Abstract
Objective
This study aimed at determining the standing spinal landmark that corresponds to the inferior tip of the scapula and determining the accuracy of experienced palpators in locating a spinous process (SP) 3 levels above and below a given SP.
Methods
The study participants were 34 asymptomatic or minimally symptomatic chiropractic students. An experienced palpator located the inferior scapular tip on each and then positioned a 2-mm lead marker about 5 cm lateral to the nearest SP. Two more markers were placed at levels intended to be 3 levels above and below the first marker placed. The locations of the scapular tip and the spinal targets were determined by comparison with a radiological criterion standard.
Results
The standing inferior scapular tip corresponded to the T8 SP on average (SD = 0.9). Having placed the first lead marker, examiners on average overshot the upper marker by 0.26 (SD = 0.51) vertebral levels and undershot the lower marker by 0.21 (SD = 0.48) vertebral levels. The modes for the placement of the 3 markers were at T5, T8, and T11.
Conclusion
Approximately 68% of patients would be palpated to have their inferior scapular tips at T7, T8, or T9. An experienced palpator can quite accurately locate vertebral levels 3 above or below a given landmark. Chiropractors and other health professionals using the typical rule of thumb linking the inferior scapular tip to the standing T7 SP have likely been applying clinical interventions at spinal locations different from those intended.
Key indexing terms: Scapula; Thoracic vertebrae; Spine; Chiropractic; Anatomy, Regional
Introduction
It is widely believed that successful treatment requires an accurate diagnosis. For patients with spinal complaints, this would mean, at minimum, that the examiner is capable of identifying a spinal location thought to exhibit a subluxation (manipulable lesion, somatic dysfunction, etc). Chiropractors and chiropractic students use a variety of manual methods to assess vertebral position and alignment, spinal joint movements, tenderness, soft tissue textural changes, muscle tone, myofascial trigger points, and sometimes skin temperature. The PARTS acronym describes this well.1
There are also several instrumented methods commonly used to assess various spinal parameters, including soft tissue compliance, thermal symmetry, pain-pressure thresholds, joint stiffness, neuromuscular function, and vertebral position.2 Among these instrumented spinal examination tools, radiography is probably the most heavily used.3 The preponderance of evidence supports the reliability of radiographic line marking4; but less is known about its validity, the extent to which parameters measured on radiographs accurately describe a flesh-and-blood patient. Many clinicians purport to visualize radiographic findings deemed relevant to chiropractic adjustive procedures and believe these improve the outcome of chiropractic care. For them, these radiological findings either constitute the primary diagnostic procedure or serve as an adjunct to other examination procedures, such as manual palpation. To make proper use of the information seen on radiographs, clinicians must be able to correlate and corroborate manual and radiographic findings. They generally use a number of rules of thumb to move from the radiograph hanging on the view box to the patient. A representative list of such rules of thumb, such as are typically taught at chiropractic colleges, is provided in Table 1.
Table 1.
Rules of thumb commonly used to identify spinal landmarks
| Landmark | Rule of Thumb |
|---|---|
| C1 | Transverse of Atlas Found Palpating Down and in From Inferior Tip of the Mastoid Process |
| C2 | Large Bifid SP |
| C3 | Usually the Smallest Vertebra in the Spinal Column |
| C6 | Last Freely Movable Spinous in Cervical Region Upon Flexion-Extension |
| C7/T1 | Longest Cervical SP. C7, 60%-70% of the Time; T1, 30%-40% of the Time |
| T3 | Found at Spines of the Scapulae |
| T4 and T5 Intervertebral Disk | Sternal Angle, Patient Supine |
| T6 | Found at the Level of the Tip of the Scapula, Patient Prone |
| T7 | Found at the Level of the Tip of the Scapula, Patient Sitting or Standing |
| T10 | Xiphisternal Junction |
| L1 | First Large Blade-Like SP |
| L4 | Across From the Crest of the Ilium When Prone |
| S2 (Second Sacral Tubercle) | Level With or Slightly Below the PSIS |
The primary goal of the present study was to investigate the accuracy of one of these rules of thumb: that linking the spinous processes (SPs) of the standing patient to the inferior tip of the scapula. Lewis et al5 had found that scapular palpation could be accurately performed so that palpation of the inferior scapular tip would likely be within 0.46 cm. Other investigators6,7 had found scapular palpation to be reliable. However, these studies did not guarantee that the information so derived would enable a clinician to accurately locate a specific spinal level. The secondary goal of the present study was to determine how accurately a manual palpator, having first targeted a putative vertebral level, could identify SPs 3 levels above and below.
