Abstract
Objective
The purpose of this study was to collect preliminary information on the effects of chiropractic spinal manipulation on reducing risk of falls in older adults with impaired balance, as assessed by the Berg Balance Scale (BBS). This information is necessary to develop a line of investigation into the role of chiropractic care on reduction of fall risk in this population.
Methods
Randomized, 2-group pretest/posttest design feasibility study with a target sample size of 10 (5 per group), conducted within the outpatient health center of a chiropractic college. Inclusion criteria were as follows: aged 60 years or older, able to stand on one leg <5 seconds, and able to attend all sessions. Patients were assigned to chiropractic care (CMT) or supervised exercise (EX) and scheduled for 2 visits per week for 8 weeks.
Results
A total of 26 people responded to recruitment; and 11 were enrolled: 6 in the CMT and 5 in the EX group. Two patients dropped out at the baseline visit when they were assigned to the EX group. One CMT patient dropped out in the seventh week because of a fall at home resulting in a leg fracture. All remaining patients were compliant with treatment protocols. Five of 6 CMT patients and 4 of 5 EX patients had baseline BBS scores <45, indicating increased risk of falls. At visit 16, 2 CMT and 1 of the 3 remaining EX patients had BBS scores <45. One mild and transient adverse event was noted.
Conclusion
Further investigation of the possible role of chiropractic care in reducing fall risk in this population appears feasible.
Key indexing terms: Chiropractic; Manipulation, Spinal; Balance, Postural; Accidental falls; Geriatrics
Introduction
Falls are the leading cause of nonfatal injury in older adults and account for two thirds of all unintentional injury deaths in this population.1 Direct medical costs of falls have been estimated at $6 billion to $8 billion per year.2 Furthermore, fall death rates have increased significantly from 1988 to 2000 for both men and women.3
According to a 2003 evidence-based guideline for fall prevention, impairments in balance, gait, and activities of daily living as well as lower extremity weakness and/or dysfunction are among the most important modifiable risk factors for falls in older adults.4 Other important modifiable risk factors include impaired mental status, use of psychotropic medications, polypharmacy, environmental hazards, and poor vision.4
There is considerable evidence for positive effects of spinal manipulation for spine-related pain.5,6 Because chronic musculoskeletal pain, such as that of osteoarthritis, is one factor affecting gait and balance in older people, chiropractic care may have an impact on fall prevention by treating joint pain and dysfunction. Furthermore, the literature suggests a possible positive effect of manipulation on cervicogenic vertigo.7,8 However, at this time, only one experimental study investigating the effect of chiropractic care on balance in older adults in relationship to fall prevention has been published.9 The purpose of this study was to collect preliminary information on the effects of chiropractic spinal manipulation on reducing risk of falls in older adults with impaired balance, as assessed by the Berg Balance Scale (BBS).
Methods
This project was a randomized, pretest/posttest design feasibility study conducted to further the development of a line of investigation into the possible effects of chiropractic care on reducing risk of falls in older adults with impaired balance. The 2 treatment groups were chiropractic care with spinal manipulative therapy (CMT) and supervised balance exercise (EX).
Its specific aims were to (1) assess the utility of various recruitment methods within the local community; (2) assess participants' compliance with treatment group assignment and study protocols; (3) develop protocols for collecting accurate data on falls from study patients; (4) assess the utility and responsiveness of the BBS and one leg standing test (OLST) in our sample population; and (5) collect preliminary information on the possible relationships of dizziness and/or chronic pain to poor balance.
Safety and other human subjects considerations
The study was approved by the Cleveland Chiropractic College institutional review board before recruitment, and all patients signed an informed consent form before any data collection or treatment. Patients' confidentiality was protected by secure storage of data in a password-protected computer and reporting of results in group form only. Their safety was protected by excluding patients for whom CMT was contraindicated and by performing a thorough physical examination, including diagnostic radiographs if indicated by the history and physical examination. All treating clinicians were licensed clinical faculty with at least 5 years' experience. The examining clinicians reviewed the results of the history, physical examination, and radiographs; determined whether eligible patients required a modification of standard diversified technique, which is consistent with recommendations for chiropractors for treating frail elderly10; and recorded this in their chart. Modifications included reduction of force, velocity, and rotation; instrument-assisted adjustments; mobilization; or flexion-distraction technique.
Adverse events were defined as any symptoms arising within 24 hours of a treatment session and persisting for more than 24 hours after onset. Clinicians asked patients at each visit about any discomfort they may have experienced since the last treatment and, if any were reported, recorded them in the clinical notes. Those symptoms meeting the definition of an adverse event were to be reported on the “Adverse Event” form and to the principal investigator, and a decision would be made about whether to continue treatment.
