Abstract
Objective
The purpose of this project was to develop and test protocols for a randomized clinical trial of a combined therapeutic approach (thoracic spine and sacroiliac joint high-velocity, low-amplitude spinal manipulation [HVLA SM] + cervical spine postisometric relaxation) and cervical spine HVLA SM for patients with subacute or chronic neck pain.
Methods
Patients were recruited in the Quad Cities in Iowa and Illinois. After a baseline assessment visit, eligible patients were randomly assigned to cervical spine HVLA SM or to the combined therapeutic approach for 4 treatment visits over 2 weeks. Outcome assessments included the Neck Disability Index, visual analog scale, and posttreatment response questionnaire. Patient outcomes were not aggregated or compared by treatment group.
Results
It took approximately 8 months of planning, which included the development of forms and protocols, pretesting the forms, and training staff and clinicians in the standardized protocols. Twelve participants were screened, and 6 patients were enrolled and randomly allocated to care over a 6-week period. All patients completed 5 visits. Five of 6 patients had an improvement on the Neck Disability Index. On the visual analog scale, 2 patients improved at 2 weeks, whereas the other 4 got worse. Five patients completed the posttreatment response questionnaire; 2 of the 5 indicated they experienced discomfort or an unpleasant reaction from the study treatments.
Conclusions
Designing a successful feasibility randomized clinical trial requires considerable planning, development and pretesting of the forms and protocols, and training clinicians and staff for standardized protocols. Patients were willing to be randomized, follow treatment protocols, complete baseline and outcome assessments, and return 83% of the follow-up questionnaires.
Key indexing terms: Feasibility studies; Manipulation, Spinal; Neck pain; Musculoskeletal manipulations; Chiropractic
Introduction
Neck pain is a common musculoskeletal problem affecting up to 30% of adults in a given year.1,2 Similar to low back pain, neck pain can be a chronic and disabling problem. Up to 5% to 10% of adults will be disabled with chronic neck pain.1,2 Presently, there is no conclusive evidence for the effectiveness of high-velocity, low-amplitude spinal manipulation (HVLA SM) or other conservative manual therapy techniques for patients with acute, subacute, or chronic neck pain. A systematic review of the effectiveness of HVLA SM and mobilization for mechanical neck disorders revealed that HVLA SM and/or mobilization when done alone was not beneficial and that, when compared with one another, neither was superior.3
High-velocity, low-amplitude spinal manipulation is commonly used by manual therapists and doctors of chiropractic to treat spinal pain; but it is also commonly associated with minor transient adverse reactions such as local pain and stiffness, fatigue, or headaches. Observational studies have investigated the frequency and percentage of patients who experience these minor transient adverse reactions. A prospective, clinic-based survey of 102 Norwegian chiropractors reported that at least one minor adverse reaction was reported by 55% of the patients some time during the course of a maximum of 6 treatment visits.4 Studies from Sweden and Great Britain reported similar percentages of patients with minor adverse reactions.5,6 Recent randomized clinical trials (RCTs) of patients with neck pain have also reported minor adverse reactions in which HVLA SM and other manual therapies were used as the primary interventions.7,8 The frequencies reported in these RCTs ranged from 9% to 28% for the most common reaction, increased neck pain.
There is preliminary evidence that HVLA SM to the thoracic spine and muscle energy technique(s) to the cervical musculature may be helpful for neck pain. Cassidy et al9,10 found that there was no statistically significant difference in patients with neck pain between HVLA SM and a muscle energy technique in terms of pain intensity. Both treatment groups demonstrated decreased pain immediately after treatment. However, only one treatment was performed; and there was no follow-up assessment beyond immediate effects. In another study, it was found that thoracic spine HVLA SM reduced neck pain more than a sham thoracic HVLA SM when measured immediately after treatment.11 The results were statistically significant; but because the sample size was small and only immediate effects were measured, the results need to be interpreted with caution. We believe that there is potential for muscle energy techniques and thoracic spine HVLA SM for relieving neck pain.
