Abstract
INTRODUCTION
This observational study was carried out to establish how surgeons performing laparoscopic cholecystectomy currently deal with the issue of spilled gallstones.
MATERIALS AND METHODS
A questionnaire was circulated amongst laparoscopic surgeons attending the annual conference of the Association of Laparoscopic Surgery of Great Britain and Ireland in November 2006.
RESULTS
Eighty-two surgeons completed the questionnaire. Only half of surgeons inform patients when gallstones are spilled. Less than 30% of surgeons inform general practitioners (GPs) of this complication, when it occurs. Less than a quarter of surgeons include this information in the consent literature provided to patients.
CONCLUSIONS
We recommend that trusts review their policy towards spilled stones either by local audit or adopt the guidance given by the UK Healthcare Commission. While some surgeons feel informing patients and GPs may unnecessarily heighten anxiety from an uncommon complication, our review of the literature suggests this position is not tenable in the current medicolegal climate.
Keywords: Laparoscopic cholecystectomy, Spilled gallstones
A recent cluster of two patients with complications of spilled gallstones following laparoscopic cholecystectomies more than 2 years previously and a complaint from one patient, provoked renewed interest in our department as to the management of gallstones spillage. The UK Healthcare Commission reviewed the case involving the complaint and wrote to our department. The letter required that we institute a system that, when gallstones were spilled at laparoscopic cholecystectomy: (i) the patient was informed; (ii) the general practitioner (GP) was notified; and (iii) information relating to this complication be mentioned in our consent form.
The purpose of this, the Healthcare Commission stated, was to raise awareness and facilitate prompt diagnosis of possible complications related to spilled and non-retrieved gallstones. This represented a deviation from current unit policy. This observational study was carried out to establish how surgeons performing laparoscopic cholecystectomy currently deal with the issue of spilled gallstones.
Materials and Methods
We carried out a survey of laparoscopic surgeons attending the annual conference of the Association of Laparoscopic Surgery (ALS) of Great Britain and Ireland in November 2006. Eighty-two surgeons completed the following questionnaire:
During a laparoscopic cholecystectomy, if stones are spilled and not retrieved, do you convert to open?
If spilled stones are not retrieved, do you inform the patient?
Do you inform the GP?
Do you mention, in your consent form, the risk of leaving spilled stones in the abdomen?
Results
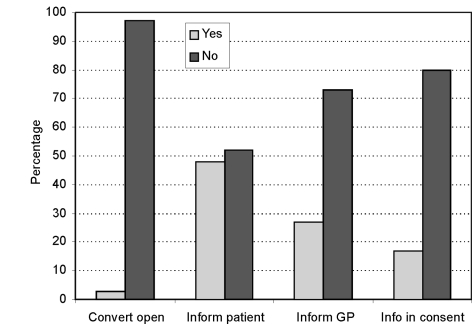
The results of the survey are summarised in Table 1 and Figure 1. Only half of surgeons inform patients when gallstones are spilled. Less than 30% of surgeons inform GPs of this complication, when it occurs. Less than a fifth of surgeons include this information in the consent literature provided to patients.
Table 1.
Survey results
| Yes | No | |
|---|---|---|
| Convert to open | 3 | 97 |
| Inform patient | 48 | 52 |
| Inform GP | 27 | 73 |
| Information in consent form | 17 | 80 |
Results are expressed as percentages.
Figure 1.
Survey results.
Discussion
Perforation of the gallbladder occurs frequently (10–40%) during laparoscopic cholecystectomy.1 The incidence of gallstone spillage is much less frequent, but the true incidence is not well known. These spilled stones should normally be retrieved during the procedure, but inability to retrieve them is an accepted situation.1,2 The rate of complications occurring from these unretrieved stones is about 0.3% of patients.3 Complications can, however, be serious and include intra-abdominal abscess formation, obstruction or fistulation (Fig. 2).4
Figure 2.
Retrieval of spilled stones from left buttock, 2 years after laparoscopic cholecystectomy.
There is good evidence to suggest that conversion at laparoscopic cholecystectomy to retrieve spilled stones is unnecessary,5 though our survey showed that 3% of surgeons suggested they would do this.
Though complications of spilled gallstones are low, they can occur many years after surgery. The Healthcare Commission and literature reviews1,3 have suggested a gold standard approach (see above) for treatment of this situation in the absence of national guidelines.
Our survey of laparoscopic surgeons showed only half the surgeons (who we presume as ALS members are most aware of complications related to laparoscopic operations) told their patients. Though this is only a small proportion of the estimated 1200–1500 surgeons performing laparoscopic cholecystectomies nationally.
Conclusions
We recommend that trusts review their policy towards spilled stones either by local audit or adopt the guidance given to us by the Healthcare Commission. While some surgeons feel informing patients and GPs may unnecessarily heighten anxiety from an uncommon complication, our review of the literature suggests this position is not tenable in the current medicolegal climate.
References
- 1.Woodfield JC, Rodgers M, Windsor JA. Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. Surg Endosc. 2004;18:1200–7. doi: 10.1007/s00464-003-8260-4. [DOI] [PubMed] [Google Scholar]
- 2.Manukyan MN, Demirkalem P, Gulluoglu BM, Tunet D, Yegen C, Yalin R, et al. Retained abdominal gallstones during laparoscopic cholecystectomy. Am J Surg. 2005;189:450–2. doi: 10.1016/j.amjsurg.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 3.Diez J, Arozamena C, Gutierrez L, Bracco J, Mon A, Sanchez Almeyra R, et al. Lost stones during laparoscopic cholecystectomy. HPB Surg. 1998;11:105–8. doi: 10.1155/1998/95874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sathesh-Kumar T, Saklani AP, Vinayagam R, Blackett RL. Spilled gall stones during laparoscopic cholecystectomy: a review of the literature. Postgrad Med J. 2004;80:77–9. doi: 10.1136/pmj.2003.006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Memon MA, Deeik RK, Maffi TR, Fitzgibbons RJ., Jr The outcome of unretrieved gallstones in the peritoneal cavity during laparoscopic cholecystectomy. A prospective analysis. Surg Endosc. 1999;13:848–57. doi: 10.1007/s004649901118. [DOI] [PubMed] [Google Scholar]