Study population
For this feasibility study, we targeted a sample size of 10 (5 per group). Eligibility criteria were as follows:
Inclusion: (1) aged 60 years or older; (2) able to stand steadily without assistance on one leg for less than 5 seconds (determined by averaging the combined time for each leg); (3) able to attend all scheduled sessions (by self-report).
Exclusion: (1) nonambulatory (wheelchair-bound) (this precludes required balance testing; however, volunteers requiring assistive devices such as canes and walkers were not excluded); (2) received chiropractic care or any other manual care procedure within the past month (by self report); (3) initiated an exercise program targeting balance and/or lower body strength within past month (by self-report); (4) contraindications to CMT or mild-exertion exercise, as determined by the clinician through physical examination and radiographs (if indicated); (5) absence of indications for CMT, as determined by the clinician through history, physical examination, orthopedic tests, and static and motion palpation; (6) unable to understand English adequately to complete study forms and questionnaires.
Recruitment strategies
Based on successful strategies used in previous studies elsewhere,9,11,12 our recruitment methods were (1) presentations at senior centers and events (primary method); (2) posters and flyers in the college and local neighborhood; (3) ads in local newspaper and/or senior publications; and (4) word of mouth and referrals through friends and family members of college employees, students, and clinic patients.
Study protocol
We screened volunteers for preliminary eligibility by phone and/or at off-site events. If eligible, they presented to the clinic; and the coordinator verified preliminary eligibility, explained the study, and obtained informed consent. An assessor conducted the BBS and the OLST to determine the second level of eligibility (able to stand on one leg for <5 seconds). If eligible, the patient was examined by the treating clinician to verify final eligibility, at which point he or she was assigned to a treatment group (see below for allocation scheme).
Treatment group allocation
We used an adaptive randomization scheme based on a minimization algorithm to equalize between-group differences in the baseline BBS score (≥46/<46) and age (≥70/<70 years). The cutpoint of 46 for the BBS was selected to balance groups in terms of risk for falls.13-15 Minimization is recommended for treatment group allocation in small studies to ensure that groups are comparable in factors expected to affect outcomes.16
Interventions
Chiropractic care
We designed this intervention to represent the usual and customary procedures used by most chiropractors.17 Thus, the intervention included spinal and extravertebral manipulation using diversified technique, soft tissue treatment such as myofascial release, and heat or cold. As stated above, clinicians used modified (lower force) adjustive procedures if the examining clinician indicated that these were warranted.
Supervised exercise
Patients in this group were instructed to perform a set of balance exercises recommended by the National Institute on Aging.18 The 8 exercises include standing hip flexion, standing hip extension, standing plantar flexion, standing knee flexion, standing side leg raise, heel-to-toe walking, standing on one foot, and standing up and sitting down without use of hands. They were supervised at each visit by a licensed chiropractor with advanced training in exercise physiology as well as more than 10 years in chiropractic practice.
Frequency and duration of care
All patients were scheduled for 2 visits per week during the 8-week treatment period (total of 16 treatment visits). The CMT office visits took approximately 10 to 15 minutes, and exercise visits took approximately 15 minutes.
Blinding
It was impossible to blind patients or treating doctors. However, the primary outcome assessment (BBS) was conducted by an assessor blinded to patients' treatment group assignment. To reduce variability in assessments, we attempted to have the same assessor conduct the BBS each time. We were unable to blind the assessors to whether the visit was baseline (VO), visit 8 (V8), or visit 16 (V16), however.
Assessment methods and instruments
Baseline information collected on all patients included demographics, health history, health habits, medication use, and history of falls. We also asked questions about their fluid, caffeinated beverage, and alcohol intake because dehydration or alcohol abuse may contribute to balance problems. A 2-question depression screener was included.19 To obtain accurate medication records, patients were asked to bring their medications to the baseline visit; and the study coordinator recorded them. To record fall data, we used 3 methods: (1) Consistent with the method recommended to collect falls data in population-based studies,20 patients were provided with fall calendars and were instructed to maintain them and return them at the end of each month. (2) Doctors asked patients at each visit whether they had experienced any falls and recorded their response on the “clinical notes” form. (3) The study coordinator asked the patient about falls in the past year and past month at the intake interview and about falls during the study period at the exit interview.
The following outcome measures were collected at baseline, V8 (after 4 weeks of treatment), and V16 (conclusion of the study). At those visits, they were completed before the patient's contact with the clinician.