Although there are no published clinical studies that suggest sacroiliac HVLA SM is helpful for neck pain, there is anecdotal evidence to suggest that a biomechanical relationship exists between the spinal regions caudal to the cervical spine and the cervical spine.12,13 Because of the scarcity of studies investigating the muscle energy technique—postisometric relaxation (PIR), and thoracic and sacroiliac HVLA SM for neck pain—this study looked at a combined therapeutic approach using thoracic spine and sacroiliac HVLA SM and PIR in patients with subacute or chronic neck pain. A long-term goal is to identify specific types of combined therapeutic approaches that are most effective in reducing neck pain and disability and that result in a low percentage of minor, transient adverse reactions.
Because RCTs are expensive and involve human participants, feasibility studies are recommended to test a study's protocols. Feasibility studies are especially important for new investigators and for investigators who are recruiting participants in a particular geographic area for the first time. The purpose of this study was to develop and test protocols for an RCT of a combined therapeutic approach and cervical spine HVLA SM for patients with subacute or chronic neck pain. Protocols tested included patient recruitment, telephone and face-to-face screening interviews, informed consent, physical examination, enrollment, and treatment procedures for HVLA SM as well as for the PIR technique to the cervical spine musculature.
Methods
It took approximately 7 months to design and pretest the study protocols and forms. An additional 3 weeks was needed to train 4 research staff and 2 clinicians for eligibility screening protocols, patient flow and administration of self-report questionnaires, and examination and treatment protocols. All members of the study team were trained with standardized protocols before patient recruitment.
Our target enrollment for this project was 6 patients with subacute or chronic neck pain. Patients were recruited using study fliers, a classified newspaper ad, and by word of mouth in Davenport, IA, and the surrounding Quad Cities in Iowa and Illinois. Patients were also recruited from a list of ineligible patients for a low back pain study at the Palmer Center for Chiropractic Research (PCCR). Initial screening was conducted with a telephone interview. Eligible participants were invited for a baseline visit within 7 days of initial screening. The baseline visit included self-report demographic and health history questionnaires, an interview to assess eligibility and administer informed consent, a physical examination, and plain film radiographs if needed to determine eligibility. Eligible participants were scheduled for a second visit where they were randomly assigned to 1 of 2 treatment groups and received their first treatment. The interview process, informed consent, and study orientation were conducted by the first author as partial fulfillment of his master's degree. This study was approved by the Palmer College of Chiropractic Institutional Review Board and met the ethical requirements for human participants.
Inclusion and exclusion criteria
Patients were eligible for the study if they were 20 to 65 years old and had a primary complaint of mechanical neck pain for at least 4 weeks. Patients with mechanical neck pain were defined as those who had a Quebec Task Force14 classification of “one” or “two.” Patients who had a secondary complaint of headache were considered for inclusion as long as they had a primary complaint of neck pain.
Potential participants were excluded if they (1) had neck pain resulting from inflammatory joint disease, infection, tumor, or fracture; (2) had comorbid disease that would contraindicate HVLA SM (eg, severe osteoporosis of spine); (3) were currently receiving treatment of neck pain by other health care providers; (4) had a previous history of stroke, or a diagnosis of a bleeding disorder, or were currently undergoing anticoagulation treatment; (5) had a grade 3 or 4 on the Quebec Task Force classification system for cervical spine disorders; (6) were pregnant; (7) had surgery to spine; (8) did not have any biomechanical joint dysfunction (as shown by palpation); (9) were unable to read and speak English; or (10) showed evidence of narcotic or other drug abuse. Potential participants were also excluded if they had ongoing personal injury or workers compensation related to neck or back pain, or were currently seeking or receiving disability for neck pain or low back pain.
Treatment assignment
At the second visit, eligible participants who gave consent to participate were randomly assigned to 1 of 2 treatment groups: (a) combined therapeutic approach or (b) cervical spine HVLA SM. The sequence of assignment was a predetermined randomization scheme (using a random number table) in a 1:1 allocation ratio. All participants were randomized by the use of sealed, opaque, sequentially numbered envelopes.
