.14.1062. [DOI] [PubMed] [Google Scholar]
- 40.Cloughesy TF, et al. Phase II trial of tipifarnib in patients with recurrent malignant glioma either receiving or not receiving enzyme-inducing antiepileptic drugs: a North American Brain Tumor Consortium Study. J Clin Oncol. 2006;24:3651–6. doi: 10.1200/JCO.2006.06.2323. [DOI] [PubMed] [Google Scholar]
- 41.Gilbert MR, et al. A phase I study of temozolamide (TMZ) and the farnesyltransferase inhibitor (FTI), lonafarnib (Sarasar, SCH66336) in recurrent glioblastoma. Proc Am Soc Clin Oncol. 2006;24:1556. [Google Scholar]
- 42.da Rocha AB, Mans DR, Regner A, Schwartsmann G. Targeting protein kinase C: new therapeutic opportunities against high-grade malignant gliomas? Oncologist. 2002;7:17–33. doi: 10.1634/theoncologist.7-1-17. [DOI] [PubMed] [Google Scholar]
- 43.Graff JR, et al. The protein kinase Cβ-selective inhibitor, enzastaurin (LY317615.HCl), suppresses signaling through the AKT pathway, induces apoptosis, and suppresses growth of human colon cancer and glioblastoma xenografts. Cancer Res. 2005;65:7462–9. doi: 10.1158/0008-5472.CAN-05-0071. [DOI] [PubMed] [Google Scholar]
- 44.Tabatabai G, et al. Synergistic antiglioma activity of radiotherapy and enzastaurin. Ann Neurol. 2007;61:153–61. doi: 10.1002/ana.21057. [DOI] [PubMed] [Google Scholar]
- 45.Fine HA, et al. Enzastaurin (ENZ) versus lomustine (CCNU) in the treatment of recurrent, intracranial glioblastoma multiforme (GBM): a phase III study. J. Clin. Oncol. 2008;26 Abstract 2005. [Google Scholar]
- 46.Halatsch ME, Schmidt U, Behnke-Mursch J, Unterberg A, Witz CR. Epidermal growth factor receptor inhibition for the treatment of glioblastoma multiforme and other malignant brain tumours. Cancer Treat Rev. 2006;32:74–89. doi: 10.1016/j.ctrv.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 47.Quang TS, Brady LW. Radioimmunotherapy as a novel treatment regimen: 125I-labeled monoclonal antibody 425 in the treatment of high-grade brain gliomas. Int J Radiat Oncol Biol Phys. 2004;58:972–5. doi: 10.1016/j.ijrobp.2003.09.096. [DOI] [PubMed] [Google Scholar]
- 48.Wygoda Z, et al. Use of monoclonal anti-EGFR antibody in the radioimmunotherapy of malignant gliomas in the context of EGFR expression in grade III and IV tumors. Hybridoma (Larchmt) 2006;25:125–32. doi: 10.1089/hyb.2006.25.125. [DOI] [PubMed] [Google Scholar]
- 49.Akabani G, et al. Dosimetry and radiographic analysis of 131I-labeled anti-tenascin 81C6 murine monoclonal antibody in newly diagnosed patients with malignant gliomas: a phase II study. J Nucl Med. 2005;46:1042–51. [PubMed] [Google Scholar]
- 50.McLendon RE, et al. Tumor resection cavity administered iodine-131-labeled antitenascin 81C6 radioimmunotherapy in patients with malignant glioma: neuropathology aspects. Nucl Med Biol. 2007;34:405–13. doi: 10.1016/j.nucmedbio.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pastan I, Chaudhary V, FitzGerald DJ. Recombinant toxins as novel therapeutic agents. Ann Rev Biochem. 1992;61:331–54. doi: 10.1146/annurev.bi.61.070192.001555. [DOI] [PubMed] [Google Scholar]
- 52.Sampson JH, et al. Progress report of a Phase I study of the intracerebral microinfusion of a recombinant chimeric protein composed of transforming growth factor (TGF)-β and a mutated form of the Pseudomonas exotoxin termed PE-38 (TP-38) for the treatment of malignant brain tumors. J Neurooncol. 2003;65:27–35. doi: 10.1023/a:1026290315809. [DOI] [PubMed] [Google Scholar]