The BBS was the primary outcome measure. The BBS is a 14-item functional test involving actions required to perform daily activities (eg, standing up, picking up an object). It takes approximately 15 minutes to conduct. Its reliability and validity in assessing balance have been documented in community-dwelling older adults, and its predictive value with respect to falls is well-established. It is considered the criterion standard for assessing older adults' risk of falls.13-15,21,22 While performing the tasks included in the BBS, the patient is scored on a 5-point (0-4) ordinal scale, with “0” assigned if the task cannot be completed and “4” indicating independence. A score less than 46 is used by most investigators to indicate a greater risk for falls.13-15
Three clinicians trained together to perform the BBS, developing a set of administration standards to ensure uniform conduct of the test.23 To assist in developing these standards, we had an introductory training session with a physical therapist with more than 20 years' experience in practice who regularly used the BBS in patient assessment.
The OLST is commonly used among physical therapists to assess postural stability. It demonstrates moderate to high interrater and test-retest reliability with adults.24,25
The Pain Disability Index (PDI) is a 7-item patient questionnaire with a scoring range of 0 to 70 designed to assess perception disability related to chronic pain.26-28 Its reliability and validity have been documented.28,29
The Dizziness Handicap Inventory (DHI) is a 25-item self-assessment scale with scores ranging from 0 (no handicap) to 100 (significant perceived handicap). Scores are highly correlated with platform posturography. The DHI has been shown to be valid, reliable, and sensitive to clinical change, with 18 points representing a clinically meaningful change.30,31
Data management and analysis
Patient forms were stored in a secure cabinet, and only data entry personnel had access to them. All study data were double key-entry verified and maintained electronically in a password-protected database on a secure network. The SPSS version 14 (SPSS, Chicago, IL) was used for data analysis. Because this was a feasibility study with a small sample, we did not aggregate the data in reporting the results; no inferential statistics were used. For patients who did not complete the study, we reported the V8 (1 month after baseline) outcome scores, if available.
Results
Recruitment, enrollment, and attrition
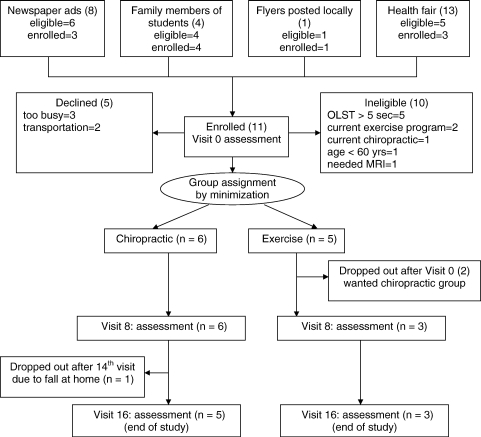
Recruitment started in the fall of 2006; a total of 26 people responded to recruiting efforts, of which 11 were enrolled in the study (42%). The distribution of responses to the various recruitment methods is shown in Fig 1. Two newspaper ads were placed, for a total of $1400. From a total of 8 responses to these ads, 3 patients were enrolled, for a cost of $467 per patient. Three project personnel hosted a booth for 4 hours at one senior health fair, which resulted in 13 responses and 3 patients enrolled. This activity had no associated monetary costs other than personnel time, and it established a liaison with members of the local senior community. Flyers and word of mouth had no costs and negligible personnel time. Flyers were posted at 10 local businesses, resulting in one enrolled patient. Word of mouth, in which interns were provided with information about the study, resulted in 4 responses from student family members, of which all 4 were enrolled.
Fig 1.
Study flow chart.
The most common reason for ineligibility was being able to stand on one leg longer than 5 seconds (5/10). The reasons eligible potential patients gave for declining to participate were being too busy to commit to the office visits required (3/5) and difficulty with transportation (2/5).
Minimization resulted in 6 patients assigned to the chiropractic group and 5 to the exercise group. Two patients in the exercise group dropped out immediately at the baseline visit because they had wanted to be assigned to the chiropractic group. These patients were the parents of a chiropractic student. One patient in the chiropractic group dropped out in the seventh week because she had a fall at home and fractured her leg, requiring hospitalization. Thus, attrition was 2 of 5 in the exercise group and 1 of 6 in the chiropractic group.
Baseline characteristics
Table 1 summarizes the 11 patients' baseline characteristics. The 2 groups were similar in most characteristics, although the chiropractic group appeared somewhat older (median age of 79 years compared with 73 years in the exercise group). Most reported positive health habits, and only one in each group screened positive for depression. Table 2 summarizes patients' reported functional impairments and comorbidities. None of the patients required routine use of assistive devices such as canes or walkers, and one in each group reported a joint replacement. Nine of 11 reported hypertension, 3 reported low back pain, and 2 (both in the chiropractic group) reported vertigo frequent enough to require treatment. Both patients with vertigo had been prescribed meclizine (an antihistamine used to treat dizziness) by their physicians but reported that it did not help. For one of these patients, the physical examination indicated a peripheral cause of vertigo, with a positive test for positional vertigo; cervicogenic vertigo was not ruled out. For the other, thorough assessment of the cervical spine for possible causes of vertigo could not be performed because of extremely restricted movement and pain.