In the chiropractic profession, in our experience, it is usually taught that the inferior tip of the scapula corresponds to the SP of either T7 when the patient is standing or T6 when the patient is prone. Inspection of textbooks, course manuals, and Internet sources (including representative sources of chiropractic and nonchiropractic literature) indicated that most sources posit the T7 SP of the standing patient to be at the same level as the inferior scapular tip, although some posit T8 and still others either T7 or T8 (Table 2). The most expansive span we encountered was found in Magee's orthopedics text, which states that the inferior tip of the scapula extends to T7 through T9.8
Table 2.
Representative citations for inferior scapular tip as it relates to spinal landmarks
| Statement | Source |
|---|---|
| T7 | |
| … the spine of T7, which overlies the level of the body of T8 … lies at the level of the inferior angle of the scapula when the arms are held by the sides. | [16] |
| Spinous process of T7—opposite the inferior angle of the scapula | [17] |
| Inferior Angle of Scapula can be palpated readily and marks the level of the 7th rib and spinous process of T7. | [18] |
| Bony landmarks—T7 Inferior angle of scapula | [19] |
| As a guide the inferior border of the scapula is located at about T7. | [20] |
| … the inferior margin of the scapula lies at the level of the T7 spinous process. | [21] |
| The inferior angle is usually reported to be in line with the spinous process of T7. It is important to recognize, however, that postural alignment of the shoulder and vertebral column can alter these relationships significantly. | [22] |
| The lower pole of the scapula lies at approximately T7. | [23] |
| Scapula, Inferior angle—opposite the spine of vertebra T7 | [24] |
| The inferior angles of the scapulae lie at the level of the spinous process of the seventh thoracic vertebra | [25] |
| T8 | |
| T8—level of inferior angle of scapula | [26] |
| … the scapula's inferior angle at the level of the T8 spinous process, a typical position… | [27] |
| … we established T8 for standardization as the nearest spinous process and measured to the inferior angle of the scapula. | [14] |
| T7-8 | |
| The thoracic SP corresponding with the inferior angle of the scapula (T7 or T8) | [5] |
| The inferior angle of the scapula is normally at the level of the T7-T8 spinous processes | [28] |
| T7/T8—Lower border of scapula | [29] |
| Landmarks—T7, T8: inferior angle of scapula | [30] |
Methods
The study population consisted of volunteer chiropractic students who were permitted to receive spinal radiographs at the college clinic free of charge. Therefore, students were not radiographed specifically for this study, which rather “harvested” the information on mostly routine anteroposterior (AP) full-spine radiographs that were ordered and obtained independently of the investigators. The inclusion criteria for the study were that the research participants must be 2 or less on an 11-point numeric pain scale in the thoracic spine. The only modification to the radiographic procedure involved taping 3 lead ball bearings (BBs) to the subject.
Standing subjects wore clinic gowns that exposed their backs during the placement of the 3 BBs, 2-mm lead markers placed on self-adhesive pads. The midthoracic SPs were palpated by either of 2 experienced chiropractors to locate the level corresponding to the inferior tip of either scapula. A BB was then placed approximately 5 cm to the left of the SP. Having placed the first BB, the examiner then palpated 3 levels superiorly and 3 levels inferiorly and placed 2 additional BBs (Fig 1).
Fig 1.
Radiograph with lead markers (BBs) in place.
An AP full-spine radiograph (30 × 90 cm) was taken of each subject subsequent to marker placement. Collimation and filtration of the x-ray beam were in accordance with the chiropractic college clinic's standard radiographic protocol. The radiographs were analyzed to determine the level of the BBs in relation to the thoracic SPs by using a ruler to draw a horizontal line through each BB, noting the SP through which it passed. A forced-call method was used, in which the assessor or assessors were required to choose the transected SP as best they could even when the level seemed equivocal. The data were analyzed using the Statistical Package for the Social Sciences for Windows, Version 12 software (SPSS Inc, Chicago, IL).
