Abstract
INTRODUCTION
It is increasingly important for surgeons to monitor the outcome of their practice for the purpose of audit. The main difficulty has been the lack of appropriate methods of assessing outcome. Outcome has traditionally been assessed by clinical means which can be inaccurate, irreproducible and subject to surgeon bias. In addition, the perspective of the patient and surgeon may differ with respect to outcome and interest has grown in patient-based scoring systems. The Oxford Shoulder Score (OSS) is one such patient-based scoring system. The main aim of this study was to assess whether a patient-based questionnaire, in this case the OSS, could be effectively used to audit outcome from shoulder surgery. A secondary aim was to assess the value of gathering outcome information by post.
PATIENTS AND METHODS
A total of 24 patients (14 male; median age 59 years; age range, 43–73 years) who had completed a pre-operative OSS questionnaire and had undergone rotator cuff repair were included in the study. Participants were assessed postoperatively at regular intervals using the OSS at hospital visits and by postal questionnaire.
RESULTS
The completion level for the OSS was 97% and the response rate to the postal questionnaire was 96%. At 3 months' post-surgery, 21 of 24 patients had improved; at final review (16–37 months), 23 patients had improved following surgery. The OSS was observed to be a robust tool for the quantitative assessment and tracking of patient outcomes after surgery.
CONCLUSIONS
This study shows the value of using a postal questionnaire to follow-up patients after surgery and demonstrates the successful use of a patient-based questionnaire to audit the outcome from shoulder surgery.
Keywords: Oxford Shoulder Score, Outcome assessment (healthcare), Shoulder, Surgery
Shoulder pain is a significant problem. Its prevalence is reported to be around 7% of the population, rising to approximately 20% in individuals over 70 years of age.1–5 It usually arises from disorders of peri-articular soft tissue, especially the rotator cuff.5,6
Shoulder pain is responsible for a significant proportion of visits to general practitioners7,8 and hospital specialists.9,10 Some patients will require surgery and, as a result, there are important socio-economic implications because of morbidity and time lost from work.11
It is increasingly important for surgeons to record the outcome from their practice for the purposes of audit; however, the main problem has been the lack of appropriate assessment methods.12 Several scoring methods have been developed to evaluate the outcome of the orthopaedic management of shoulder conditions but these derive from clinical and radiological data and are dependent on the surgeons' judgement.13
It is increasingly apparent that clinical assessments of key aspects of outcome are often inaccurate and not reproducible.14,15 In addition, the concerns and priorities of the patient and surgeon may differ.16 Methods are required which elicit the patient's perception of the outcome.17 This has led to increased interest in patient-based assessments.
Research has shown that reports from patients can be reliable, valid and sensitive to clinical change.18 The evidence also suggests that patient-based questionnaires are a useful adjunct to clinical assessment in shoulder disorders.12 Where a questionnaire is used, it should be short, practical, reliable, valid and sensitive to clinical change.
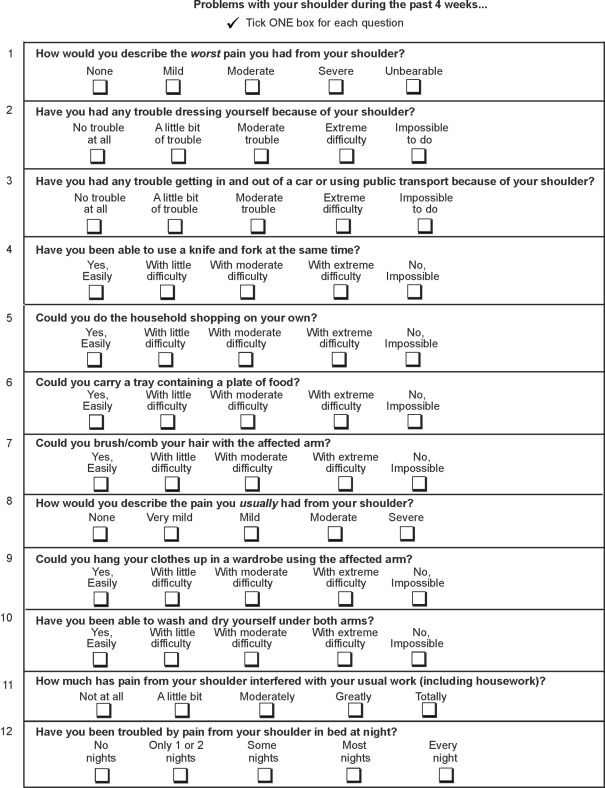
The Oxford Shoulder Score (OSS) is a patient-based questionnaire used to assess shoulder pain. It is a condition-specific questionnaire, completed unaided by the patient. It contains a mixture of pain and function questions, derived from over 200 initial question models based on in-depth patient and clinician interviews. It has been validated against clinician-based and general health status measures.5,12 The OSS is sensitive to clinical change, is simple to complete and has proved to be consistently reliable in determining the outcome from shoulder surgery.5,12
The aim of this study was to assess whether a patient-based questionnaire can be effectively used to audit shoulder surgery. In particular we wished to evaluate whether the surgeon can use a patient-based questionnaire to track the outcome over time of an individual, or a group, undergoing a particular surgical procedure.