Table 1.
Baseline characteristics by group
| Chiropractic n = 6 | Exercise n = 5 | Total n = 11 | |
|---|---|---|---|
| Age (y)a | 79 (67-92) | 73 (63-81) | 73 (63-92) |
| Sex (Women/Men) | 3/3 | 3/2 | 6/5 |
| Marital Status | |||
| Married/Living With Partner | 2 | 3 | 5 |
| Living Alone/Divorced | 3 | 1 | 4 |
| Living Alone Because of Death of Spouse | 1 | 1 | 2 |
| Race/Ethnicity | |||
| Hispanic/Latino | 0 | 2 | 2 |
| White | 5 | 3 | 8 |
| Did Not Respond | 1 | 0 | 1 |
| Education (Highest Level Completed) | |||
| High School | 3 | 2 | 5 |
| Some College | 1 | 0 | 1 |
| College Degree | 1 | 1 | 2 |
| Postgraduate Degree | 1 | 2 | 3 |
| Employment | |||
| Retired | 6 | 4 | 10 |
| Employed Part-Time | 0 | 1 | 1 |
| Positive Response to Depression Screenb | 1 | 1 | 2 |
| Use of Alcohol | |||
| Never | 4 | 3 | 7 |
| Occasionally | 2 | 2 | 4 |
| Use of Tobacco | |||
| Current Use | 2 | 0 | 2 |
| Past Use | 1 | 2 | 3 |
| Never Used | 3 | 3 | 6 |
| Aerobic Exercise (Walking) | |||
| Never | 1 | 2 | 3 |
| 1-2 Times Per Week | 3 | 0 | 3 |
| 3 or More Times Per Week | 2 | 3 | 5 |
| Other Exercise (Stretching, Gardening) | |||
| Never | 2 | 2 | 4 |
| 1-2 Times Per Week | 1 | 1 | 2 |
| 3 or More Times Per Week | 2 | 2 | 4 |
| Water Consumed Daily (Cups Reported)a | 5 (4-8) | 4 (3-6) | 4.5 (3-8) |
| Caffeinated Drinks Consumed Daily (Cups Reported)a | 2 (0-10) | 2 (0-5) | 2 (0-10) |
Unless otherwise specified, frequencies rather than proportions are displayed because of the small sample size.
Median (minimum-maximum).
Depression screener: a yes to either of the following 2 questions is considered indicative of depression: Over the past 2 weeks, have you felt down, depressed, or hopeless? Over the past 2 weeks, have you felt little interest or pleasure in doing things?
Table 2.
Baseline functional impairments and comorbidities
| Chiropractic n = 6 | Exercise n = 5 | Total n = 11 | |
|---|---|---|---|
| Use of Assistive Device (Cane, Walker) | 0 | 0 | 0 |
| Joint Replacement | 1 (Great Toe) | 1 (Knee) | 2 |
| Visual Impairment | |||
| Corrective Lenses | 6 | 5 | 11 |
| Eye Examination in Last Year | 5 | 4 | 10 |
| Current Conditions Reported | 5 | 3 | 8 |
| Hypertension | 5 | 4 | 9 |
| Low Back Pain | 1 | 2 | 3 |
| Arthritis | 1 | 1 | 2 |
| Diabetes | 1 | 1 | 2 |
| Fibromyalgia | 2 | 0 | 2 |
| Vertigo | 2 | 0 | 2 |
Unless otherwise specified, frequencies rather than proportions are displayed because of the small sample size.
Medication use
All patients who used medications brought them on their first visit or brought a list that they had prepared at home directly from the medication labels. Recording their medications was a time-consuming task for the study coordinator; and because of time constraints, the medication form was hastily completed and difficult for the data entry staff to decipher; 6% (3/53) of the separate entries for medications for the data set of 11 patients were indecipherable.
Number of prescription medications ranged from 0 to 16, with a median of 4. One patient reported no medication use. Antihypertensive medications were most common (9 of 11), followed by lipid-lowering medications (3) and medications for gastroesophageal reflux disease (3) and thyroid hormone (3). Two patients were diabetic, and 2 were taking medication to control dizziness. Only one used a prescription pain medication. With respect to nonprescription medications and supplements, 4 took vitamin supplements, 3 took aspirin, and 1 took a nonaspirin pain medication.
Reporting of falls data
As shown in Table 3, at the intake interview, 6 patients recalled having a fall in the past year and 3 in the past month. All but one of the 11 patients forgot to complete and bring in their fall calendars, so no data on falls during the study were available through this method. Clinicians asked patients about falls at each visit and recorded falls for 4 patients, one of whom reported 4 falls during the study. Only one of these falls required treatment. This fall was reported on the clinical notes form by the clinician after he called the patient to follow up because of her cancellation of an appointment during week 7 of the study. She had fallen at home, was taken to the emergency department, and subsequently required surgery for a fractured leg, therefore dropping out of the study. At the exit interview, one of the patients who had reported a fall to the clinician did not report it at this interview, which took place at the end of the 8-week study period. The patient who reported 4 falls to the clinician during the study reported 7 falls at the exit interview, over the same period. None of these falls required treatment.