This project was approved by the institutional review board of the Palmer College of Chiropractic. Each participant read and signed an informed consent form, and was provided an opportunity to ask questions of the investigators at that time.
Results
The study sample consisted of 34 subjects; 41%, female; mean age, 26 years; mean height, 73.6 cm; and mean weight, 172 kg.
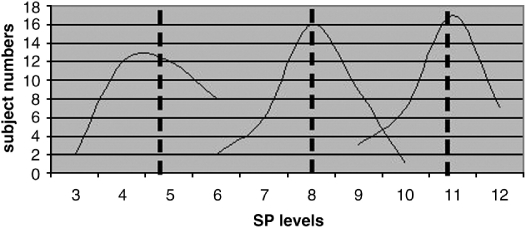
The range for the placement of the first (middle) BB was T6 through T10, and its mean placement was at T8.03, SD = 0.9 (ie, very slightly inferior to the T8 SP). The range for the BB presumed to be 3 levels above the first BB positioned was T3 through T6, and its mean was T4.76. The range for the BB presumed to be 3 below the first positioned was T9 through T12, and its mean was T10.82. Having placed the middle BB, the examiners on average overshot the upper BB by 0.26 (SD = 0.51) vertebral levels (about 1 cm) and undershot the lower BB by 0.21 (SD = 0.48) vertebral levels. The modes for the placement of the 3 BBs were at T5, T8, and T11. Table 3 (left) shows the levels at which the BBs were placed, as does Fig 2, in which the dashed vertical lines show the mean placement locations. Table 3 (right) shows that the mean difference between the upper and middle BBs was 3.3 spinal levels (SD = 0.51), that between the middle and lower BBs was 2.8 spinal levels (SD = 0.48), and that between the upper and lower BBs was 6.0 levels (SD = 0.78).
Table 3.
Ball bearing level (left) and mean differences (right)
| Upper | Middle | Lower | Upper and Middle BBs | Middle and Lower BBs | Upper and Lower BBs | |
|---|---|---|---|---|---|---|
| Mean | 4.76 | 8.03 | 10.82 | 3.26 | 2.79 | 6.06 |
| SD | 0.89 | 0.90 | 0.87 | 0.51 | 0.48 | 0.78 |
| Median | 5.0 | 8.0 | 11.0 | 3.0 | 3.0 | 6 |
| Mode | 4/5 | 8 | 11 | 3.0 | 3.0 | 6 |
| Minimum | 3 | 6 | 9 | 2 | 2 | 5 |
| Maximum | 6 | 10 | 12 | 4 | 4 | 8 |
Fig 2.
Ball bearing positions in relation to thoracic SPs.
The data show that the initial placement of the BB corresponding to the inferior tip of the scapula was very close to the T8 SP. Table 4 provides the data on how often the examiners positioned the BBs at the T8 SP, as well as levels intended to be 3 levels above and below the scapular tip target.
Table 4.
Frequency of SP identification in relation to the scapular tip, 3 levels above and below initial BB placement at T8
| 2 Levels Above | 1 Level Above | On Target, T8 | 1 Level Below | 2 Levels Below | |
|---|---|---|---|---|---|
| T8 SP | 2 (6%) | 6 (18%) | 16 (47%) | 9 (26%) | 1 (3%) |
| T5 SP (3 Levels Above) | 2 (6%) | 12 (35%) | 12 (35%) | 8 (24%) | 0 (0%) |
| T11 SP (3 Levels Below) | 3 (9%) | 7 (21%) | 17 (50%) | 7 (21%) | 0 (0%) |
Discussion
The results of this study are not consistent with the common belief that the inferior tip of the scapula is at the level of the T7 SP in a standing patient. Using the scapular tip as a palpatory landmark resulted in placing the BB closer on average to the T8 SP. This isconsistent with another study we currently have in press,9 which also finds the scapular tip to be on average near the SP of T8. Because the first BB placed tended to be near the T8 SP, the upper BB corresponded closely to the T5 SP and the lower BB to the T11 SP. The medians were indeed T5, T8, and T11.