Frequency and duration of treatment
All participants were scheduled for 4 treatment visits over a 2-week period. An a priori decision was made to classify participants as noncompliers if they did not complete the active care regimen within 14 calendar days.
Treatment protocols
Two experienced, licensed doctors of chiropractic from PCCR were the treating doctors. One of the doctors, a graduate of Northwestern College of Chiropractic, had 15 years of clinical experience, whereas the other, a graduate of Palmer College of Chiropractic, had 4 years of experience. The HVLA SM was administered at each visit to the vertebral levels that were found to be hypomobile according to diagnostic manual palpation techniques.15 The number of levels adjusted at each visit was up to the discretion of the treating doctor. The treating doctor recorded the vertebral levels treated with its corresponding restriction listing as well as whether a release was produced. In addition, patients were asked about the occurrence of any cointerventions (eg, non–study-related medical/chiropractic treatment) or any new trauma during the course of the treatment schedule to account for any confounding variables. It is important to test the feasibility of incorporating questions about cointerventions and new trauma into each doctor/patient visit because the existence of any cointerventions in a large powered study (if conducted) can misrepresent the results and falsely influence the reader if not accounted for.
Cervical spine HVLA SM treatment group
The cervical spine group only received HVLA SM to C0 through C7 vertebral levels, at the discretion of the doctor.
Combined therapeutic approach group
The combined therapeutic approach group received HVLA SM to T1 through T12 vertebral levels and the sacroiliac joints, at the discretion of the doctor. The muscle energy technique, PIR, was also administered at each treatment visit by the treating doctor according to the Lewit procedure.16 The muscle or muscle group found to have the most hypertonicity by passive range of motion assessment and the quality of end feel was chosen to be the muscle or muscle group treated. This procedure was done in 2 sets of 3 repetitions. The muscle or muscle groups that the doctor was able to assess and treat included the left or right scalene muscles (anterior, middle, and posterior), the left or right upper trapezius, the left or right levator scapula, and the suboccipital muscles. These muscles were chosen because they are thought to be overactive or shortened in patients.16
Data collection
Data collection at baseline included medical history, onset of neck pain, level of neck disability and pain, and physical signs and symptoms. The physical signs and symptoms were obtained by a standard physical examination performed on all eligible participants by a study clinician. Plain film radiographic studies were taken only if necessary to assess eligibility.
Neck Disability Index
The Neck Disability Index (NDI) was used to assess the level of neck disability. The NDI is a 10-item questionnaire that asks patients to rate how their neck pain is affected by activities of daily living. The total NDI scores were converted to a percentage score (0-100); and from that, a change score was calculated (from baseline to 2 weeks). For those instances where there was one missing value to an item, the total score was based on a percentage score of 90. The NDI has been found to have good reliability as well as good construct and concurrent validity in an ambulatory clinic population.17 It has also been shown to possess stable psychometric properties (evidenced by high internal consistency; α = .92) and is thought to provide an objective means of assessing the disability of patients with neck pain.18
Visual analog scale
The visual analog scale (VAS) was used to assess the intensity of the patient's pain. We used a continuous scale that asked patients to think about their neck pain during the past week and to rate their pain level by marking on a 100-mm line, anchored with “no pain” and the “worst pain you have ever felt.” This is a well-accepted method of documenting pain intensity levels. Studies have shown that the VAS has high reliability.19-22 Concurrent validity studies with other measures of pain and loss of function were also high.23
Sociodemographic data
Sociodemographic variables included age, sex, ethnicity, race, education level, and marital status.