Table 3.
Comparison of methods of collecting falls data
| ID | Intake Interview |
Fall Calendar | Exit Interview | Clinical Notes | |
|---|---|---|---|---|---|
| Past Year | Past Month | ||||
| Chiropractic | |||||
| 29 | Yes; Did Not Remember How Many | 3 | No Dataa | 7; No Treatment | 4; No Treatment |
| 47 | 3 | 0 | No Dataa | 0 | 0 |
| 95 | 0 | 1 | 0 (4-wk Calendar Only) | Not Done; Dropped Out Week 7b | 1; Noted From Phone Callb; Resulted in Leg Fracture and Hospitalization |
| 11 | 0 | 0 | No Dataa | None Reported | 0 |
| 67 | 0 | 0 | No Dataa | 1, No Treatment | 1; No Treatment |
| 01 | 1 | 1 | No Dataa | 0 | 0 |
| Exercise | |||||
| 85 | 0 | 0 | No Dataa | 0 | 1; Radiographs but No Treatment |
| 79 | 1 | 0 | No Dataa | 0 | 0 |
| 27 | 0 | 0 | No Dataa | 0 | 0 |
| 71 | 1 | 0 | Dropped Out | – | – |
| 56 | 1 | 0 | Dropped Out | – | – |
Unless otherwise specified, frequencies rather than proportions are displayed because of the small sample size.
Patients forgot to bring fall calendars.
Clinician followed up by phone after patient called to cancel her next appointment because of a fall at home (unrelated to treatment); patient could not continue the study because of a fractured leg requiring surgery.
Modification of CMT
Of the 6 patients in the chiropractic group, 5 required modification of standard diversified technique. Four patients had osteoporosis advanced enough to require a low-force approach (2 women aged 71 and 92 years and 2 men aged 73 and 87 years). They were treated using instrument-assisted adjusting only. One man, aged 85 years, with ligament ossification and degenerative disk disease in the cervical spine was treated using modified diversified (less force, speed and rotation) and instrument-assisted adjusting.
Outcomes
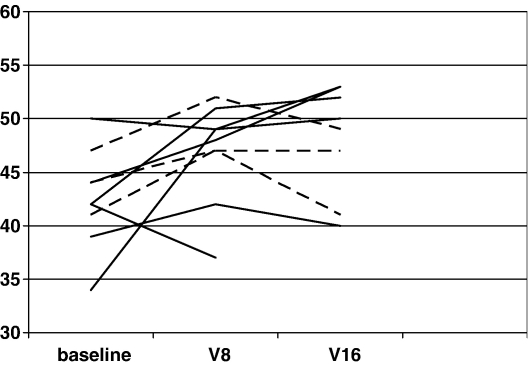
Scheduling required that different assessors conducted the BBS for 4 patients out of the total of 9. Fig 2 graphically illustrates the BBS scores over time, at V0, V8 (1 month from baseline), and V16 (the final visit, 2 months from baseline). Improvement was apparent for most patients at V8, without additional substantial change observed at V16.
Fig 2.
Berg Balance Scale scores at V0, V8 (1 month from baseline), and V16 (2 months from baseline). The chiropractic group is denoted by the solid line, and the exercise group is denoted by the dashed line.
Table 4 shows V0 and V16 scores for the study patients. Five of 6 patients in the chiropractic group and 4 of 5 patients in the exercise group had baseline BBS scores at or below the cutoff score of 45, indicating increased risk of falls. At V16, 2 of 6 in the chiropractic group and 1 of the 3 remaining in the exercise group had BBS scores <45. The OLST scores did not show a consistent trend, although in both groups, changes appeared to be slight from baseline to V16. Baseline PDI scores varied a great deal among patients, although patients with high baseline scores showed substantial improvements at V16. The DHI scores also varied a great deal; but among patients whose baseline DHI scores indicated considerable impairment due to dizziness, none of V0 to V16 change scores were greater than 18 points, indicating lack of clinically meaningful change. The 2 patients (patients 29 and 95) who were on medications for their dizziness both had high baseline DHI scores. The clinical notes for patient 95, who subsequently dropped out because of a fall in her home, consistently reported no change or little change in her dizziness during treatment; and her DHI score at V8 reflected this, being unchanged from her baseline. Patient 29, whose clinical notes consistently indicated that she felt that her dizziness was improving, showed an improved DHI score (from 80 to 68).
Table 4.