The examiners displayed a considerable degree of internal consistency in their manual palpation: having located a spinal landmark corresponding to the inferior tip of the scapula, they could accurately (SD approximately one half of a vertebral level) locate other spinal levels thought to be 3 levels above or below. Thus, if an examiner were able to accurately locate a spinal level, using it to in turn identify other nearby spinal levels would be warranted. The palpator would have a 68% chance of being within an interval spanning the nearby target and one half a vertebral level above and below, and a 95% chance of being within an interval one vertebral level above and below the target.
In general, it is important that any health care professional needing to locate spinal levels on a patient realize that there is variability in patients' anatomy on the one hand and some degree of examiner error on the other. To further complicate matters, the examiners could be using a “rule” of some kind to locate spinal landmarks that is not valid. Broadbent et al,10 for example, found that anesthetists, trying to locate a specific lumbar segment, identified a level one above the target in 51% of cases and were correct only 29% of the time. Furness et al,11 comparing the accuracy of palpation and ultrasound, had a similar outcome: palpation was only 30% accurate in identifying a lumbar level.
For the sake of simplicity in this discussion, we will round off the SDs seen in this study, which averaged 0.89 for the 3 levels palpated, to 1.0, or one vertebral level. Given our finding that the inferior scapular tip is on average near the T8 SP, the SD of 1 level means that about 68%s of patients would be palpated to have their inferior scapular tips at T7, T8, or T9 and that about 95% of patients would have their scapular tips palpated between the SPs of T6 through T10. Thus, anatomical variation among patients adds to probable examiner errors such that any rule of thumb linking the scapular tip to a specific spinal level identifies at best a 3-bone range more likely to include the tip than not, rather than a point location in which to have confidence.
Although this finding should be a matter of concern for all health care professions that routinely depend on such rules of thumb to find anatomical landmarks (eg, anesthetists, surgeons, nurses, diskographers, physical therapists), we herein limit our discussion to the implications for the chiropractic profession. In our study, we make no attempt to determine or even discuss whether clinically relevant subluxations (subluxation-equivalents,12 somatic dysfunctions, manipulable lesions, etc) can be seen on radiographs. On the other hand, it would be argued that many chiropractors do make just that claim.13 So long as that is the case, chiropractors who take radiographs to identify subluxations must realize that it is not as easy as it seemed to go from the view box to the flesh-and-blood patient.
Each of the following parameters has an influence on the accuracy of locating a spinal level seen on a radiograph on a patient:
-
1.
Identifying a spinal level on the radiograph, taking into account radiological distortion
-
2.
Using a rule of thumb that purportedly associates that spinal level with another more easily palpated anatomical landmark, such as the iliac crest, vertebra prominens, or scapular tip
-
3.
Accurately identifying that anatomical landmark on the patient
-
4.
Knowing if and how the patient's position (standing, seated, prone, or supine) influences the accuracy of the rule of thumb
-
5.
Accurately identifying the vertebral level coinciding with the anatomical landmark on the patient
We presume that criteria 1, 3, and 5 are not overly problematic; but the present study suggests that criteria 2 and 4 represent matters of some concern, especially criterion 2. The rule of thumb most used in chiropractic and elsewhere—that the inferior scapular tip lies at the SP of T7—is, on average, off by about a level. That means that any spinal landmark located starting from this landmark is likely to be phase-shifted by about one vertebral level, winding up one level below what was intended. Moreover, patient anatomical variation is such that even “correcting” the rule of thumb would at best direct the chiropractor to a 3-level spinal region more likely than not to contain the level seen on the radiograph, not the point location that is generally desired. Finally, because there is little information available concerning criterion 4, the assumption that there is yet another rule of thumb validly associating an anatomical location in the standing position with what is seen in a seated or prone patient is unwarranted. In the study at hand, we simply do not know, whatever SP the scapular tip relates to in the standing position, to what SP it relates to in the prone position. Simply stipulating it to coincide with the T6 SP, as is commonly done as we have seen, is not justifiable. As our preliminary observations have shown (not herein reported), it is likely that the physical characteristics of the patient, how he or she is positioned on the table (particularly the arm position), and the type of table itself are likely to have an impact on standing/prone relationships.