Posttreatment response questionnaire
The posttreatment response questionnaire (PTRQ) inquires about a patient's incidence, type, onset, duration, and dysfunction of any minor adverse reactions that may have occurred from treatment. This instrument is based on a similar one used by Hurwitz et al.24 It asks 5 main questions. The first question is, “Did you experience any discomfort or unpleasant reaction from chiropractic care during the past two weeks?” It asks about the type of discomfort and lists a group of the more common minor adverse reactions that have been reported in previous clinical trials and observational studies. Afterward, for each reported symptom, the questionnaire asks the patient to rate the following: the level of discomfort they experienced on a 0 to 10 numerical rating scale (0 = no discomfort and 10 = unbearable discomfort); how long after treatment the discomfort started (<30 minutes, 30 minutes to 4 hours, 4 hours to 24 hours, and>24 hours); how long the discomfort lasted (<10 minutes, 10 minutes to 1 hour, 1 hour to 24 hours, and>24 hours); and how much their discomfort affected normal daily activities at home or at work(“not at all,” “a little,” and “a lot”).
The NDI and VAS were administered at baseline and at the participants' last visit. The PTRQ was mailed to each participant within 24 hours of completing the last visit.
Data analysis was performed using SPSS PC for Windows, version 13.0 (SPSS Inc, Chicago, IL). Descriptive statistics were performed on baseline characteristics and outcome variables. Follow-up data were reported for each of the 6 patients and were not aggregated. No formal hypothesis testing between treatment groups was performed because of the small sample size and because the primary goal of this study was to develop and assess study protocols.
Results
Pretesting the forms before the study began was valuable to ensure the items and patient instructions were clear and understandable and to minimize missing data from participants. The baseline assessment forms went through 2 rounds of iterative feedback before recruitment began.
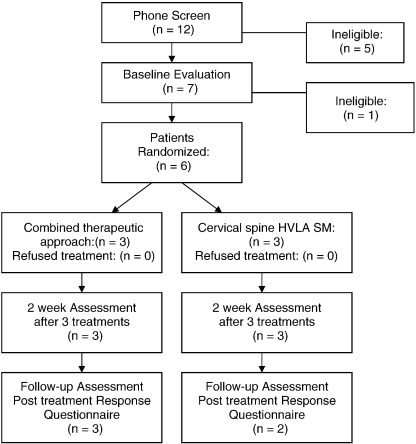
Twelve individuals were recruited from a classified newspaper ad (n = 4), a list of ineligible participants from an ongoing low back study (n = 5), and by word of mouth/study flier (n = 3). Of these, 5 were ineligible because of no current neck pain (n = 2), onset of neck pain less than 1 month (n = 2), and active care for neck pain (n = 1) (Fig 1). The study chiropractors performed 7 physical examinations. One patient was ineligible at the physical examination because of dizziness reproduced during a provocative vertebral-basilar artery insufficiency test (we excluded this patient as a precautionary measure because of the possible complications to HVLA SM). Six participants were enrolled in the study over a period of 6 weeks. All participants attended 5 visits. Five patients were female (Table 1). The average age was 48 years, all were white, 4 had some college or a college degree, and 5 had neck pain with greater than 6 months' duration. The combined therapeutic approach group had slightly higher disability scores on the NDI than the cervical spine group at baseline.
Fig 1.
Flowchart of study visits, recruitment, enrollment, and follow-up.
Table 1.
Baseline characteristics: frequencies
| Characteristic | CTA Group (n = 3) | Cervical HVLA Group (n = 3) | All (n = 6) |
|---|---|---|---|
| Age (y)a | 42 (12) | 54 (10) | 48 (12) |
| Sex: Female | 3 | 2 | 5 |
| Race/Ethnicity: White/Non-Hispanic | 3 | 3 | 6 |
| Marital Status: Married | 1 | 2 | 3 |
| Education: Some College or College Degree | 2 | 2 | 4 |
| Neck Pain Onset >6 mo | 2 | 3 | 5 |
| NDI (0-100)b | 34.0 (12-34) | 24.0 (20-38) | 29.0 (12-38) |
| VAS (0-100 mm)b | 35.0 (9-36) | 29.0 (27-50) | 32.0 (9-50) |
CTA, Combined therapeutic approach.