Comparison of BBS, OLST, DHI, and PDI baseline (V0) and end point (V16) scores for all patients, ordered by baseline BBS score (n = 11)
| BBSa |
OLSTa |
PDIb |
DHIb |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | V 0 | V 16 | V0-V16 | V0 | V16 | V0-V16 | V0 | V16 | V0-V16 | V0 | V16 | V0-V16 |
| Chiropractic Group | ||||||||||||
| 29 | 34 | 50 | 16 | 3 | 2 | −1 | 39 | 29 | −10 | 80 | 68 | −12 |
| 47 | 39 | 40 | 1 | 2 | 1 | 1 | 36 | 38 | 2 | 8 | 40 | 32 |
| 95c | 42 | (37) | (−5) | 1 | (1) | (0) | 16 | (8) | (−8) | 48 | (48) | (0) |
| 11 | 42 | 52 | 10 | 2 | 1 | −1 | 14 | 2 | −12 | 12 | 6 | −6 |
| 67 | 44 | 53 | 9 | 2 | 4 | 2 | 1 | 2 | 1 | 4 | 12 | 8 |
| 01 | 50 | 53 | 3 | 8 | 13 | −5 | 41 | 29 | −12 | 42 | 44 | 2 |
| Exercise Group | ||||||||||||
| 85 | 41 | 41 | 0 | 2 | 2 | 0 | 0 | 1 | 1 | 24 | 26 | 2 |
| 71d | 42 | . | . | 2 | – | – | 56 | . | . | 68 | . | . |
| 79 | 44 | 47 | 3 | 2 | 1 | −1 | 7 | 7 | 0 | 6 | 6 | 0 |
| 56d | 45 | . | . | 1 | – | – | 41 | – | – | 38 | – | – |
| 27 | 47 | 49 | 2 | 5 | 5 | 0 | 16 | 12 | −4 | 10 | 2 | −8 |
Patients are listed in order of baseline BBS score (possible range, 0-56).
Higher scores indicate increased function.
Higher scores indicate decreased function (increased handicap).
This patient dropped out after V14; scores in parentheses are her V8 scores.
These patients dropped out after V0.
Adverse events
Two transient negative effects to treatment were recorded in the chiropractic group and none in the exercise group. One of these was mild and transient soreness in the back lasting less than 24 hours. The other was neck pain and headache that lasted approximately 24 hours and so was classified as an adverse event by our definition. The clinician applied an ice pack to the patient's neck; the symptoms resolved, and the patient completed the study with no further negative effects.
Discussion
When considering the results, it must be kept in mind that this was a feasibility study with a small sample; so it is inappropriate to make inferences about treatment efficacy for either treatment. Therefore, the discussion focuses on the study's process-oriented specific aims.
The first specific aim was to assess the utility of our recruitment methods. This study replicated the experience of similar studies at a different location in demonstrating that personal contact with senior centers and events is the most productive and economical recruitment method.9,11,12
The second specific aim was to assess compliance with treatment group assignment and study protocols. It appears from our results that assigning patients to a group they do not prefer may increase attrition, with 2 patients dropping out immediately when they were not assigned to their preferred group. Patients adhered well to the treatment schedule, with the only other dropout being due to medical necessity. For collecting medication information, it appeared that bringing medications in to be recorded by the coordinator was inefficient in terms of personnel use. Our next study therefore uses the method of mailing the medication list to patients for them to complete the list before the baseline visit, at which time the coordinator need only check it for legibility.
The third specific aim was to develop protocols for collecting accurate data on falls from study patients. Although use of a falls calendar has been recommended as the preferred method for collecting population-based data,20 we found that patients forgot to bring their calendars with them; and reminder phone calls would place an additional demand on staff time. Building a question about falls into the clinical notes form appears to be an effective way to collect falls data from patients who are currently under care, reducing the likelihood of recall bias that may be expected when the question is only asked at an exit interview.
The fourth specific aim was to assess the utility and responsiveness of the BBS and OLST in our sample population. Nine patients (all but 2, one in each group) had baseline BBS scores ≤45, indicating balance impaired enough to increase fall risk. Of these 9, 7 entered treatment; and of these, 4 increased their BBS score above the fall risk threshold by the end of the study. Overall score changes ranged from 0 to 16 points. This indicates that the BBS appears to be responsive over time and has some degree of variability. The OLST, on the other hand, did not appear to have a direct relationship to risk of falls demonstrated by the BBS because it was ≤5 seconds even in patients with BBS scores >45. Furthermore, the OLST did not demonstrate improvement on retest even when the BBS did. This has implications for future studies because we have to date used the OLST to screen patients for inclusion; it might be more meaningful, although more time consuming, to use the BBS score to determine eligibility.