If, as we suspect, chiropractors have been using the standing T7 SP = scapular tip and the prone T6 = scapular tip rules for finding thoracic locations, they have not been introducing forces where they thought they were. Consistently being one vertebral below the target suggested by radiography results in systematic bias, whereas not taking into account that the scapular tip lies within a range rather than a single place introduces random error.
The sources of error we highlight are not entirely insuperable. We believe a clinician could improve his or her accuracy by simply revising the traditional spinal landmark rule of thumb and looking for the scapular tip to be on average one level lower than previously thought. Even more importantly, provided the scapula tip may be visualized on the radiograph, the clinician need not presume what spinal level corresponds to the scapular tip. That information may be directly visualized. Even at that, the chiropractor would still have to determine how that landmark changes going from the standing to the prone or seated position.
Limitations of the study
The data gathered in this study, whose participants consisted of asymptomatic or minimally symptomatic young adults, may not be typical of populations at large.
We did not standardize on palpating the right or the left scapular tip in this study, nor did we record which was palpated for each subject. However, other studies suggest9,14 that the right scapula (more generally, the scapula on the side of the dominant arm) is usually somewhat lower. Having used the left and right scapular tips as a landmark in our study, without having noted which for each subject, we suspect that the mean level for the scapula tip found in this study (8.03, ie, just below the T8 SP) lies somewhat below the mean actual position of the scapula on the nondominant arm and slightly above the mean actual position of the scapula on the dominant arm.
Because all the radiographs in our study were AP full-spine projections, the x-ray beam took an inferior to superior path in passing successively through the vertebral bodies and the inferior scapular angles, thus projecting the scapular tips lower in relation to the spine than they actually are. In another study in press,9 we calculate that the scapular tip would thus be approximately 0.5 cm (approximately one quarter of a typical midthoracic vertebral body) lower than reported therein.
This study is a secondary analysis of data generated during the course of a different study with unrelated goals, but which did involve locating the SP of T7. In that other study, it did not, from a methodological point of view, matter how the examiner attempted to locate the SP of T7. As a result, for about 5 subjects, one of the investigators in the present study attempted to locate the T7 SP by counting down from the vertebra prominens rather than by palpating the scapular tip. Because we do not know the accuracy of this other palpatory method for finding the SP of T7, we cannot determine exactly how much this inconsistency effected our calculations. On the other hand, under the conservative assumption that the spinal level identified by this other method could have been as much as one segment different from the scapular tip method, our overall mean calculation for the SP corresponding to the scapular tip would change by less than 15% of a vertebral level. This would not come close to vitiating our conclusion that the inferior scapular tip is on average very close to the T8 SP. Using the vertebra prominens as a landmark to find a thoracic SP might be very error-prone, given that the vertebra prominens corresponds to the SP of C7 about 70% of the time and of T1 the rest of the time.15
We did not attempt to calculate the interexaminer reliability of scapular tip or SP palpation, although other investigators have indeed done so and found it adequate.5-7 Likewise, we did not calculate the interexaminer reliability of our radiographic line marking comparing scapular and spinal landmarks. On the other hand, a comprehensive review article found many examples of radiographic line marking to be reliable.4
Conclusions
Knowing which thoracic SP corresponds on average to the inferior tip of the scapula might be of clinical value to several health care professions. The investigators have not assumed that the outcome of chiropractic or other types of manual care for spinal complaints is made better by identifying misalignments or other radiological parameters on radiograph. However, chiropractors who believe such information improves the outcome of care and who believe the diagnostic specificity imbued in radiographic line marking improves the clinical outcomes will have to derive an alternative explanation for their presumed good clinical outcomes, at least in the thoracic spine, if they used the rule of thumb investigated in this study. As an alternative, under the assumption that the films provide useful clinical information, their results may have been suboptimal.