In addition to selecting an appropriate measure to audit outcome, the surgeon needs also consider how the information is to be gathered. It may be costly to provide extra clinic appointments for audit purposes, and patients are often unable or unwilling to attend for assessment on multiple occasions after treatment.
One solution is the use of a postal questionnaire. Administration of questionnaires is usually simpler to organise than additional clinics and the response rate higher than attendance at supplementary clinics.19 A good response avoids additional clinic costs and minimises inconvenience to both surgeon and patient. A further aim, therefore, was to assess the response rate and quality of completion of a patient-based postal questionnaire.
Patients and Methods
Patients attending shoulder clinics, pre-admission clinics and for day-case surgery within our unit were invited to complete an OSS, as part of routine clinical practice.
The OSS consists of 12 questions each with five response options (Appendix 1). Each option carries a score from 1 (best) to 5 (worst). The scores from each question combine to give a total score with a range from 12 (best, no pain or functional impairment) to 60 (worst).
In addition, the patients completed a basic information form which elicited details about their age, gender, employment and carer status. Younger patients and those who are in employment or a full time carer may have higher expectations and require a greater level of function following surgery. They may be expected to be less satisfied following surgery.
Whether the rotator cuff tear affected the dominant shoulder was also recorded. Where the dominant shoulder is affected a patient's function may be more limited, particularly with respect to activities of daily living.
Information as to whether their condition was of sudden onset and related to an injury was also gathered.
Where a claim for legal compensation existed this was also recorded, as this group tend to report worse results after surgery.20
We recorded the size of the cuff tear found at the time of surgery, another factor potentially associated with outcome. Although a matter of debate, a poorer prognosis may be expected with a larger rotator cuff tear even where surgery was performed.21,22
This pilot study included all 24 patients who had completed a questionnaire and had undergone surgery to repair a rotator cuff tear between May 2002 and October 2003. Patients attended clinics at various time points during their care and, therefore, the sample included patients who had been followed prospectively.
Of the 24 patients who underwent rotator cuff surgery all had an arthroscopy initially, followed by open surgery in 23 patients and arthroscopic cuff repair in one patient. Of those 23 who had open surgery, one patient had an irreparable cuff tear and two patients had tears that were only amenable to partial repair. A good repair was achieved in the remainder.
In addition to rotator cuff surgery, 23 had a sub-acromial decompression. Sixteen were performed arthroscopically, six open and one both arthroscopic and open. In one patient, no abnormality of the acromion was found at arthroscopy and so acromioplasty was not performed.
To evaluate the postal aspect of the study and to gather further follow-up data on individual patients, a copy of the OSS was posted to all 24 patients. Prospective follow-up data were, therefore, gathered up to a maximum of 3.1 years postoperatively (minimum follow-up 16 months). Patients were asked to return a blank copy if they did not wish to participate. If not returned, patients were contacted once by telephone.
Results
Participant information is shown in Table 1. Table 2 contains shoulder specific details for the cohort. A total of 119 questionnaires were completed and 97% (116) of these were completed in full. Questionnaires with missing data (n = 3) were excluded from subsequent analysis. Where more than one pre-operative questionnaire was completed, the score closest to surgery was analysed.
Table 1.