Mean (SD).
Median (range).
Outcome scores for each patient are provided in Table 2. Five of the 6 patients had an improvement on the NDI, and 1 patient had no change. On the VAS, 2 patients improved, whereas the other 4 worsened.
Table 2.
Outcomes by patient
| Treatment Group | Patient | NDI (%) Baselinea | NDI (%) Week 2a | NDI Change Score | VAS (mm) Baselinea | VAS (mm) Week 2a | VAS Change Score |
|---|---|---|---|---|---|---|---|
| Csp HVLA | 1 | 38 | 20 | +18 | 50 | 27 | +23 |
| 2 | 24 | 12 | +12 | 29 | 54 | −25 | |
| 3 | 20 | 20 | 0 | 27 | 9 | +18 | |
| CTA | 1 | 34 | 28 | +6 | 36 | 77 | −41 |
| 2 | 12 | 11 | +1 | 9 | 10 | −1 | |
| 3 | 34 | 26 | +8 | 35 | 65 | −30 |
Change score = baseline to 2 weeks. Plus sign indicates improvement; minus sign indicates worsening effect.
Csp, Cervical spine.
Scale of 0 to 100.
One patient was contacted twice to complete and return the PTRQ. After 2 weeks, 5 of the 6 patients returned the questionnaire. Of those 5 patients, 2 indicated that they experienced discomfort or an unpleasant reaction from the chiropractic care they received in the study during the past 2 weeks. One of the patients in the cervical spine HVLA SM group experienced increased neck pain/stiffness and dizziness/imbalance that were rated mild in severity. This patient's onset of complaints began less than 30 minutes after the treatment, lasted less than 10 minutes in duration, and did not affect the patient's normal daily activities. The other patient who had an unpleasant reaction from treatment was in the combined therapeutic approach group. This patient experienced severe neck pain/stiffness, with the onset of symptoms more than 24 hours after the treatment and a duration that lasted more than 24 hours; and the adverse reaction affected the patient's daily activities a lot. The information that the PTRQ captures was designed as an outcome measure and was not part of the adverse events grading and reporting protocols. Because there were no adverse events reported to the doctors when the patients were probed during the treatment visits, we can only speculate that the 2 minor adverse events to treatment occurred on the patients' last visit.
According to the exit interviews, patients were satisfied with the level of service and attention they received. One patient wished the study duration was longer, and another patient wished he or she had HVLA SM to the entire spine.
Discussion
Recruitment, enrollment, and follow-up of patients were completed over 10 weeks; and as a result, the duration of the treatment schedule was short and the sample size was small. Although the duration of treatment schedule and sample size were feasible for the purposes of completing the project during a master's program, the patient-related data reported in the results must be interpreted with caution. A sample size of 6 patients is not large enough for any type of formal statistical testing of within- or between-group differences. This sample size is also not large enough to assess the feasibility of a full-scale RCT. There was no budget for patient recruitment, and we did not establish a priori criteria for estimating effective recruitment strategies. Six weeks of recruitment was necessary to enroll 6 patients. Word of mouth, a no-cost classified advertisement in a weekly newspaper, and contacting patients who were ineligible for a concurrent low back pain study will be insufficient to conduct a full-scale RCT; the latter method may also lead to selection bias.
A limitation to this study was that a priori criteria for estimating effective recruitment strategies were not established. In addition, this small feasibility study was not designed to determine effect sizes; and no a priori statistical comparisons were planned. All 3 of these issues need to be addressed in a larger pilot study before planning a large-scale RCT.
The 2-week treatment duration used in this study is not representative of manual therapy practice guidelines for patients with subacute or chronic neck pain. Longer treatment duration of at least 4 to 6 weeks is more typical for patients with subacute or chronic spinal conditions. Patients may have benefited from a longer treatment period because 5 of the 6 patients had an onset of neck pain greater than 6 months at the time they enrolled in the study.