At the other extreme, chiropractors who have argued that segmental specificity may not be critical to the outcome of chiropractic might find their views to some degree supported by this study. If they have been getting good outcomes despite having used a questionable rule of thumb for locating spinal levels, the suggestion is that segmental specificity may not be required for such good clinical outcomes. Thus, the radiographic examination thought necessary for this segmental specificity would be unnecessary, although radiographs might be warranted for other reasons, such as ruling out contraindications to manipulation or visualizing gross spinal pathology. In that case, the information provided by radiographs taken to visualize spinal subluxation may not warrant either the biological or monetary cost of exposing patients to ionizing radiation.
Acknowledgment
The authors thank the Palmer College of Chiropractic West–Tasman Clinic Department of X-ray and especially the assistance of Russell Wilson, RTR, CRT. The authors would like to also thank our research assistant, Mr Morgan Young, for his help in executing the project. This research was performed at Palmer College of Chiropractic West and supported by the Palmer Center for Chiropractic Research.
References
- 1.Bergmann T. P.A.R.T.S. joint assessment procedure. Chiropr Tech. 1993;5(3):135–136. [Google Scholar]
- 2.Cooperstein R., Gleberzon B. Technique systems in chiropractic. Churchill Livingstone; Edinburgh: 2004. pp. 21–62. [Google Scholar]
- 3.Christensen M.G. Job analysis of chiropractic. A project report, survey analysis and summary of the practice of chiropractic within the United States. National Board of Chiropractic Examiners; Greeley (CO): 2000. p. 125. [Google Scholar]
- 4.Harrison D.E., Harrison D.D., Troyanovich S.J. Reliability of spinal displacement analysis of plain x-rays: a review of commonly accepted facts and fallacies with implications for chiropractic education and technique. J Manipulative Physiol Ther. 1998;21(4):252–266. [PubMed] [Google Scholar]
- 5.Lewis J., Green A., Reichard Z., Wright C. Scapular position: the validity of skin surface palpation. Man Ther. 2002;7(1):26–30. doi: 10.1054/math.2001.0405. [DOI] [PubMed] [Google Scholar]
- 6.Greenfield B., Catlin P.A., Coats P.W., Green E., McDonald J.J., North C. Posture in patients with shoulder overuse injuries and healthy individuals. J Orthop Sports Phys Ther. 1995;21(5):287–295. doi: 10.2519/jospt.1995.21.5.287. [DOI] [PubMed] [Google Scholar]
- 7.Sobush D.C., Simoneau G.G., Dietz K.E., Levene J.A., Grossman R.E., Smith W.B. The Lennie test for measuring scapular position in healthy young adult females: a reliability and validity study. J Orthop Sports Phys Ther. 1996;23(1):39–50. doi: 10.2519/jospt.1996.23.1.39. [DOI] [PubMed] [Google Scholar]
- 8.Magee D.J. Orthopedic physical assessment. 4th ed. Saunders; Philadelphia (PA): 2002. p. 458. [Google Scholar]
- 9.Haneline M.T., Cooperstein R., Young M., Ross J. Determining spinal level using the inferior angle of the scapula as a reference landmark: a retrospective analysis of 50 x-rays. J Chiropr Educ. 2007;21:104–105. [PMC free article] [PubMed] [Google Scholar]
- 10.Broadbent C.R., Maxwell W.B., Ferrie R., Wilson D.J., Gawne-Cain M., Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55(11):1122–1126. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 11.Furness G., Reilly M.P., Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002;57(3):277–280. doi: 10.1046/j.1365-2044.2002.2403_4.x. [DOI] [PubMed] [Google Scholar]
- 12.Cooperstein R., Gleberzon B.J. Toward a taxonomy of subluxation-equivalents. Top Clin Chiropr. 2001;8(1):49–60. [Google Scholar]
- 13.Plaugher G. The role of plain film radiography in chiropractic clinical practice. Chiropr J Aust. 1992;22(4):153–161. [Google Scholar]
- 14.Gibson M.H., Goebel G.V., Jordan T.M., Kegerreis S., Worrell T.W. A reliability study of measurement techniques to determine static scapular position. J Orthop Sports Phys Ther. 1995;21(2):100–106. doi: 10.2519/jospt.1995.21.2.100. [DOI] [PubMed] [Google Scholar]
- 15.Stonelake P.S., Burwell R.G., Webb J.K. Variation in vertebral levels of the vertebra prominens and sacral dimples in subjects with scoliosis. J Anat. 1988;159:165–172. [PMC free article] [PubMed] [Google Scholar]
- 16.Anatomy for Anaesthetists—Anatomy Relevant to Epidural and Subarachnoid Blockade, Anaesthesia UK. http://www.frca.co.uk/article.aspx?articleid=100361.