Participant information
| Gender | |
| Male | 14 (58.3%) |
| Female | 10 (41.7%) |
| Age (years): median, [range] | 59 [43–73] |
| 41–50 | 6 (25%) |
| 51–60 | 9 (38%) |
| 61–70 | 7 (29%) |
| 71–80 | 2 (8%) |
| Employment status | |
| Paid employment | 15 (full time 10) (63%) |
| Retired | 7 (29%) |
| Unemployed | 2 (8%) |
| Regularly care for children or dependent adult | |
| Yes | 8 (33.3%) |
| No | 16 (66.6%) |
Table 2.
Shoulder-specific details for participants
| Condition affecting dominant shoulder | |
| Yes | 20 (83.3%) |
| No | 4 (16.7%) |
| Injury related | |
| Yes | 16 (sports 1, work 5, other 10) (66.7%) |
| No | 8 (33.3%) |
| Sudden onset of symptoms | |
| Yes | 13 (54.2%) |
| No | 11 (45.8%) |
| Involves legal claim for compensation | |
| Yes | 0 (0%) |
| No | 21 (87.5%) |
| Maybe | 1 (4.2%) |
| Unknown (item not completed) | 2 (8.3%) |
| Size of rotator cuff tear | |
| Small (< 1 cm) | 1 (4.2%) |
| Moderate (1–3 cm) | 8 (33.3%) |
| Large (3–5 cm) | 12 (50%) |
| Massive (> 5cm) | 3 (12.5%) |
The response rate to the subsequent postal questionnaires was 96% (23 of 24 patients). All returned questionnaires were fully completed. Of note, the single non-responder had completed a questionnaire at a clinic near to the date of the postal questionnaire.
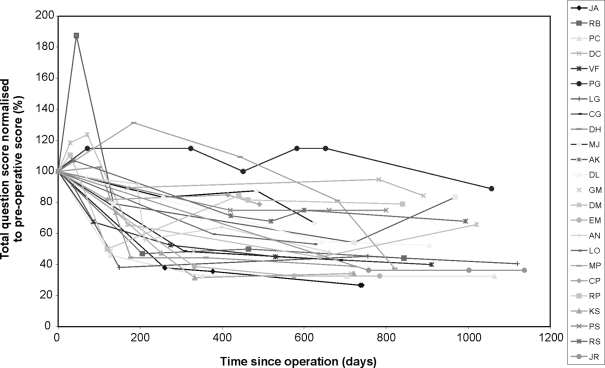
Figure 1 shows the overall scores for the group following surgery, normalised for their pre-operative score to allow comparison.
Figure 1.
Normalised outcome scores for cohort.
Overall scores improved following surgery, although not all individuals followed the same recovery and, for some, there were interesting patterns. These were reviewed in conjunction with medical notes to seek an explanation.
The score for patient ‘PG’ appears to rise following surgery. ‘PG’ had a large cuff tear and impingement, treated by open sub-acromial decompression and rotator cuff repair. Clinically, she made a slow initial recovery with on-going signs of impingement. The cuff repair was felt to be intact until 18 months (529 days) postoperatively. At this time, she had signs of weakness as well as impingement. A re-rupture was suspected and a massive tear was confirmed by ultra-sound scan. She underwent a revision open rotator cuff repair and open sub-acromial decompression 649 days after initial surgery. The cuff tear was found to be massive and irreparable. At clinical review following revision surgery, she had improved pain and function. This clinical pattern is well reflected in the outcome scores for this patient. The scores were slow to improve and there is a correlation between the rise in outcome score and diagnosis of re-rupture. Following revision surgery, her score showed improvement.
The score for patient ‘MP’, who had a moderate cuff tear and underwent open rotator cuff repair and sub-acromial decompression, was slow to improve after surgery. A review of the medical notes found that there had been a delay in the patient receiving physiotherapy due to concurrent illness but, once commenced, she went on to make a steady recovery. At over 2 years, her score had improved by 62%.
Some patients already discharged from clinic and who appeared to have a good outcome from surgery later showed a rise in their scores which may reflect a deterioration. They were contacted for a brief telephone interview to seek an explanation.
Patient ‘DM’ had a large cuff tear and had an arthroscopic sub-acromial decompression and open rotator cuff repair. No particular event was cited by the patient to account for the change. She described a slight deterioration in terms of pain and function and felt she had reached a plateau in her recovery. Components of her OSS reflected this description.