In terms of administration of the BBS, it appears unavoidable that different assessors may need to conduct the test on the same patient at baseline and follow-up visits. It is also unavoidable that these assessors will be aware of whether the visit is baseline or follow-up. Consequently, for our next study, we have begun videotaping the BBS, with 2 trained, blinded assessors reviewing all tapes in random order.
The final specific aim was to collect preliminary information on the possible relationships of dizziness and chronic pain to poor balance. Four patients had relatively high scores at baseline for both the PDI and DHI, and all but one of these had a BBS score suggesting increased risk of falls. Four patients had high baseline scores for neither the PDI nor DHI, and all but one of these also had an increased risk for falls. Furthermore, although it is impossible to draw firm conclusions with posttest scores for only 9 patients, no consistent pattern was observed with respect to improvements, except that the DHI did not show a clinically meaningful improvement in any of the patients, even those who improved in terms of the BBS. This indicates that we need to collect more in-depth data on patients' experience of the interrelationships of balance, dizziness, and chronic pain in future studies. We have therefore instituted more detailed patient questionnaires and more detailed examination procedures for our next study.
In addition to the observations made related to the study's specific aims, it is also noteworthy that adverse events were rare and transient, even in this population of relatively frail elderly patients. This is not surprising because of the modified application of manipulative techniques, consistent with recommendations and very likely with the usual approach of practicing doctors of chiropractic to the treatment of elderly patients.10 Also of interest is the observation that functional improvement was seen at 4 weeks and did not usually improve appreciably further by 8 weeks.
Conclusion
Further investigation of the possible role of chiropractic care in reducing fall risk in this population appears feasible. Future studies are needed to explore the optimal frequency and duration of care required to reach and maintain the level of function indicating a decreased risk for falls. Currently, we have a study under way following for 1 year patients on different schedules of chiropractic care as well as a comparison group receiving only home exercise instruction.
Acknowledgment
The authors thank Jennifer Bedard, Emily Culver, and Judith Polipnick, DC, PhD, for their essential work in coordinating the processes of research and patient management. We would also like to thank Debbie McHenry, Tonia Wertman, Mekeia Johnson, and Billie Stremmel, who were generous with their time and assistance, enabling research activities to be integrated into the busy schedule of the Cleveland teaching clinic. We would also like to express our gratitude to Rickard Thomas, DC, and Lawrence Beem, DC, for their clinical expertise and dedication in serving as research clinicians. This study was funded by the Cleveland Chiropractic College, Kansas City, MO.
References
- 1.Tinetti M.E. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 2.Carroll N., Slattum P., Cox F. The cost of falls among the community-dwelling elderly. J Manag Care Pharm. 2005;11(4):307–316. doi: 10.18553/jmcp.2005.11.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention and Control . Centers for Disease Control and Prevention; Washington: 2006. A toolkit to prevent senior falls.http://www.cdc.gov/ncipc/pub-res/toolkit/toolkit.htm [monograph on the Internet] [cited 2006 Aug 26]. Available from: [Google Scholar]
- 4.Karlberg M., Magnusson M., Malmstrom E.M., Melander A., Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. 1996;77(9):874–882. doi: 10.1016/s0003-9993(96)90273-7. [DOI] [PubMed] [Google Scholar]
- 5.Bigos S, Bowyer O, Braen G, et al. Acute low back problems in adults. Clinical practice guideline no. 14. AHCPR publication no. 95-0642. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services. December 1994. Available from:http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.chapter.25870.