- 53.D’Abaco GM, Kaye AH. Integrins: molecular determinants of glioma invasion. J Clin Neurosci. 2007;14:1041–8. doi: 10.1016/j.jocn.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 54.MacDonald TJ, et al. Preferential susceptibility of brain tumors to the antiangiogenic effects of an av integrin antagonist. Neurosurgery. 2001;48:151–7. doi: 10.1097/00006123-200101000-00026. [DOI] [PubMed] [Google Scholar]
- 55.Nabors LB, et al. A phase I trial of EMD 121974 for treatment of patients with recurrent malignant gliomas. Neuro Oncol. 2004;6:379. [Google Scholar]
- 56.Vigushin DM, Coombes RC. Histone deacetylase inhibitors in cancer treatment. Anti-cancer Drugs. 2002;13:1–13. doi: 10.1097/00001813-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 57.Chinnaiyan P, Vallabhaneni G, Armstrong E, Huang SM, Harari PM. Modulation of radiation response by histone deacetylase inhibition. Int J Radiat Oncol Biol Phys. 2005;62:223–9. doi: 10.1016/j.ijrobp.2004.12.088. [DOI] [PubMed] [Google Scholar]
- 58.Shaked Y, et al. Cellular and molecular surrogate markers to monitor targeted and non-targeted antiangiogenic drug activity and determine optimal biologic dose. Curr Cancer Drug Targets. 2005;5:551–9. doi: 10.2174/156800905774574020. [DOI] [PubMed] [Google Scholar]
- 59.Takano S, et al. Concentration of vascular endothelial growth factor in the serum and tumor tissue of brain tumor patients. Cancer Res. 1996;56:2185–90. [PubMed] [Google Scholar]
- 60.Peles E, et al. Angiogenic factors in the cerebrospinal fluid of patients with astrocytic brain tumors. Neurosurgery. 2004;55:562–7. doi: 10.1227/01.neu.0000134383.27713.9a. discussion 567–8. [DOI] [PubMed] [Google Scholar]
- 61.Kerbel R, Folkman J. Clinical translation of angiogenesis inhibitors. Nat Rev Cancer. 2002;2:727–39. doi: 10.1038/nrc905. [DOI] [PubMed] [Google Scholar]
- 62.Cha S, et al. Dynamic, contrast-enhanced perfusion MRI in mouse gliomas: correlation with histopathology. Magn Reson Med. 2003;49:848–55. doi: 10.1002/mrm.10446. [DOI] [PubMed] [Google Scholar]
- 63.Kaminogo M, et al. Diagnostic potential of short echo time MR spectroscopy of gliomas with single-voxel and point-resolved spatially localised proton spectroscopy of brain. Neuroradiology. 2001;43:353–63. doi: 10.1007/s002340000473. [DOI] [PubMed] [Google Scholar]
- 64.Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci USA. 1990;87:9868–72. doi: 10.1073/pnas.87.24.9868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jouanneau E. Angiogenesis and gliomas: current issues and development of surrogate markers. Neurosurgery. 2008;62:31–50. doi: 10.1227/01.NEU.0000311060.65002.4E. discussion 50–2. [DOI] [PubMed] [Google Scholar]
- 66.Anderson SA, et al. Noninvasive MR imaging of magnetically labeled stem cells to directly identify neovasculature in a glioma model. Blood. 2005;105:420–5. doi: 10.1182/blood-2004-06-2222. [DOI] [PubMed] [Google Scholar]
- 67.Kang HW, Torres D, Wald L, Weissleder R, Bogdanov AA., Jr Targeted imaging of human endothelial-specific marker in a model of adoptive cell transfer. Lab Invest. 2006;86:599–609. doi: 10.1038/labinvest.3700421. [DOI] [PubMed] [Google Scholar]