Patient ‘DC’ appeared to have shown little improvement despite surgery. However, his pre-operative score was only 19 and, although this declined to 16, with a low score initially it would be difficult for surgery to produce a dramatic improvement. Pain, particularly at night, had been his main symptom pre-operatively and had improved with surgery. This was reflected in his scores for Q1 and Q12, which fell from 3/5 pre-operatively to 1/5 postoperatively. From his perspective, surgery was worthwhile, despite a low pre-operative score, having improved his main complaint of night pain.
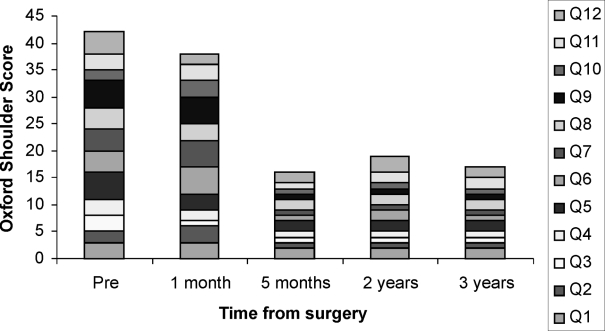
Figure 2 presents an example of changes in one individual's overall score and its components following surgery. The overall score improved by 1 month although interestingly, at this stage, the score for some questions actually rose (Q2, 6, 7 and 10) or were unchanged (Q9). All were function questions and the rise very likely reflects the initial deterioration in function reasonably expected after surgery. By 5 months, all components had markedly improved representing a good global recovery.
Figure 2.
Outcome score for an individual.
Discussion
This study demonstrates that the OSS can be used to audit the outcome of a group undergoing a particular procedure, in this case rotator cuff repair. Results indicate an overall improvement in the cohort following surgery and show changes in elements of pain and function at different stages. This information is useful for audit and pre-operative counselling about expected outcome.
The OSS can also usefully demonstrate an individual's overall progress and components of recovery following surgery. This is useful for both patient and surgeon. For the patient, the OSS serves as a useful measurement of progress. The surgeon, meanwhile, obtains an independent measure by which to judge an individual's progress and compare it to the benchmark for the group. If the trend in an individual's score diverges from the cohort, the surgeon may be alerted to a problem.
Good correlation was apparent between the OSS and clinical findings, demonstrated when outliers were contacted and their medical notes reviewed. Therefore, it appears sensitive to clinical change, and confirms the results of previous studies in this regard.5,12
Of all questionnaires, 97% were completed fully, showing that the questionnaire was easy to complete and data collection using the OSS was comprehensive. The response rate to the postal questionnaire was very high (96%), higher than quoted for some other self-administered postal questionnaires.23 All returned postal questionnaires were complete. This indicates that the OSS can be used to follow a cohort for audit purposes without needing additional clinics, enabling the surgeon to obtain long-term longitudinal follow-up in a more cost-effective manner.
A postal questionnaire helps to reduce the numbers of discharged patients lost to follow-up. This gives a better reflection of true outcome by including all patients who have undergone surgery and not just those attending clinics in the early postoperative phase or because of on-going problems. The return of a postal questionnaire showing a rise in outcome score may highlight a problem requiring patient recall prompted by the surgeon rather than solely by the patient.
The main weakness of this study was the small sample size. However, the key aim was not to draw absolute conclusions about outcome from rotator cuff surgery but rather to consider whether the use of a patient-based questionnaire is helpful in auditing shoulder surgery.
A larger prospective study is now required to confirm the findings of this pilot study. It would be interesting to investigate whether the outcome, measured with the OSS, varies with age, gender and size of cuff tear, as expected. A larger cohort would also allow benchmarking of the OSS against current methods of assessing clinical outcome and allow a standardised cut-off for good or poor clinical outcome to be determined.