The study protocols and forms used in this study were efficient and effective in that they allowed us to reach our enrollment and follow-up goals. Pretesting the forms was essential to ensure that the items and patient instructions were clear and understandable and to minimize missing data. All forms were fully and appropriately completed by patients during the study, with the exception of the PTRQ. Two patients did not complete the questionnaire according to instructions. One patient did not answer the first question (“Did you experience any discomfort or unpleasant reaction from chiropractic care during the past two weeks?”) and then circled “0” for the severity of each of the listed symptoms. We interpreted this response to mean the patient did not have discomfort or unpleasant reaction from care. The other patient checked “No” to the first question and then marked that he or she had mild neck pain and dizziness/imbalance. We interpreted this response to mean that the patient meant to check “Yes” to question 1 and did have discomfort or unpleasant reaction from care. Because of the inconsistent responses from patients on this form, we believe this form needs to be improved to ensure that the instructions are understandable. The integrity of the data depends on the clarity of study forms.
Another limitation of this study was that the PIR technique was performed by clinicians with limited experience with this technique and with a relatively short training period. Although the clinicians were trained in the application of the technique for several hours over 2 weeks, this training is not equivalent to a clinician who uses this technique on a regular basis. This lack of experience with delivering PIR may explain why the combined therapeutic approach group experienced the results they did. On the other hand, this combined therapeutic approach may not be helpful for patients with subacute or chronic neck pain. Because HVLA SM in combination with PIR is common in practice, well-designed full-scale trials are needed to determine the efficacy of this care. If deemed efficacious, then the next step would be a practice-based or pragmatic trial to determine effectiveness.
Conclusion
Designing even a small RCT is challenging and involves many personnel. Careful planning and teamwork are essential for the design and successful conduct of an RCT. The study protocols and forms used in this project were efficient, collected comprehensive data, and allowed us to reach our goals. This study provided us with valuable experience in the conduct of a feasibility study of an RCT. The integrity of clinical trials is dependent on methods or protocols. It is more advantageous to spend the time and energy to get the methods “right” (standardized) during the planning stages than to figure out how the methods were implemented after the study is completed. It is important for new investigators to appreciate the benefits of careful planning and design of a study's protocols before the start of a study. A study with a more comprehensive recruitment effort is still needed to determine the feasibility of a larger trial for patients with neck pain at PCCR, but PCCR now has the protocols and data collection processes in place to conduct such a trial.
Acknowledgment
The authors would like to thank the following people for making this study successful: Drs Cynthia Long and Dana Lawrence for assisting in the design and serving on the advisory committee for the first author, Dr Robert Rowell for assisting in the development of forms and protocols and serving as a clinician, Dr Steve Rylander for being a study clinician, Therese Devlin, Tammi White, Lori Byrd, and Dr Andrea Haan for assisting in the implementation of the study and the recruitment of participants. We would also like to thank Lance Corber for the data management and development of data sets, Lynne Carber for programming the Web scheduler to incorporate this project among several funded trials that were ongoing at PCCR, and Dr Cheryl Hawk for her critical review and insightful suggestions to the final manuscript.
Footnotes
The authors declare that they have no competing interests. This study was supported in part by a grant from the National Institutes of Health (K30-AT-00977-04) and was conducted in a facility constructed with support from a Research Facilities Improvement Grant (C06 RR15433) from the National Center for Research Resources, National Institutes of Health.