- 6.Meeker W., Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136(3):216–227. doi: 10.7326/0003-4819-136-3-200202050-00010. [DOI] [PubMed] [Google Scholar]
- 7.Heikkila H., Johansson M., Wenngren B.I. Effects of acupuncture, cervical manipulation and NSAID therapy on dizziness and impaired head repositioning of suspected cervical origin: a pilot study. Man Ther. 2000;5(3):151–157. doi: 10.1054/math.2000.0357. [DOI] [PubMed] [Google Scholar]
- 8.Reid S.A., Rivett D.A. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. 2005;10(1):4–13. doi: 10.1016/j.math.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Hawk C., Rupert R., Colonvega M., Hall S., Boyd J., Hyland J. Chiropractic care for older adults at risk for falls: a preliminary assessment. J Am Chiropr Assoc. 2005;42:10–18. [Google Scholar]
- 10.Bougie J. Geriatric practice–specific issues. In: Haldeman S., editor. Principles and practice of chiropractic. 3rd ed. McGraw-Hill; New York: 2005. pp. 1079–1098. [Google Scholar]
- 11.Hawk C., Rupert R., Colonvega M., Boyd J., Hall S. Comparison of bio-energetic synchronization technique and customary chiropractic care for older adults with chronic musculoskeletal pain. J Manipulative Physio Ther. 2006;29(7):540–549. doi: 10.1016/j.jmpt.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 12.Hawk C., Hyland J., Rupert R., Colonvega M., Hall S. Assessment of balance and risk for falls in a sample of community-dwelling adults aged 65 and older. Chiropr Osteopat. 2006;14(1):3–13. doi: 10.1186/1746-1340-14-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bogle-Thorbahn L., Newton R. Use of the Berg balance test to predict falls in elderly persons. Phys Ther June. 1996;76(6):576–583. doi: 10.1093/ptj/76.6.576. [DOI] [PubMed] [Google Scholar]
- 14.Lajoie Y., Gallagher S.P. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11–26. doi: 10.1016/s0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 15.Shumway-Cook A., Baldwin M., Polissar N.L., Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77(8):812–819. doi: 10.1093/ptj/77.8.812. [DOI] [PubMed] [Google Scholar]
- 16.Green H., McEntegart D., Byrom B., Ghani S., Shepherd S. Minimization in crossover trials with non-prognostic strata: theory and practical application. J Clin Pharm Ther. 2001;26(2):121–128. doi: 10.1046/j.1365-2710.2001.00332.x. [DOI] [PubMed] [Google Scholar]
- 17.Christensen M.G., Kollasch M.W., Ward R. Job analysis of chiropractic 2005: a project report, survey analysis, and summary of the practice of chiropractic within the United States. National Board of Chiropractic Examiners; Greeley (Colo): 2005. pp. 134–137. [Google Scholar]
- 18.National Institute on Aging . USDHHS; Washington: 2004. Exercise: a guide from the National Institute on Aging [monograph on the Internet]. NIH publication no. 01-4258.www.niapublications.org/exercisebook/ExerciseGuideComplete.pdf [cited Jul 2007]. Available from: [Google Scholar]
- 19.Whooley M.A., Avins A.L., Miranda J., Browner W.S. Case-finding instruments for depression. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lamb S.E., Jorstad-Stein E.C., Hauer K., Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 21.Whitney S.L., Poole J.L., Cass S.P. A review of balance instruments for older adults. Am J Occup Ther. 1998;52(8):666–671. doi: 10.5014/ajot.52.8.666. [DOI] [PubMed] [Google Scholar]
- 22.Harada N., Chiu V., Damron-Rodriguez J., Fowler E., Siu A., Reuben D.B. Screening for balance and mobility impairment in elderly individuals living in residential care facilities. Phys Ther. 1995;75(6):462–469. doi: 10.1093/ptj/75.6.462. [DOI] [PubMed] [Google Scholar]
- 23.Mount J., Bolton M., Cesari M., Guzzardo K., Tarsi J. Group balance skills class for people with chronic stroke: a case series. J Neurol Phys Ther. 2005;29(1):24–33. doi: 10.1097/01.npt.0000282259.81949.0e. [DOI] [PubMed] [Google Scholar]
- 24.Drusini A.G., Eleazer G.P., Caiazzo M. One-leg standing balance and functional status in an elderly community-dwelling population in northeast Italy. Aging Clin Exp Res. 2002;14(1):42–46. doi: 10.1007/BF03324416. [DOI] [PubMed] [Google Scholar]
- 25.Atwater S., Crowe T., Deitz J., Richardson P. Interrater and test-retest reliability of two pediatric balance tests. Phys Ther. 1990;(70):79–87. doi: 10.1093/ptj/70.2.79. [DOI] [PubMed] [Google Scholar]
- 26.Chibnall J.T., Tait R.C. The Pain Disability Index: factor structure and normative data. Arch Phys Med Rehabil. 1994;75(10):1082–1086. doi: 10.1016/0003-9993(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 27.Tait R.C., Chibnall J.T., Krause S. The Pain Disability Index: psychometric properties. Pain. 1990;40(2):171–182. doi: 10.1016/0304-3959(90)90068-O. [DOI] [PubMed] [Google Scholar]
- 28.Tait R.C., Pollard C.A., Margolis R.B., Duckro P.N., Krause S.J. The Pain Disability Index: psychometric and validity data. Arch Phys Med Rehabil. 1987;68(7):438–441. [PubMed] [Google Scholar]
- 29.Gronblad M., Jarvinen E., Hurri H., Hupli M., Karaharju E.O. Relationship of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) with three dynamic physical tests in a group of patients with chronic low-back and leg pain. Clin J Pain. 1994;10(3):197–203. doi: 10.1097/00002508-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Jacobson G.P., Newman C.W. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116(4):424–427. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 31.Clendaniel R. Outcome measures for assessment of treatment of the dizzy and balance disorder patient. Otolaryngol Clin North Am. 2000;33(3):519–533. doi: 10.1016/s0030-6665(05)70225-5. [DOI] [PubMed] [Google Scholar]