- 17.CV 7—Surface Anatomy of the Respiratory System and Heart. From Cognitive Cardiovascular Notes, University of Manitobahttp://umanitoba.ca/faculties/medicine/units/cardiology/cvnotes/cv7.htm.
- 18.From PTA 2102 Anatomy and Movement Course Notes, Murray State College Physical Therapy Assistants Program. Gary Robinson MS, PT, PCS instructor. http://www.mscok.edu/~grobinson/PTA2102/Surface%20Anatomy%20Practice.pdf.
- 19.PASSOR Musculoskeletal Physical Examination Competencies List—Prepared by the PASSOR Task Force on Musculoskeletal Education, American Academy of Physical Medicine and Rehabilitation, Jay Smith, MD, Chair. http://www.aapmr.org/passor/attachmt/msk.pdf.
- 20.Grand Rounds Article: The Five-Minute Shoulder Exam, by Mario R. Taillon, MD, FRCSC. 2004 Continuing Professional Learning, University of Saskatchewan, Canada. http://www.usask.ca/cme/articles/fmse/index.php.
- 21.Epidural Anesthesia, Raymond Graber, MD, 8/15/2000. University Hospitals of Cleveland, Department of Anesthesiology. http://www.uhcanesthesia.com/ClinDiv/Anesthesiology/Regional%20Anesthesia/epid/view.
- 22.Kinesiology: The Mechanics & Pathomechanics of Human Movement, Oatis, C.A. 1st ed. 2004, Philadelphia: Lippincott Williams & Wilkins. xx, 899 p. Kinesiology of the Upper Extremity, Chapter 8—Structure and Function of the Bones and Joints of the Shoulder Girdle. p 119.
- 23.Doncaster & Bassetlaw Hospitals NHSFT—The Scope of Professional Practice—Training Package For: Insertion of Lumbar and Thoracic Epidural Catheters. Compiled by Steve Gosney (Advanced Anaesthetic Practitioner) (January 2005). http://www.wise.nhs.uk/surgery/NationalGoodPractice/downloads/4/4d8.doc.
- 24.From Surface Anatomy IV: Musculoskeletal Examination of the Upper Limb, CHA 400/200 Developmental, Gross & Radiologic Anatomy Notes, Douglas Gross, MD, PhD. 2004 University of California, Davis.
- 25.From Skeletal And Developmental Anatomy for Students of Chiropractic, p. 106, by Robert A. Walker, Owen Lovejoy, M. Elizabeth Bedford, and William Yee. Used at New York Chiropractic College, Seneca Falls, New York. Full text available at http://www.fadavis.com/related-resources/1-1886-1.pdf.
- 26.Gross Anatomy Lab Instructions and Guidelines. PTH 1252 (Clinical Gross Anatomy 1) Notes, Northeastern University, Bouv College of Health Sciences, Physical Therapy. http://www.ptd.neu.edu/pth1252/LAB.doc.
- 27.Shoulder Anatomy and Function 1—Occupational Therapy/Physical Therapy 7143 Control of Human Movement 1 Laboratory Procedures. University of Oklahoma. Dave Thompson, PT. http://moon.ouhsc.edu/dthompso/NAMICS/labs/shldr1.htm.
- 28.The University of Queensland, School of Biomedical Sciences, Department of Anatomical Sciences, AN212 Lecture—POSTURE, Prepared by Dr Vaughan Kippers. http://www.uq.edu.au/~anvkippe/an212/posture.html.
- 29.The Back—gp-training.net. http://www.gp-training.net/rheum/backpain/index.htm.
- 30.From Musculoskeletal System Notes, NU 325 Health Assessment, University of South Alabama College of Nursing. http://www.southalabama.edu/nursing/baldwinco/325musculoskeletal.PDF.