References
- 1.Cote P., Cassidy J.D., Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 1998;23(15):1689–1698. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Bovim G., Schrader H., Sand T. Neck pain in the general population. Spine. 1994;19(12):1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Gross A.R., Hoving J.L., Haines T.A., Goldsmith C.H., Kay T., Aker P. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine. 2004;29(14):1541–1548. doi: 10.1097/01.brs.0000131218.35875.ed. [DOI] [PubMed] [Google Scholar]
- 4.Senstad O., Leboeuf-Yde C., Borchgrevink C. Frequency and characteristics of side effects of spinal manipulative therapy. Spine. 1997;22(4):435–440. doi: 10.1097/00007632-199702150-00017. [DOI] [PubMed] [Google Scholar]
- 5.Leboeuf-Yde C., Hennius B., Rudberg E., Leufvenmark P., Thunman M. Side effects of chiropractic treatment: a prospective study. J Manipulative Physiol Ther. 1997;(8):511–515. [PubMed] [Google Scholar]
- 6.Barrett A.J., Breen A.C. Adverse effects of spinal manipulation. J R Soc Med. 2000;93(5):258–259. doi: 10.1177/014107680009300511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bronfort G., Evans R., Nelson B., Aker P.D., Goldsmith C.H., Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26(7):788–797. doi: 10.1097/00007632-200104010-00020. [DOI] [PubMed] [Google Scholar]
- 8.Hoving J.L., Koes B.W., de Vet H.C. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136(10):713–722. doi: 10.7326/0003-4819-136-10-200205210-00006. [DOI] [PubMed] [Google Scholar]
- 9.Cassidy J.D., Lopes A.A., Yong-Hing K. The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: a randomized controlled trial. J Manipulative Physiol Ther. 1992;15(9):570–575. [PubMed] [Google Scholar]
- 10.Cassidy J.D., Lopes A.A., Yong-Hing K. Re: the immediate effect of manipulation vs. mobilization on pain and range of motion in the cervical spine: a randomized controlled trial (letter) J Manipulative Physiol Ther. 1993;16(4):279–280. [PubMed] [Google Scholar]
- 11.Cleland J.A., Childs J.D., McRae M., Palmer J.A., Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10(2):127–135. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Greenman PE. Principles of manual medicine. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1996. p. 175, 205-7.
- 13.Porterfield J.A., DeRosa C. Mechanical neck pain: perspectives in functional anatomy. W.B. Saunders; Philadelphia: 1995. p. 3. [Google Scholar]
- 14.Spitzer W.O., Skovron M.L., Salmi L.R., Cassidy J.D., Duranceau J., Suissa S. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. 1995;20(8 Suppl):1S–73S. [PubMed] [Google Scholar]
- 15.Peterson D.H., Bergman T.F. Chiropractic technique: principles and procedures. Churchill Livingstone; Philadelphia: 1993. Joint assessment principles and procedures; pp. 39–95. [Google Scholar]
- 16.Chaitow L. An introduction to muscle energy techniques. In: Chaitow L., editor. Muscle energy techniques. 3rd ed. Churchill Livingstone; Edinburgh: 2006. pp. 13–57. [Google Scholar]
- 17.Vernon H.T., Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409. [PubMed] [Google Scholar]
- 18.Hains F., Waalen J., Mior S. Psychometric properties of the neck disability index. J Manipulative Physiol Ther. 1998;21(2):75–80. [PubMed] [Google Scholar]
- 19.Huskisson E.C. Measurement of pain. Lancet. 1974;2:127. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 20.Huskisson E.C. Measurement of pain. J Rheumatol. 1982;9:768. [PubMed] [Google Scholar]
- 21.Huskisson E.C. Visual analogue scales. In: Melzack R, editor. Pain measurement and assessment. Raven Press; New York: 1983. [Google Scholar]
- 22.Dixon J.S., Bird H.A. Reproducibility along a 10-cm vertical visual analogue scale. Ann Rheum Dis. 1981;40:87. doi: 10.1136/ard.40.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott J., Huskisson E.C. Vertical or horizontal visual analogue scales. Ann Rheum Dis. 1979;38:560. doi: 10.1136/ard.38.6.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hurwitz E.L., Morgenstern H., Vassilaki M., Chiang L.M. Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA neck pain study. Spine. 2005;30(13):1477–1484. doi: 10.1097/01.brs.0000167821.39373.c1. [DOI] [PubMed] [Google Scholar]