Appendix 1 The Oxford Shoulder Score questionnaire
References
- 1.Chakravarty KK, Webley M. Disorders of the shoulder: an often unrecognised cause of disability in elderly people. BMJ. 1990;300:848–9. doi: 10.1136/bmj.300.6728.848-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chard MD, Hazleman R, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34:766–9. doi: 10.1002/art.1780340619. [DOI] [PubMed] [Google Scholar]
- 3.Badley EM, Tennant A. Changing profile of joint disorders with age: findings from a postal survey of the population of Calderdale, West Yorkshire, United Kingdom. Ann Rheum Dis. 1992;51:366–71. doi: 10.1136/ard.51.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Schaardenburg D, Van den Brande KJ, Ligthart GJ, Breedveld FC, Hazes JMW. Musculoskeletal disorders and disability in persons aged 85 and over: a community survey. Ann Rheum Dis. 1994;53:807–11. doi: 10.1136/ard.53.12.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593–600. [PubMed] [Google Scholar]
- 6.Uhtoff HK, Sarkar K. An algorithm for shoulder pain caused by soft tissue disorders. Clin Orthop. 1990;254:121–7. [PubMed] [Google Scholar]
- 7.McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice. 4th National Study 1991–2. London: HMSO; 1995. Office of Population Censuses and Surveys, Series MB5 No 3. [Google Scholar]
- 8.Croft P. Measuring up to shoulder pain. Ann Rheum Dis. 1998;57:65–6. doi: 10.1136/ard.57.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bamji AN, Dieppe PA, Haslock DI, Shipley ME. What do rheumatologists do? A pilot audit study. Br J Rheumatol. 1990;29:295–8. doi: 10.1093/rheumatology/29.4.295. [DOI] [PubMed] [Google Scholar]
- 10.Croft P, Pope D, Zonca M, O'Neill T, Silman A. Measurement of shoulder related disability: results of a validation study. Ann Rheum Dis. 1994;53:525–8. doi: 10.1136/ard.53.8.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ekberg K, Bjorkqvist B, Malm P, Bjerre-Kiely B, Axelson O. Controlled two year follow up of rehabilitation for disorders in the neck and shoulders. Occup Environ Med. 1994;51:833–8. doi: 10.1136/oem.51.12.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dawson J, Hill G, Fitzpatrick R, Carr A. The benefits of using patient-based methods of assessment. Medium-term results of an observational study of shoulder surgery. J Bone Joint Surg Br. 2001;83:877–82. doi: 10.1302/0301-620x.83b6.11316. [DOI] [PubMed] [Google Scholar]
- 13.MacDonald DA. The shoulder and elbow. In: Fairbank JC, Carr A, editors. Outcome Measures in Orthopaedics. Oxford: Butterworth Heinemann; 1993. pp. 144–73. [Google Scholar]
- 14.Drake BG, Callaham CM, Dittus RS, Wright JG. Global rating systems used in assessing knee arthroplasty outcomes. J Arthroplasty. 1994;9:409–17. doi: 10.1016/0883-5403(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 15.Conboy VB, Morris RW, Kiss J, Carr AJ. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br. 1996;78:229–32. [PubMed] [Google Scholar]
- 16.Wright JG, Rudicel S, Feinstein AR. Ask patients what they want: evaluation of individual complaints before total hip replacement. J Bone Joint Surg Br. 1994;76:229–34. [PubMed] [Google Scholar]
- 17.Amadio PC. Editorial. Outcomes measurement: more questions; same answers. J Bone Joint Surg Am. 1993;75:1583–4. doi: 10.2106/00004623-199311000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Fitzpatrick R, Fletcher A, Gore S, Jones D, Spiegelhalter D, Cox D. Quality of life measures in health care. I: Applications and issues in assessment. BMJ. 1992;305:1074–7. doi: 10.1136/bmj.305.6861.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dawson J, Carr A. Editorial. Outcomes evaluation in orthopaedics. J Bone Joint Surg Br. 2001;83:313–5. doi: 10.1302/0301-620x.83b3.12148. [DOI] [PubMed] [Google Scholar]
- 20.Watson EM, Sonnabend DH. Outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11:201–11. doi: 10.1067/mse.2002.122271. [DOI] [PubMed] [Google Scholar]
- 21.Sonnabend DH, Watson EM. Structural factors affecting the outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11:212–8. doi: 10.1067/mse.2002.122272. [DOI] [PubMed] [Google Scholar]
- 22.Iannotti JP. Full-thickness rotator cuff tears: factors affecting surgical outcome. J Am Acad Orthop Surg. 1994;2:87–95. doi: 10.5435/00124635-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Eaker S, Bergstrom R, Bergstrom A, Adami HO, Nyren O. Response rate to mailed epidemiologic questionnaires: a population based randomized trial of variations in design and mailing routines. Am J Epidemiol. 1998;147:74–82. doi: 10.1093/oxfordjournals.aje.a009370. [DOI] [PubMed] [Google Scholar]